Nursing Management: Respiratory disorders and diseases – Flashcards
Unlock all answers in this set
Unlock answersquestion
Acute Respiratory Distress Syndrome
answer
is a severe form of acute lung injury characterized by sudden and progressive noncardiogenic pulmonary edema, increasing bilateral infiltrates, hypoxemia refractory to supplemental oxygen, and reduced lung compliance.
question
Pathophysiology of ARDS
answer
- occurs as a result of an inflammatory trigger that initiates the release of cellular and chemical mediators, which injure the alveolar capillary membrane. - Protein-rich fluid leaks into the alveolar and interstitial spaces, impairing ventilation and surfactant. - Without surfactant, the lungs become extremely stiff, the alveoli collapse, and severe hypoxemia develops. - Blood returning to the lung for oxygen is shunted back to the heart markedly reduced in oxygen.
question
Risk factors for ARDS
answer
• Direct injury to the lungs such as smoke inhalation, pulmonary contusion • Indirect insult to the lungs such as septic shock or massive fluid resuscitation
question
Dx of ARDS
answer
• History of systemic or pulmonary risk factors • Acute onset of respiratory distress • Bilateral pulmonary infiltrates, clinical absence of left-sided heart failure • Ratio of PaO2 to fraction of inspired oxygen (Fio2) of less than 200 mm Hg (severe refractory hypoxemia)
question
Medical Management of ARDS
answer
• Identify and treat the underlying condition - provide aggressive, supportive care using intubation and mechanical ventilation with positive end-expiratory pressure (PEEP). • Monitor ABG values, pulse oximetry, and pulmonary artery pressures. • Treat hypovolemia carefully, avoiding overload; inotropics or vasopressors may be required.
question
Pharmacologic Therapy for ARDS
answer
- there is not specific medication for ARDS • IV sedation with lorazepam, midazolam, dexmedetomidine, propofol, or short-acting barbiturates and analgesics combat anxiety and agitation from hypoxemia and intubation. • Neuromuscular blockers such as pancuronium, vecuronium, atracurium, and rocuronium for continued inadequate oxygenation.
question
Nutritional Therapy for ARDS
answer
• Provide nutritional support (15 to 20 kcal/ kg daily). • Enteral feeding is considered first; however, parenteral nutrition may be required.
question
Nursing Management: ARDS
answer
• Closely monitor the patient in the intensive care unit. • Provide respiratory modalities including oxygen, nebulizer therapy, chest physiotherapy, endotracheal intubation or tracheostomy, mechanical ventilation, suctioning, bronchoscopy. • Turn the patient frequently; prone position may be attempted. • Reduce anxiety by explaining all procedures and providing care in a calm, reassuring manner.
question
Ventilator Considerations for ARDS
answer
• Identify any problems with ventilation that may cause anxiety: hypoxemia, sensations caused by PEEP, tube blockage, pneumothorax, pain, level of dyspnea, or ventilator malfunction. • Closely monitor patients on paralytic agents: Ensure the patient is not disconnected from ventilator and that ventilator and patient alarms are on at all times, provide eye care, explain neuromuscular blockade to the family.
question
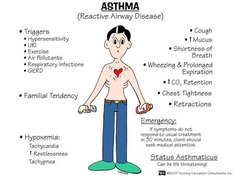
Asthma
answer
is a complex disease of the airways characterized by recurring and variable symptoms, airflow obstruction, and bronchial hyperresponsiveness.
question
Pathophysiology of Asthma
answer
- is reversible and diffuse airway inflammation - acute inflammation leads to airflow limitation and changes in the airways - bronchoconstriction occurs - airway edema develops and becomes more progressive as asthma severity increases
question
Risk Factors: Asthma
answer
• Antigens: Pollens, molds, dust mites, animal dander, food • Occupational exposure: Baking products, toluene • Environmental factors: Tobacco smoke, air pollution, diet • Viruses, sinus infections, postnasal drip • Cold dry air • Exercise, hard laughing, crying, yelling, emotions, and stress
question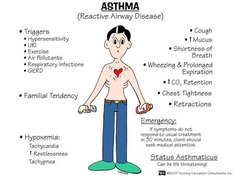
S/S: Asthma
answer
- frequently occur at night or early morning and may awaken patients - may occur suddenly or over days
question
Physical Exam: Asthma
answer
- generalized wheezing initially heard during expiration. - b/w asthma episodes exam findings may be normal
question
Dx: Asthma
answer
- ABGs - Pulmonary function tests - Family, environment, and occupational history is taken to assess for allergic causes • Methacholine challenge, exercise challenge, or the administration of cold air to induce symptoms • Sputum culture and blood test • Chest X-ray
question
Ongoing Assessment and Monitoring: Asthma
answer
- perform physical assessment - determine the patient's degree of risk for exacerbation - Assess ability to participate in normal activities, the frequency of exacerbations, and monitoring of pulmonary function by periodic spirometry or home peak flow monitoring. - Perform a history of the patient's symptoms, self-care measures used, sequence of the current asthma episode, and response to medication and treatments used, including complementary and alternative therapy. - Administer medications as prescribed and monitor the patient's response. - Educate and prepare patient for discharge with focus on treatment, medication administration, management of asthma triggers, prevention and treatment of future exacerbations, and follow-up.
