Foundations Chapter 48 Skin Integrity and Wound Care practice question – Flashcards
Unlock all answers in this set
Unlock answersquestion
Which sign is an early indication of pressure that resolves without tissue loss if the pressure is eliminated? 1 Pallor or molting 2 Dark red or purple discoloration 3 Blanchable erythema 4 Nonblanchable erythema
answer
3 Blanchable erythema is an early indication of pressure that resolves without tissue loss if the pressure is removed. Pallor or molting is a sign of persistent hypoxia. Dark red or purple discoloration may indicate potential damage to blood vessels and tissue. Nonblanchable erythema is a sign of a stage I pressure ulcer.
question
Arrange the events that occur during the proliferative phase of wound healing in chronological order. 1. Contraction of the wound 2. Synthesis of collagen from fibroblasts 3. Migration of the epithelial cells from the wound edges 4. Mixing of collagen with granulation tissue
answer
2, 4, 1, 3 The proliferative phase of wound healing lasts 3 to 24 days. Fibroblasts produce collagen that provides a matrix for granulation. Then, the collagen mixes with the granulation tissue to form a matrix that supports reepithelialization. It also provides mechanical and structural support to a wound. The wound contracts during this process to reduce the area that requires healing. Finally, the epithelial cells migrate from the wound edges to resurface.
question
A patient who has an acute wound due to trauma is admitted to the emergency unit. Which nursing action for wound care is the priority in this situation? 1 Educating the patient about wound care 2 Positioning the patient in different angles 3 Encouraging the patient to drink 6 to 8 L of water 4 Applying a sterile dressing as per the health care provider's order
answer
4 An acute wound due to trauma needs an immediate intervention, such as the application of a sterile dressing to reduce bleeding and prevent sepsis. The nurse may educate the patient about hygiene and wound care, have the patient change positions to prevent pressure ulcers, and encourage the patient to drink 6 to 8 L of water to promote cell function, but these are all secondary to stopping the bleeding.
question
When cleaning a wound, which action is incorrect? 1 Using two separate swabs to clean the affected site 2 Irrigating from the least to most contaminated area 3 Applying noncytotoxic solutions using gentle friction 4 Cleaning from the surrounding skin to the site of incision
answer
4 The nurse should clean away from the wound to prevent contamination. Two separate swabs are to be used: one to clean from the top of the incision toward the draining site and another to clean from the bottom of the incision toward the draining site. Irrigation fluid should flow from the least to most contaminated area to prevent transmission of bacteria. Application of pressure while cleaning the wound should be avoided, but gentle friction may be applied while cleaning the traumatic wound with the noncytotoxic solution.
question
Which type of ulcer can be dressed with a transparent or hydrocolloid dressing? 1 Stage I 2 Stage II 3 Stage III 4 Stage IV
answer
1 A stage I pressure ulcer is an intact ulcer that can be dressed with a transparent or hydrocolloid dressing. Composite film, hydrocolloid, and hydrogel dressings are appropriate for stage II pressure ulcers. Hydrocolloid, hydrogen gel covered with foam, calcium alginate, and gauze dressings are appropriate for stage III pressure ulcers. Hydrogel covered with foam, calcium alginate, and gauze dressings are appropriate for stage IV pressure ulcers.
question
In a supine position, which site is not at risk for a pressure ulcer? 1 Ischium 2 Elbow 3 Occipital bone 4 Medial knee
answer
4 The medial knee may be at risk for a pressure ulcer in a patient who is in a side-lying position, but not in a supine position. The ischium, elbow, and occipital bone are all sites at risk for pressure ulcers in an immobilized supine patient.
question
A patient who has a stage III pressure ulcer develops a body temperature of 103° F. While changing the wound dressing, the nurse finds purulent discharge with an odor coming from the wound. What will the nurse suspect is occurring in the patient? 1 Bruising 2 Infection 3 Internal bleeding 4 Blanchable erythema
answer
2 A patient who has a stage III pressure ulcer has full-thickness skin loss. Purulent drainage with a characteristic odor and a fever are indications of wound infection. Skin discoloration to bluish and purplish color are manifestations of bruising. Internal bleeding manifests as swelling and bluish discoloration at the affected part. Blanchable erythema is visible skin redness that becomes white when pressure is applied and reddens when pressure is relieved, but it does not come with fever and purulent discharge.
