Flashcards for USMLE STEP 1 Neurology
Unlock all answers in this set
Unlock answersquestion
The notochord induces what to differentiate into what?
answer
Induces overlying ECTODERM to differentiate into NEUROECTODERM and form NUERAL PLATE
question
Neural plate then gives rise to?
answer
Neural tube and neural crest cells
question
Notochord becomes what?
answer
Nucleus pulposus of the intervertebral disks in adults
question
Alar Plate
answer
Dorsal [Sensory] Same orientation as spinal cord
question
Basal Plate
answer
Ventral [Motor] Same orientation as the spinal cord
question
How does FGF affect chordin and noggin?
answer
FGF regulates chordin and noggin to down regulate BMP which leads to neural plate induction
question
Three Primary Vesicles
answer
1. Forebrain [Prosencephalon] 2. Midbrain [Mesencephalon] 3. Hindbrain [Rhombencphaln]
question
The Forebrain gives rise to:
answer
1. Telencephalon [Cerebral hemispheres, lateral ventricles] 2. Diencephalon [Thalamus, Third Ventricle]
question
The Midbrain gives rise to:
answer
1. Mesencephalon [Midbrain, aqueduct]
question
The Hindbrain gives rise to:
answer
1. Metencephalon [Pons, cerebellum, upper part of the fourth ventricle] 2. Myelencephalon [Medulla, Lower part of the fourth ventricle]
question
CNS/PNS Origins
answer
Neuroectoderm = CNS neurons, ependymal cell [Inner lining of ventricles, makes CSF], oligodendrocytes, astrocytes Neural crest cells = PNS, schwann cells Mesoderm = Microglia [Like Macrophages, originate from Mesoderm]
question
Neural tube defects
answer
NEUROPORES fail to fuse [4th week] ? Persistent connection between amniotic cavity and spinal canal Associated with: 1. Low folate levels before conception and during pregnancy 2. ? a-fetoprotein levels [AFP] in amniotic and maternal serum 3. ? AChE in amniotic fluid [Helpful confirmatory test] -- Fetal AChe in CSF transudates across defect into amniotic fluid
question
Spina bifida occulta

answer
Failure of bony spinal canal to close, NO STRUCTURAL HERNIATION Usually seen at lower vertebral levels DURA INTACT Associated w/ tuft of hair or skin dimple at level of bony defect NORMAL AFP
question
Meningocele

answer
Meninges [BUT NO NEURAL TISSUES] herniates through bony defect
question
Meningomyelocele

answer
Meninges and neural tissue herniate through bony defect Associated w/ Arnold-Chiari Type II Malformation
question
Anencephaly

answer
Malformation of the ANTERIOR NEURAL TUBE ? 1. No forebrain 2. Open calvarium Clinical Findings: 1. ? a-fetoprotein levels [AFP] 2. Polyhydramnios [No swallowing center in brain] 3. Associated w/ MATERNAL TYPE I DIABETES 4. Maternal folate supplementation ? risk
question
Holoprosencephaly
answer
Failure of LEFT AND RIGHT HEMISPHERES TO SEPARATE Usually occurs during the 5th and 6th week May be related to mutations in the SONIC HEDGEHOG signaling pathway Moderate form = Cleft lip/palate Severe form = Cyclopia Seen in: 1. PATAU SYNDROME 2. FETAL ALCOHOL SYNDROME
question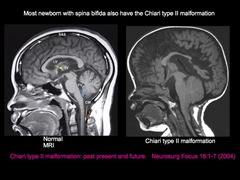
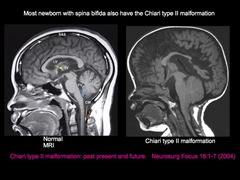
Chiari Type II Malformation
answer
Posterior fossa malformation Significant HERNIATION of the CEREBELLAR TONSILS and VERMIS through FORAMEN MAGNUM with AQUEDUCTAL STENOSIS and HYDROCEPHALUS Patients often present w/: 1. Lumbosacral meningomyelocele 2. Paralysis below the defect
question
Dandy-Walker Malformation
answer
AGENESIS of CEREBELLAR VERMIS with CYSTIC ENLARGEMENT of the 4th ventricle Fills enlarged posterior fossa Associated w/: 1. Hydrocephalus 2. Spina bifida
question
Syringomyelia

answer
Cystic cavity [Syrinx] within SPINAL CORD If central canal = Hydromyelia Crossing anterior spinal commissural fibers are typically damaged CAPE-LIKE BILATERAL LOSS OF PAIN and TEMPERATURE in the UPPER EXTREMITIES Fine touch sensation is preserved Associated w/: 1. Arnold Chiari malformation 2. Trauma 3. Tumor Most common C8-T1 [CERVICAL ENLARGEMENT]
question
Arnold Chiari Type I Malformation
answer
CEREBELLAR TONSILLAR ECTOPIA > 3-5 mm Congenital Usually asymptomatic in childhood Manifests w/ HEADACHE and CEREBELLAR SYMPTOMS
question
Which arches form the anterior 2/3rds of the tongue
answer
1st and 2nd brachial arches -- Sensation via CN V -- Taste via CN VII
question
Which arches form the posterior 1/3rd of the tongue
answer
3rd and 4th brachial arches --Sensation and taste via CN IX -- Extreme posterior vagus
question
Motor innervation of the tongue
answer
CN XII [Hypoglossal nerve] to: 1. Hyoglossus = Retracts and depresses tongue 2. Genioglossus = Protrudes tongue 3. Styloglossus = Draws sides of tongue upward to create a trough for swallowing CN X [Vagus] to: 1. Palatoglossus = Elevates posterior tongue during swallowing
question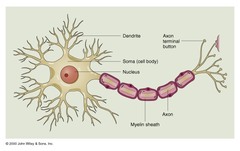
Neurons
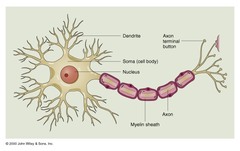
answer
Signal-transmitting cells of the nervous system Permanent cells = DO NOT DIVIDE IN ADULTHOOD Signal relaying cells w/ dendrites [Receive input], cell bodies, and axons [Send output] CELL BODIES AND DENDRITES CAN BE SEEN ON NISSLE STAINING [Stains RER] RER is not present in an axon
question
Loss of Nissle substance indicates
answer
Irreversible hypoxic damage = Red neuron
question
Injury to axon results in what?
answer
Wallerian degeneration ? 1. Degeneration distal to the injury 2. Axonal retraction proximally 3. Allows for regeneration of axon [If in PNS]
question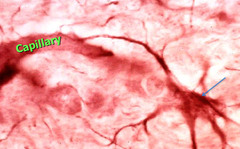
Astrocytes
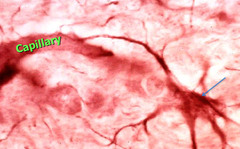
answer
Functions: 1. Physical support 2. Repair 3. K+ metabolism 4. Removal of excess neurotransmitter 5. Component of the blood brain barrier via foot process interaction w/ perivascular space 6. Glycogen fuel reserve buffer 7. Reactive gliosis in response to neural injury 8. DERIVED FROM NEUROECTODERM
question
Astrocyte Marker
answer
GFAP
question
Microglia