question
Patient Education: Asthma
answer
- Assist patients to identify and manage asthma triggers, monitor for early warning signs of acute episodes, and maintain proper medication management. - Collaborate with patient to identify comorbid conditions, side effects, financial issues, living conditions, different beliefs about asthma, and other factors may influence the patient's adherence to the asthma management plan.
question
Pharmacologic Therapy: Asthma
answer
- Control of persistent asthma is accomplished primarily with regular use of anti-inflammatory medications; inhaled cortico-steroids are treatment of choice. Patient should use a spacer and rinse the mouth after use to prevent thrush. • Long-acting beta2-adrenergic agonists (salbutamol and formoterol) with inhaled corticosteroid • Leukotriene modifiers inhibitors/ antileukotriene: Montelukast (Singulair), zafirlukast (Accolate), and zileuton (Zyflo) • Cromolyn sodium and nedocromil stabilize mast cells; used for persistent asthma, exercise-induced asthma, and those not tolerating inhaled corticosteroids • Omalizumab (anti-IgE) is used as an additional therapy for patients with severe, persistent asthma who have sensitivity to specific allergens. • Occasionally used medications include methylxanthines, anticholinergic ipratropium. • Oral corticosteroids regain quick control of asthma during exacerbations - long-term corticosteroid use may be needed with uncontrolled, severe, persistent asthma.
question
Quick relief medications are used for the....
answer
immediate treatment of asthma symptoms
question
Long-acting medications are used to achieve and ...
answer
maintain control of persistent asthma
question
Environmental Control and Management of Triggers of Asthma
answer
• Skin testing is useful in some patients to identify specific allergens and in patients who may be candidates for immunotherapy. • Help patients develop a trigger management plan.
question
What are the Comorbid Conditions of Asthma
answer
allergic bronchopulmonary aspergillosis (fungal infection) gastroesophageal reflux disease (GERD) obesity obstructive sleep apnea rhinitis sinusitis stress depression
question
High-risk situations for patient at high risk for asthma death and need to seek medical care early during an exacerbation are ...
answer
- history of previous severe exacerbation requiring intensive care and/ or intubation - two or more hospitalizations or more than three emergency room visits in the past year - using more than two canisters of a short acting beta agonist (SABA) per month - difficulty perceiving worsening asthma - low socioeconomic status/ inner-city residence - illicit drug use - severe psychiatric illness - major comorbid conditions.
question
What are the complications of having asthma?
answer
- status asthmaticus - respiratory failure
question
Status Asthmaticus
answer
Is a severe asthma episode that is refractory to initial therapy. It is a medical emergency.
question
Risk Factors for Status Asthmaticus
answer
- viral or respiratory infection - exposure to trigger or exercise in cold environment - nebulizer abuse - nonadherence to controller medications
question
S/S of Status Asthmaticus
answer
• Similar to those in asthma; however, increased in severity, without recovery with usual treatments • Wheezing, tachycardia, diaphoresis, and a widened pulse may occur along with severe hypoxemia. • Progresses to minimal air movement, and the "quiet chest" reflects impending respiratory failure.
question
Why is a quiet chest worrisome in a patient with status asthmaticus?
answer
the nurse considers that airflow can be so limited that wheezing cannot be detected.
question
Medical and Nursing Management of status asthmaticus
answer
- actively assess patient's airway and response to treatment - administer fluids, systemic corticosteroids, bronchodilators, and energy conservation. • Intubation and mechanical ventilation may be needed to keep saturation over 95%. • Administer heliox, magnesium sulfate, and leukotriene modifiers. • Ensure patient's room is quiet and free of respiratory irritants (eg, flowers, perfumes, or odors of cleaning agents) - nonallergenic pillows should be used.
