Exam 3 Menopause – Flashcards
Unlock all answers in this set
Unlock answersquestion
What is menopasue?
answer
diagnosed after 12 months of amenorrhea with no obvious pathologic cause
question
When does menopause occur? And what May cause it to come early?
answer
Average age 50-51 years No relationship between menarche and age of menopause Marriage, childbearing, height, weight, and prolonged use of oral contraceptives do not influence age of menopause. *Smoking is associated with early menopause.*
question
What are symptoms of menopause and helpful to establish it?
answer
May be associated with vasomotor symptoms, sleep disturbance, and vaginal/urinary symptoms Estradiol <20 pg/mL and follicle-stimulation hormone level 21-100 mU/mL helpful in establishing the diagnosis
question
According to the 2010 US census, of the 155 million women in this country, 41 million were 55 years of age or older. Most of these women had or shortly would have their last menstrual period, thus becoming postmenopausal. how long will a women on average live after menopause?
answer
woman at age 55 years can expect to live another 28 years, a large portion of the female population is without ovarian function and lives about one-third of their lives after this function ceases. "Consequently, physicians caring for women must understand the hormonal and metabolic changes associated with the menopause, or "change of life," and the potential benefits and risks of hormone therapy (HT)."
question
Induced menopause =
answer
permanent cessation of menstruation after bilateral oophorectomy or ablation of ovarian function (ie, by chemotherapy or radiation)
question
Premature menopause =
answer
menopause reached at or before age 40 and can be natural or induced
question
Perimenopause/menopause =
answer
menstrual cycle and hormonal changes that occur a few years before and 12 months after the final menstrual period resulting from natural menopause. the menstrual cycle is likely to be irregular and when other symptoms or complaints may be experienced.
question
Menopause =
answer
final menstruation
question
Postmenopause =
answer
phase of life that comes after the menopause.
question
*graph of the reproductive cycle staging*
answer
Few years riot and one year after.
question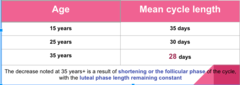
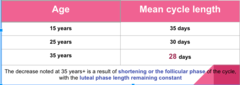
Decades of mature reproductive life are characterized by a generally regular menses and a slow, steady decrease in cycle length that looks like what?
answer
The decrease noted at 35 years+ is a result of shortening or the follicular phase of the cycle, with the luteal phase length remaining constant
question
*Graph of women ages below 45 and over 45 and hormones they go through?*

answer
25-35
question
What causes negative feedback on FSH. What does this mean.
answer
Inhibin - hormone synthesized and secreted by the ovarian oocyte. As oocyte number decreases, inhibin levels fall, resulting in a rise in FSH levels (diagnostic marker of menopause). Follicular atresia results in declining estrogen and inhibin The irregular episodes of vaginal bleeding in premenopausal women represent the irregular maturation of ovarian follicles with or without hormonal evidence of ovulation.
question
A 52-year-old female presents with a primary complaint of amenorrhea for the past 6 months. She also reports dyspareunia, recurrent headache, and infrequent episodes of night sweats. Diagnostic work-up reveals increased serum FSH levels. Which additional laboratory findings would most likely be seen in this patient?
answer
a. Increased estradiol & decreased LH b. Increased progesterone & increased LH *c. Decreased estrogen & Increased LH* d. Decreased Progesterone & Increased testosterone
question
Two types of menopause:
answer
Physiologic menopasue artificial menopause
question
what is physiologic menopause?
answer
Oocytes responsive to gonadotropins (LH, FSH) disappear from the ovary The few remaining oocytes stop responding to the Gonadotropins (LH, FSH) Can be hastened by: Severe infections tumor of reproductive tract Excessive exposure to ionizing radiation Chemo-therapeutic drugs Surgical procedures impairing ovarian blood supply Endocrine or chromosomal abnormalities
question
Artificial Menopause
answer
Permanent cessation Surgical removal of ovaries When laparotomy is performed for intra-abdominal or pelvic disease (hysterectomy for leiomyomata) Elective bilateral oophorectomy (prevention of ovarian cancer) Radiation therapy Irradiation to ablate ovarian function SE of intra-abdominal disease (damaged by infection or neoplasia)
question
Premature Menopause/Premature Ovarian Failure
answer
Spontaneous amenorrhea before age 40 Prevalence - 0.9% Cessation of menstruation and the development of climacteric (period of decrease of reproductive capacity in women, culminating in menopause) symptoms (hot flushes) and complaints can occur as early as a few years after menarche. *Etiology is unknown. FSH >30 mlU/ml*
question
What are the 2 stages of perimenopause?
