Pharmacology- Exam2 – NSAIDS, Acetaminophen, & Medicines used in Gout – Flashcards
Unlock all answers in this set
Unlock answersquestion
Antipyretic
answer
A drug that reduces fever (eg, aspirin, NSAIDs, acetaminophen) MOA: suppress prostaglandin synthesis in the CNS that is stimulated by pyrogens and thereby reduces fever
question
Cyclooxygenase (COX)
answer
The enzyme at the head of the enzymatic pathway for prostaglandin synthesis
question
Cytotoxic drug
answer
Drugs that interfere with essential metabolic processes, especially DNA maintenance and replication and cell division. Such drugs generally kill rapidly dividing cells and are used for cancer chemotherapy and immunosuppression
question
Disease-modifying antirheumatic drugs (DMARDs)
answer
Diverse group of drugs that modify the inflammatory processes underlying rheumatoid arthritis; they have a slow (weeks to months) onset of clinical effects
question
Nonsteroidal anti-inflammatory drugs (NSAIDs)
answer
Inhibitors of cyclooxygenase; the term nonsteroidal differentiates them from steroid drugs that mediate anti-inflammatory effects through activation of glucocorticoid receptors (eg, cortisol)
question
Reye's syndrome
answer
A rare syndrome of *rapid liver degeneration* and *encephalitis* in *children* treated with *aspirin* during a *viral* infection
question
Tumor necrosis factor-alpha (TNF-alpha)
answer
A cytokine that plays a central role in inflammation
question
Uricosuric agent
answer
A drug that increases the renal excretion of uric acid
question
Xanthine oxidase
answer
A key enzyme in the purine metabolism pathway that converts hypoxanthine -> to xanthine -> to uric acid
question
Which NSAIDs have moderate effectiveness?
answer
Ibuprofen and naproxen
question
Which NSAID has greater anti-inflammatory effectiveness?
answer
Indomethacin
question
Which NSAID has greater analgesic effectiveness?
answer
Ketorolac
question
Aspirin: MOA
answer
- irreversibly inhibits COX *COX-1:* totally shut down, so platelet can't make more *COX-2:* turns enzyme into lipoxygenase, converted to 15-Lipoxin A4, which is an anti-inflammatory compound - better at inhibiting COX-1 than COX-2, meaning it's better at preventing CV events in people who are at risk of CVD. However, not in people who are not at risk
question
COX-_ is primarily expressed in *non*inflammatory cells.
answer
COX-*1* is primarily expressed in *non*inflammatory cells.
question
COX-_ is expressed in activated lymphocytes, polymorphonuclear cells, and other inflammatory cells.
answer
COX-*2* is expressed in activated lymphocytes, polymorphonuclear cells, and other inflammatory cells.
question
Asprin's effect on the Macula Densa
answer
- Macula Densa determines renal blood flow and GFR - COX-2 event, so Aspirin effects water/salt retention COX-2 inhibition in the kidney leads to -> retention of water and sodium which can lead to -> hypertension
question
Nonselective NSAIDs: MOA
answer
- acetylate and inhibit both cyclooxygenase isoforms and thereby decrease prostaglandin and thromboxane synthesis throughout the body. - Release of prostaglandins necessary for homeostatic function is disrupted, as is release of prostaglandins involved in inflammation.
question
COX-2-selective inhibitors
answer
- have less effect on the prostaglandins involved in homeostatic function, particularly those in the GI tract -> less GI toxicity and side effects - also, little to no anti-platelet effect since COX-1 is not inhibited as strongly, if at all Examples: Celecoxib, Rofecoxib, Valdecoxib
question
COX-2 selective inhibitors: Toxicity
answer
- highly selective COX-2 inhibitors such as rofecoxib and valdecoxib carry an increased risk of myocardial infarction and stroke. The increased risk of arterial thrombosis is believed to be due to the COX-2 inhibitors having a greater inhibitory effect on endothelial prostacyclin (PGI2) formation than on platelet TXA2 formation. - Drug interaction: Celecoxib is metabolized by same CYP450 enzyme as warfarin - Valdecoxib: increased CVD in bypass patients -> removed from market - Rofecoxib: increased edema, HTN, and mortality -> removed from market
question
Major difference between the mechanisms of action of aspirin and other NSAIDs:
answer
- aspirin (but not its active metabolite, salicylate) acetylates and thereby *irreversibly* inhibits cyclooxygenase, whereas the inhibition produced by other NSAIDs is reversible. - The irreversible action of aspirin results in a *longer duration* of its antiplatelet effect and is the basis for its use as an antiplatelet drug
question
Analgesic effect of NSAIDs
answer
- less well understood - Activation of peripheral pain sensors may be diminished as a result of reduced production of prostaglandins in injured tissue -a central mechanism is operative.