answer
Phagocytic scavenger cells of CNS [Mesodermal, mononuclear origin] Activated in response to tissue damage NOT READILY DISCERNIBLE BY NISSL stain HIV-INFECTED MICROGLIA FUSE TO FORM MULTINUCLEATED GIANT CELLS IN CNS
question
Myelin
answer
? Conduction velocity of signals transmitted down axons ? Saltatory conduction of action potential at nodes of Ranvier [HIGH CONCENTRATIONS of Na+ channels] CNS = Oligodendrocyte [Single sheath, 50 axons] PNS = Schwann cells [Single sheath, single axon] Wraps and insulates axons ? Space constant and ? Conduction velocity
question
Schwann cells
answer
Each Schwann cells myelinates only 1 PNS aon Also promotes axonal regeneration Derived from NEURAL CREST ? Conduction velocity of signals transmitted down axons ? Saltatory conduction of action potential at nodes of Ranvier [HIGH CONCENTRATIONS of Na+ channels] May be INJURED IN GUILLAIN-BARRE SYNDROME
question
Acoustic Schwannoma
answer
Typically located in the internal acoustic meatus [CN VIII] If BILATERAL, strongly associated with NEUROFIBROMATOSIS TYPE 2
question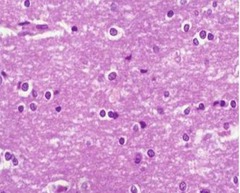
Oligodendroglia
answer
Myelinated axons of neurons in CNS Each oligodendrocyte can myelinate ~30 axons PREDOMINANT TYPE OF GLIAL CELL IN WHITE MATTER Derived from NEUROECTODERM FRIED EGG appearance histologically Injured in: 1. Multiple Sclerosis 2. Multifocal progressive leukoencephalopathy [PML] 3. Leukodystrophies
question
Free nerve endings
answer
C = Slow, unmyelinated fibers A? = Fast, myelinated fibers Location: All skin, epidermis, some viscera Sense: Pain, temperature
question
Meissner Corpuscles
answer
Large myelinated fibers, adapt quickly Location: Glabrous [Hairless] skin Senses: Dynamic, light touch/position sense
question
Pacinian Corpuscles
answer
Large, myelinated fibers, adapt quickly Location: Deep skin layers, ligaments, joints Senses: Vibration, pressure
question
Merkel Discs
answer
Large, myelinated fibers, adapt quickly Location: Fingertips, superficial skin Senses: Pressure, deep static touch [Shapes, edges], position sense
question
Ruffini Corpuscles
answer
Dendritic endings w/ CAPSULE ADAPT SLOWLY Location: Fingertips and joints Senses: Pressure, slippage of objects along surface of skin, joint angle change
question
Endoneurium
answer
Invests single nerve fiber layers [INFLAMMATORY INFILTRATE IN GUILLAIN BARRE SYNDROME] Inner
question
Perineurium
answer
PERMEABILITY BARRIER Surrounds fascicle of nerve fibers MUST BE REJOINED IN MICROSURGERY FOR LIMB REATTACHMENT Around
question
Epineurium
answer
Dense connective tissue that surrounds entire nerve [Fascicles and blood vessels] Epi = Outer
question
Norepinephrine
answer
? Anxiety ? Depression Location: Locus coeruleus [Pons] = Stress and Panic
question
Dopamine
answer
? Huntington's Disease ? Parkinson's Disease ? Depression Location: Ventral tegmentum and substantia nigra pars compacta [Midbrain]
question
5-HT [Serotonin]
answer
? Anxiety ? Depression Location: Raphe nuclei [Pons, medulla, midbrain]
question
ACh
answer
? Parkinson's Disease ? Alzheimer's Disease ? Huntington's disease Location: Basal nucleus of Meynert
question
GABA
answer
? Anxiety ? Huntington Disease Location: Nucleus Accumbens = Reward center, pleasure, addiction, fear
question
Blood brain barrier
answer
Prevents circulating substances [Bacteria and blood] from reaching the CSF/CNS Formed by 3 structures: 1. Tight Junctions between nonfenestrated capillary endothelial cells 2. Basement membrane 3. Astrocyte foot processes Glucose and amino acids cross slowly by CARRIER-MEDIATED transport mechanisms NONPOLAR/LIPID-Soluble cross rapidly via diffusion
question
Specialized brain regions w/ fenestrated capillaries and no blood brain barrier
answer
Allow molecules in blood to affect brain function 1. Area postrema = Vomiting after chemo 2. OVLT = Osmotic sensing Or neurosecretory products to enter circulation 1. Neurohypophysis = ADH release
question
Infarction and/or neoplas destroys what to cause vasogenic edema?
answer
Endothelial tight junction ? vasogenic edema
question
Blood barriers:
answer
1. Blood brain barrier 2. Blood testis barrier 3. Maternal-fetal blood barrier of placenta
question
Hypothalamus
answer
Wears TAN HATS 1. Thirst and water balance 2. Adenohypophysis control [Regulates anterior pituitary] 3. Neurohypophysis [Releases hormones in hypothalamus] 4. Hunger 5. Autonomic regulation 6. Temperature 7. Sexual urges Inputs [AREAS NOT PROTECTED BY BBB] 1. OVLT = Organum vasculosum of the lamina terminalis -- Senses changes in osmolality 2. Area Postrema [Responds to emetics]
question
Vasopressin [ADH] is produced where?
answer
Supraoptic nucleus of the hypothalamus
question
Oxytocin is produced where?
answer
Paraventricular nucleus
question
Lateral Area of the Hypothalamus
answer
1. Hunger 2. Destruction ? Anorexia, failure to thrive 3. INHIBITED BY LEPTIN If you zap your lateral, you shrink laterally
question
Ventromedial Area of the Hypothalamus
answer
1. Satiety 2. Destruction [Craniopharyngioma] ? Hyperphagia 3. STIMULATED BY LEPTIN
question
Anterior Hypothalamus
answer
Cooling, parasympathetic A/C = Anterior, cooling
question
Posterior Hypothalamus
answer
Heating, sympathetic If you zap your Posterior hypothalamus, you become a Poikilothermic [Cold-blooded, like a snake]
question
Suprachiasmatic Nucleus
answer
CIRCADIAN RHYTHMS You sleep to be charismatic
question
Sleep cycle is regulated by what?
answer
Sleep cycle is regulated by the circadian rhythm [Driven by the suprachiasmatic nucleus of the hypothalamus] SCN is regulated by the environment [Light]
question
Circadian rhythms control nocturnal release of what?
answer
1. ACTH 2. Prolactin 3. Melatonin 4. Norepinephrine SCN ? Norepinephrine release ? Pineal Gland ? Melatonin
question
Two Stages of Sleep:
answer
1. Rapid-eye movement [REM] and non-REM -- Extraocular movements during REM sleep due to activity of the PPRF [Paramedian pontine reticular formation/conjugate gaze center] -- Occurs every 90 minutes, duration ? throughout the night At night, BATS, Drink Blood Awake [Eyes open] = Beta Awake [Eyes closed] = Alpha Non-REM N1 =Theta Non-REM N2 = Spindle and K complex Non-REM N3 = Delta REM = Beta
question
What is associated w/ ? REM sleep and delta wave sleep?
answer
1. Alcohol 2. Benzodiazepines 3. Barbiturates 4. Norepinephrine
question
Treatment for bedwetting [Enuresis]
answer
Oral desmopressin [ADH analog] Preferred over imipramine [Due to adverse effects]
question
Treatment for night terrors and sleep-walking
answer
Benzodiazepine
question
Awake [Eye's open]
answer
Alert, active mental concentration Beta [Highest frequency, lowest amplitude]
question
Awake [Eye's closed]
answer
Alpha waves
question
Non-REM Sleep: Stage N1 [5%]
answer
Light sleep Theta waves
question
Non-REM Sleep: Stage N2 [45%]
answer
Deeper sleep, when bruxism occurs Sleep spindles and K complexes
question
Non-REM Sleep: Stage N3 [25%]
answer
Deepest non-REM sleep [Slow-wave sleep] When: 1. Sleepwalking 2. Night Terrors 3. Bedwetting occurs Delta wave [Lowest frequency, highest amplitude]
question
REM Sleep [25%]
answer
1. LOSS OF MOTOR TONE 2. ? Brain O2 use 3. ? Variable pulse and pressure 4. When dreaming and penile/clitoral tumescence occurs 5. May serve memory processing function Beta wave
question
Thalamus
answer
Major relay for all ascending sensory information [EXCEPT OLFACTION]
question
VPL of Thalamus
answer
1. Spinothalamic and dorsal columns/medial lemniscus INFO: Pain, temperature, touch, vibration, proprioception Destination: 1° Somatosensory cortex
question
VPM of Thalamus
answer
1. Trigeminal and gustatory pathway INFO: Face sensation, taste Destination: 1° somatosensory cortex Notes: Makeup goes on the face
question
LGN of Thalamus
answer
1. CN II INFO: Vision Destination: Calcarine sulcus Lateral = Light
question
MGN of Thalamus
answer
1. Superior olive and inferior colliculus of tectum INFO: Hearing Destination: Auditory cortex of temporal lobe Medial = Music
question
VL of Thalamus
answer
1. Basal ganglia, cerebellum INFO: Motor Destination: Motor cortex
question
Limbic System
answer
Collection of neural structures involved in 1. Emotion 2. Long-term memory 3. Olfactory 4. Behavior modification 5. ANS function STRUCTURES: 1. Hippocampus 2. Amygdala 3. Fornix 4. Mammillary bodies 5. Cingulate gyrus RESPONSIBLE FOR [5 F's]: 1. Feeding 2. Fleeing 3. Fightin 4. Feeling 5. Sex
question
Osmotic Demyelination Syndrome [Central pontine myelinolysis]
answer
Clinical Manifestations: 1. Acute paralysis 2. Dysarthria 3. Dysphagia 4. Diplopia 5. LOC 6. Can cause locked-in syndrome MASSIVE AXONAL DEMYELINATION IN PONTINE WHITE MATTER 2° to osmotic changes [Commonly iatrogenic, can be due to overly rapid correction of hyponatremia] -- Results in cerebral edema/herniation Correcting serum Na+ too fast: 1. From low to high, your pons will die! [Osmotic Demyelination Syndrome] 2. From high to low, your brains will blow! [Cerebral edema/herniation]
question
Cerebellum
answer
Modulates movement, aids in coordination and balance Input: 1. Contralateral cortex via middle cerebellar peduncle 2. Ipsilateral proprIoceptive Information via Inferior cerebellar peduncle from spInal cord Output: 1. Sends information to the contralateral cortex to modulate movement -- Output nerves = Purkinje cells ? Deep nuclei of the cerebellum ? Contralateral cortex via superior cerebellar peduncle Deep nuclei [Lateral to medial] = Don't Eat Greasy Foods 1. Dentate 2. Emboliform 3. Globose 4. Fastigial
question
Lateral Lesions to the Cerebellum
answer
Voluntary movement of extremities PROPENSITY TO FALL TOWARD IPSILATERAL SIDE
question
Medial Lesions to the Cerebellum
answer
Lesions involving midline structures [Vermal cortex, fastigial nuclei] and/or flocculonodular lobe ? 1. Truncal ataxia [Wide-based cerebellar gait] 2. Nystagmus 3. Head tilting 4. Generally, midline lesions result in BILATERAL MOTOR DEFICITS affect AXIAL and PROXIMAL LIMB MUSCULATURE
question
Basal Ganglia
answer
Important in voluntary movements and making postural adjustments Receives cortical input, provides negative feedback to cortex to modulate movement Striatum = Putamen [Motor] + Caudate [Cognitive] Lentiform = Putamen + Globus pallidus D1 receptor = DIrect pathway Indirect = Inhibitory
question
Excitatory pathway in the basal ganglia
answer
Cortical inputs stimulate striatum, stimulating release of GABA [Disinhibits the thalamus via the GPi/SNr] = ? Motion
question
Inhibitory pathway in the basal ganglia
answer
Cortical inputs stimulate the striatum [Disinhibits STN via GPe, STN stimulates GPi/SNr to inhibit thalamus] = ? Motion
question
Dopamine binds to what in the basal ganglia
answer
D1 receptors stimulating the excitatory [Direct pathways] D2 inhibiting the inhibitory pathway ? ? Motion
question
Athetosis
answer
Slow, writhing movements, ESPECIALLY SEEN IN FINGERS Locations of Lesion: Basal ganglia [Huntington] WRITHING, SNAKE-LIKE MOVEMENT
question
Chorea
answer
Sudden, jerky, purposeless movements Location of Lesion: Basal ganglia [Huntington] CHOREA = Dance-like
question
Dystonia
answer
Sudden, involuntary muscle contractions Example: Writer's cramp Blepharospasm [Sustained eye twitch]
question
Essential Tremor
answer
HIGH-FREQUENCY tremor w/ SUSTAINED POSTURE [Outstretched arms], WORSENED w/ MOVEMENT Often familial Patient's often self-mediate w/ EtOH = ? Tremor amplitude Treatment: B-blockers, Primidone
question
Hemiballismus
answer
Sudden, wild flingin of 1 arm +/- IPSILATERAL LEG Location: CONTRALATERAL subthalamic nucleus [Lacunar stroke]
question
Intention Tremor
answer
Slow zigzag motion when pointing/extending toward target Location: Cerebral dysfunction
question
Myoclonus
answer
Sudden, brief, uncontrolled muscle contraction JERK HICCUPS common in metabolic abnormalities such as renal and liver failure
question
Resting tremor
answer
Uncontrolled movement of distal appendages [Most appreciable in hands] Tumor ALLEVIATED BY INTENTIONAL MOVEMENT Example: Parkinson's disease [Pill-rolling tremor]
question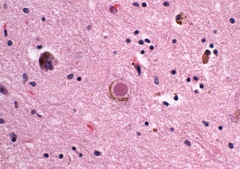
Parkinson's Disease
answer
Degenerative disorder of CNS associated w/ LEWY BODIES [Composed of a-synuclein = Intracellular eosinophilic inclusions] and LOSS OF DOPAMINERGIC NEURONS [Depigmentation] of substantia nigra pars compacta Parkinson TRAPS your body: 1. Tremor [Pill-rolling tremor at rest 2. Rigidity 3. Akinesia [or bradykinesia] 4. Postural instability 5. Shuffling gait
question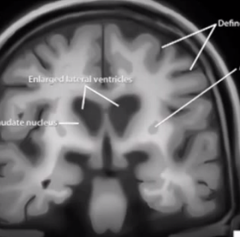
Huntington's Disease
answer
AUTOSOMAL DOMINANT Trinucleotide repeat on chromosome 4 [CAG repeats] -- Caudate loses ACh and GABA Symptoms manifest between ages 20-50 Clinical Manifestations: 1. Choreiform movements 2. Aggression 3. Depression 4. Dementia [Sometimes mistaken for substance abuse] Labs: 1. ? Dopamine 2. ? ACh 3. ? GABA Neuronal cell death via NMDA-R binding and GLUTAMATE TOXICITY ATROPHY OF CAUDATE NUCLEI w/ ex vacuo DILATION OF FRONTAL HORNS
question
Aphasia
answer
Higher-order inability to speak [Language deficit]
question
Dysarthria
answer
Motor inability to speak [Movement deficit]
question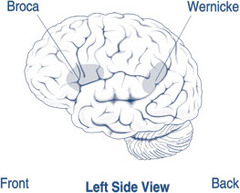
Broca's Area
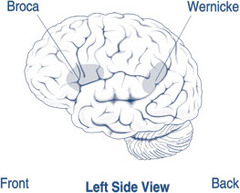
answer
NONFLUENT aphasia Intact comprehension with IMPAIRED REPETITION INFERIOR FRONTAL GYRUS OF FRONTAL LOBE
question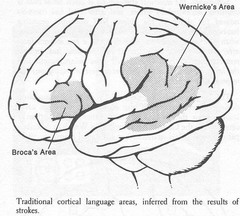
Wernicke' Area
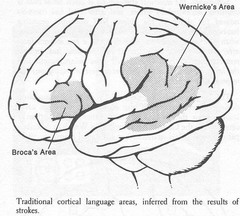
answer
FLUENT aphasia with IMPAIRED COMPREHENSION and REPETITION SUPERIOR TEMPORAL GYRUS OF TEMPORAL LOBE Wernick is Wordy but makes no sense
question
Conduction Aphasia
answer
Poor repetition but fluent speech, INTACT COMPREHENSION Caused by damage to the arcuate fasciculus Can't repeat phrases like "NO, IFS, ANDS, or BUTS"
question
Global
answer
NONFLUENT APHASIA WITH IMPAIRED COMPREHENSION Arcuate fasciculus, Broca's, and Wernicke's areas affected
question
Transcortical motor
answer
Nonfluent aphasia with good comprehension and intact repetition
question
Transcortical sensory
answer
Poor comprehension with fluent speech and intact repetition
question
Mixed transcortical
answer
Nonfluent speech, poor comprehension, INTACT REPEPTITON
question
Amygdala Lesion [Bilateral]
answer
Kluver-Bucy Syndrome = Disinhibited behavior [Hyperphagia, hypersexuality, hyperorality] Associated w/ HSV-1
question
Frontal lobe Lesion
answer
Disinhibition and deficits in concentration, orientation, judgement May have a reemergence of primitive reflexes
question
Nondominant parietal-temporal cortex Lesion
answer
HEMISPATIAL NEGLECT [Agnosia of the contralateral side of the world]
question
Dominant parietal-temporal cortex Lesion
answer
1. Agraphia 2. Acalculia 3. Finger agnosia 4. Left-right disorientation GESTERMANN SYNDROME
question
Reticular Activating System [Midbrain] Lesion
answer
Reduced levels of arousal and wakefulness [Coma]
question
Mammillary Bodies [Bilateral] Lesion
answer
Wernicke-Korsakoff Syndrome 1. Confusion 2. Ophthalmoplegia 3. Ataxia 4. Memory loss [Anterograde and retrograde amnesia] 5. Confabulation 6. Personality changes Associated w/ B1 [Thiamine] Deficiency and excessive EtOH use Can be precipitated by GLUCOSE w/out B1 to a B1-deficient patient Wernicke problems in a can of beer: 1. Confusion 2. Ataxia 3. Nystagmus
question
Basal Ganglia Lesion
answer
May result in a tremor at rest, chorea, athetosis Parkinson's Disease Huntington's Disease
question
Cerebellar Hemisphere Lesion
answer
1. Intention tremor 2. Limb ataxia 3. Loss of balance 4. Damage to cerebellum ? Ipsilateral deficits FALL TOWARD THE SIDE OF THE LESION Cerebellar hemispheres are LATERALLY LOCATED and affect the LATERAL LIMBS
question
Cerebellar Vermis Lesion
answer
1. Truncal ataxia 2. Dysarthria Vermis is CENTRALLY LOCATION affects the CENTRAL LIMBs
question
Subthalamic Nucleus Lesion
answer
CONTRALATERAL hemiballismus
question
Hippocampus [Bilateral]
answer
Anterograde amnesia = Inability to make new memories
question
Paramedian Pontine Reticular Formation
answer
Eyes look away from the side of lesion
question
Frontal Eye fields
answer
Eyes look toward the side of the lesion
question
Watershed Zones
answer
Between 1. Anterior/middle cerebral 2. Posterior/Middle cerebral DAMAGE IN SEVERE HYPOTENSION 1. Upper arm/leg weakness 2. Defects in higher-order visual processing
question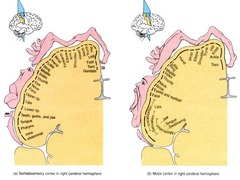
Homunculus
answer
Topographic representation of motor and sensory areas in cerebral cortex Distorted image is due to certain body regions being more richly innervated and thus having ? cortical representations
question
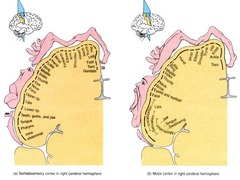
Regulation of cerebral perfusion
answer
Brain perfusion relies on tight autoregulation Cerebral perfusion is mostly driven by PCO2 [PO2 modulates perfusion in severe hypoxia] Therapeutic hyperventilation [? PCO2], helps ? ICP in cases of 1. Acute cerebral edema [Stroke, trauma] via vasoconstriction Fainting in panic attacks due to ? perfusion
question
Hypoxemia and cerebral perfusion
answer
? cerebral perfusion pressure only when PO2 ; 5o mmHg
question
Cerebral perfusion pressure is proportional to what
answer
Cerebral perfusion pressure is proportional to PCO2 until PCO2 ; 90 mmHg
question
Cerebral perfusion and blood pressure
answer
Cerebral perfusion lies on pressure gradient between mean arterial pressure [MAP] and ICP ? blood pressure or ? ICP ? ? Cerebral perfusion pressure [CPP] CPP = MAP - ICP If CPP = 0, there is not cerebral perfusion ? Brain death
question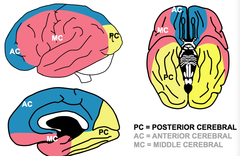
MCA Lesion
answer
1. Motor cortex = Upper limb and face [Contralateral paralysis] 2. Sensory cortex = Upper limb and face [Contralateral loss of sensation] 3. Temporal lobe = Wernicke Area 4. Frontal lobe = Broca's Area APHASIA IF IN DOMINANT [Usually left hemisphere] HEMINEGLECT IF IN NONDOMINANT [Usually right hemisphere]
question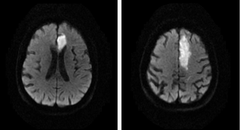
ACA Lesion
answer
1. Motor cortex = Lower limb [Contralateral paralysis] 2. Sensory cortex = Lower limb [Contralateral loss of sensation]
question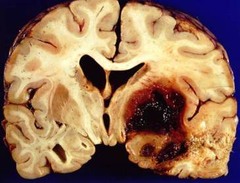
Lenticulostriate Artery Lesion
answer
Striatum [Putamen = Motor, Caudate = Cognitive, Internal capsule Contralateral hemiparesis/hemiplegia COMMON LOCATION OF LACUNAR INFARCTS, 2° to unmanaged hypertension
question
Anterior Spinal [ASA]
answer
1. Lateral corticospinal tract = Contralateral hemiparesis [Upper and lower limbs] 2. Medial lemniscus = ? Contralateral proprioception 3. Caudal medulla = Hypoglossal nerve [Ipsilateral hypoglossal dysfunction = Tongue licks the lesion] STROKE COMMONLY BILATERAL
question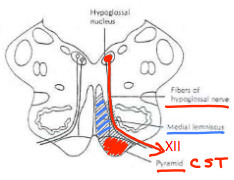
Medial Medullary Syndrome
answer
Caused by infarct of paramedian branches of ASA and vertebral arteries
question
PICA Lesion
answer
1. Lateral medulla -- Vestibular Nuclei -- Lateral Spinothalamic tract -- Spinal trigeminal nucleus -- Nucleus ambiguus -- Sympathetic fibers -- Inferior cerebellar peduncle [Proprioceptive information] Clinical Manifestations: 1. Vomiting 2. Vertigo 3. Nystagmus 4. ? Pain and temperature sensation from IPSILATERAL FACE and CONTRALATERAL BODY 5. DYSPHAGIA 6. HOARSENESS 7. ? Gag reflex 8. Ipsilateral horner syndrome 9. Ataxia 10. Dysmetria
question![Lateral Medullary [Wallenberg Syndrome] Lesion Lateral Medullary [Wallenberg Syndrome] Lesion](https://studyhippo.com/wp-content/uploads/2018/04/lateral-medullary-wallenberg-syndrome-lesion.png)
Lateral Medullary [Wallenberg Syndrome] Lesion
![Lateral Medullary [Wallenberg Syndrome] Lesion Lateral Medullary [Wallenberg Syndrome] Lesion](https://studyhippo.com/wp-content/uploads/2018/04/lateral-medullary-wallenberg-syndrome-lesion.png)
answer
Nucleus ambiguus effects are SPECIFIC TO PICA lesion "Don't PICA Horse [Hoarseness] that can't eat [Dysphasia]
question
ACA
answer
LATERAL PONS 1. Cranial facial nerve 2. Vestibular nuclei 3. Facial nuclei 4. Spinal trigeminal nuclei 5. Cochlear nuclei 6. Sympathetic fibers MIDDLE AND INFERIOR CEREBELLAR PEDUNCLES 1. Ataxia 2. Dysmetria Clinical Manifestations: 1. Vomiting 2. Vertigo 3. Nystagmus 4. PARALYSIS OF FACE 5. ? Lacrimation, salivation 6. ? Taste from anterior 2/3rd of tongue 7. IPSILATERAL ? pain and temperature 8. CONTRALATERAL ? pain and temperature
question
Lateral Pontine Syndrome
answer
Facial nucleus effects are specific to AICA lesions FACIAL DROOP means AICA's pooped
question
PCA
answer
1. Occipital cortex 2. Visual cortex [CONTRALATERAL hemianopia w/ macular sparing]
question
Basilar Artery
answer
1. Pons 2. Medulla 3. Lower Midbrain 4. Corticospinal and corticobulbar tracts 5. Ocular cranial nerve nuclei 6. Paramedian pontine reticular formation Clinical Manifestation [LOCKED IN SYNDROME]: 1. Preserved consciousness and blinking 2. Quadriplegia 3. Loss of voluntary facial, mouth, and tongue movement 4. Locked-in syndrome
question
Anterior Communicating Artery [ACom]
answer
Most common lesion is ANEURYSM Can lead to STROKE SACCULAR [BERRY] aneurysm can impinge cranial nerves VISUAL FIELD DEFECTS [Due to compression of the optic chiasm] LESIONS ARE TYPICALLY ANEURYSMS, not strokes
question
Posterior Communicating Artery [PCom]
answer
Common site of saccular aneurysm CN III palsy = EYES DOWN AND OUT [Ptosis and mydriasis] LESIONS ARE TYPICALLY ANEURYSMS NOT STROKES
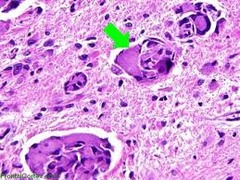
question![Saccular [Berry] Aneurysm Saccular [Berry] Aneurysm](https://studyhippo.com/wp-content/uploads/2018/04/saccular-berry-aneurysm.png)
Saccular [Berry] Aneurysm
![Saccular [Berry] Aneurysm Saccular [Berry] Aneurysm](https://studyhippo.com/wp-content/uploads/2018/04/saccular-berry-aneurysm.png)
answer
Occurs at bifurcations in the CIRCLE OF WILLIS Most common site is JUNCTION OF ANTERIOR COMMUNICATING and ANTERIOR CEREBRAL Rupture [Most common complication] ? Subarachnoid hemorrhage *** WORST HEADACHE OF MY LIFE Can also lead to hemorrhagic stroke Can cause: 1. Bitemporal hemianopia via compression of optic chiasm Associated with: 1. ADPKD 2. Ehlers-Danlos Syndrome 3. Advanced age 4. HTN 5. Smoking 6. ? Risk in black
question
Charcot-Bouchard Microaneurysm
answer
Chronic HTN Affects small vessels [Basal ganglia, thalamus]
question
Central Post-Stroke Pain Syndrome
answer
Neuropathic pain due to THALAMIC LESIONS Initial paresthesia followed in WEEKS TO MONTHS by 1. Allodynia [Ordinarily painless stimuli cause pain] 2. Dysesthesia OCCURS IN 10% of STROKE PATIENTS
question
Epidural hematoma