question
Chronic Bronchitis
answer
A type of chronic obstructive pulmonary disease (COPD), results in airflow limitation. It is defined as the presence of cough and sputum production for at least 3 months in each of 2 consecutive years.
question
Pathophysiology of Chronic Bronchitis
answer
Chronic mucus hypersecretion, thickening of the epithelium, smooth muscle hypertrophy, and airway inflammation are implicated in remodeling of the airways and decreasing the size of the airway lumen.
question
Risk Factors for Chronic Bronchitis
answer
• Cigarette smoking, tobacco smoke, second-hand smoke, fetal exposure to smoke • Occupational dust and chemicals • Indoor and outdoor air pollution • Infection (history of severe respiratory infections, history of tuberculosis in those > 40 years old) • Viral, bacterial, and mycoplasmal infections can produce acute exacerbations.
question
S/S of Chronic Bronchitis
answer
dyspnea, chronic cough, and sputum production.
question
Dx of Chronic Bronchitis
answer
• Pulmonary function tests • Arterial blood gas (ABG) - Chest X-ray - CT scan
question
Cancer of the larynx
answer
is a malignant tumor in and around the larynx (voice box).
question
Risk Factors for Laryngeal Cancer
answer
• Male • Aged 60 to 70 years • African Americans • Exposure to carcinogens: Tobacco (smoke, smokeless) and alcohol and their combined effects • Occupational or environmental exposure: Asbestos, wood dust, coal dust, steel dust, cement dust, tar products, leather, formaldehyde, and iron compounds and fumes have also been implicated. - straining the voice - chronic laryngitis - nutritional deficiencies (riboflavin) - family predisposition - weakened immune system.
question
S/S of Laryngeal Cancer
answer
• Hoarseness - harsh, raspy, low-pitched voice • Persistent cough - pain and burning in the throat when drinking hot liquids and citrus juices • Palpable lump in the neck • Later symptoms: Dysphagia, dyspnea, unilateral nasal obstruction or discharge, persistent hoarseness or ulceration, foul breath • Enlarged cervical nodes, weight loss, general debility, and pain radiating to the ear may occur with metastasis.
question
Dx of Laryngeal Cancer
answer
• Indirect laryngoscopy • Endoscopy, virtual endoscopy, optical imaging, CT, MRI, and PET scanning (to detect recurrence of tumor after treatment) • Direct laryngoscopic examination under local or general anesthesia • Biopsy of suspicious tissue
question
Medical Management of Laryngeal Cancer
answer
- Surgery - Radiation therapy - Chemotherapy
question
Surgical Management of Laryngeal Cancer
answer
- total laryngectomy - voice-sparing surgeries: vocal cord stripping, cordectomy, partial laryngectomy, supraglottic laryngectomy, hemilaryngectomy
question
Nursing Management of Laryngeal Cancer
answer
• Teach the patient undergoing complete laryngectomy that the natural voice and ability to sing, laugh, and whistle will be lost, but that special training can provide a means for communicating. • Review equipment and teach importance of coughing and deep-breathing exercises. - reduce anxiety and depression - place patient in semi-fowler's or fowler's position • Observe the patient for restlessness, labored breathing, apprehension, and increased pulse rate, • Use opioids cautiously, providing adequate analgesia for turning, coughing, and deep breathing. • Provide suctioning to remove secretions, avoiding disruption of the suture line. • Monitor pulse oximetry. • Encourage and assist the patient with early ambulation to prevent atelectasis, pneumonia, and deep vein thrombosis (DVT). • Recognize that the laryngectomy tube (shorter than a tracheostomy tube but has a larger diameter) is the patient's only airway; humidification is required if no inner cannula is present. (Care is the same as for tracheostomy tube). Reassure the patient that excess mucus will diminish over time. • Establishing an effective means of communication is the primary goal in the rehabilitation of the laryngectomy patient. • Provide a magic slate; place IV in nondominant arm for ease of writing. • Picture-word-phrase board or hand signals may be used for those who cannot write. • Give patient adequate time to communicate - NPO for several days after surgery - Swallowing study to determine when able to start oral feedings - when able to eat - diet of thickened liquids - remain with patient during initiate oral feedings - keep suction setup at bedside if needed • The nurse instructs the patient to avoid sweet foods, which increase salivation and suppress the appetite. • The patient is instructed to rinse the mouth with warm water or mouthwash after oral feedings and to brush the teeth frequently. • Changes in taste and olfactory sensation adapt, often with return of interest in eating. - Monitor weight and laboratory data to ensure that nutritional and fluid intake are adequate. - Skin turgor and vital signs are assessed for signs of decreased fluid volume. - promote positive body image and self-esteem
question
Patient Education for patient with Laryngeal Cancer
answer
• Maintaining a positive approach is important when caring for the patient and includes promotion of self-care activities. • Patient and family should begin participating in self-care activities as soon as possible. • Support the patient and the family, especially when explaining the tubes, dressings, and drains that are in place postoperatively.