question
A patient with an abdominal wound from a motor vehicle accident comes into the emergency room with evisceration. The nurse immediately places sterile gauze soaked in sterile saline over the extruding tissues. What is the rationale for this nursing action? 1 To reduce pain 2 To prevent infection 3 To prevent pressure ulcers 4 To prevent periwound edema
answer
2 Evisceration is a medical emergency in which the visceral organs protrude through a wound opening. Immediate application of sterile gauze soaked in sterile saline over the extruding tissues helps to prevent bacterial invasion, infection, and drying of the tissues. Analgesics will be used to reduce pain. Pressure ulcer prevention will not be a primary concern in an emergency situation such as this. Saline-soaked gauze will not prevent edema.
question
Which pressure ulcer site is found immediately distal to the buttock? 1 Sole 2 Ischium 3 Sacrum 4 Scapula
answer
2 The ischium pressure ulcer site is just below the buttock on the upper thigh. The sole pressure ulcer site is found on the bottom of the foot. The sacrum pressure ulcer site is on the tailbone, or just above the gluteal area. The scapula pressure ulcer site is found on the shoulder blade.
question
Which type of wound drainage is shown in the image? 1 Serous 2 Purulent 3 Sanguineous 4 Serosanguineous
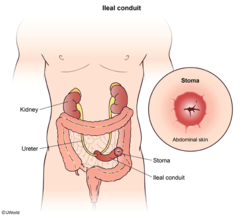
answer
4
question
According to the Braden Scale for predicting pressure ulcer risk, which factor most puts the patient at risk for developing a pressure ulcer?
answer
Poor nutrition Of these factors, the patient's poor nutrition carries the highest risk for the patient developing a pressure ulcer. The better the nutrition, the lower the risk. Moist, not dry, skin puts a patient at a greater risk for developing a pressure ulcer. Although frequent, rather than occasional, activity is ideal for reducing the risk for developing a pressure ulcer, the more immobile the patient is, the greater the chance of pressure ulcer development. Slightly limited sensory perception puts a patient at less of a risk than does very limited or completely limited sensory perception.
question
While assessing a patient who has a pressure ulcer, the nurse finds black wound tissue. In which stage is this pressure ulcer? 1 Stage I 2 Stage II 3 Stage III 4 Unstageable
answer
4 Black tissue is characteristic of an eschar. Because the eschar obscures the depth of the wound, this ulcer is unstageable. Stage I ulcers manifest as localized nonblanchable redness over intact skin. Stage II ulcers are characterized by partial-thickness dermis loss. Stage III ulcers are characterized by full-thickness skin loss to the extent that subcutaneous fat may be visible.
question
Chronologically arrange the steps for using a syringe and needle to collect a sample for a wound culture. 1. Applying suction to the 10-mL mark 2. Removing skin flora with a disinfectant solution 3. Moving the needle back and forward at different angles for two to four explorations 4. Using a 10-mL disposable syringe with a 22-gauge needle
answer
2, 4, 1, 3 The nurse first cleans the intact skin with a disinfectant solution to remove skin flora. The nurse then uses a 10-mL disposable syringe with a 22-gauge needle for extracting the wound drainage for culture. Then, 0.5 mL of air is drawn into the syringe to ease the suction up to the 10-mL mark. Lastly, the nurse moves the needle back and forward at different angles for two to four explorations, expels the excess air from the syringe, and prepares the syringe for the laboratory.
question
The nurse is preparing a care plan for a patient who has a pressure ulcer on the coccyx. Which part of the plan is included to provide comfort to the patient? 1 Repositioning the patient every 90 minutes 2 Cleaning and massaging around the affected area 3 Elevating the head of the patient's bed to 30 degrees 4 Applying a moisture barrier ointment over the ulcer
answer
4 Ointments may decrease friction with the sheets and cover the affected area, encouraging healing and moisture in open ulcers and minimizing patient discomfort. The patient should be repositioned every 90 minutes to reduce pressure over vulnerable areas of the body, but this does not necessarily relieve the patient's discomfort. Elevation of the patient's head of the bed is avoided to minimize further pressure on the sacrum and coccyx. Rubbing or massaging the affected areas may cause tissue damage, so this is avoided.