answer
EARLY - (-2)
question
Early - (-2) perimenopause stage
answer
Menstrual cycles remains regular Cycle length changes by 7 days or more (i.e. length is now 24 days vs. 31)
question
LATE - (-1) perimenopause stage
answer
Interval of amenorrhea of > 60 days Characterized by increased variability in cycle length. FSH is usually > 25 IU/L Most women begin to experience symptoms including vasomotor symptoms Sleep disturbances Duration typically 1-3 years
question
Can Menopause be Prevented?
answer
Nothing can prevent menopause(ovarian function cannot be prolonged indefinitely), nothing can be done to postpone its onset or slow its progress. However, artificial menopause can often be prevented. When ionizing radiation is used for treatment of intra-abdominal disease, incidental ablation of ovarian function often cannot be avoided. In such cases, if an operation will serve equally well to treat the disease, it should be used in preference in order to preserve the ovaries.
question
3 menopause physical changes?
answer
Reproductive Tract Urinary Tract Regression of breast size
question
What happens to the Reproductive tract in menopause?
answer
Atrophic changes vaginal epithelium- can lead to Atrophic vaginitis Cervix - can lead to Dyspareunia Uterine - beneficial for those with endometriosis and uterine myomas (become asymptomatic) Ovarian - small size if an ovary is palpated on an exam you must have a high degree of suspicion and ovarian neoplasm must be considered.
question
What happens to the urinary tract in menopause?
answer
Atrophic changes Bladder - Atrophic cystitis Urethra - Urethral Caruncle formation Recurrent UTI's
question
Atrophic and Recurrent Cystitis characterized by what?
answer
characterized by urinary urgency, frequency, incontinence, and dysuria.
question
What is a Urethral Caruncle?
answer
Benign fleshy outgrowth at the urethral meatus. Loss of urethral tone, with pouting of the meatus and thinning of the epithelium, favors the formation of a urethral caruncle with resultant: dysuria, meatal tenderness, and occasionally hematuria.
question
Clinical Conditions Associated with Menopause include?
answer
Atrophic Vaginitis Hot Flushes Osteoporosis Sexual Dysfunction
question
What pathogenesis causes atrophic vaginitis?
answer
Smooth, shiny, pale epithelial surface due to increasingly sparse capillary bed. ?in vaginal PH due to reduced glycogen in the vaginal epithelium ?bacterial invasion due to disappearance of lactobacilli.
question
What are atrophic vaginitis S;S?
answer
Vaginal Complaints Pruritus, burning, soreness, dyspareunia, Leukorrhea, thin watery or serosanguineous discharge. Minimal trauma with examinations or coitus may result in slight vaginal bleeding. Urinary complaints: Urinary frequency, urgency, dysuria, and urge incontinence,
question
How do you diagnose and treat atrophic vaginitis?
answer
Diagnosis based on patient symptomatology and physical exam Treatment water -soluble lubricants Vaginal estrogen preparations preferred (vs. systemic combo's)
question
What is the most COMMON and characteristic symptom of peri-menopause?
answer
Hot Flushes Present in 75% of women 82% have the symptom > 1 year 25-50% complain of the symptom > 5 years Length varies from 1-10 minutes Average length of 4 minutes Frequency varies from 1-2/hour to 1-2/week. In women with severe flushes, the mean frequency is 54 minutes
question
How would a patient describe a hot flash?
answer
Begin with a sensation of pressure in the head, much like a headache. Progresses in intensity until the physiologic flush occurs. characterized as a feeling of heat or burning in the face, neck, and chest, Followed immediately by an outbreak of sweating Affects the entire body Particularly prominent over the head, neck, upper chest, and back. Palpitations may also be experienced. Less common symptoms include: Weakness, Fatigue, Faintness, Vertigo
question
Hot flushes are a greater annoyance than most physicians recognize. Patients frequently complain of night sweats and insomnia. There is a close relationship between hot flushes occurrence and nighttime awakening. What might this lead to?