answer
Rupture of MIDDLE MENINGEAL ARTERY [Branch of the MAXILLARY] Often 2° to fracture of temporal bone LUCID INTERVAL Rapid expansion under systemic arterial pressure ? TRANSTENTORIAL herniation, CN III Palsy CT show BICONVEX [Lentiform], Hyperdense blood collection NOT CROSSING SUTURE LINES Can cross FALX and TENTORIUM
question
Subdural hematoma
answer
Rupture of BRIDGING VEINS SLOW VENOUS BLEED [Less pressure =Hematoma develops over time] Seen in: 1. Elderly 2. Alcoholics 3. Blunt trauma 4. SHAKEN BABY SYNDROME [Predisposing factors = Brain atrophy, shaking, whiplash] CRESCENT-SHAPED hemorrhage that CROSSES SUTURE LINES MIDLINE SHIFT Cannot cross falx, tentorium
question
Subarachnoid hemorrhage
answer
Rupture of ANEURYSM [Berry/saccular aneurysm in Ehlers-Danlos and ADPKD] or ARTERIOVENOUS MALFORMATION Rapid time course WORST HEADACHE OF MY LIFE Bloody or yellow spinal tap [Xanthochromia] 2-3 days afterward, risk of vasospasm due to blood breakdown [Not visible on CT, treat w/ NIMODIPINE] and rebleed [Visible on CT]
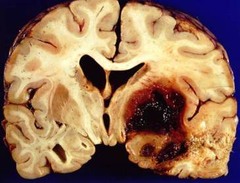
question![Intraparenchymal [Hypertensive] Hemorrhage Intraparenchymal [Hypertensive] Hemorrhage](https://studyhippo.com/wp-content/uploads/2018/04/intraparenchymal-hypertensive-hemorrhage.png)
Intraparenchymal [Hypertensive] Hemorrhage
![Intraparenchymal [Hypertensive] Hemorrhage Intraparenchymal [Hypertensive] Hemorrhage](https://studyhippo.com/wp-content/uploads/2018/04/intraparenchymal-hypertensive-hemorrhage.png)
answer
Commonly caused by SYSTEMIC HTN Also seen w/ 1. AMYLOID ANGIOPATHY [Recurrent lobar hemorrhagic stroke in elderly 2. Vasculitis 3. Neoplasm Typically occurs in BASAL GANGLIA, INTERNAL CAPSULE [Charcot-Bouchard Aneurysm of lenticulostriate vessels]
question
Ischemic Brain Disease/Stroke
answer
Irreversible damage begins after 5 minutes of hypoxia [Due to glucose dependence] Most vulnerable: 1. Hippocampus 2. Neocortex 3. Cerebellum 4. Watershed areas Ischemic HYPOxia = HYPOcampus most vulnerable
question
Stroke Imaging
answer
Noncontrast CT to exclude hemorrhage [Before tPA can be given] CT detects changes in 6-24 hours Diffusion weighed MRI can detect ischemia w/in 3-30 minutes
question
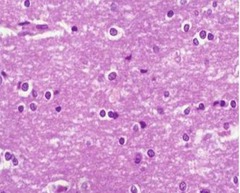
Time since ischemia event and histologic factors
answer
12-48 hours = Red neurons 48-72 hours = Necrosis + neutrophils 3-5 days = Macrophages [Microglia] 1-2 weeks = Reactive gliosis + vascular proliferation ; 2 weeks = Glial scar
question
Hemorrhagic Stroke [15%]
answer
Intracerebral bleeding, often due to: 1. HTN 2. Anticoagulation 3. Cancer [Abnormal vessels can bleed] May be 2° to ischemic stroke followed by reperfusion [? Vessel fragility] BASAL GANGLIA ARE THE MOST COMMON SITE OF INTRACRANIAL HEMORRHAGE
question
Ischemic Stroke [85%]
answer
Acute blockage of vessels ? Disruption of blood flow and subsequent ischemia ? LIQUEFACTIVE NECROSIS Three Types 1. Thrombotic = Clot forms directly at site of infarction [Commonly MCA] 2. Embolic = Embolus from another part of the body obstructs vessel -- Can affect multiple vascular territories -- Examples: Atrial fibrillation, DVT w/ patent foramen ovale 3. Hypoxic = Hypoperfusion or hypoxemia -- Common during CARDIOVASCULAR SURGERIES -- TENDS TO AFFECT WATERSHED AREAS Treatment: tPA [If w/in 3-4.5 hours of onset and no hemorrhage/risk of hemorrhage] Reduce risk w/ medical therapy: 1. Aspirin 2. Clopidogrel 3. Optimum control of BP, blood sugars, lipids 4. Treat conditions that ? atrial fibrillation
question
Transient Ischemic Attack [TIA]
answer
Brief, reversible episode of focal neurologic dysfunction without acute infarction [- MRI] Majority resolves in ; 15 minutes, deficits due to FOCAL ISCHEMIA
question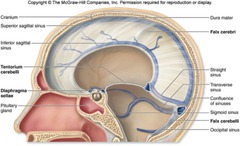
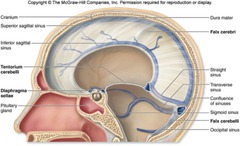
Dural Venous Sinuses
answer
Large venous channels that run through the dura Drain blood from cerebral veins and receive CSF from arachnoid granulation EMPTIES INTO JUGULAR VEINS
question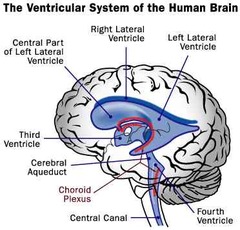
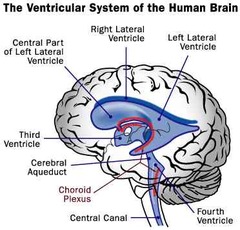
Ventricular System
answer
Lateral ventricle ? 3rd ventricle via right and left interventricular foramen of Monro 3rd ventricle ? 4th ventricle via cerebral aqueduct [of Sylvius] 4th ventricle ? Subarachnoid space via 1. Formina of Luschka [Lateral] 2. Foramina of Magendie [Medial]
question
CSF
answer
Is made from the ependymal cells of the choroid plexus Reabsorbed in by subarchnoid granulation and then drains into the dural venous sinuses
question
Idiopathic Intracranial Hypertension [Pseudotumor cerebri]
answer
? ICP with no apparent cause on imaging [No hydrocephalus, obstruction of CSF outflow] Patients present w/: 1. Headaches 2. Diplopia [Usually from CN VI palsy] 3. Non mental status alterations 4. Papilledema [Seen on exam] Risk factors: 1. Being a woman of child-bearing years 2. Vitamin A excess 3. DANAZOL [Synthetic steroid suppresses GnRH] Lumbar Puncture reveals ? opening pressure and provides headache relief Treatment: 1. Weight loss 2. Acetazolamide [Carbonic anhydrase inhibitor] 3. Topiramate [Anticonvulsant] 4. Invasive procedures for refractory cases [Repeat lumbar puncture, CSF shunt placement, nerve fenestration surgery]
question
Communicating Hydrocephalus
answer
? CSF absorption by arachnoid granulations ? ? ICP, papilledema, herniation [Arachnoid scarring post-meningitis + chronic subdural hematomas]
question
Normal Pressure Hydrocephalus
answer
AFFECTS ELDERLY, idiopathic CSF pressure elevated only EPISODICALLY Does not result in ? subarchnoid space volume EXPANSION OF VENTRICLES distorts the fibers of the CORONA RADIATA ? Triad: 1. Urinary Incontinence = Wet 2. Ataxia = Wobbly 3. Cognitive Dysfunction [Sometimes reversible] = Wacky
question
Noncommunicating hydrocepahlus
answer
Caused by STRUCTURAL BLOCKAGE of CSF circulation through the ventricular system [Stenosis of aqueduct of Sylvius, Colloid cyst blocking foramen of Monro]
question
Ex vacuo ventriculomegaly
answer
Appearance of ? CSF on imaging is due to DECREASED BRAIN TISSUE [Neuronal atrophy] 1. Alzheimer's disease 2. Advanced HIV 3. PICK DISEASE ICP is NORMAL, Triad is not seen
question
Spinal Nerves
answer
There are 31 pairs of spinal nerves in total: 1. 8 cervical 2. 12 thoracic 3. 5 Lumbar 4. 5 Sacral 5. 2 coccygeal Nerves C1-C7 exit ABOVE the corresponding vertebrae C8 spinal nerve exits BELOW C7 and above T1 All other spinal nerves exit BELOW
question
Vertebral disk herniation
answer
Nucleus pulposus [Soft central disk] herniates through annulus fibrosus [Outer ring] Usually POSTEROLATERALLY at L4-L5, L5-S1
question
Spinal Cord - Lower Extent
answer
In adults, the spinal cord extends to the lower border of L1-L2 Subarachnoid space [Which contains CSF] extends to lower border of S2 vertebrae Lumbar puncture is usually performed at L3/L4 or L4/L5 [Level of the cauda equina]
question
Goal of lumbar puncture
answer
To obtain a sample of CSF w/out damaging spinal cord To keep the cord alive, go in between L3-L5
question
Spinal Cord Mnemonics
answer
Legs [Lumbosacral] are Lateral in Lateral Corticospinal tract Dorsal columns are organized as you are, hands at side, arms out side legs [Cuneatus outside of gracilis]
question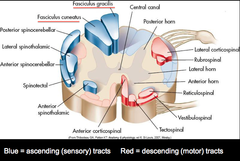
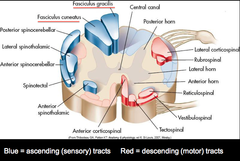
Ascending Tracts
answer
1. Dorsal Column [Pressure, vibration, touch, proprioception] 2. Fasciculus gracilis [Lower body, legs] 3. Fasciculus cuneatus [Upper body, arms] 4. Lateral spinothalamic tract [Pain and temperature] 5. Anterior spinothalamic tract [Touch, pressure] ASCENDING TRACTS SYNAPSE THEN CROSS
question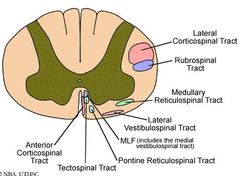
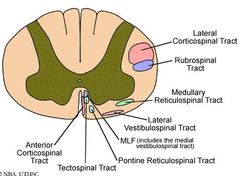
Descending Tracts of Spinal Cord
answer
1. Lateral corticospinal tract [Voluntary motor] 2. Anterior corticospinal tract [Voluntary motor]
question
Dorsal Column
answer
Ascending pressure, vibration, fine touch, proprioception 1st Order Neuron = -- Sensory nerve endings ? Cell body in dorsal root ganglion -- Enters spinal cord, SYNAPSES IN IPSILATERAL NUCLEUS CUNEATUS OR GRACILIS ? ascends ipsilaterally in dorsal column 2nd Order Neuron -- Decussates in medulla ? Ascends CONTRALATERALLY in MEDIAL LEMNISCAL ? Synapses in the VPL [Thalamus] 3rd Order Neuron Sensory cortex
question
Spinothalamic Tract
answer
Ascending [Lateral] pain and temperature, [Anterior] Crude touch and pressure 1st Order Neuron = -- Sensory nerve endings [A? and C Fibers]? Cell body in dorsal root ganglion -- Enters spinal cord, SYNAPSES IN IPSILATERAL GRAY MATTER [Spinal cord] ? 2nd Order Neuron -- Decussates at ANTERIOR WHITE COMMISSURE ? Ascends CONTRALATERALLY ? Synapses in the VPL [Thalamus] 3rd Order Neuron Sensory cortex
question
Lateral Corticospinal Tract
answer
Descending, Voluntary movement of contralateral limbs UMN: Cell body in 1° motor cortex ? Descends ipsilaterally through INTERNAL CAPSULE, most fibers decussate at CAUDAL MEDULLA [Pyramidal decussation] ? Descends CONTRALATERALLY 1st Synapse: 1. Cell body of ANTERIOR HORN LMN: Leaves spinal cord Synapse II: NMJ
question
UMN Lesions Signs
answer
Clinical Manifestations: 1. Weakness 2. Hyperreflexia 3. Hypertonia 4. Positive Babinski [Normal in infants] 5. SPASTIC paralysis 6. CLASP KNIFE SPASTICITY Upper MN = Everything up [Tone, DTR, toes]
question
LMN Lesion Signs
answer
Clinical Manifestations: 1. Weakness 2. Hyporeflexia 3. Hypotonia 4. Atrophy 5. Fasciculations [Muscle twitching] 6. FLACCID paralysis Lower MN = Everything lowered [Tone, DTR, toes]
question
Werdnig Hoffman Disease
answer
Poliomyelitis and spinal muscular atrophy LMN lesions only [Due to destruction of anterior horns] FLACCID PARALYSIS
question
Multiple Sclerosis
answer
Due to demyelination MOSTLY WHITE MATTER OF CERVICAL REGION Random and ASYMMETRIC lesions due to demyelination Clinical Manifestations: 1. Scanning speech 2. Intention tremor 3. Nystagmus
question![Amyotrophic Lateral Sclerosis [ALS] Amyotrophic Lateral Sclerosis [ALS]](https://studyhippo.com/wp-content/uploads/2018/04/amyotrophic-lateral-sclerosis-als.jpg)
Amyotrophic Lateral Sclerosis [ALS]
![Amyotrophic Lateral Sclerosis [ALS] Amyotrophic Lateral Sclerosis [ALS]](https://studyhippo.com/wp-content/uploads/2018/04/amyotrophic-lateral-sclerosis-als.jpg)
answer
Combined UMN and LMN deficits with NO SENSORY LOSS or oculomotor deficits Can be caused by SUPEROXIDE DISMUTASE 1 defect Clinical Manifestations: 1. Commonly presents as fasciculations with eventual ATROPHY AND WEAKNESS OF HANDS 2. Fatal 3. Riluzole treatment modestly ? survival by ? presynaptic glutamate release Lou Gehrig disease = Give RiLOUzole [Glutamate antagonist]
question
Complete Occlusion of Anterior Spinal Artery
answer
SPARES DORSAL COLUMN and LISSAUER TRACT Upper thoracic ASA territory is WATERSHED AREA Artery of Adamkiewicz supplies ASA below T8
question
Tabes Dorsalis
answer
Caused by 3° Syphilis Results from degeneration [Demyelination] of DORSAL COLUMNS and roots ? 1. Impaired sensation and proprioception 2. Progressive sensory ataxia [Inability to sense or feel legs ? poor coordination] Associated w/ 1. Charcot joints 2. Shooting pain 3. Argyll Robertson pupil 4. ABSENCE OF DTRs and + Romberg Sign
question
Syringomyelia