question
The nurse performs the skin and risk assessment on a patient who has diabetes and limited mobility due to a fractured left hip and finds that the skin is intact without any skin disintegration. Which nursing intervention should the nurse provide to the patient? 1 Place a pillow under the patient's calves. 2 Position the patient at a 30-degree medial turn. 3 Use standard hospital foam mattresses for the patient. 4 Recommend alternating pressure support surfaces for the patient.
answer
1 Although the patient's skin is currently healthy, the patient's diabetes and limited mobility put this patient at a high risk for developing pressure ulcers. As a preventive measure, the nurse should place a pillow under the calves of the patient to elevate the heels to reduce the risk of heel breakdown. Such patients should be positioned at a 30-degree lateral, not medial, turn position to avoid typical at-risk pressure points. The nurse should use higher-specification foam mattresses rather than standard hospital foam mattresses. Alternating pressure support surfaces are needed for patients who already have ulcers. These are not necessary for this patient.
question
Which factor does not put a patient at risk for burns during heat therapy? 1 Very young age 2 Areas of edema 3 Abscessed tooth 4 Peripheral vascular disease
answer
3 Applying heat to an abscessed tooth may increase a patient's risk for infection due to the possibility of rupture, but it will not necessarily increase the risk for burns. Because very young patients have thin skin, they are at an increased risk for burns during heat therapy. Because areas of edema and peripheral vascular disease both cause a patient to have decreased sensory perception, patients with these conditions are also at an increased risk for burns during heat therapy.
question
Upon assessing a patient's surgical incision on the left hip, the nurse observes reddened periwound tissue, foul drainage, and open areas between the staples. What is the likely nursing diagnosis? 1 Risk for infection 2 Risk for inflammation 3 Impaired skin integrity related to limited mobility 4 Impaired physical mobility related to incisional pain
answer
1 The nurse's observations of reddened tissue, drainage, and open areas between the staples are characteristic of infection. The reddened periwound tissue may also indicate inflammation, but the drainage and open areas do not. Impaired skin integrity related to limited mobility would be characterized by pressure ulcers and reactive hyperemia. Impaired physical mobility related to incisional pain would be indicated by the patient reporting pain, resisting assisted movement, and not moving in bed.
question
What action will the nurse take while removing a dressing on an older adult patient? 1 Pull the skin from the adhesive 2 Pull the adhesive from the skin 3 Push the skin away from the adhesive 4 Push the adhesive away from the skin
answer
3 Because the skin of older patients has reduced elasticity and is thinner, the nurse should protect the patient's skin from injury during dressing removal by pushing the skin away from the adhesive. Pulling the skin from the adhesive, pulling the adhesive from the skin, and pushing the adhesive away from the skin may tear the patient's skin.
question
What are the therapeutic benefits of heat application? Select all that apply. 1 It decreases tissue oxygen needs. 2 It promotes the movement of waste products. 3 It reduces blood flow to injured body parts. 4 It improves blood flow to injured body parts. 5 It improves delivery of leukocytes to the wound site.
answer
2, 4, 5 The application of heat is helpful in promoting the movement of waste products and nutrients, improving blood flow to injured body parts, and aiding in the delivery of leukocytes to the wound site. Therapeutic application of cold reduces tissue oxygen needs and blood flow to injured body parts.
question
What is characteristic of stage III pressure ulcers? 1 Underlying muscle is exposed 2 Slough may be present, but it does not obscure the depth of tissue loss. 3 Discoloration of the skin, warmth, edema, hardness, and/or pain may be present. 4 It presents as a shallow, open ulcer with a red-pink wound bed without slough.
answer
2 In a stage III pressure ulcer, there is full-thickness skin loss. Slough may be present, but it does not obscure the depth of tissue loss. In a stage IV pressure ulcer, there is full-thickness tissue loss, exposing bone, tendon, or muscle. In a stage I pressure ulcer, there may be discoloration of the skin, warmth, edema, hardness, or pain. In a stage II pressure ulcer, partial-thickness loss of dermis presents as a shallow, open ulcer with a red-pink wound bed without slough.
question
What should the nurse consider when developing a nursing plan for an immobile patient whose skin is intact but is at a high risk for impaired skin integrity? Select all that apply. 1 Consider either a low-air-loss, alternating pressure, or air-fluidized support surface. 2 Use a pillow under the calves so that the heels are elevated to reduce the risk of heel breakdown. 3 Consider the use of a wheelchair cushion. 4 Use an active support surface, such as an overlay or mattress, when frequent manual repositioning is difficult. 5 Avoid prolonged head-of-bed elevation and a slouched position that places pressure and shear on the sacrum and coccyx.