answer
Women with frequent flushes may experience flushes and awakenings hourly, which may cause profound sleep disturbance that may in turn, cause cognitive (memory) and affective (anxiety) disorders.
question
Pathogenesis of hot flushes?
answer
Exact mechanism is unknown Some evidence it is a result of a central thermoregulatory function defect. CNS concentrations of norepinephrine and serotonin likely play an important role. Serotonin is also thought to be important in thermoregulation
question
What are Treatments for hot flushes?
answer
Progestins - Second line treatment Avoid in patients with breast disease Clonidine SSRI's and SNRI's - Second Line Treatment Black Cohosh (herbal) - modest effects (concern with stimulation of breast and uterine tissues) Gabapentin - decreases hot flashes by 50-80% (comparable to estrogen in studies!). However sedation is a major side effect limiting its use. Tibolone (synthetic steroid)
question
What is osteoporosis?
answer
Systemic skeletal disorder characterized by: Low bone mass Microarchitectural deterioration of bone tissue, Increase in fragility of bone Susceptibility to risk of fracture. Although gradual bone loss occurs in all humans with aging, this loss is accelerated in women after cessation of ovarian function. After attainment of peak bone mass by age 25-30 years, bone loss begins, accelerates in women at menopause, and then slows again but continues into advanced years at a rate of 1-2% per year Women can lose up to 20% of their bone mass in the 5-7 years after menopause.
question
Bone loss produces minimal symptoms, but leads to reduced skeletal strength. Thus osteoporotic bones are more susceptible to fractures. Most common site of fractures are?
answer
vertebral body, proximal femur, distal forearm/wrist.
question
Pathogenesis for osteoporosis?
answer
Bone loss occurs because bone resorption is excessive, bone formation is decreased, peak bone mass is low, or a combination of all 3 factors. Ovarian estrogen and estrogen administered postmenopausally are protective against osteoporosis. The exact mechanisms by which estrogen regulates bone remodeling are incompletely understood. Estrogens likely modulate osteoclast and osteoblast function possibly via: Effects on cytokines Effects on growth factors transforming growth factor-? tumor necrosis factor-? (TNF-?).
question
Diagnosis & Monitoring for osteoporosis involves what?
answer
TOC - DEXA scan Bone mineral density (BMD) results are reported using T and Z scores. T score = number of standard deviations (SD) above or below the mean bone mineral density for sex-matched young normal controls. Z score = compares the patient with an age- and sex-matched population. Normal bone density is defined as a T score > -1.0 SD at the spine, hip or forearm. Osteopenic = T scores -1.0 to -2.5, osteoporotic = T scores < -2.5.
question
How is osteoporosis treated?
answer
Calcium = Minimum 1200 mg Vitamin D (800-1000 IU/d) Smoking cessation Avoid alcohol Weight bearing and muscle strengthening exercise Bisphosphonates Calcitonin (peptide hormone) Estrogen Used to be the mainstay of therapy for prevention and treatment of postmenopausal osteoporosis. However, health risks > benefits. Parathyroid hormone
question
What is sexual dysfunction?
answer
hypo-estrogenic state leads to atrophy of the internal genitalia. Symptoms of vaginal atrophy include: Dyspareunia (painful intercourse) suboptimal sexual functioning Diminished genital sensation (and therefore decreased sensory output in the arousal phase) Lessened glandular secretions, Decreased vaginal expansion
question
What is the treatment for sexual dysfunction?
answer
Local Estrogen cream (preferred vs. systemic) Testosterone - modest improvement in libido
question
What is Postmenopausal Period (stage +1)
answer
The first 6 years following the final menstrual period (FMP) 12 months following the FMP marks the end of the menopausal transition FSH continues to increase
question
Every woman with menopausal symptoms deserve explanation of what she is experiencing to dispel fear, and to address her symptoms, and reassurance. Such as what?
answer
No rx required = ovarian function is maintaining some uterine bleeding. -If having hot flushes with ovarian function low dose OCP's can be rx'd.
question
Estrogen HRT Therapy - Indications
answer
Some findings suggest estrogens prevent many common conditions of aging, such as: Alzheimer's disease and Congestive Heart Disease. Estrogen therapy has only been proven to be effective in: The prevention of osteoporosis, Treatment of vasomotor symptoms Treatment of vulvovaginal atrophy
question
Hormone Replacement Therapy complications?