answer
Sprinx expands and damages ANTERIOR WHITE COMMISSURE of SPINOTHALAMIC TRACT [2nd order neurons] 1. Bilateral loss of pain and temperature [C8-T1] 2. Seen in Chiari Type I Malformation 3. Can expand and affect other tracts
question
Vitamin B12 Deficiency
answer
Subacute Combine Degeneration Demyelination of DORSAL COLUMNS, LATERAL CORTICOSPINAL TRACTS, and SPINOCEREBELLAR TRACTS 1. Gait ataxia 2. Paresthesia 3. Impaired position and vibration sense
question
Poliomyelitis
answer
Caused by poliovirus [Fecal-oral transmission] Replicates in OROPHARYNX and SMALL INTESTINE before spreading via bloodstream to CNS Infection causes destruction of cells in ANTERIOR HORN of spinal cord [LMN] Symptoms [LMN Signs] 1. Weakness 2. Hypotonia 3. Flaccid paralysis 4. Fasciculations 5. Hyporeflexia 6. Muscle atrophy 7. Signs of infection [Malaise, headache, fever, nausea] Findings: 1. CSF w/ ? WBC and slight ? protein [NO CHANGE IN CSF GLUCOSE] 2. Virus recovered from throat or stool
question
Spinal Muscular Atrophy [Werdnig-Hoffman Disease]
answer
Congential degeneration of anterior horns of spinal cord ? LMN FLOPPY BABY w/ marked hypotonia and TONGUE FASCICULATIONS Infantile type has median age of death at 7 months AUTOSOMAL RECESSIVE INHERITANCE
question
Friedrich Ataxia

answer
AUTOSOMAL RECESSIVE Trinucleotide repeat [GAA] on chromosome 9 in the gene that encodes FRATAXIN [Iron binding protein] Leads to MITOCHONDRIAL DYSFUNCTION Degeneration of multiple spinal tracts 1. Muscle weakness 2. Loss of DTRs, vibratory sense, proprioception 3. STAGGERING GAIT 4. FREQUENT FALLING 5. Nystagmus 6. Dysarthria 7. Pes Cavus 8. Hammer toes 9. DIABETES MELLITUS, HYPERTROPHIC CARDIOMYOPATHY [Cause of death] 10. Presents in childhood w/ KYPHOSCOLIOSIS
question
Brown-Sequard Syndrome

answer
Hemisection of spinal cord Findings: 1. Ipsilateral UMN signs BELOW level of lesion 2. Ipsilateral loss of tactile, vibration, proprioception sense BELOW level of lesion [Due to dorsal column damage] 3. CONTRALATERAL pain and temperature loss below level of lesion [Loss of spinothalamic] 4. Ipsilateral loss of ALL SENSATION AT LEVEL OF LESION 5. Ipsilateral LMN signs IF lesion occurs ABOVE T1 = PATIENT WILL PRESENT WITH HORNER SYNDROME [Due to damage of the oculosympathetic pathway]
question
Landmark Dermatomes: C2
answer
Posterior half of skull [ca]
question
Landmark Dermatome: C3
answer
High turtleneck shirt
question
Landmark Dermatome: C4
answer
Low collar shirt
question
Landmark Dermatome: T4
answer
At the nippel [The Teat pore]
question
Landmark Dermatome: T7
answer
Xiphoid Process
question
Landmark Dermatome: T10
answer
At the umbilicus [Important for early appendicitis pain referral] T10 at the belly butTEN
question
Landmark Dermatome: L1
answer
Inguinal ligament LI =Inguinal Ligament
question
Landmark Dermatome: L4
answer
Included kneecap Down on ALL 4's
question
S2, S3, S4
answer
Erection and sensation of the penis S2, S3, S4 Keeps the penis off the floor
question
S1, S2
answer
Buckle my shoe [Achilles tendon reflex]
question
L3. L4
answer
Kick the door [Patellar reflex]
question
C5, C6
answer
Pick up sticks [Biceps reflex]
question
C7, C8
answer
Lay them straight [Triceps reflex]
question
L1, L2
answer
Testicles move [Cremaster reflex]
question
S3, S4
answer
Winks galore [Anal wink reflex]
question
Primitive Reflexes
answer
CNS reflexes that are present in healthy infant, but are absent in neurologically intact adult Normally disappear w/in the first year of life Primitive reflexes are inhibited by a mature developing frontal lobe May reemerge in an adult following FRONTAL LOBE LESIONS ? Of inhibition of this reflex
question
Moro Reflex
answer
"Hanging on for life" Reflex = Abduct/Extend when startled, then draw together
question
Rooting Reflex
answer
Movement of head toward side of cheek if mouth or cheek is stroked [Nipple seeking]
question
Suckling Reflex
answer
Sucking response when roof of mouth is touched
question
Palmar Reflex
answer
Curling of fingers if palms are stroked
question
Plantar Reflex
answer
DORSIFLEXION of large toe and FANNING OF OTHER TOES upon plantar stimulation Babinski sign - Presence of this reflex in an adult, may signify an UML
question
Galant Reflex
answer
Stroking along one side of the spine while newborn is in a ventral position [Face down] causes LATERAL FLEXION OF LOWER BODY TOWARD STIMULATED SIDE
question
CN nuclei that lie medially
answer
III, IV, VI, XII "Factors of 12, except 1 and 2"
question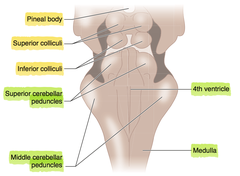
Dorsal View of Brainstem
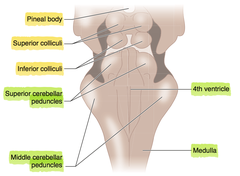
answer
Pineal Gland = Melatonin secretion, circadian rhythms Superior Colliculi = Conjugate vertical gaze center Inferior Colliculus = Auditory Your EYES are ABOVE your EARS
question
Parinaud Syndrome
answer
Paralysis of the conjugate vertical gaze due to lesion in SUPERIOR COLLICULUS [Stroke, hydrocephalus, pinealoma]
question
Cranial Nerve Nuclei
answer
Located in the tegmentum portion of brain stem [Between dorsal and ventral portions] Midbrain = Nuclei CN III, IV Pons = Nuclei CN V, VI, VII, VIII Medulla = Nuclei CN IX, X, XII Spinal Cord = Nucleus of CN XI Lateral Nuclei = Sensory [aLar plate] --- Sulcus limitans Medial Nuclei = Motor [Basal Plate]
question
Cranial Nerve and Vessel Pathways: Cribriform plate
answer
CN I
question
Cranial Nerve and Vessel Pathways: Middle Cranial Fossa
answer
CN II-IV [Through sphenoid bone] 1. Optic canal = CN II, ophthalmic artery, central retinal vein 2. Superior Orbital Fissure = CN III, IV, V1, VI, ophthalmic vein, sympathetic fibers 3. Foramen Rotundum [CN V2] 4. Foramen Ovale [CN V3] 5. Foramen Spinosum [Middle Meningeal Artery]
question
Cranial Nerve and Vessel Pathways: Internal Auditory Meatus
answer
CN VII, VIII
question
Jugular Foramen
answer
CN IX, X, XI, jugular vein
question
Hypoglossal canal
answer
CN XII
question
Foramen Magnum
answer
Spinal roots of XI, brain stem, vertebral arteries
question
Olfactory Nerve
answer
CN I Smell [ONLY CN WITHOUT THALAMIC RELAY TO CORTEX] Sensory
question
Optic Nerve
answer
CN II Sight Sensory
question
Oculomotor
answer
CN III 1. Eye movement [SR, IR, MR, IO] 2. Pupillary constriction -- Sphincter pupillae = Edinger-Westphal nucleus, muscarinic receptors 3. Accomodation 4. Eyelid opening [Levator palpebrae MOTOR
question
Trochlear
answer
CN IV Eye movement [SO] Motor
question
Trigeminal
answer
CN V 1. Mastication 2. Facial sensation [Ophthalmic, Maxillary, Mandibular divisions 3. Somatosensation from anterior 2/3 of tongue BOTH
question
Abducens
answer
CN VI Eye movement [LR] MOTOR
question
Facial
answer
CN VII 1. Facial movements 2. Taste from anterior 2/3rd of tongue 3. Lacrimation, salivation [Submandibular, Sublingual glands] 4. Eye closing [Orbicularis oculi] 5. Stapedius muscle in ear [Nerve courses through parotid gland but does not innervate it]
question
Vestibulocochlear
answer
CN VIII Hearing and balance Sensory
question
Glossopharyngeal
answer
1. Taste and somatosensation from posterior 2/3 of tongue 2. Swallowing 3. Salivation [Parotid gland] 4. Monitoring carotid body and sinus chemo- and baroreceptors 5. Stylopharyngeus [Elevates pharynx, larynx] BOTH
question
Vagus
answer
CN X 1. Taste from epiglottic region 2. Swallowing 3. Soft palate elevation 4. Midline uvula 5. Talking 6. Coughing 7. Thoracoabdominal viscera 8. Monitoring aortic arch chemo- and baroreceptors BOTH
question
Accessory
answer
CN XI 1. Head turning, shoulder shrugging [SCM, trapezius] MOTOR
question
Hypoglossal
answer
CN XII Tongue movement MOTOR
question
Mnemonic for Cranial Nerves
answer
Some Say Marry Money But My Brother Says Big Brains Matter Most
question
Nucleus Solitarius
answer
Visceral SENSORY information [Taste baroreceptors, gut distension] CN VII, IX, X
question
Nucleus aMbiguus
answer
MOTOR innervation of pharynx, larynx, upper esophagus [Swallowing, palate deviation] IX, X, XI [Cranial portion]
question
Dorsal Motor Nucleus
answer
Sends autonomic [Parasympathetic] fibers to: 1. Heart 2. Lungs 3. Upper GI CN X
question
Cranial Nerve Reflex; Corneal
answer
AFFERENT: V1 [Ophthalmic nasociliary branch] EFFERENT: VII [Temporal branch, orbicularis oculi]
question
Cranial Nerve Reflex: Lacrimation
answer
AFFERENT: V1 [Loss of reflex does not preclude emotional tears] EFFERENT: VII
question
Jaw Jerk Reflex
answer
AFFERENT: V3 [Sensory - Muscle spindle from masseter] EFFERENT: V3 [Motor - Masseter]
question
Pupillary Reflex
answer
AFFERENT: CN II EFFERENT: CN III
question
Gag Reflex
answer
AFFERENT: CN IX EFFERENT: CN X
question
CN V Motor Lesion
answer
Jaw deviates TOWARD SIDE OF LESION, due to unopposed force from opposite pterygoid muscle
question
CN X Lesion
answer
Uvula deviates AWAY FROM SIDE OF LESION Weak side collapses and uvula points away
question
CN XI LEsion
answer
Weakness turning head to CONTRALATERAL side of lesion [SCM] Shoulder droop ON SIDE OF LESION [Trapezius] The left SCM contracts to help turn head to the right
question
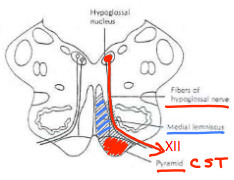
CN XII Lesion [LMN]
answer
Tongue deviates TOWARD SIDE of lesion [TONGUE LICKS THE LESION] due to weakened tongue muscles on affected side
question
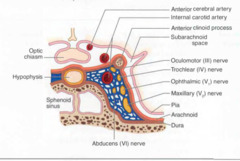
Cavernosus Sinus
answer
Collection of venous sinuses ON EITHER SIDE OF THE PITUITARY Blood from eye and superficial cortex ? Cavernous sinus ? Internal jugular vein 1. CN III. IV, V1, VI and occasionally V2 plus postganglionic sympathetic pupillary fibers en route to orbit all pass through the cavernous sinus 2. Nerves that control extraocular muscles V1 and V2 CAVERNOUS PORTION OF INTERNAL CAROTID ARTERY is also here
question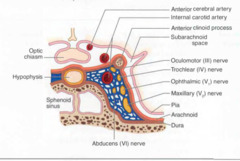
Cavernous Sinus Syndrome
answer
Present w/ 1. Variable ophthalmoplegia 2. ? Corneal sensation 3. Horner Syndrome 4. Occasional ? maxillary sensation 5. 2° pituitary mass effect 6. Carotid-cavernous fistula 7. Cavernous sinus thrombosis related to infection CN VI is most susceptible to injury
question
Outer Ear
answer
Visible portion of ear [Pinna], includes auditory canal and eardrum TRANSFERS sound waves via vibration of eardrum
question
Middle Ear
answer
AIR-FILLED SPACE with three bones called the ossicles 1. Malleus 2. Incus 3. Stapedius CONDUCT AND AMPLIFY SOUND from eardrum to inner ear
question
Inner Ear
answer
SNAIL-SHAPED, fluid-filled cochlea Contains basilar membrane that vibrates 2° to sound waves Vibrations are transduced via specialized hair cells ? Auditory nerve signaling ? brain stem Each frequency leads to a vibration at specific locations on the basilar membrane [Tonotopy] 1. Low frequency sounds heard at apex near helicotrema [Wide and flexible] 2. High frequency heard best at base of cochlea [Thin and rigid]
question
Conductive Hearing Loss
answer
Abnormal [Bone ; Air] = Localizes to affected ear
question
Sensorineural Hearing Loss
answer
Normal [Air ; Bone] = Localizes to unaffected ear
question
Noise induced
answer
Damage to STEREOCILIATED CELLS in ORGAN OF CORTI Loss of HIGH-FREQUENCY hearing 1st Sudden extremely loud noises can produce hearing loss due to TYMPANIC MEMBRANE RUPTURE
question
Cholesteatoma

