OB-GYN (Oncology) – Flashcards
Unlock all answers in this set
Unlock answersquestion
Why has the incidence of Cervical Cancer decreased 4 fold in 40 years?
answer
1) Pap Smear screening 2) HPV vaccine
question
There are two main types of cervical cancer and BOTH are influenced by HPV. What are they?
answer
1) *Squamous Cell (80%) 2) Adenocarcinoma
question
Which types of HPV are responsible for 70% of al cervicle cancer
answer
HPV 16, 18
question
What does the progression of cervical cancer require?
answer
Persistent HPV infection for many years
question
Next to breast cancer, cervical cancer is the second most common cancer in females worldwide. Is this the case in the U.S.?
answer
NO
question
What are the risk factors for cervical cancer?
answer
**(somewhat similar to RF for persistent HPV infection) 1) STDs - HPV—types 16, 18 associated with highest risk - HIV 2) Low socioeconomic status 3) > 1 sexual partner 4) Immunosuppression 5) Tobacco 6) Hx of previous cervical disease 7) DES exposure
question
What is the most common presenting symptom in cervical cancer?
answer
Post coital bleeding and AUB, including post menopausal
question
What are late findings of cervical cancer?
answer
1) Persistent vaginal discharge 2) Pelvic pain/leg swelling 3) Urinary symptoms
question
What should be done if a woman has visible lesions?
answer
Refer for colposcopy
question
Can a rectal exam for staging local invasion of cervical cancer?
answer
Yes
question
What should be done to stage local and distant disease?
answer
Imaging
question
What is stage I cervical cancer?
answer
Stage I disease confined to cervix A—microscopic B—clinical disease
question
What is the MOST common gynegological malignancy in the US?
answer
Endometrial cancer
question
Are there amy useful screening tests for endometrial cancer?
answer
No
question
***What do 90% of patients with endometrial cancer experience?
answer
Abnornormal uterine bleeding (evaluate all women >35 years old)
question
What are the risk factors for endometrial cancer?
answer
1) ***Unopposed estrogen*** e.g. anovulatory cycles (compare with ovarian cancer) 2) Obesity (increased peripheral conversion of androgens) 3) Affluent (compare with cervical cancer) 4) White 5) Low parity 6) Post-menopausal (particularly if on estrogen replacement w/o progestin) 7) Type 2 DM 8) Women with Lynch syndrome (familial nonpolyposis colorectal cancer)
question
Is the prognosis of cervical cancer good?
answer
Absolutely. 96% 5-yr survival rate if confined to uterus (68% of patients) Take out the uterus and you are good to go
question
What is the work-up for endometrial cancer?
answer
1) Endometrial biopsy (EMB) - Positive for cancer - Negative (90% diagnostic accuracy) 2) Transvaginal Ultrasound
question
Is transvaginal ultrasound sufficient in the evaluation of premenopausal women?
answer
NO. Because there is no standardization of acceptable stripe thickness. For premenopausal women we go straight to biopsy
question
What is the initial diagnostic test in postmenopausal women?
answer
Transvaginal ultrasound 4 mm endometrial stripe requires endometrial biopsy +/- D&C
question
Where is the endometrial stripe measured from?

answer
It is Measured from echogenic interface between the endometrium/myometrium both anterior and posterior
question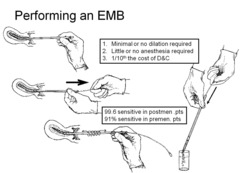
Can I do an endometrial biopsy?
answer
Yes its pretty easy
question
What are the 4 possible endometrial results?
answer
1) Benign, proliferative, secretory, atrophic 2) Hyperplasia without atypia - Progesterone treatment - Endometrial biopsy every 3-6 months 3) Hyperplasia with atypia - Hysterectomy - If refused, progesterone then every 3 month endometrial biopsy is recommended 4) Cancer Staging and treatment
question
What is the 2nd most common gynecologic malignancy?
answer
Ovarian Cancer - Risk is 1 in 70 in a lifetime - Risk increases from age 40 to age 60 - Median age at dx is 61
question
What is the most common cause of gynecological cancer deaths?
answer
Ovarian Cancer (5-yr survival ~40%)
question
What are the risk factors for ovarian cancer?
answer
1) Low/no parity 2) Breast/colon cancer 3) Tobacco
question
What things are protective for ovarian cancer?
answer
1) Multiparity 2) Oral contraceptive pill (OCP) use 3) History of breastfeeding So....Take birth control pills, stop and have a baby, breastfeed, go back on pills, have 3 more kids and breastfeed them all, get your tubes tied and don't smoke
question
What is the screening test for breast cancer?
answer
There isnt one. A bimanual examination during the annual exam is the most appropriate examination for early detection of ovarian cancer.
question
Is CA-125 a screening test for ovarain cancer?
answer
No. Except possibly in the familial syndromes (e.g. BRCA1 mutation on chromosome 17) exhibiting a genetic component consistent with the disease, but may be used for post-treatment surveillance of ovarian cancer.
question
What must be done with a woman with Familial Ovarian Cancer Syndrome (BRCA-1, BRCA-2)?
answer
1) Frequent pelvic exams (Annual) 2) Annual Trans-vaginal ultrasound (TVUS) 3) Serum markers (CA-125) every 6-12 months **Begining at age 30-55
question
What is the most common physical exam finding in ovarian cancer?
answer
Pelvic mass/ascites
question
What are the late findings assoicated with ovarian cancer?
answer
1) Anorexia 2) Early satiety 3) Weight loss 4) Constipation 5) Frequent UTIs in menopausal patient
question
What will a transvaginal ultrasound show in a patient with ovarian cancer?