question
Complication of Posop Laryngeal Cancer
answer
• Respiratory distress and hypoxia • Hemorrhage • Infection • Wound breakdown • Aspiration • Tracheostomal stenosis
question
Risk Factors for Lung Cancer
answer
• Tobacco smoke, passive smoking/ second-hand smoke • Occupational and environmental agents (vehicle emissions, pollutants, urban areas, radon gas, arsenic, asbestos, chromates, coal fumes, radiation) • Male • Genetic predisposition • Underlying diseases (chronic obstructive pulmonary disease [COPD], tuberculosis [TB]) • Family history (close relative with lung cancer) • Low intake of fruits and vegetables
question
S/S of Lung Cancer
answer
• Cough or change in a chronic cough is the most common symptom. • Cough starts as a dry, persistent cough, without sputum production. When obstruction of airways occurs, the cough may become productive due to infection. • Dyspnea occurs frequently. • Hemoptysis or blood-tinged sputum may be expectorated. • Chest or shoulder pain may indicate chest wall or pleural involvement by a tumor. • Pain is a late manifestation, and may be related to metastasis to the bone. • Recurring fever is an early symptom in response to a persistent infection distal to the tumor. • Suspect lung cancer in people with repeated unresolved upper respiratory tract infections. • Nonspecific symptoms of weakness, anorexia, and weight loss also may be present.
question
Dx: Lung Cancer
answer
• Chest X-ray, CT scans, fiberoptic bronchoscopy for brushings, washings and biopsies of suspicious areas • Transthoracic fine needle aspiration • Endoscopy with transesophageal ultrasound and biopsy • PET scan, ultrasound of liver, CT of brain, MRI, and mediastinoscopy or mediastinotomy for biopsy • Pulmonary function tests, arterial blood gas analysis, ventilation/ perfusion scans, and exercise testing
question
Surgical Management of Lung Cancer
answer
- Lobectomy - Pneumonectomy
question
Medical Management of Lung Cancer
answer
- Chemotherapy - Radiation Therapy - Surgery - Palliative therapy
question
What are the treatment-related complications involving Lung Cancer?
answer
- respiratory failure - diminished cardiopulmonary function - pulmonary fibrosis - pericarditis - myelitis - cor pulmonale - pneumonitis - pulmonary toxicity
question
Nursing Management: Lung Cancer
answer
• Instruct patient and family about side effects of the specific treatment and strategies, such as dyspnea, fatigue, nausea and vomiting, anorexia, and fatigue. • Help the patient and family cope with therapeutic measures. • Maintain patent airway through the removal of excess secretions - deep-breathing exercises, chest PT, directed cough, suctioning, and in some instances bronchoscopy are performed. • Administer bronchodilators as prescribed to promote bronchial dilation. • Provide supplemental oxygen as needed. • Encourage the patient to assume positions that promote lung expansion and to perform breathing exercises for lung expansion and relaxation. • Provide patient education about energy conservation and airway clearance. A referral to a pulmonary rehabilitation program may be helpful in managing respiratory symptoms. - providing psychological support
question
COPD
answer
is a disease characterized by airflow limitation that is not fully reversible. The airflow limitation is usually progressive and associated with an abnormal inflammatory response of the lung.
question
Pathophysiology of COPD
answer
is characterized by an increase in mucus-producing cells, and chronic lung and structural changes resulting from a continuing cycle of destruction and repair. Affected are the proximal and peripheral airways, lung parenchyma, and pulmonary vasculature.
question
Emphysema
answer
an abnormal enlargement of the air spaces. beyond the terminal bronchioles, with destruction of the walls of the alveoli. The alveolar and interstitial attachments are reduced, predisposing them to collapse during exhalation. External airway compression and obstruction is caused by hyperinflation and air trapping. The panacinar or panlobular form causes uniform destruction of acinus, where alveoli are located (hereditary form is related to deficiency of alpha1-antitrypsin). A centrilobular form is related to smoking; alveolar ducts and bronchioles in the center of lobules of the upper lobes are primarily affected.