answer
Endometrial cancer Breast Cancer Thromboembolic Disease Stroke Uterine Bleeding Gallbladder Disease Lipid Metabolism
question
Hormone Replacement Therapy contraindications?
answer
Undiagnosed abnormal Vaginal bleeding Known, suspected, or hx of breast cancer Active DVT, PE or hx of these conditions Arterial thromboembolic disease (MI, Stroke) Liver dysfunction/dz
question
What are guidlines for managing HRT?
answer
Osteoporosis Hot flashes Atrophic Vaginitis 4. Progestogen-Estrogen Therapy
question
Before discussing the management of estrogen replacement, it is necessary to review the complications of and contraindications to this type of therapy. Complications and Contraindications play an important role in the ultimate decision regarding treatment for all patients. Complications included in Endometrial cancer?
answer
Most highly charged issue with HRT Estrogen stimulation of endometrium unopposed by progesterone, causes ENDOMETRIAL PROLIFERATION, HYPERPLASIA, and NEOPLASIA. 2- to 8-fold risk ratios ***it is recommended that a progestogen be added to ET to reduce the risk of endometrial hyperplasia or carcinoma *** THERE IS INCREASING RISK OF PROGESTOGENS RELATED TO BREAST CANCER IN HRT PTS.
question
HRT Complications of breast cancer?
answer
Risk Factors Early age menarch Older age at menopause Protective Factor Early oophorectomy Many studies have been published since 1974 re HRT and breast cancer. Results vary. The recent prospective, randomized WHI trial estrogen/progestin arm - ? risk of invasive breast cancer estrogen-alone arm - breast cancer risk was not increased Long-term use (4-10 years) = ?risk Addition of Progesetin may actually ? risk Risk does not vary dependent on family hx of breast cancer or benign breast dz.
question
HRT Complications of thrombotic disease and stroke?
answer
Affects synthesis of coagulation factors via liver Use of Transdermal estrogens is probably associated with ?risk ?risk noted in both EPT and estrogen-alone arm
question
HRT complications and Contraindications for uterine bleeding?
answer
Occurs in the majority of patients given estrogen/progestin combos ? bleeding Can occur during treatment-free interval (scheduled bleeding) Can occur during medication administration (Unscheduled bleeding). Hyperplastic endometrium is a serious side effect. In women using a combined continuous regimen of estrogen and progestin, bleeding is common in the first several months, does not indicate serious pathology. If the bleeding is heavy or prolonged, = biopsy **If endometrial hyperplasia is present, EPC medications d/c'd, or ? progestin dose, or add progestin daily. a repeat biopsy should be performed to check for continuing endometrial hyperplasia
question
In women taking estrogen only, the incidence of endometrial hyperplasia can be as high as 25% after only 12 months of therapy. What is seen and what is done in this case?
answer
Hyperplasia occurs in women who do not experience vaginal bleeding, bleed only during the medication-free interval, or bleed during drug administration. *** pretreatment biopsy and yearly endometrial biopsies are necessary in all women receiving estrogens alone to assess for the presence of hyperplasia***
question
HRT complications for gallbladder disease?
answer
Estrogens cause increased amounts of cholesterol to collect in bile. Leading to increased synthesis of cholesterol. Bile normally has a 75-90% cholesterol, small increases = stone formation. ¾ gallstones are composed predominantly of cholesterol.
question
HRT complications for Lipid metabolism?
answer
Estrogen replacement also has an impact on circulating lipids. many of these effects are favorable. ? HDL ? LDL
question
Contraindications for HRT inlude
answer
1. UNDIAGNOSED ABNORMAL VAGINAL BLEEDING 2. KNOWN, SUSPECTED OR HX OF BREAST CANCER 3. ACTIVE DVT, PE OR HX OF THESE CONDITIONS 4. ARTERIAL THROMBOEMBOLIC DISEASE (MI, STROKE) 5. LIVER DYSFUNCTION AND DISEASE 6. ENDOMETRIAL CANCER
question
Estrogen, a steroid hormone, is derived from the androgenic precursors androstenedione and testosterone by means of aromatization. In order of potency these estrogens go like?