answer
2, 4, 5 For an immobile patient whose skin is intact but is at high risk for impaired skin integrity, the nurse should plan to use a pillow under the calves so that the heels are elevated to reduce the risk of heel breakdown. The nurse should also use an active support surface, such as an overlay or mattress, when frequent manual repositioning is difficult. Avoiding should also be part of the nursing plan prolonged head-of-bed elevation and a slouched position that places pressure and shear on the sacrum and coccyx. The nurse should consider using either low-air-loss, alternating pressure, or air-fluidized support surface for patients who already have pressure ulcers. The nurse will also consider using a wheelchair cushion for a patient who has a sacral or coccyx pressure ulcer.
question
What are the implications for healing of a surgical incision? Select all that apply. 1 Heals by epithelialization 2 Lacks wound contraction 3 Clean and intact wound edges 4 Lacks granulation tissue formation 5 Heals quickly with minimal scar formation
answer
1, 3, 5 In the case of a wound caused by a surgical incision, healing occurs by epithelialization, the edges are clean and intact, and healing is quick with minimal scar formation. Wound contraction is present, not absent. Granulation tissue forms.
question
What step is a component of the planning phase for a patient who has impaired skin integrity? 1 Involve the patient and family in choosing interventions. 2 Apply standards of practice outlining expected outcomes. 3 Examine the patient's skin for impairment of skin integrity. 4 Ask the patient for his or her perception of skin integrity after the intervention.
answer
1 Involving the patient who has impaired skin integrity and his or her family in choosing interventions is part of the planning phase. Applying the standards of practice outlining the expected outcomes is part of the evaluation phase. Examining the patient's skin for impairment of skin integrity is part of the assessment phase. Asking the patient for his or her perception of skin integrity after the intervention is part of the evaluation phase.
question
A nursing instructor discusses with a nursing student the changes that occur in the skin with aging. Which of the student's statements indicates the need for further teaching? 1 "The elasticity of the skin decreases with age." 2 "The collagen content of the skin increases with age." 3 "The underlying muscle and tissues become thinner with age." 4 "The older adult's skin can be easily torn in response to mechanical trauma."
answer
2 The collagen content of the skin decreases, not increases, with age. The remaining statements indicate understanding. The elasticity of the skin decreases with aging, and the underlying muscle and tissues thin. Because of these changes, the older adult's skin can be easily torn in response to mechanical trauma.
question
Which interventions are part of the nursing intervention classification (NIC) of pressure management? Select all that apply. 1 Repositioning the patient every 90 minutes 2 Irrigating the wound with a saline solution two times per day 3 Avoiding the use of massage around the open area 4 Dressing the area two times per day per provider prescription 5 Elevating the head of the patient's bed to no more than 30 degrees
answer
1, 3, 5 Repositioning the patient every 90 minutes, avoiding the use of massage around the open area, and elevating the head of the bed to no more than 30 degrees are parts of the nursing intervention classification (NIC) of pressure management. Irrigating a wound with a saline solution and dressing the area twice a day are interventions that are parts of the NIC of wound care.
question
A patient's wound drainage appears thick and yellow. Which type of drainage is this considered? 1 Serous 2 Purulent 3 Sanguineous 4 Serosanguineous
answer
2 Purulent drainage is thick and yellow, green, tan, or brown. Serous drainage is clear, watery plasma. Sanguineous drainage is bright red, indicating active bleeding. Serosanguineous drainage is pale pink and watery.
question
Which statement is true regarding cold application? 1 It causes vasodilation. 2 It reduces blood viscosity. 3 It decreases muscle tension. 4 It increases tissue metabolism
answer
3 Cold application decreases muscle tension and helps relieve pain. Heat, not cold, application causes vasodilation, reduced blood viscosity, and increased tissue metabolism due to increase in blood flow.
question
Which can cause an acute wound? Select all that apply. 1 Trauma 2 Pressure 3 Surgical incision 4 Vascular compromise 5 Repetitive insults to tissue
answer
1, 3 Trauma and surgical incision can cause acute wounds. Pressure, vascular compromise, and repetitive insults to tissue can cause chronic, not acute, wounds.