answer
Overgrowth of DESQUAMATED KERATIN DEBRIS within MIDDLE EAR SPACE May erode ossicles, mastoid air cells ? CONDUCTIVE hearing loss
question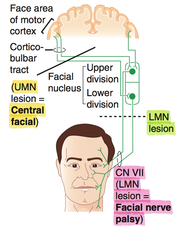
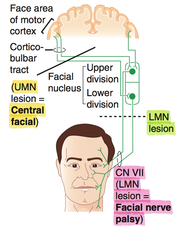
UMN Facial Lesion
answer
Lesion of the motor cortex or connection between cortex and facial nucleus Contralateral paralysis of lower face FOREHEAD SPARED DUE TO BILATERAL UMN LESION
question
LMN Facial Lesion
answer
IPSILATERAL paralysis of the upper and lower face
question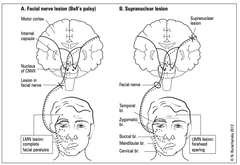
Facial Nerve Palsy
answer
Complete destruction of the facial nucleus itself or its branchial efferent fibers [Facial nerve proper] Peripheral ipsilateral facial paralysis [ABSENT FOREHEAD CREASES and DROOPING SMILE] with inability to close eye on involved side Can occur idiopathically [Bell's palsy], gradual recover in most cases Can be associated with: 1. Lyme Disease 2. Herpes Simplex [Less common] 3. Herpes Zoster [Ramsey Hunt Syndrome] 4. Sarcoidosis 5. Tumors 6. Diabetes TREAT W/ CORTICOSTEROIDS
question
Mastication muscles
answer
3 muscles close jaw [Masseter, Temporalis, Medial Pterygoid] 1 muscle opens [Lateral Pterygoid] All are innervated by CN V, V3 [Trigeminal nerve] M's Much L Lowers "It takes more to keep your mouth shut"
question
Refractive Errors
answer
Common cause of impaired vision, correctable with glasses
question
Hyperopia
answer
Eye too SHORT for refractive power of cornea and lens ? Light focused BEHIND RETINA
question
Myopia
answer
Eye too LONG for refractive power of cornea and lens ? Light focused in FRONT of the retina
question
Astigmatism
answer
Abnormal CURVATURE of the cornea ? Different refractive power at different axises
question
Presbyopia
answer
AGE-RELATED impaired ACCOMMODATION [Focusing on near objects] possibly due to ? LENS ELASTICITY Often necessitates reading glasses
question
Cataract
answer
Painless, OFTEN BILATERAL opacification of lens ? 1. ? Vision Risk factors: 1. ? Age 2. Smoking 3. Ethanol 4. Excessive sunlight 5. Prolonged CORTICOSTEROID USE 6. CLASSIC GALACTOSEMIA 7. GALACTOKINASE DEFICIENCY 8. Diabetes mellitus [Sorbitol] 9. Trauma 10. Infection
question
Glaucoma
answer
OPTIC DISK ATROPHY with characteristic CUPPING [Thinning of outer rim of optic nerve head] Usually w/ ? IOP [Intraocular pressure] and PROGRESSIVE PERIPHERAL FIELD LOSS
question
Open Angle
answer
Associated with: 1. ? Age 2. African American 3. Family hx PAINLESS, more common in US Primary = Cause unclear Secondary = BLOCKED TRABECULAR MESHWORK FROM WBCS [uveitis], RBCs [Vitreous hemorrhage], retinal elements [Retinal detachment]
question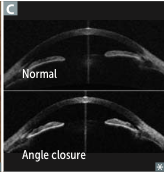
Closed/Narrow Angle
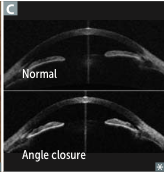
answer
Primary = ENLARGEMENT of FORWARD MOVEMENT OF LENS against central iris [Pupil margin] ? 1. OBSTRUCTION OF NORMAL AQUEOUS FLOW THROUGH THE PUPIL 2. Fluid builds up behind iris [Pushing peripheral iris against the cornea] 3. Impedes through through trabecular network Secondary = HYPOXIA from retinal disease [Diabetes mellitus, vein occlusion] -- Induces vasoproliferation in iris that contracts angle
question
Chronic Close/Narrow Angle Closure
answer
Often asymptomatic with damage to optic nerve and peripheral vision
question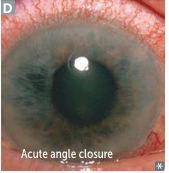
Acute Closed/Narrow Angle Closure
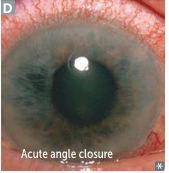
answer
TRUE OPHTHALMIC EMERGENCY ? IOP pushes iris forward = Angle closes abruptly 1. Very PAINFUL 2. RED EYE 3. SUDDEN VISION LOSS 4. HALOS around lights 5. Rock-hard eye 6. FRONTAL HEADACHE Do not given epinephrine b/c of its mydriatic effects
question
Uveitis
answer
Inflammation of the uvea [Anterior uveitis, choroiditis/posterior uveitis] May have 1. Hypopyon [Accumulation of pus in the anterior chamber] 2. Conjunctival redness Associated w/ systemic inflammatory disorders: 1. Sarcoidosis 2. RA 3. Juvenile idiopathic arthritis 4. HLA-B27-associated conditions
question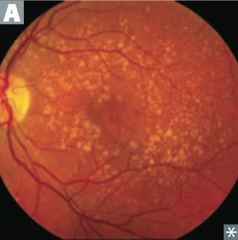
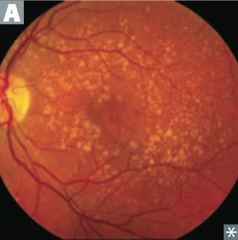
Age-Related Macular Degeneration
answer
Degeneration of macula [Central area of retina] Causes: 1. Distortion [Metamorphopsia] and eventual LOSS OF CENTRAL VISION [Scotomas] DRY [NONEXUDATIVE] 1. 80% of cases 2. Deposition of yellowish extracellular material in and beneath Bruch membrane and retinal pigment epithelium [Drusen] w/ gradual ? in vision 3. Prevent w/ MULTIVITAMIN and ANTIOXIDANT SUPPLEMENTS WET [Exudative] 1. 10-15% 2. Rapid vision loss due to bleeding 2° to choroidal neovascularization 3. Treat w/ anti-VEGF injections [Ranibizumab] or laser
question
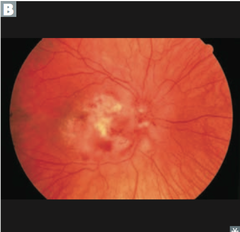
Diabetic Retinopathy
answer
RETINAL DAMAGE due to chronic hyperglycemia Two Types: 1. NONPROLIFERATIVE --. Damaged capillaries leak blood ? Lipids and fluids seep into retina -- Hemorrhages and macular edema -- Treatment - Blood-sugar control, macular laser 2. PROLIFERATIVE -- Chronic hypoxia ? New blood vessel formation with resultant traction on retina -- Treatment: Peripheral retinal photocoagulation, anti-VEGF [Bevacizumab]
question
Retinal Vein Occlusion
answer
Blockage of central or branch retinal vein due to COMPRESSION from nearby ARTERIAL ATHEROSCLEROSIS Retinal hemorrhages and venous engorgement Edema in affected areas
question
Retinal Detachment
answer
Separation of NEUROSENSORY layer of retina [Photoreceptor layer w/ RODS AND CONES] from outermost pigmented epithelium [Normally shields excess light, supports retina] Degeneration of photoreceptors ? Vision loss May be 2° to: 1. Retinal breaks 2. Diabetic traction 3. Inflammatory effusions Visualized on fundoscopy by the splaying and paucity of retinal vessels Correlation with cross-sectional optical ultrasound BREAKS MORE COMMON IN PATIENTS W/ HIGH MYOPIA -- Often preceded by posterior vitreous detachment [FLASHES and FLOATERS] and eventual monocular loss of vision LIKE A CURTAIN BEING DRAWN DOWN SURGICAL EMERGENCY
question
Central Retinal Artery Occlusion
answer
Acute, PAINLESS, monocular vision loss Retina CLOUDY with attenuated vessels and CHERRY RED spot on fovea [Center of macula]
question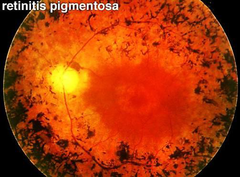
Retinitis Pigmentosa
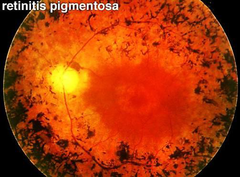
answer
INHERITED RETINAL DEGENERATION Painless, progressive, vision loss beginning w/ NIGHTBLINDNESS [Rods affected first] Bone spicule-shaped deposits around macula
question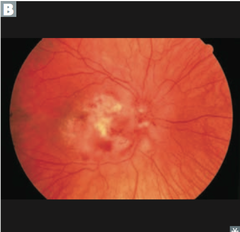
Retinitis
answer
Retinal edema and necrosis leading to scar OFTEN VIRAL [CMV, HSV, HZV] Associated w/ IMMUNOSUPPRESSION
question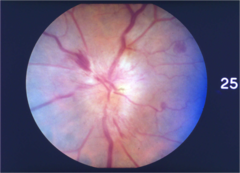
Papilledema
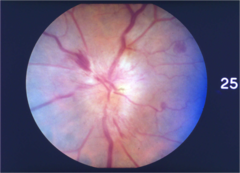
answer
Optic disk swelling [Usually BILATERAL] due to ? ICP [2° to mass effect] Enlarged BLIND SPOT and ELEVATED OPTIC DISC w/ BLURRED MARGINS
question
Miosis
answer
Constriction, PARASYMPATHETIC 1. 1st neuron = Edinger-Westphal nucleus to ciliary ganglion via CN III 2. 2nd neuron = Short ciliary nerves to pupillary sphincter muscles
question
Pupillary Light Reflex
answer
Light in either retina sends a signal via CN II to pretectal nuclei in MIDBRAIN that activates bilateral EDINGER-WESTPHAL NUCLEI Pupils constrict bilaterally [Consensual reflex] Resul: Illumination in one eye ? Bilateral pupillary constriction
question
Mydriasis
answer
DILATION, SYMPATHETIC 1st neuron: Hypothalamus to ciliospinal center of Budge [C8-T2] 2nd neuron: Exit at T1 to superior cervical ganglion [Travels along the cervical sympathetic chain near lung apex, subclavian vessels] 3rd neuron = Plexus along internal carotid, through cavernous sinus, enter orbit as LONG CILIARY NERVE to pupillary dilator muscles SYMPATHETIC fibers also innervate SMOOTH MUSCLE OF EYELID [Minor retractors] and SWEAT GLANDS OF FOREHEAD AND FACE
question
Marcus Gunn Pupil
answer
AFFERENT pupillary defect Due to OPTIC NERVE DAMAGE or SEVERE RETINAL INJURY ? Bilateral pupillary constriction when light is shone in the eye relative to unaffected Test w/ SWINGING FLASHLIGHT TEST
question
Horner Syndrome
answer
SYMPATHETIC DENERVATION OF FACE 1. Ptosis [Slight drooping of eyelid = Superior tarsal muscle] 2. Anhidrosis [Absence of sweating] and flushing [Rubor] of affected side of face 3. Miosis [Pupil constriction] Associated w/ lesion of spinal cord ABOVE T1 1. Pancoast tumor 2. Brown-Sequard syndrome [Cord hemisection] 3. Late stage syringomyelia ANY INTERRUPTION RESULTS IN HORNERS PAM is Horny
question
CN VI
answer
Lateral Rectus
question
CN IV
answer
Superior oblique LR6SO4 Abducts, intorts, and depresses while abducted
question
CN III
answer
Innervates all eye muscles except [LR, SO]
question
Obliques
answer
go OPPOSITE [Left SO and IO tested with patients looking to the right] IOU: IO tested looking up
question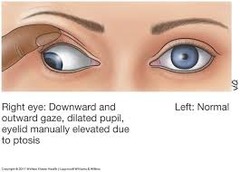
CN III Damage
answer
CN III has both motor [Central] and parasympathetic [Peripheral] components Motor output to ocular muscles = Affected primarily by VASCULAR DISEASE [Diabetes mellitus: Glucose ? Sorbitol] -- Due to ? diffusion of oxygen and nutrients to interior fibers from compromised vasculature that resides on outside of nerves DOWN AND OUT Parasympathetic output = Fibers on periphery are 1st affected by compression [PICA aneurysm, uncal herniation] -- Diminished or absent pupillary reflex -- Blown pupil often w/ down and out gaze
question
CN IV Damage