answer
Complex cystic mass
question
What is most useful in following ovarian cancer treatment?
answer
Serum marker CA-125
question
What else may Serum marker CA-125 be useful in?
answer
Postmenopausal patients in combination with clinical evaluation/US
question
What is a sustained elevation of Serum Marker CA-125 mean?
answer
1) 80% in non-mucinous epithelial ovarian tumors 3) Most beneficial in postmenopausal pelvic mass, >65u/ml is 75% predictive of malignancy
question
What does variable elevation of Serum Marker CA-125 mean?
answer
1) Endometriosis, leiomyomata, PID 2) Hepatitis, cirrhosis 3) CHF 4) Other malignancies
question
Vulvular cancer is usually caused by Squamous Cell Carcinoma. What are the two hypotheses?
answer
1) Young/HPV/vulvar intraepithelial neoplasia (VIN) 2) Older/chronic inflammation/lichen sclerosus *Caucasian women over 65
question
What is the second most common type of vulvar cancer?
answer
Malignant Melanoma *Bottom line (Any suspicious lesion or pigmented lesion requires biopsy)
question
What is Gestational Trophoblastic Disease (GTD) unique?
answer
Because maternal lesions arise from fetal tissue (trophoblastic epithelium of placenta)
question
What are the 3 types of Gestational Trophoblastic Disease (GTD)?
answer
1) Benign hydatidiform mole (noninvasive) 2) Invasive mole (in the middle) 3) Choriocarcinoma---- frankly malignant * All of these are associated with functional trophoblastic material * All are associated with high levels of Beta HCG
question
Is the majority of Gestational Trophoblastic Disease (GTD) bengign or malignant?
answer
Benign
question
What are the ris factors for Gestational Trophoblastic Disease (GTD)?
answer
1) age > 35 2) age < 20 3) Hx of trophoblastic tissue
question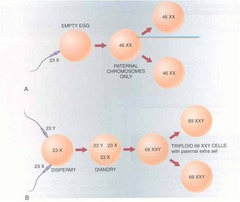
What are the 2 varietes of Hydatidiform Moles (Mole means false conception in latin)
answer
1) Complete Hydatidiform mole 2) Partial Hydatidiform mole
question
What is complete Hydatidiform mole?
answer
1) No identifiable fetal features 2) Generalized hydatidiform swelling of villi 3) Diffuse trophoblastic hyperplasia 4) Diploid paternal: 90% 46XX/10% 46XY 5) hCG typically >100K, (nl preg peaks at <100K) In the complete mole, it appears that the ovum is inactivated while the sperm (or two) duplicates.
question
What is partial Hydatidiform mole?
answer
LESS SEVERE 1) Fetal features identifiable (triploidy stigmata) 2) Focal swelling chorionic villi 3) Focal trophoblastic hyperplasia 4) Triploid: 2/3 paternal 5) May detect Fetal heart tones In the event of a partial mole with a complete fetus, the fetus usually manifests stigmata of triploidy e.g. growth retardation and multiple congenital malformations
question
What is the clinical presentation of Hydatidiform moles?
answer
1) Vaginal bleeding in this population portends anemia in 50% 2) Increase in uterine size disproportionate to gestational age is classic, despite 50% occurrence. . It is due to expanded chorionic tissue, retained blood, and exuberant trophoblast, and is thus closely associated with increased hCG levels, which in turn lead to hyperemesis and hyperthyroidism.
question
How is a complete mole diagnosed?

answer
1) Ultrasound (US) "snowstorm" PATHOGNOMONIC (because all of the fluid filled grape like villi are bouning sound waves) 2) CBC to exclude anemia
question
How is a partial mole diagnosed?
answer
1) Detected after tissue examination of a spontaneous abortion (SAB) 2) Ultrasound - Focal placental cysts/gestational sac +/- fetus
question
***What is the clinical presentation of a complete mole?
answer
1) Vaginal Bleeding in the 1st Trimester 2) Hyperemsis Gravidara 3) Increased risk of pre-eclampsia 4) Expulsion of Grape like Vessicles 5) Uterus is larger than expected for dates 6) Hyperthyrodism
question
***What is the clinical presentation of a partial mole?
answer
1) Same as complete mole but less severe 2) Uterus is smaller than expected for dates
question
Describe an invasive mole
answer
1) Occurs in 5-10% of molar pregnancies 2) Complete mole extends into myometrium
question
How is the diagnosis of an invasive mole made?
answer
Persistent HCG levels following evacuation of molar pregnancy
question
Do invasive moles metastasize?
answer
No
question
What is required to treat an invasive mole?
answer
Hysterectomy
question
What population of patients are at a higher risk for Choriocarcinoma?
answer
1) 50% have a preceding molar pregnancy 2) 50% have preceding SAB, induced AB, ectopic or normal pregnancy *Persistent HCG levels after any of these is Choriocarcinoma until proven otherwise
question
Describe Choriocarcinoma
answer
1) Highly anaplastic 2) No chorionic villi 3) Necrosis and hemorrhage 4) Rapidly invasive 5) Hematogenous metastasis - Common: Vagina and Lungs - Other: CNS, GI/liver, kidney
question
What is the treatment for Choriocarcinoma?
answer
Chemotherapy
question
How long should B-HCG levels be followed for any molar pregnancy (particularly Choriocarcinoma)?
answer
- Followed monthly for 1 year - Up to 5 years if metastases
question
How long is contraception recommended after a molar pregnancy?
answer
6-12 months
question
Is there an increased risk of a molar pregnancy if you had it once?
answer
Yes. - Increased risk of subsequent GTN, esp in women >40 - No increased risk of obstetric complications once pregnant