answer
1. 17 (beta)-estradiol (E2), 2. estrone (E1), 3. estriol (E3). The synthesis and actions of these estrogens are complex. In brief, these forms of estrogen can be summarized as follows: Estradiol - Primarily produced by theca and granulosa cells of the ovary; it is the predominant form of estrogen found in premenopausal women Estrone - Formed from estradiol in a reversible reaction; this is the predominant form of circulating estrogen after menopause Estriol - The estrogen the placenta secretes during pregnancy; in addition, it is the peripheral metabolite of estradiol and estrone; it is not secreted by the ovary
question
ONLY GENERAL GUIDELINES CAN BE OFFERED b/c risks and benefits must be evaluated for each patient. Indications for HRT use is what?
answer
Hot Flushes Atrophic Vaginitis MODERATE TO SEVERE hot flashes and Atrophic Vaginitis: - therapy may be used for the shortest duration possible; minimal or no symptoms may not require hormones. Prevention of Osteoporosis ET for osteoporosis prevention is generally reserved for those women who are otherwise using estrogen for menopausal symptoms and/or who cannot tolerate other antiresorptive therapies.
question
Hot Flushes guidelines for HRT are what?
answer
Standard dosage of Oral estrogen, such as 0.3-0.625 mg of conjugated equine estrogens 0.5 mg oral estradiol 0.025 mg transdermal estradiol, Higher doses may be necessary to relieve hot flashes. *** Progressive reduction of dosage should be attempted as soon as feasible *** Additional formulations containing estradiol, synthetic estrogens, and estrogens plus progestins are also available
question
Atrophic guidelines for HRT are what?
answer
Vaginal preparations are preferred over systemic estrogens These preparations are available in the form of: Creams (ie, CEEs or estradiol 0.25-2 g PM for 2 weeks, followed by twice weekly), Tablets (10 ?g estradiol given nightly for 2 weeks, followed by twice weekly) Rings (estradiol releasing rings, which remain in place for 3 months at a time) *** With the tablets, rings, and lowest dose creams, endometrial proliferation is RARE.***
question
Osteoporosis guidelines for HRT are what?
answer
ET for osteoporosis prevention is generally reserved for those women who are otherwise using estrogen for menopausal symptoms and/or who cannot tolerate other antiresorptive therapies. There are several options available for use of EHT or EPT for prevention of osteoporosis ORAL OLDER HIGHER DOSING 0.625 mg of conjugated equine estrogens, LOWER DOSING ALSO PREVENTS BONE LOSS, NOT AS WELL AS HIGHER DOSES! 0.3 mg of conjugated equine estrogens, & 0.5 mg of micronized estradioL TRANSDERMAL 0.05 mg of transdermal estradiol, and 1 mg of micronized estradiol, & 0.025-mg transdermal patches low-dose(0.014 mg/d) estradiol approved for prevention of osteoporosis. *** With the tablets, rings, and lowest dose creams, endometrial proliferation is RARE.***
question
How do you maintain the most bone density in before menopause?
answer
"Early commencement of prophylaxis after cessation of ovarian function will maintain the highest bone density. Initiation of HT well after the menopause will stop bone loss, but will not return bone density to that which was present at the time of the menopause."
question
A serious outcome of ERT is occurrence of endometrial hyperplasia or cancer. How is this combated?
answer
Progestogens oppose the action of estrogen on the endometrium. Significant reduction of the occurrence of endometrial cancer with estrogen plus progestogen compared with estrogen alone. high-dose estrogens (1.25 mg or greater of CEEs) = 32% hyperplasia, low doses estrogens (0.625 mg or less) stimulated 16% hyperplasias estrogen plus progestins, the occurrence of hyperplasia was 6% , In comparing length, progestogen therapy reduced the occurrence of hyperplasia to: 7 days = 4%, 10 days = 2%, 12 days eliminated hyperplasia.
question
How is Progestin-Estrogen Therapy administered?
answer
administer a progestogen 12-14 days each month If this is accomplished, 80-90% of women will experience some vaginal bleeding Administer a lower dosage, 2.5 mg, continuously. Many newer formulations of hormone therapy contain both estrogen and progestin The combined, continuous administration of estrogen plus progestogen is the most common mode of administration today.
question
This regimen promotes endometrial atrophy results in what?