answer
Eyes move upward, particularly with CONTRALATERAL gaze HEAD TILT TOWARD SIDE OF LESION Problems going down stairs, may present w/ compensatory head tilt in opposite direction
question
CN VI Damage

answer
MEDIALLY directed eye that cannot abduct
question
Visual Field Defects: Bitemporal hemianopsia
answer
Pituitary lesion, chiasm
question
Visual Field Defects: Left upper quadrant anopia
answer
Right temporal lesion, MCA
question
Visual Field Defects: Left lower quadrant anopia
answer
Right parietal lesion, MCA
question
Visual Field Defects: Left hemianopia w/ macular sparing
answer
PCA infarct
question
Visual Field Defects: Central scotoma
answer
Macular degeneration
question
Meyer Loop
answer
Inferior retina, loops around inferior horn of lateral ventricle
question
Dorsal Optic Radiation
answer
Superior retina, takes SHORTEST PATH via INTERNAL CAPSULE
question
When an image hits the 1° Visual cortex, it is
answer
Upside down, left-right reversed
question
Internuclear Ophthalmoplegia
answer
Medial longitudinal fasciculus [MLF] = Pair of tracts that allow for crosstalk between CN VI and CN III nuclei Coordinates both eyes to move in the same horizontal direction HIGHLY MYELINATED [Must communicated quickly to move at the same time] Lesions may be unilateral or bilateral [Seen in MS]
question
Lesion in MLF
answer
Internuclear ophthalmoplegia [INO] results in conjugate horizontal gaze palsy Lack of communication does not stimulate CN III to stimulate medial rectus to fire when CN VI nucleus activates Abducting eye gets NYSTAGMUS [CN VI overfires to stimulate CN III] CONVERGENCE NORMAL Direction term [right INO, left INO] refers to which eye is paralyzed
question
Alzheimer Disease
answer
Most common cause of DEMENTIA in elderly DOWN SYNDROME patients have ? risk of developing Alzheimer's [Typically before age 40] Familial Form [10%] associated with: 1. ApoE2 ? risk 2. ApoE4 ? risk 3. APP, presenilin-1, presenilin-2, = ? Risk of early onset WIDESPREAD CORTICAL ATROPHY -- Narrowing of gyri, widening of sulci -- ? ACh SENILE PLAQUES IN GRAY MATTER = Extracellular B-amyloid core [May cause amyloid angiopathy ? intracranial hemorrhage] AB [Amyloid B] synthesized by cleaving amyloid precursor APP NEUROFIBRILLARY TANGLE = Intracellular, hyperphosphorylated tau protein INSOLUBLE cytoskeletal elements NUMBER OF TANGLES CORRELATED w/ DEGREE OF DEMENTIA
question
Dementia
answer
A ? in cognitive ability, memory, or function with intact conciousness
question![Frontotemporal Dementia [Pick Disease] Frontotemporal Dementia [Pick Disease]](https://studyhippo.com/wp-content/uploads/2018/04/frontotemporal-dementia-pick-disease.png)
Frontotemporal Dementia [Pick Disease]
![Frontotemporal Dementia [Pick Disease] Frontotemporal Dementia [Pick Disease]](https://studyhippo.com/wp-content/uploads/2018/04/frontotemporal-dementia-pick-disease.png)
answer
Clinical Manifestations: 1. Dementia 2. Aphasia 3. Parkinsonian effects 4. Change in personality SPARES PARIETAL LOBE and POSTERIOR 2/3 of superior temporal gyrus PICK BODIES = Silver staining spherical tau protein aggregates
question
Lewy Body Dementia
answer
Initially dementia and hallucinations [haLEWYcinations] followed by parkinsonian features a-synuclein defect [Lewy bodies primarily cortical]
question
Creutzfeldt Jakob Disease
answer
Rapidly progressive [Weeks to months] dementia with MYOCLONUS Spongiform cortex [Associated w/ prions] Prions [PrPc ? PrPsc] B-pleated sheet are resistant to proteases
question
Multi-infarct Dementia [Vascular dementia]
answer
2nd most common cause of DEMENTIA IN ELDERLY
question
Other Causes of Dementia
answer
1. Syphilis 2. HIV [Associated w/ foamy macrophages and multinucleated giant cells, prominent endothelial cells] 3. Vitamins B1, B3, or B12 deficiency 4. Wilson disease 5. Normal pressure hydrocephalus [Wet, Wacky, Wobbly]
question
Multiple Sclerosis
answer
AUTOIMMUNE INFLAMMATION and DEMYELINATION of CNS [Brain and spinal cord] Patients can present with: 1. Optic neuritis [Sudden loss of vision resulting in Marcus Gun pupil] 2. INO 3. Hemiparesis 4. Hemisensory symptoms 5. BLADDER AND BOWEL INCONTINENCE Relapsing and remitting course Most often affects women in their 20-30s Charcot Classic Triad [SIN]: 1. Scanning speech 2. Intention tremor [Also Incontinence and INO] 3. Nystagmus
question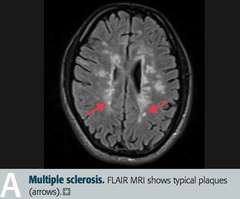
Findings in MS
answer
1. ? Protein [IgG] in CSF 2. Oligoclonal bands are diagnostic 3. MRI is gold standard 4. PERIVENTRICULAR PLAQUES [Areas of oligodendrocyte loss and reactive gliosis] with destruction of axons 5. Multiple white matter lesions separated in time and space
question
Treatment
answer
Slow progression of disease with DMARDs [B-interferon, natalizumab] Treat acute flares w/ IV STEROID Symptomatic treatment for Neurogenic bladder: 1. Catheterization 2. Muscarinic antagonists SPASTICITY 1. Baclofen 2. GABAB receptor agonist PAIN = OPIOIDS
question
Acute Inflammatory Demyelinating Polyradiculopathy
answer
Common common subtype of GUILLIAN BARRE Autoimmune condition that destroys SCHWANN CELLS ? Inflammation and demyelination of peripheral nerves and motor fibers SYMMETRIC ASCENDING muscle weakness/paralysis beginning in lower extremities FACIAL paralysis [50% of cases] May see autonomic dysregulation: 1. Cardiac irregularities 2. Hypertension or hypotension 3. Sensory abnormalities Almost all patients survive, majority recover completely after weeks to months Findings: 1. ? CSF protein with NORMAL CELL COUNT [Albuminocytologic dissociation] 2. ? Protein may cause papilledema Associated with: 1. Campylobacter jejuni infection [Autoimmune attack of peripheral myelin due to MOLECULAR MIMICRY and STRESS] RESPIRATORY SUPPORT IS CRITICAL UNTIL RECOVERY Treatment: 1. Plasmapheresis 2. IV Immunoglobulins
question
Acute Disseminated [Postinfectious] Encephalomyelitis
answer
Multifocal PERIVENTRICULAR inflammation and demyelination after infection [Measles, VZV] or vaccinations [Rabies, smallpox]
question
Charcot-Marie-Tooth
answer
Hereditary Motor and Sensory Neuropathy [HMSN] Group of progressive disorders related to: 1. Defective production of proteins involved in structure and function of peripheral nerves or the myelin sheath AUTOSOMAL DOMINANT Associated with: 1. Scoliosis 2. Foot deformities [High or flat arches]
question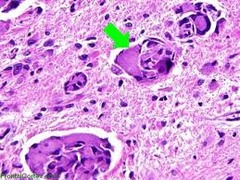
Krabbe Disease
answer
AUTOSOMAL RECESSIVE LYSOSOMAL STORAGE DISEASE Due to deficiency of GALACTOCEREBROSIDASE Buildup of galactocerebroside and psychosine destroys myelin Findings: 1. Peripheral neuropathy 2. Developmental delay 3. Optic atrophy 4. GLOBOID CELLS
question
Metachromatic Leukodystrophy
answer
AUTOSOMAL RECESSIVE LYSOSOMAL STORAGE DISEASE Most commonly due to ARYLSULFATASE A deficiency Buildup of sulfatides ? Impaired production and destruction of myelin sheath Findings: 1. Central and peripheral demyelination 2. Ataxia 3. Dementia
question
Progressive Multifocal Leukoencephalopathy
answer
Demyelination of CNS due to DESTRUCTION OF OLIGODENDROCYTES Associated w/ JC virus Seen in 2-4% of AIDS patients [Reactivation of latent virus] Rapidly progressive, usually fatal ? Risk associated w/ Natalizumab, Rituximab
question
Adrenoleukodystrophy
answer
X-LINKED genetic disorder Typically affecting MALES Disrupts metabolism of VERY LONG CHAIN FATTY ACIDS ? 1. Excessive build-up in CNS, adrenal glands, testes 2. Progressive disease that can lead to long-term coma/death 3. ADRENAL GLAND CRISIS
question
Seizures
answer
Characterized by synchronized, high-frequency neuronal firing. Variety of forms
question
Partial [Focal] Seizure
answer
AFFECTS SINGLE AREA OF BRAIN Most commonly in MEDIAL TEMPORAL LOBE Often preceded by seizure AURA, can secondarily generalize
question
Simple Partial Seizure
answer
Consciousness intact Motor, sensory, autonomic, psychic
question
Complex Partial Seizure
answer
Impaired Consciousness
question
Generalized Absence Seizure [Petit mal]
answer
3 Hz, NO POSTICTAL confusion, blank stare
question
Generalized Myoclonic Seizure
answer
Quick, repetitive jerks
question
Generalized Tonic-Clonic Seizure [Grand Mal]
answer
Alternating stiffening and movement
question
Generalized Tonic Seizure
answer
Stiffening
question
Generalized Atonic Seizures
answer
Drop seizures [Falls to floor], commonly mistaken for fainting Typically starts in childhood [6 months - 5 years]
question
Epilepsy
answer
Disorder of recurrent seizures [Febrile seizures are not epilepsy]
question
Status epilepticus
answer
Continuous or recurring seizures that may result in brain injury Variably defined as > 10-30 minutes
question
Causes of Seizure by Age 1. Children 2. Adults 3. Elderly
answer
CHILDREN 1. Genetic 2. Infection [Febrile] 3. Trauma 4. Congenital 5. Metabolic ADULTS 1. Tumor 2. Trauma 3. Stroke 4. Infarction ELDERLY 1. Stroke 2. Tumor 3. Trauma 4. Metabolic 5. Infection
question
Cluster Headache
answer
Unilateral Duration: 15 min- 3 hours, repetitive REPETITIVE BRIEF HEADACHES Excruciating, PERIORBITAL pain w/ LACRIMATION and RHINORRHEA May induce horner's syndrome More common in MALES Treatment: 100% O2
question
Tension Headache
answer
BILATERAL Duration: ; 30 minutes [Typically 4-6 hours], Constant STEADY PAIN Treatment: Analgesics, NSAIDs, Acetaminophen, Amitriptyline for chronic pain
question
Migraine
answer
Unilateral Duration: 4-72 hours Clinical Manifestation [POUND] 1. Pounding/Pulsatile 2. One-day duration 3. Unilateral 4. Nausea and vomiting 5. Disabling 6. PHOTOPHOBIA or PHONOPHOBIA 7. May have aura Due to irritation of CN V, meninges, blood vessels [Release of substance P, calcitonin gene-related peptide, vasoactive peptide] Treatment: 1. Abortive therapies [Triptans, NSAIDs] 2. Prophylaxis [Propranolol, Topiramate, Ca2+ channel blockers]
question
Other causes of headaches:
answer
1. Subarachnoid Hemorrhage 2. Meningitis 3. Hydrocephalus 4. Neoplasia 5. Arteritis
question
Trigeminal Neuralgia
answer
REPETITIVE SHOOTING PAIN in the distribution of CN V Typically lasts for ; 1 minute
question
Vertigo
answer
Sensation of spinning while actually stationary Subtype of dizziness, but distinct from light-headedness
question
Peripheral vertigo
answer
MORE COMMON INNER EAR ETIOLOGY 1. Semicircular debris 2. Vestibular nerve infection 3. Meniere Disease Positional testing ? DELAYED HORIZONTAL NYSTAGMUS
question
Central vertigo
answer
BRAIN STEM or CEREBELLAR lesion STROKE affecting VESTIBULAR or POSTERIOR FOSSA TUMOR Findings: 1. Direction change of nystagmus 2. Skew deviation 3. Diplopia 4. Dysmetria Positional testing ? Immediate nystagmus in any direction, may change directions FOCAL NEUROLOGIC FINDINGS
question
Sturge-Weber Syndrome