question
What type of wound drainage is considered sanguineous? 1 Clear, watery plasma 2 Bright red, active bleeding 3 Thick and yellow, green, tan, or brown 4 Pale pink, watery mixture of clear and red fluid
answer
2 Bright red fluid indicative of active bleeding is considered sanguineous wound drainage. Clear, watery plasma is considered serous wound drainage. Thick and yellow, green, tan, or brown fluid is considered purulent wound drainage. A pale pink, watery mixture of clear and red fluid is considered serosanguineous wound drainage.
question
Which is the most effective intervention for compromised skin integrity? 1 Preventing breakdown 2 Administering medication 3 Implementing wound care 4 Monitoring wound healing
answer
1 The most effective intervention for compromised skin integrity and wound care is prevention of skin breakdown. Whereas administering medication, implementing wound care, and monitoring wound healing are all important nursing actions, prevention is the first step.
question
Which nursing interventions minimize the risk for pressure ulcer development? Select all that apply. 1 Repositioning the patient every two hours 2 Using a draw sheet to assist with repositioning 3 Conducting a nutritional assessment every 8 hours 4 Applying barrier creams for patients who are incontinent 5 Providing education related to preventing skin breakdown
answer
1, 2, 4, 5 Three major areas of nursing interventions for prevention of pressure ulcers are: (1) skin care and management of incontinence, such as applying barrier creams for patients who are incontinent; (2) mechanical loading and support devices, which include proper positioning and the use of therapeutic surfaces, such as repositioning the patient every 2 hours and using a draw sheet during repositioning; and (3) education, such as information related to preventing skin breakdown. Conducting a nutritional assessment is important; however, this is a part of assessment and is not necessary every 8 hours.
question
Which nursing intervention is appropriate for a patient who is at risk for skin breakdown due to moisture? 1 Keep the skin dry and free of maceration 2 Provide a pressure-redistribution surface 3 Consult a dietician for nutritional assessment 4 Provide a trapeze to facilitate movement in bed
answer
1 Whereas all of these interventions are appropriate for a patient who is at risk for skin breakdown, the one specific to a patient at risk for skin breakdown due to moisture is to keep the skin dry and free of maceration. Providing a pressure-redistribution surface is appropriate for a patient who is at risk for skin breakdown due to decreased sensory perception. Consulting a dietician for a nutritional assessment is appropriate for a patient who is at risk for skin breakdown due to poor nutrition. Providing a trapeze to facilitate movement in bed is appropriate for a patient who is at risk for skin breakdown due to friction and shear.
question
Which interventions should the nurse implement when providing care to a patient at risk for skin breakdown due to urinary incontinence? Select all that apply. 1 Provide adequate fluid intake 2 Reposition the patient off at-risk areas often 3 Apply a moisture-barrier ointment 4 Cleanse perineal area with no-rinse cleaner 5 Protect pressure points from medical devices
answer
2, 3, 4 For a patient at risk for skin breakdown due to urinary incontinence, the nurse should reposition the patient off at-risk areas often, apply a moisture-barrier cream, and cleanse the perineal area with an on-rinse cleaner. Whereas providing adequate fluid intake and protecting pressure points from medical devices are appropriate interventions for a patient who is at risk for skin breakdown, these do not address the risk for skin breakdown due to urinary incontinence.
question
For which pressure ulcers would the nurse include education related to both granulation and reepithelialization? Select all that apply. 1 Stage I 2 Stage II 3 Stage III 4 Stage IV 5 Unstageable
answer
3, 4 Stage III and IV pressure ulcers are expected to heal through granulation and reepithelialization, so the nurse would educate the patients on these expected changes. The nurse would teach a patient with a stage I ulcer about healing over 7 to 14 days, a patient with a stage II ulcer about healing via reepithelialization, and a patient with an unstageable ulcer about softening the eschar with debridement.
question
Which nursing intervention is appropriate for a patient who is at risk for infection due to a surgical incision at the right hip? 1 Applying moisture barrier cream 2 Obtaining a wound culture as needed 3 Providing analgesics prior to wound care 4 Using correct repositioning techniques
answer
2 Whereas all of these interventions are appropriate for a patient with impaired skin integrity, the intervention that is specific to a patient at risk for infection is obtaining a wound culture as needed. Applying a moisture barrier is appropriate when the patient's skin integrity is compromised due to limited mobility. Providing analgesics and using correct repositioning techniques are appropriate interventions for impaired physical mobility related to incisional pain.