answer
amenorrhea in 70-90% if used for more than 1 year. The remaining 30-10% will bleed occasionally, bleeding usually being less frequent, shorter, and lighter than with sequential therapy. Other SE's" fatigue, depression, breast tenderness, bloating, cramps, HA's, Inc risk of breast cancer!
question
Short term vs. Long term Risk of HRT includes?
answer
Women who have been receiving long-term estrogen-progestin hormone replacement therapy, even in the absence of complications, should be encouraged to stop, especially if they do not have menopausal symptoms.
question
HRT RECAP Benefits
answer
Reduce sexual dysfunction Improve sleep problems Improve hot flushes and night sweats Reduce aching joints/muscles Improve vaginal dryness Prevents bone loss and osteoporotic fractures HRT may reduce colorectal cancer risk other potential benefits possible reduction in total mortality in women < 60 years old may reduce risk of diabetes may reduce risk of osteoarthritis may reduce risk of cataracts
question
HRT RECAP risks
answer
Increase risk of ovarian cancer Increase risk of endometrial cancer Increase risk of breast cancer Increased risk of gallstones Vasomotor sx may worsen after stopping estrogen therapy mortality due to lung cancer long-term hormone replacement therapy increases risk of Cardiovascular disease: coronary events, venous thromboembolism, stroke,
question
United States Preventive Services Task Force (USPSTF) recommendations for HRT?
answer
Routine use of combined estrogen and progestin not recommended for prevention of chronic conditions in postmenopausal women (USPSTF Grade D) Routine use of estrogen alone not recommended for prevention of chronic conditions in postmenopausal women who have had a hysterectomy (USPSTF Grade D) Estrogens with or without progestins should be prescribed at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman
question
Synthetic ESTROGEN
answer
Most widely prescribed for years — estrogens like Premarin and progestins like Provera, as well as low-dose OCP's Synthetics refer to man-made hormones — hormones that are made from chemical sources that approximate the hormones the human body makes. Also refers to Premarin, although made from a natural source (horse urine), aren't the same as endogenous estrogens Many synthetic estrogens are stronger than human estrogen Supporters of bio-identical hormones argue that this may cause your liver to work harder than with the bio-identical estrogens. This claim has not been proven by the currently available science. *** Most widely studied form of estrogen
question
Bio-identical Hormone Therapy
answer
These hormones do not approximate your hormones; they have the same exact chemical structure as the hormones made by ovaries. Supporters argue that, d/t same structure the body should be better equipped to work with them. The argument, typically, is that we can more easily metabolize them and break them down so our livers and kidneys can excrete them once they've done their work. Cenestin is a conjugated estrogen. It's natural in that it's made from plant sources, but it's not bio-identical to human estrogens. It's the plant-based copy of Premarin. Natural estrogens include: Estrace, Estratab, Ogen, the estradiol patches such as Climara, Alora, Vivelle,Estraderm, Esclim, FemPatch, etc, Tri-Est
question
Many women express a preference for bioidentical hormones (BHT), with the expectation that they are safer, with comparable efficacy Varying formulations which are not used consistently amongst patients or practitioners Bioidentical hormones are plant-derived compounds that have the same chemical and molecular structure as those of hormones produced by the human body. Pharmacists can custom prepare and package (compound) bioidentical hormones according to a physician's specifications. After results of the WHI were reported in 2002, interest in bioidentical hormones does what
answer
increased b/c they have been promoted as a safer alternative to traditional hormone therapy, with the ability to tailor dosages of various estrogens. Although the existing studies on bioidentical hormones have not shown an increase in breast cancer, these studies have been too short in duration or methodologically flawed to show changes. These findings have unfortunately been interpreted as proof of safety rather than as inconclusive. This may be misleading to the public.
question
The primary disadvantages of bioidentical hormone therapy
answer
Preparations have not undergone rigorous clinical testing for safety or efficacy They are not regulated by the FDA. Safety questions, Quality assurance The purity, potency, and quality of the products is not standard labeling does not need to include the warning the FDA now requires for traditional hormone therapy.
question
The FDA has declared that claims of compounding pharmacies; stating ?
answer
That BHT drugs avoid the risks of FDA-approved treatments and these drugs reduce the risk of serious illness such as heart disease, stroke, or breast cancer are not supported by credible scientific evidence. They further state that safety and efficacy of estriol in these formulations has not been proven.