answer
Congenital, non-inherited [Somatic] developmental anomaly of NEURAL CREST DERIVATIVES [Mesoderm/Ectoderm] 1. Due to activating mutation of GNAQ 2. Affects small [Capillary-sized] blood vessels ? Port wine stain of face 2. Nevus flammeus = Non-neoplastic birthmark in CN V1/V2 distribution 3. Ipsilateral leptomeningeal angioma 4. Seizures/epilepsy 5. Intellectual disability 6. Episcleral hemangioma 7. ? IOP ? Early onset GLAUCOMA STURGE-Weber 1. Sporadic, port-wine stain 2. Tram track calcifications 3. Unilateral 4. Retardation [Intellectual disability] 5. Glaucoma, GNAQ 6. Epilepsy
question
Tuberous Sclerosis

answer
HAMARTOMAS 1. Hamartomas in CNS 2. Angiofibromas 3. MITRAL REGURGITATION 4. Ash-leaf spots 5. Cardiac RHABDOMYOMA 6. Autosomal dOminant 7. Mental retardation [Intellectual disability] 8. Renal Angiomyolipoma 9. Seizures, Shagreen patches ? Incidence in subependymal astrocytomas and ungual fibromas
question![Neurofibromatosis Type I [Von Recklinghausen Disease] Neurofibromatosis Type I [Von Recklinghausen Disease]](https://studyhippo.com/wp-content/uploads/2018/04/neurofibromatosis-type-i-von-recklinghausen-disease.png)
Neurofibromatosis Type I [Von Recklinghausen Disease]
![Neurofibromatosis Type I [Von Recklinghausen Disease] Neurofibromatosis Type I [Von Recklinghausen Disease]](https://studyhippo.com/wp-content/uploads/2018/04/neurofibromatosis-type-i-von-recklinghausen-disease.png)
answer
1. Cafe-au-lait spots 2. Lisch nodules [Pigmented iris hamartomas] 3. Cutaneous neurofibromas 4. Optic gliomas 5. Pheochromocytomas Mutated NF1 TUMOR SUPPRESSOR GENE [Neurofibromin = Negative regulator of RAS] on chromosome 17 Skin tumors of NF-1 are derived from neural crest cells
question
von Hippel-Lindau Disease
answer
X-Linked Recessive HEMANGIOBLASTOMAS [High vascularity w/ HYPERCHROMATIC NUCLEI] in: 1. Retina 2. Brainstem 3. Cerebellum 4. Spine Angiomatosis = Cavernous hemangiomas in skin, mucosa, organs BILATERAL RENAL CELL CARCINOMAS Pheochromocytomas
question![Glioblastoma Multiforme [Grade IV Astrocytoma] Glioblastoma Multiforme [Grade IV Astrocytoma]](https://studyhippo.com/wp-content/uploads/2018/04/glioblastoma-multiforme-grade-iv-astrocytoma.png)
Glioblastoma Multiforme [Grade IV Astrocytoma]
![Glioblastoma Multiforme [Grade IV Astrocytoma] Glioblastoma Multiforme [Grade IV Astrocytoma]](https://studyhippo.com/wp-content/uploads/2018/04/glioblastoma-multiforme-grade-iv-astrocytoma.png)
answer
Common, HIGHLY MALIGNANT 1° brain tumor with ~ 1 year survival Found in CEREBRAL HEMISPHERES CAN CROSS CORPUS CALLOSUM [Butterfly glioma] Stain astrocytes for GFAP Histology: 1. Pseudopalisading 2. Pleomorphic tumor cells 3. Border CENTRAL AREAS OF NECROSIS and hemorrhage
question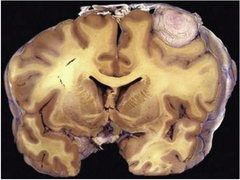
Meningioma
answer
Common, typically BENIGN 1° brain tumor Most often occurs in CONVEXITIES of hemispheres near surfaces of the brain and PARASAGITTAL SINUS Arises from ARACHNOID CELLs EXTRA-AXIAL [External to brain parenchyma] May have a DURAL ATTACHMENT [Tail] Often asymptomatic, may present w/: 1. Seizures 2. Focal neurologic signs Treatment = Resection or radiosurgery Histology: 1. SPINDLE cells concentrically arranged in WHORLED PATTERN 2. PSAMMOMA BODIES [Laminated calcifications]
question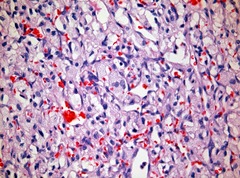
Hemangioblastoma
answer
Most often CEREBELLAR Associated w/ von-Hippel-Lindau syndrome Found with RETINAL ANGIOMAS Can produce ERYTHROPOIETIN ? 2° Polycythemia Histology: 1. Closely arranged, thin-walled capillaries with minimally intervening parenchyma
question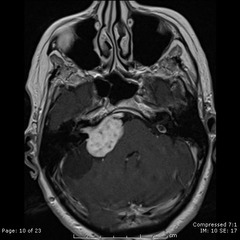
Schwannoma
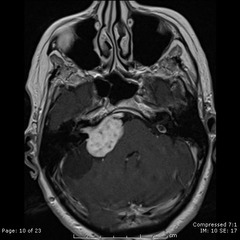
answer
Classically at CEREBELLOPONTINE ANGLE, but can be anywhere along peripheral nerve Schwann cell origin [S-100] Often LOCALIZED TO CN VIII ? Vestibular schwannoma Resectable or treatable w/ stereotactic radiosurgery BILATERAL VESTIBULAR SCHWANNOMA = NF2
question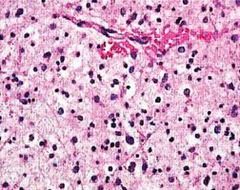
Oligodendroglioma
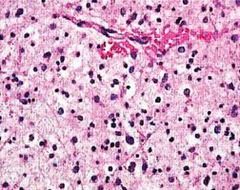
answer
Relatively rare, slow growing Most often in FRONTAL LOBES CHICKEN-WIRE capillary pattern Histology: 1. Oligodendrocytes = FRIED EGG cells [Round nuclei with clear cytoplasm] OFTEN CALCIFIED
question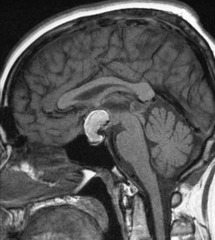
Pituitary Adenoma
answer
Most commonly prolactinoma Bitemporal hemianopia [Normal visual fields above] due to pressure on the Optic Chiasm
question![Pilocytic [Low-Grade] Astrocytoma Pilocytic [Low-Grade] Astrocytoma](https://studyhippo.com/wp-content/uploads/2018/04/pilocytic-low-grade-astrocytoma.png)
Pilocytic [Low-Grade] Astrocytoma
![Pilocytic [Low-Grade] Astrocytoma Pilocytic [Low-Grade] Astrocytoma](https://studyhippo.com/wp-content/uploads/2018/04/pilocytic-low-grade-astrocytoma.png)
answer
Usually well-circumscribed In CHILDREN Found in the POSTERIOR FOSSA [Cerebellum] May be supratentorial GFAP + Benign, good prognosis ROSENTHAL FIBERS = Eosinophilic, corkscrew fibers CYSTIC + SOLID
question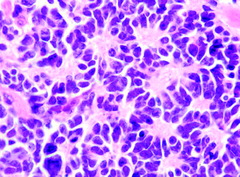
Medulloblastoma
answer
HIGHLY MALIGNANT CEREBELLAR tumor A form of primitive NEUROECTODERM Can compress 4th ventricle causing hydrocephalus Can send DROP METASTASES to spinal cord HOMER-WRIGHT ROSETTE Solid, SMALL BLUE CELLS
question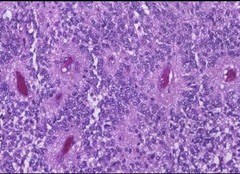
Ependymoma
answer
Ependymal cells most commonly found in the 4th ventricle Can cause hydrocephalus POOR PROGNOSIS Characteristic perivascular rosettes Rod-Shaped Blepharoplasts [Basal ciliary bodies] found near nucleus
question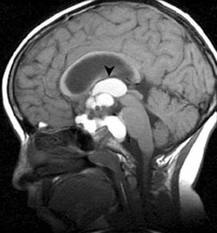
Craniopharyngioma
answer
Benign CHILDHOOD tumor Can cause bitemporal hemianopia MOST COMMON CHILDHOOD SUPRATENTORIAL tumor Derived from remnants of Rathke's pouch Calcification common
question![Cingulate [Subfalcine] Herniation under Falx Cerebri Cingulate [Subfalcine] Herniation under Falx Cerebri](https://studyhippo.com/wp-content/uploads/2018/04/cingulate-subfalcine-herniation-under-falx-cerebri.png)
Cingulate [Subfalcine] Herniation under Falx Cerebri
![Cingulate [Subfalcine] Herniation under Falx Cerebri Cingulate [Subfalcine] Herniation under Falx Cerebri](https://studyhippo.com/wp-content/uploads/2018/04/cingulate-subfalcine-herniation-under-falx-cerebri.png)
answer
Can compress anterior cerebral artery
question![Downward Transtentorial [Central] Herniation Downward Transtentorial [Central] Herniation](https://studyhippo.com/wp-content/uploads/2018/04/downward-transtentorial-central-herniation.png)
Downward Transtentorial [Central] Herniation
![Downward Transtentorial [Central] Herniation Downward Transtentorial [Central] Herniation](https://studyhippo.com/wp-content/uploads/2018/04/downward-transtentorial-central-herniation.png)
answer
Caudal displacement of brain stem ? Rupture of PARAMEDIAN BASILAR ARTERY BRANCHES ? Duret's hemorrahges
question
Uncal Herniation
answer
Uncus = Medial Temporal lobe 1. Compresses Ipsilateral CN III [Blown pupil, down and out] 2. Ipsilateral PCA [Contralateral homonymous hemianopia] 3. Contralateral Crus cerebri at the Kernohan notch [Ipsilateral paresis = False localization sign]
question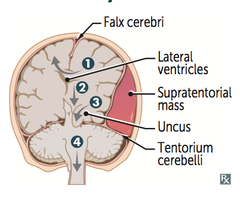
Cerebellar Tonsillar Herniation into the Foramen Magnum
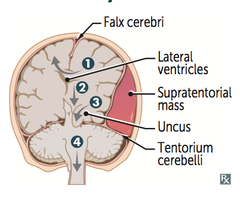
answer
Coma and death result when the herniations compress the brain stem
question
Glaucoma Drugs
answer
? IOP via ? Amount of aqueous humor [Inhibits synthesis/secretion of ? drainage]
question
a-agonists
answer
Drugs: Epinephrine [a1], Brimonidine [a2] MOA: 1. ? Aqueous humor synthesis via vasoconstriction 2. ? Aqueous humor synthesis Side Effects: 1. Mydriasis [a1] = Do not use in CLOSED-ANGLE glaucoma 2. Blurry vision 3. Ocular hyperemia 4. Foreign body sensation 5. Ocular allergic rxns 6. Ocular pruritus
question
B-blockers
answer
Timolol, Betaxolol, Carteolol MOA: ? Aqueous humor synthesis
question
Acetazolamide
answer
MOA: ? Aqueous humor synthesis via inhibition of carbonic anhydrase
question
Direct Cholinomimetics [Pilocarpine, Carbachol] Indirect Cholinomimetics [Physostigmine, Echothiophate]
answer
MOA: ? Outflow of aqueous humor via CONTRACTION OF CILIARY MUSCLE and OPENING OF TRABECULAR NETWORK Use pilocarpine in emergencies = Very effective at opening meshwork into canal of Schlemm Adverse Effects: Miosis and cytoplasm [Contraction of ciliary muscle]
question
Latanoprost [PGF2a]
answer
? Outflow of aqueous humor Adverse Effect: Darkens color of iris [Browning]
question
Opioid Analgesics
answer
Drugs: Morphine, Fentanyl, Codeine, Loperamide, Methadone, Meperidine, Dextromethorphan, Diphenoxylate, Pentazocine MOA: Acts as agonists at opioid receptors [? = Morphine, ? = Enkephalin, ? = dynorphin] to modulate synaptic transmission Opens K+ channels, closes Ca2+ channels ? ? Synaptic transmission Inhibits release of 1. ACh 2. Norepinephrine 3. 5-HT 4. Glutamate 5. Substance P
question
Clinical Use of Opioids
answer
1. Pain 2. Cough suppression [Dextromethorphan] 3. Diarrhea [Loperamide, diphenoxylate] 4. Acute pulmonary edema 5. Maintenance programs for heroin addicts [Methadone, buprenorphine + Naloxone]
question
Toxicity of Opioids
answer
1. Addiction 2. Respiratory depression 3. Constipation 4. Miosis [Pinpoint pupils] 5. Addictive 6. CNS depression w/ other drugs TOLERANCE DOES NOT DEVELOP TO MIOSIS AND CONSTIPATION Toxicity treated w/ Naloxone or Naltrexone [Opioid receptor antagonist]
question
Butorphanol
answer
MOA: ?-opioid receptor agonist and ? partial agonist Produces analgesia Clinical Use: 1. Severe pain [Migraine, labor] 2. Causes less respiratory depression than full opioid agonists Adverse Effects: 1. Can cause opioid withdrawal symptoms if a patient is also taking full opioid agonist [Competition for opioid receptors] 2. Overdose not easily reversed with naloxone
question
Tramadol
answer
MOA: Very weak opioid agonist Also inhibits 5-HT and Norepi REUPTAKE [Works on multiple neurotransmitters -Tram it all w/ TRAMADOL] Clinical Use: 1. Chronic pain Toxicity: 1. Similar to opioid 2. DECREASES SEIZURE THRESHOLD 3. SEROTONIN SYNDROME
question
Ethosuximide [Epilepsy]
answer
ABSENCE SEIZURES MOA: Blocks thalamic T-Type Ca2+ Channels Side Effects [EFGHIJ]: 1. Fatigue 2. GI upset 3. Headache 4. Itching 5. SJS
question
Benzodiazepines [Epilepsy]
answer
FIRST LINE TREATMENT IN STATUS EPILEPTICUS 1. Diazepam, Lorazepam, Clonazepam MOA: ? GABAA action Side effects 1. Sedation 2. Tolerance 3. Dependence 4. Respiratory depression and hypotension
question
Phenytoin, Fosphenytoin [Parenteral]
answer
MOA: ? Na channel inactivation, zero order kinetics Side Effects: 1. Nystagmus, diplopia 2. Ataxia 3. Sedation 4. GINGIVAL HYPERPLASIA 5. Hirsutism 6. Peripheral neuropathy 5. MEGALOBLASTIC ANEMIA 6. Teratogenic [Fetal hydantoin syndrome] 7. SJS 8. Osteopenia
question
Carbamazepine [Epileptic]
answer
1st LINE FOR TRIGEMINAL NEURALGIA MOA: ? Na channel inactivation, potentiates K+ efflux Side Effects: 1. Diplopia 2. Ataxia 3. Blood dyscrasias [AGRANULOCYTOSIS, APLASTIC ANEMIA] 4. Liver toxicity 5. SIADH 7. SJS 8. Osteopenia
question
Valproic acid [Epileptic]
answer
USED FOR MYOCLONIC SEIZURES, BIPOLAR DISORDER MOA: ? Na channel inactivation, ? GABA concentration by inhibiting GABA transaminase Side Effects: 1. FATAL hepatotoxicity [Check LFTs] 2. Neural tube defects [Spina bifida] 3. Tremor 4. Weight gain 5. Contraindicated in pregnancy