question
Danger of NSAIDs
answer
- Cyclooxygenase inhibitors also interfere with the homeostatic function of prostaglandins. - Most important, they reduce prostaglandin-mediated cytoprotection in the GI tract and autoregulation of renal function - GI: particularly important how NSAIDs cause increased acid secretion and decreased mucus secretions -> ulcers
question
Aspirin: 3 therapeutic dose ranges
answer
1. *Low range* (<300 mg/d) is effective in reducing platelet aggregation 2. *Intermediate doses* (300-2400 mg/d) have antipyretic and analgesic effects 3. *High doses* (2400-4000 mg/d) are used for an anti-inflammatory effect; also causes increased body temp
question
Aspirin: Pharmacokinetics
answer
- readily absorbed and is hydrolyzed in blood and tissues to acetate and salicylic acid. - Salicylate is a reversible nonselective inhibitor of cyclooxygenase. Duration of activity is longer than pharmacokinetic half-life of drug due to irreversible COX inhibition - Elimination of salicylate is first order at low doses, with a half-life of 3-5 h. At high doses, half-life increases to 15 h or more and elimination becomes zero order. - Excretion is via the kidney.
question
Ibuprofen
answer
- well absorbed after oral administration - half-life of about 2 h, is relatively safe - GI toxicity, nephrotoxicity hypersensitivity due to increased leukotrienes - Drug Interaction: interference with aspirin's antithrombotic action
question
Which NSAIDs are noted for having the longest half-lives?
answer
Naproxen and piroxicam
question
Uses of other Nonselective NSAIDs
answer
- treatment of mild to moderate pain, especially the pain of musculoskeletal inflammation such as that seen in arthritis and gout. Do not act centrally, they act peripherally - many other conditions, including dysmenorrhea, headache, and patent ductus arteriosus in premature infants. - reduce polyp formation in patients with primary familial adenomatous polyposis. Long-term use of NSAIDs reduces the risk of colon cancer.
question
Ketorolac
answer
- notable as a drug used mainly as a systemic *analgesic,* not as an anti-inflammatory (although it has typical nonselective NSAID properties). - only NSAID available in a *parenteral* formulation.
question
Aspirin: Toxicity
answer
- most common effect from therapeutic anti-inflammatory doses = *gastric upset* - Chronic use can result in gastric ulceration, upper GI bleeding, and *renal damage* including acute failure and interstitial nephritis. - increases bleeding time - aspirin hypersensitivity - Reye's syndrome - there's no specific antidote for aspirin
question
Aspirin hypersensitivity
answer
- When prostaglandin synthesis is inhibited by even small doses of aspirin, persons with aspirin hypersensitivity (especially associated with nasal polyps) can experience *asthma* from the increased synthesis of leukotrienes. This results from the pathway being re-routed to Lipoxygenase - This type of hypersensitivity to aspirin precludes treatment with any NSAID.
question
High doses of aspirin: Toxicity
answer
- tinnitus - vertigo - hyperventilation - respiratory alkalosis
question
Very high doses of aspirin: Toxicity
answer
- metabolic acidosis - dehydration - hyperthermia - collapse - coma - death
question
Nonselective NSAIDS: Toxicity
answer
- associated with significant *GI disturbance,* but the incidence is lower than with aspirin. - risk of *renal damage* with any of the NSAIDs, especially in patients with preexisting renal disease. Because these drugs are cleared by the kidney, renal damage results in higher, more toxic serum concentrations. - Use of parenteral *ketorolac* is generally restricted to 72 h because of the risk of GI and renal damage with longer administration. - Serious hematologic reactions have been noted with *indomethacin*
question
COX-2-selective inhibitors
answer
- *reduced GI effects,* including gastric ulcers and serious GI bleeding. - same risk of *renal damage,* presumably because COX-2 contributes to homeostatic renal effects.
question
Compare Prostacyclin & Thromboxane A2
answer
- Prostacyclin (PGI2) is *vasoprotective,* promoting vasodilation and inhibition of platelet aggregation - TXA2 has opposite effects
question
Phenacetin
answer
- toxic prodrug that is metabolized to acetaminophen - still available in some other countries.