question
Which pressure ulcer is expected to heal through granulation and reepithelialization? 1 Stage I 2 Stage II 3 Stage IV 4 Unstageable
answer
3 Stage IV pressure ulcers are expected to heal through granulation and reepithelialization. Wound care for a stage I pressure ulcer is aimed at slow healing without epidermal loss over 7 to 14 days. Stage II pressure ulcers are expected to heal through reepithelialization. Wound care for an unstageable pressure ulcer includes debridement done to soften the eschar.
question
Which nursing intervention is appropriate for a patient who is at risk for skin breakdown due to friction and shear? 1 Keep the skin dry and free of maceration 2 Provide pressure-redistribution surface 3 Consult a dietician for nutritional assessment 4 Provide a trapeze to facilitate movement in bed
answer
4 Whereas all of these interventions are appropriate for a patient who is at risk for skin breakdown, the one specific to a patient at risk for skin breakdown due to friction and sheer is to provide a trapeze to facilitate movement in the bed. Keeping the skin dry and free of maceration is appropriate for a patient who is at risk for skin breakdown due to moisture. Providing a pressure-redistribution surface is appropriate for a patient who is at risk for skin breakdown due to decreased sensory perception. Consulting a dietician for a nutritional assessment is appropriate for a patient who is at risk for skin breakdown due to poor nutrition.
question
Which nursing action is appropriate when providing care to a patient who has intact skin but is at high risk for impaired skin integrity of the heels? 1 Avoid prolonged elevation of the head of the bed 2 Order a standard hospital foam mattress 3 Consider an alternating pressure support surface 4 Place a pillow under the calves
answer
4 The nursing action that is appropriate for a patient who has intact skin but is at high risk for impaired skin integrity of the heels is to place a pillow under the calves to decrease the risk for heel breakdown. Avoiding prolonged elevation of the head of the bed is appropriate for a high-risk patient who already has a pressure ulcer. Ordering a standard hospital foam mattress is appropriate for a high-risk patient who is not at risk for impaired skin integrity. Considering an alternating pressure support surface is appropriate for a patient who is already diagnosed with an ulcer.
question
Which nursing interventions are appropriate for a patient who is at risk for pressure ulcer development due to impaired mobility or friction and shear? Select all that apply. 1 Assisting with meals 2 Applying a moisture barrier cream 3 Establishing a schedule for repositioning 4 Limiting head elevation to 30 degrees 5 Repositioning with a transfer board surface
answer
3, 4, 5
question
Which task can be delegated to nursing assistive personnel (NAP) in caring for a patient who has pressure ulcers? 1 Applying an elastic bandage 2 Performing wound irrigation 3 Implementing negative-pressure wound therapy 4 Assessing the patient for the risk of additional pressure ulcers
answer
1 The task of applying an elastic bandage can be delegated to nursing assistive personnel (NAP). The task of performing wound irrigation cannot be delegated to NAP, because it requires a sterile technique for wound care. The task of implementing negative-pressure wound therapy cannot be delegated to NAP. NAP are not allowed to assess patients for the risk of pressure ulcers; only health care providers can perform this assessment.
question
Which intervention can be performed by nursing assistive personnel (NAP) while caring for a patient who has a chronic wound? 1 Cleaning the wound if there is any drainage 2 Performing sterile dressing of the wound 3 Redressing the wound if the dressing becomes dislodged 4 Reporting changes in the skin integrity to the registered nurse immediately
answer
4 The role of nursing assistive personnel (NAP) in providing care to a patient who has a chronic wound is to report changes in the skin integrity to the nurse immediately. The NAP should not clean the wound in case of any drainage, but should notify the nurse immediately. The NAP should not perform the sterile dressing, but can perform the nonsterile dressing for the chronic wound. The NAP should report to the nurse if the dressing of the wound is dislodged, but should not redress the wound.
question
The nurse notes a quarter-sized area of blanchable erythema over the patient's sacral area. The nurse knows this finding is likely due to what? 1 Friction 2 Pressure 3 Massage 4 Sheering force
answer
2 Blanchable erythema is an early indication of pressure; therefore, the nurse knows this finding on the patient's sacral area is due to pressure. Friction may not cause blanchable erythema in the patient, but it increases the risk of developing pressure ulcers. Massage may not be responsible for developing blanchable erythema in the patient, but it reduces the risk of pressure ulcers. Blanchable erythema does not indicate sheering force.