question
Risk Factors for COPD
answer
• Cigarette smoking • Environmental tobacco smoke (second-hand smoke, fetal exposure due to smoking during pregnancy) • Occupational dust and chemicals (organic dusts, inorganic dusts, chemical agents, fumes) • Indoor and outdoor air pollution (cooking or heating in poorly ventilated areas) • History of severe respiratory infections, history of tuberculosis in those over 40 years old
question
S/S of COPD
answer
- dyspnea, chronic cough and sputum production; begins with dyspnea on exertion and worsens over time. In severe COPD, dyspnea may occur at rest. • Chronic cough and sputum production often precede the development of airflow limitation by many years. In early-stage disease, an early morning productive cough of white to clear sputum may be present. During exacerbations, increased sputum quantity and viscosity may occur, with changes in sputum color. • Hyperinflation causes increased anterior to posterior diameter of the chest, called "barrel chest." • Bilateral intercostal retractions at the posterior axillary line, horizontal fixation of the ribs in the inspiratory position, and hyperresonance to percussion (particularly in thin individuals) develops. • Diminished breath sounds with prolonged exhalation (bronchovesicular breath sounds) and adventitious sounds (coarse crackles, rhonchi, and wheezes) are often heard when the patient has increased secretions, bronchial hyperreactivity, or an exacerbation.
question
Dx: COPD
answer
- Pulmonary Function test - bronchodilator reversibility teseting - ABG - Chest X-ray - CT - Screening for alpha1-antitrypsin deficiency
question
Medical Management: COPD
answer
- smoking cessation - pharmacotherapy - antidepressants - varenicline • Bronchodilators, corticosteroids, or anticholinergics via metered dose inhaler or nebulizer may be prescribed. • Influenza and pneumococcal vaccinations reduce incidence of pneumonia, hospitalizations for cardiac conditions, and deaths. A vaccine to protect against Haemophilus influenzae, a common cause of COPD exacerbations, is currently in development. - antibiotics for acute infections - cough suppressants - oxygen therapy - bullectomy - lung volume reduction surgery - lung transplantation - pulmonary rehabilitation
question
What is pulmonary rehabilitation?
answer
• The primary goals of rehabilitation are to reduce symptoms, improve quality of life, and increase participation in everyday activities using a multidisciplinary approach. • Breathing exercises, learning to pace activities, physical reconditioning and endurance, energy conservation, skills training, and psychological support are included. • Nutritional counseling and medication education are other important components of rehabilitation.
question
Preventing and Managing Exacerbations and Complications
answer
• Exacerbations are characterized by a change in the patient's baseline dyspnea, cough, and/ or sputum production, which warrants a change in management. • Exacerbations are associated with worsening prognosis and an accelerated decline in pulmonary function. • Signs and symptoms may include increased dyspnea, increased sputum production and purulence, respiratory failure, changes in mental status, or worsening blood gas abnormalities. • The primary causes of acute exacerbations include infection (bacterial and viral), heart failure, and response to pollutants and allergens. • Prevention of exacerbations is associated with preservation of pulmonary function and a decrease in hospitalizations. Some pharmacological agents, such as inhaled long-acting beta adrenergics (LABAs) combined with steroids (Advair, Symbicort) and the anticholinergic agent Spiriva, have been associated with a prolonged time between exacerbations. • Bronchodilators, inhaled or systemic corticosteroids, antibiotics, oxygen therapy, and intensive respiratory interventions may be used. • Early treatment with antibiotics in patients needing hospitalization for an acute exacerbation may result in improved outcomes. • Indications for hospitalization for acute exacerbation include severe dyspnea that does not respond adequately to initial therapy, confusion or lethargy, respiratory muscle fatigue, paradoxical chest wall movement, peripheral edema, worsening or new onset of central cyanosis, persistent or worsening hypoxemia, and the need for noninvasive or invasive assisted mechanical ventilation. • Ventilatory support may be required until the underlying cause, such as infection, can be treated. • Other complications of COPD include pneumonia, atelectasis, pneumothorax, and pulmonary arterial hypertension. • Suspect pulmonary hypertension in patients complaining of dyspnea and fatigue disproportionate to pulmonary function abnormalities; enlargement of the central pulmonary arteries on chest X-ray, echocardiography suggestive of right ventricular enlargement, and elevated plasma B-type natriuretic peptide (BNP) may be present. Anticipate stabilization of the underlying lung disease, with administration of long-term supplemental oxygen and diuretics.