question
_______________ is the only OTC non-anti-inflammatory analgesic commonly available in the US.
answer
Acetaminophen
question
Acetaminophen: MOA
answer
- mechanism of *analgesia = unclear* - only a *weak COX-1 and COX-2 inhibitor* in peripheral tissues, which accounts for its lack of anti-inflammatory effect; does not directly inhibit PGH2 synthase, it binds a substrate that makes the enzyme work so it *interferes with PG synthesis* - may inhibit a third enzyme, COX-3, in the CNS
question
Acetaminophen: Effects
answer
- analgesic and antipyretic agent - lacks anti-inflammatory or antiplatelet effects - used in hemophiliacs
question
Acetaminophen: Toxicity
answer
- at therapeutic dosages -> *negligible toxicity;* no platelet effect, no uric acid effect, no GI effect - when taken in overdose or by patients with severe liver impairment -> dangerous *hepatotoxin* - mechanism of toxicity: involves oxidation to cytotoxic intermediates by *phase I CYP450,* which occurs when the body has low amounts of substrates for phase II conjugations (acetate and glucuronide). Prompt administration of *acetylcysteine,* a sulfhydryl donor, required - People who regularly consume 3 or more alcoholic drinks per day are at increased risk of acetaminophen-induced hepatotoxicity
question
Disease-Modifying Antirheumatic Drugs - DMARDs
answer
- heterogeneous group of agents that have anti-inflammatory actions in several connective tissue diseases. - called disease-modifying drugs because some evidence shows slowing or even reversal of joint damage, an effect never seen with NSAIDs. - also called slow-acting antirheumatic drugs because it may take 6 wk to 6 mo for their benefits to become apparent.
question
Corticosteroids
answer
- can be considered anti-inflammatory drugs with an intermediate rate of action (ie, slower than NSAIDs but faster than other DMARDs). - However, too toxic for routine chronic use - reserved for temporary control of severe exacerbations and long-term use in patients with severe disease not controlled by other agents.
question
Gout
answer
- associated with increased serum concentrations of uric acid. - Acute and Chronic Two Goals of Treatment: 1. Treat inflammation 2. Treat cause
question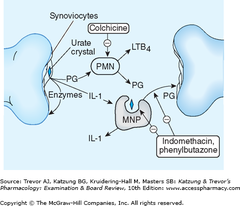
Acute gout attacks
answer
- involve joint inflammation initiated by precipitation of uric acid crystals. - Treatment strategies include: 1. reducing inflammation during acute attacks with colchicine, NSAIDs, or glucocorticoids 2. accelerating renal excretion of uric acid with uricosuric drugs such as probenecid or sulfinpyrazone 3. reducing the conversion of purines to uric acid by xanthine oxidase, using allopurinol or febuxostat
question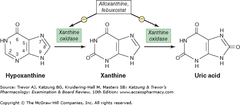
Xanthine Oxidase
answer
- enzyme that converts purines like hypoxanthine to xanthine and xanthine to uric acid, leading possibly to crystal deposits and gout - inhibited by allopurinol and febuxostat
question
NSAIDS in Gout
answer
- such as indomethacin - effective in inhibiting the inflammation of acute gouty arthritis. - reduce prostaglandin formation - inhibit crystal phagocytosis by macrophages - along with glucocorticoids, reduce the synthesis of inflammatory mediators in the gouty joint
question
Colchicine
answer
- *selective inhibitor of microtubule assembly* - reduces leukocyte migration and phagocytosis - may also reduce production of leukotriene B4 and decrease free radical formation. - since it reacts with tubulin and interferes with microtubule assembly, it's a general *mitotic poison.* Tubulin is necessary for normal cell division, motility, and many other processes.
question
______ or _____________ are preferred for the treatment of acute gouty arthritis.
answer
*NSAIDs* or *glucocorticoids* are preferred for the treatment of acute gouty arthritis.
question
Colchicine: Clinical Use and Precautions
answer
- doses required cause significant *GI disturbance,* particularly diarrhea. - Lower doses are used to prevent attacks of gout in patients with a history of multiple acute attacks. - also of value in the management of *familial Mediterranean fever*
question
Familial Mediterranean Fever
answer
- disease of unknown cause characterized by fever, hepatitis, peritonitis, pleuritis, arthritis, and, occasionally, amyloidosis. - managed by colchicine
question
Toxicity of Gout medications
answer
- NSAIDs can cause renal damage, and indomethacin can additionally cause bone marrow depression. - Short courses of glucocorticoids can cause behavioral changes and impaired glucose control. - Because colchicine can severely damage the liver and kidney, dosage must be carefully limited and monitored. Overdose is often fatal.