question
Gabapentin [Epileptic]
answer
MOA: Primarily inhibits high-voltage-activated Ca2+ channels, designed as GABA analog Side Effects: 1. Sedation 2. Ataxia
question
Phenobarbital [Epileptic]
answer
FIRST LINE IN NEONATES MOA: ? GABAA action Side Effects: 1. Sedation 2. Tolerance 3. Dependence 4. Cardiorespiratory depression
question
Topiramate [Epileptic]
answer
Also used for migraine prevention MOA: Blocks Na channels, ? GABA action Side Effects: 1. Sedation 2. Mental dulling 3. Kidney stones 4. Weight loss
question
Lamotrigine [Epileptic]
answer
MOA: Blocks voltage-gated Na channels, blocks glutamate release Side Effects: 1. SJS
question
Levetiracetam [Epileptic]
answer
MOA: Unknown, may modulate GABA and glutamate release
question
Tiagabine [Epileptic]
answer
MOA: ? GABA by inhibiting reuptake
question
Vigabatrin [Epileptic]
answer
MOA: ? GABA by irreversibly inhibiting GABA Transaminase
question
SJS
answer
Prodrome of fever, malaise followed by rapid onset of erythematous/pruritic macules [Oral, ocular, genital]. Skin lesions progress to epidermal necrosis and sloughing
question
Barbiturates
answer
Drugs: Phenobarbital, Pentobarbital, Thiopental, Secobarbital MOA: Facilitate GABAA action by ? DURATION of Cl- channel opening ? ? Neuron firing CONTRAINDICATED IN PORPHYRIA Clinical Use: 1. Sedative for anxiety 2. Seizures 3. Insomnia 4. Induction of anesthesia [Thiopental] Adverse Effects: 1. Respiratory and cardiovascular depression [Can be fatal] 2. CNS depression [Can be exacerbated by EtOH use] 3. Dependence 4. Drug interactions [Induces CYP450] Treatment of OD = Supportive [Assist respirations, maintain BP]
question
Benzodiazepines
answer
Drugs: Diazepam, lorazepam [Anticonvulsants], Triazolam [Insomnia], Temazepam, Oxazepam, Midazolam, Chlordiazepoxide, Alprazolam MOA: Facilitate GABAA action by ? FREQUENCY of Cl- channel opening ? REM sleep Most have long half-lives and active metabolites, exceptions [ATOM = High addictive potential]: 1. Alprazolam 2. Triazolam 3. Oxazepam 4. Midazolam
question
What binds GABAA
answer
Benzos, Barbs, EtOH
question
Clinical Use of Benzodiazepines
answer
1. Anxiety 2. Spasticity 3. Status epilepticus [Diazepam, Lorazepam] 4. Detoxification [Especially alcohol withdrawal] 5. Night terrors, sleepwalking 6. General anesthetic [Amnesia, muscle relaxant] 7. Hypnotic [Insomnia]
question
Benzodiazepine Toxicity
answer
1. Dependence 2. Addictive CNS depression effects w/ alcohol 3. Less risk of respiratory depression and coma than with barbiturates Treat overdose with: Flumazenil [Competitive antagonist at GABA benzodiazepine receptor]
question
Nonbenzodiazepine Hypnotics
answer
Drugs: Zolpidem, Zaleplon, eZopiclone [All ZZZs put you to sleep] MOA: Act via the BZI subtype of GABA receptor Effects reversed by Flumazenil Clinical use: 1. Insomnia Adverse Effects: 1. Ataxia 2. Headaches 3. Confusion Short duration because of rapid metabolism by liver enzymes. Unlike older sedative-hypnotics, cause only modest day-after psychomotor depression and a few amnestic effects ? Dependence risk compared to benzos
question
Anesthetics - General Principles
answer
1. CNS drugs must be lipid soluble [Cross the BBB] or be actively transported 2. Drugs w/ ? solubility in blood = Rapid induction and recovery time 3. Drugs w/ ? solubility in lipid = ? Potency = 1/MAC
question
Minimal Alveolar Concentration [MAC]
answer
Inhaled anesthetic = Required to prevent 50% of subjects from moving in response to noxious stimulant [skin incision] Examples: Nitric oxide [N2O] has ? solubility in blood and ? lipid solubility = Fast induction and low potency Halothane = ? Lipid and blood solubility, high potency and slow induction
question
Inhaled anesthetics
answer
Drugs: Halothane, enflurane, isoflurane, sevoflurane, methoxyflurane, N2O Effects: 1. Myocardial depression 2. Respiratory depression 3. Nausea/emesis 4. ? Cerebral blood flow [? Cerebral metabolic demand] Adverse Effects: 1. Hepatotoxicity [Halothane] 2. Nephrotoxicity [Methoxyflurane] 3. Proconvulsant [Enflurane] 34. Expansion of trapped gas in the body [N2O]
question
Malignant Hyperthermia
answer
Rare. life-threatening hereditary condition in which inhaled anesthetics [N2O] and succinylcholine induce FEVER and SEVERE MUSCLE CONTRACTIONS Treatment = Dantrolene
question
Intravenous Anesthetics: Barbiturates
answer
Thiopental HIGH POTENCY, HIGH SOLUBILITY Rapid re-entry into brain Used for induction of anesthesia and short surgical procedures Effect terminated by rapid redistribution into tissue [skeletal muscle] and fat ? Cerebral flow
question
Intravenous Anesthetics: Benzodiazepines
answer
Midazolam most commonly used for ENDOSCOPY Used adjunctively with gaseous anesthetics and narcotics May cause SEVERE POST-OPERATIVE RESPIRATORY DEPRESSION ANTEROGRADE AMNESIA ? BlP Treat OD: Flumazenil
question
Arylcyclohexylamines [Ketamine]
answer
PCP analogs that act as dissociated anesthetics Block NMDA receptors CARDIOVASCULAR STIMULANTS Cause: 1. Disorientation 2. Hallucination 3. Bad dream 4. ? Cerebral blood flow
question
Opioids
answer
Morphine, fentanyl Used with other CNS depressants during general anesthesia
question
Propofol
answer
Used for sedation in the ICU, rapid anesthesia induction, short procedures LESS POST-OPERATIVE NAUSEA than thiopental Potentiates GABAA
question
Local Anesthetics
answer
Esters = Procaine, cocaine, tetracaine Amides = Lidocaine, Mepivacaine, Bupivacaine [Amides have two I's] MOA: Binds Na+ channels by binding to specific receptor on inner portion of channel Preferentially binds to ACTIVATED NA+ CHANNELS [Most effective in firing neurons] 3° amine local anesthetics penetrate membrane in uncharged form, then bind to ion channels as charged form
question
Principle of Local Anesthetics
answer
Can be given with vasoconstrictors [Usually epinephrine] to enhance local action ? ? Bleeding, ? anesthesia by ? systemic concentration In infected [Acidic] tissue ALKALINE anesthetics are CHARGED and CANNOT PENETRATE MEMBRANE effectively ? Need more anesthetic
question
Order of Nerve Blockade for Local Anesthetics
answer
Small-diameter > Large Diameter Myelinated fibers > Unmyelinated fibers SIZE PREDOMINATES OVER MYELINATION such that small myelinated fibers > small unmyelinated fibers > large myelinated fibers > large unmyelinated fibers Order of Loss: 1. Pain 2. Temperature 3. Touch 4. Pressure
question
Toxicity of Local Anesthetics
answer
1. CNS excitation 2. Severe cardiovascular toxicity [Bupivacaine] 3. Hypertension/Hypotension 4. Arrhythmias [Cocaine] 5. Methemoglobinemia [Benzocaine]
question
Neuromuscular Blocking Drugs
answer
Muscle paralysis in surgery or mechanical ventilation Selective for motor [vs. autonomic] nicotinic receptors
question
Depolarizing Neuromuscular Blocking Agents
answer
Drug: Succinylcholine MOA: Strong ACh receptor agonist, produces SUSTAINED DEPOLARIZATION and PREVENTS MUSCLE CONTRACTION Reversal of Blockade: 1. Phase I [Prolonge depolarization] = No antidote -- Block potentiated by cholinesterase inhibitors 2. Phase II [Repolarized but blocked] = ACh receptors are available but desensitized Antidote = Cholinesterase Inhibitors Complications: 1. Hypercalcemia 2. Hyperkalemia 3. Malignant hyperthermia
question
Nondepolarizing Neuromuscular Blocking Agents
answer
Drugs: Tubocurarine, Atracurium, Mivacurium, Pancuronium, Vecuronium, Rocuronium MOA: Competitive antagonist, compete w/ ACh receptors Reversal of blockade: 1. NEOSTIGMINE [Must be given with atropine to prevent muscarinic effects = Bradycardia] 2. Edrophonium 3. Other cholinesterase inhibitors
question
Dantrolene
answer
MOA: Prevents release of Ca2+ from sarcoplasmic reticulum of skeletal muscle Clinical Use: 1. Malignant hyperthermia 2. Neuroleptic malignant syndrome [Toxicity of antipsychotic drugs]
question
Baclofen
answer
MOA: Inhibits GABAB receptors at spinal cord, inducing skeletal muscle relaxation Clinical Use: Muscle spasms
question
Cyclobenzaprine
answer
MOA: Centrally acting skeletal muscle relaxant Structurally related to TCAs Similar anticholinergic side effects Clinical Use: Muscle spasms
question
Dopamine Agonists
answer
Ergot = Bromocriptine Non-ergot [Preferred] = Pramipexole, Ropinirole
question
? Dopamine Availability
answer
Amantadine ? Dopamine release and ? Dopamine Reuptake Also used as an antiviral against influenza A and rubella Toxicity 1. Ataxia 2. Livedo Reticularis
question
? L-dopa availability
answer
Agents prevent peripheral [pre-BBB] L-dopa degradation ? ? L-dopa entering CNS ? ? Central L-dopa available for conversion to dopamine Levodopa [L-dopa]/Carbidopa = Carbidopa block peripheral conversion of L-Dopa to dopamine by inhibiting DOPA decarboxylase Also reduces side effects of peripheral L-dopa conversion into dopamine [Nausea and Vomiting] Entacapone, Tolcapone = Prevent peripheral L-dopa degradation to 3-O-methyldopa [3-OMD] by inhibiting COMT
question
Prevent dopamine breakdown
answer
Agents act centrally [post-BBB] to block break down of dopamine ? ? Available Dopamine 1. Selegiline = Blocks conversion of dopamine into 3-MT by selectively inhibiting MOA-B 2. Tolcapone = Blocks conversion of dopamine by DOPAC by inhibiting central COMT
question
Curb Excess Cholinergic Activity
answer
Benztropine [Antimuscarinic, improves TREMOR and RIGIDITY, but has little effect on BRADYKINESIA]
question
L-Dopa
answer
Drug: Levodopa/Carbidopa MOA: ? LEvel of dopamine in the brain Unlike dopamine, L-dopa can cross the BBB and is converted by dopa decarboxylase in the CNS to dopamine Carbidopa [Peripheral dopa decarboxylase inhibitor] is given with L-dopa to ? the bioavailability of L-dopa in the brain and limit peripheral side effects Clinical Use: Parkinson's Disease Adverse Effects: Arrhythmias from ? peripheral formation of catecholamines Long-term use can lead to dyskinesia following administration [on-off phenomenon] Akinesia between doses
question
Selegiline
answer
Selectively inhibits MOA-B, which preferentially metabolizes dopamine over norepinephrine and 5-HT, ? availability of dopamine Clinical Use: Adjunctive agent to L-dopa in treatment of PArkinson Disease Toxicity: May enhance adverse effects of L-dopa
question
Alzheimer drugs [Memantine]
answer
Drug: Memantine MOA: NMDA receptor antagonist, helps prevent excitotoxicity [Mediated by Ca2+] Toxicity: Dizziness, confusion, hallucination
question
Alzheimer drugs [Donepezil, Galantamine, Rivastigmine, Tacrine]
answer
MOA: AChE inhibitors Toxicity: Nausea, dizziness, insomnia
question
Huntington Disease Drugs
answer
Neurotransmitter changes in Huntington Disease [? GABA, ? ACh, ? Dopamine] Treatments: 1. Tetrabenazine and Reserpine = Inhibit vesicular monoamine transporter [VMAT] -- Limits DOPAMINE VESICLE PACKAGE AND RELEASE 2. Haloperidol = D2 receptor antagonist
question
Triptans
answer
Sumatriptan MOA: 5-HT 1B/1D agonist -- INHIBITS TRIGEMINAL NERVE ACTIVATION -- Prevents vasoactive peptide release -- Induces vasoconstriction Clinical Use: Acute migraine, cluster headache attacks Adverse Effects: 1. Coronary vasospasm [Contraindicated in patients w/ CAD or Prinzmetal angina] Mild paresthesia