question
Nursing Management: COPD
answer
• Obtain information about shortness of breath (dyspnea), cough, and sputum production; change in sputum color, quantity, or thickness, or increased fatigue and a decreased ability to perform one's usual activities is noted. • To assess progress of the disease, use a numerical scale based on 0 to 10 (with 0 being no shortness of breath and 10 being the worst) when quantifying dyspnea. • Assess for the presence of other medical problems , allergies, history of smoking in pack years, current smoking, a history of past exacerbations and pulmonary hospitalizations including a history of intubations, a description of how the patient spends a usual day, sleep quality and amount, problems with mood (anxiety and/ or depression), and what self-care measures the patient is currently using. • Observe breathing pattern and body position; accessory muscle use, shoulder elevation, use of the tripod position (leaning forward with the arms braced on the knees), and increased respiratory rate are indicative of respiratory distress • Assess for quality (good aeration or diminished) of breath sounds, the presence of adventitious sounds (crackles or wheezes), and whether the adventitious sounds clear with cough. • Review laboratory data: Pulmonary function tests, tests of oxygenation, and radiological studies. - Promoting Smoking Cessation • Assess underlying causes and manage dyspnea with bronchodilators, assisting with activities of daily living, providing oxygen therapy for hypoxemia, and teaching strategies for relieving increased shortness of breath and for limiting future episodes. • Assist patient with breathing retraining; pursed-lip breathing helps slow exhalation and is thought to prevent the collapse of the small airways, decreasing hyperinflation. It may promote relaxation and allow patients to gain control of their breathing and reduce feelings of panic. A simple explanation to patients is that pursed-lip breathing makes "more room to breathe." • Suggest the use of a small hand-held fan directing flow onto the cheek to reduce the sensation of dyspnea. • Teach relaxation techniques, such as progressive muscle • Teach patients how to pace activities with their breathing and plan for dyspnea-producing activities. For climbing stairs, climb more slowly and only during exhalation; use a pause-breathe in, exhale and climb one to two steps. • When dyspnea is not adequately responsive to medications and breathing techniques, opioids may be needed; concerns over physical dependence, addiction, and respiratory depression should be addressed. Opioids should not be withheld in very severe patients for whom palliative care is the goal. • Monitor for hypoxemia with pulse oximetry and arterial blood gas measurements; administer supplemental oxygen as indicated. Maintain oxygen saturation at 90% or higher to protect vital organ function. • Teach importance of adhering to the oxygen prescription; the presence or absence of dyspnea is an unreliable symptom of hypoxemia. • Monitor for cognitive impairment, which is increased in hypoxemic patients; administer long-term oxygen to improved cardiac and cognitive function and prognosis. • Teach patient the number of hours per day to wear oxygen, the dose of oxygen (usually given as number of liters per minute), and special instructions for using oxygen for sleep and exercise. • Monitor patients with chronic bronchitis and those experiencing an acute exacerbation for increased sputum, quantity, viscosity, and weakness or fatigue, which impairs effective airway clearance. • Assist patient in eliminating or reducing pulmonary irritants including cigarette smoking, second-hand smoke, aerosol cleaning and household products, and cooking fumes. • Teach directed or controlled coughing and to drink enough fluid to prevent dehydration. • Provide chest physiotherapy with postural drainage and/ or mechanical percussion and vibration and suctioning. • Observe for exercise intolerance secondary to exacerbations, hospitalizations, and systemic corticosteroids (associated with myopathy, especially of legs), which add to decreased activity, muscle weakness, and fatigue. • Assist patient with early mobilization during acute exacerbation, including those in intensive care. • Teach patient to alternate high-energy with low-energy activities throughout the day; consider use of walking aids and consultation with occupational and physical therapists. • Nutrition therapy is aimed at assessing the nutritional status of the patient, treating the underlying cause, and stabilizing weight and body composition. Patients may be underweight, of normal weight but have decreased muscle mass, or be overweight because of increased fat mass or increased fluid retention. • Provide oral nutritional supplements to increase body weight and respiratory function. Caution patients to avoid negating the effectiveness of supplements by using them as meal substitutes. • Time bronchodilators before meals; assist severely dyspneic patients during meal times to minimize energy spent eating; teach patients to eat small, frequent meals to help them avoid becoming too full; and encourage the choice of calorie-rich foods when indicated. • Consider referring patients to dieticians and encouraging progressive periods of exercise aimed at increased muscle mass. Overweight patients may need the help of nutrition education by a dietician to help them lose weight safely. Exercise should be encouraged to help patients increase muscle mass.