question
Uricosuric Agents: MOA
answer
- Normally, over 90% of the uric acid filtered by the kidney is reabsorbed in the proximal tubules. - *Probenecid and sulfinpyrazone* are weak acids that compete with uric acid for reabsorption by the weak acid transport mechanism in the proximal tubules and thereby *increase uric acid excretion* - At low doses, may also compete with uric acid for secretion by the tubule and occasionally can elevate, rather than reduce, serum uric acid concentration. - Elevation of uric acid levels by this mechanism occurs with aspirin (another weak acid) over much of its dose range.
question
Uricosuric Agents: Effects
answer
- inhibit the secretion of a large number of other weak acids like penicillin and methotrexate in addition to inhibiting the reabsorption of uric acid
question
True or False: Uricosuric drugs are used orally to treat chronic gout. These drugs are of no value in acute episodes.
answer
True
question
Uricosuric Agents: Toxicity
answer
- can cause an attack of acute gout during the early phase of their action, this can be avoided by simultaneously administering colchicine or indomethacin. - These are *sulfonamides,* so may share allergenicity with other classes of sulfonamide drugs like diuretics, antimicrobials, and oral hypoglycemic drugs - increased uric acid in kidney tubules can precipitate and form stones; must drink lots of water to prevent this. - increased UA in plasma is a risk factor for CVD
question
Allopurinol: MOA
answer
- inhibit xanthine oxidase to reduce production of uric acid - converted to *oxypurinol* or *alloxanthine* by xanthine oxidase; *alloxanthine is an irreversible suicide inhibitor* of the enzyme - allopurinol and alloxanthine inhibit other enzymes involved in purine and pyrimidine metabolism
question
Febuxostat / Uloric: MOA
answer
- a *nonpurine* reversible inhibitor of xanthine oxidase; therefore, does not interfere with purine metabolism - *more selective* and *more efficacy* than allopurinol and alloxanthine, but no evidence that it will prevent next gout attack any better - takes longer for mobilization to be acheived, so need to wait longer after the first attack before starting this
question
Xanthine Oxidase Inhibitors: Effects
answer
- increases [hypoxanthine] and [xanthine] (more soluble) - decreases [uric acid] (less soluble) -> *less precipitation of uric acid crystals in joints and tissues* - Clinical trials suggest that febuxostat is more effective than allopurinol in lowering serum uric acid.
question
Xanthine Oxidase Inhibitors: Pharmacokinetics and Clinical Use
answer
- given orally in the management of chronic gout. - Like uricosuric agents, these drugs are usually withheld for 1-2 weeks after an acute episode of gouty arthritis and are administered in combination with colchicine or an NSAID to avoid an acute attack. - Allopurinol is also used as an adjunct to cancer chemotherapy to slow the formation of uric acid from purines released by the death of large numbers of neoplastic cells.
question
Allopurinol: Toxicity
answer
- causes GI upset and rash - rarely may cause peripheral neuritis, vasculitis, or bone marrow dysfunction including aplastic anemia. - interferes with anti-cancer drugs and warfarin clearance
question
Xanthine Oxidase Inhibitors: Drug Interactions
answer
- Allopurinol inhibits the metabolism of mercaptopurine and azathioprine, drugs that depend on xanthine oxidase for elimination. - Febuxostat can cause liver function abnormalities, headache, and GI upset.
question
Most Toxic NSAIDs
answer
- Indomethacin - Piroxicam - Diclofenac - Tolmetin
question
Least Toxic NSAIDs
answer
- Aspirin - Salicylates - Ibuprofen
question
Which NSAID has the least evidence of causing cardiovascular incidents?
answer
Naproxen
question
Pegloticase, Krystexxa
answer
- Porcine uricase ("pig" rhymes with "Peg") - contains polyethylene glycol, which extends efficacy - for people who don't respond to other treatments - inject every 2-4 weeks - "chews up" uric acid in plasma - use prednisone, antihistamine because the body recognizes the pig enzyme as foreign
question
Pegloticase, Krystexxa: Side effects
answer
1. gout flares, resulting from mobilization from plasma 2. anaphylaxis, so it's only given in hospital setting 3. caution using in people with CVD
question
Rilonacept
answer
- fusion protein: one side is an IL-4 receptor, while the other is an immunoglobulin - has nothing to do with uric acid! - IL-1 is an important mediator in gout, - this drug *"gobbles up" IL-1* - used in chronic gout, but it's expensive - only in people unable to be treated by other methods