question
The nurse determines the patient's risk of developing ulcers using the Braden Scale and finds the score to be 16. Which nursing interventions are appropriate for the patient to decrease the risk of skin breakdown? Select all that apply. 1 Protecting the patient's heels 2 Turning the patient frequently 3 Providing pressure-redistribution surfaces 4 Providing foam-wedges for 40-degree lateral position 5 Applying a moisturizer to the patient's wound regularly
answer
1, 2, 3 A patient with a score of 16 on the Braden scale indicates that the patient is at risk for pressure ulcers. The patient in this condition should be provided with interventions that protect the heels, because this site is more susceptible to ulcer formation. The patient should frequently be turned to prevent the risk of pressure ulcer development. The patient should also be provided with pressure-redistribution surfaces to prevent ulcer formation. Foam wedges should be provided for the 30-degree lateral position, not the 40-degree lateral position. Application of moisturizer should be avoided in the patient, because it increases the risk of ulcer formation.
question
The nurse is evaluating the outcome of a patient provided with negative-pressure wound therapy (NPWT) for pressure ulcers. Which nursing action is appropriate for determining the patient's level of comfort while providing the treatment? 1 Determining the drainage and odor of the wound 2 Verifying proper negative-pressure in the patient's wound 3 Asking the patient to rate the pain using a scale of 0 to 10 4 Comparing the wound size with a baseline wound assessment
answer
3 Asking the patient to rate the pain using a scale of 0 to 10 helps the nurse determine the patient's level of comfort during the procedure. Inspecting the condition of the wound and noting the drainage condition and odor helps determine the status of wound healing, but not the patient's level of comfort. Verifying airtight dressing seal and proper negative pressure helps achieve prescribed vacuum level of the therapy. Comparing the wound size and condition with a baseline wound assessment helps provide objective information of wound healing.
question
The nurse observes that a patient with pressure ulcers has a score on the Braden Scale of 11. What would the nurse suspect from this observation? 1 The patient is at high risk of development of pressure ulcers. 2 The patient is at moderate risk of pressure ulcer development. 3 The patient should be taken to the intensive care unit. 4 The patient's condition can be managed in a few days.
answer
1 The Braden Scale provides a baseline for comparing increased or decreased risk for development of pressure ulcers that helps plan for interventions. If the score is 10 to 12, then the patient is at high risk of developing pressure ulcers; therefore, this patient is considered at a high risk of pressure ulcer development. If the score is 13 to 14, then the patient is at moderate risk of developing pressure ulcers. If the score is lower than 9, it indicates severe complication and the patient should be taken to the intensive care unit immediately. If the score is high, it indicates low risk, and the condition can be managed in a few days with minimal interventions.
question
Which fluids if exposed to the skin pose the highest risk for skin breakdown? 1 Ascitic fluids 2 Biliary secretions 3 Gastric secretions 4 Purulent wound exudates
answer
3 Continuous exposure of the skin to body fluids may cause skin breakdown, thus causing pressure ulcers. Therefore, exposure of the skin to gastric secretions poses the highest risk for skin breakdown. This is mainly due to the digestive quality that is responsible for the skin irritation. Ascitic fluids, biliary secretions, and purulent wound exudates carry a moderate risk of skin breakdown.
question
While assessing a patient with the Braden Scale, the nurse suspects that the patient is at very high risk of pressure ulcer development. What might be the patient's score? 1. 8 2. 10 3. 13 4. 17
answer
1 The Braden Scale provides a baseline for comparing increased or decreased risk for development of pressure ulcers that helps plan for patient interventions. The lower the Braden Scale score, the worse the prognosis of the disease. The patient is considered to be at a very high risk for developing pressure ulcers if the score is 9 or below; therefore, the patient with a score of 8 would be at a very high risk for pressure ulcer development. If the score is 10 to 12, then the patient is at high risk for developing pressure ulcers. If the score is 13 to 14, then the patient is at moderate risk for developing pressure ulcers. A score of 15 to 18 indicates risk of the general population when it comes to developing pressure ulcers.
question
What color is sanguineous drainage on a patient's dressing? 1 Pink 2 Clear 3 Yellow 4 Bright red
answer
4 Sanguineous drainage indicates fresh bleeding and is bright red. Serosanguineous drainage is pink. Serous drainage is clear. Purulent drainage is thick and yellow.



