Nursing Process (Pain & Comfort) – Flashcards
Unlock all answers in this set
Unlock answersquestion
The Nursing Process for Comfort
answer
1. Assessment 2. Diagnosing 3. Outcome Identification 4. Implementing 5. Evaluating
question
What is the fifth VS?
answer
Assessing for Pain
question
Nurses Responsibility
answer
1. explore the pain experience through the EYES of the client 2. Pt. have the right to appropriate assessment and management
question
Possible Barriers in Pain Assessment
answer
1. The nurse is the authority of the pt. pain (BIASES OF NURSE) -> nurses overestimate or underestimate the pain experience and withhold medication 2. Visible signs accompanying pain can verify it's existence and severity (lack of pain expression does NOT mean lack of pain) 3. Cognitively impaired older clients who are unable to use pain scales (want to use appropriate rating scale and give time)
question
Client's self report of pain
answer
SINGLE MOST RELIABLE INDICATOR of the existence and intensity of pain and any related discomfort
question
Components of pain assessment (characteristics)
answer
1. location 2. duration 3. intensity 4. quality 5. chronicity 6. AG factors 7. alleviating factors 8. physiologic indicators 9. behavioral responses 10. effects of pain on ADLs
question
Location
answer
Ask to tell or point to all areas of discomfort - "where is the pain located?" -document on a body diagram (as a useful baseline of the pain should change) -use anatomical landmarks and descriptive terminology ex) pain is localized in the right upper abdominal quad
question
Duration
answer
"when did the pain begin?" "how long has it lasted?" "does it occur at the same time each day?" "how often does it reoccur?"
question
Intensity
answer
*most subjective and most useful characteristic for reporting pain* -Pain scales
question
types of pain scales
answer
-verbal descriptive scale (VDS)-> none/uncomfortable/horrible/agonizing -numerical rating scale (NRS) -> rate pain from scale of 0-10 -visual analog scale (VAS) -> a straight line, representing a continuum of intensity (no pain _____________________ unbearable pain) -numerical rating scale -universal pain assessment tool -WILDA
question
numerical rating scale
answer
no pain: 0-1 mild pain: 2-3 moderate pain: 4-6 severe pain: 7-9 pain as bad as it can be: 10
question
values of "pain scales" to measure pain
answer
-easy to use -not time consuming -descriptive scales are useful in assessing severity in pain & evaluating changes in clients condition -pain scale CANNOT be used to compare the pain of one client to that of another
question
wrong baker faces
answer
pain rating scale -use for 3yrs and older
question
FLACC
answer
f:face l:legs a:activity c:cry c:consolability -use for children 2months - 7yrs of age -used for cognitively impaired adults and children (non responsive)
question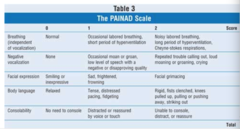
PainAD
answer
-pain scale -use for pt with dementia
question
WILDA
answer
w: words to describe pain I: intensity (0-10) l: location d: duration a: aggravating/alleviating factors -how does pain affect -are you experiencing any other symptoms -things to check: VS, PMH, knowledge of pain, use of noninvasive techniques
question
Oucher Scale
answer
ethnically specific options -ages 3-12 yrs
question
method for assessing pain
answer
1. pt self report 2. report of family member 3. nonverbal indicators 4. physiologic measures
question
Quality
answer
-no common vocal for description of pain -> "in your own words, how would you describe the pain?" (crushing, throbbing, sharp or dull, pricking, burning, aching) -some commonly used terms: 1. crushing or vise-like = MI 2. sharp or stabbing = surgical incision 3. burning = neuropathic pain
question
chronocity
answer
(chronology) -pattern to pain-> have pt keep journal
question
Aggravating factors
answer
-events or conditions that precipitate or aggravate pain -actions that cause a painful response
question
Alleviating factors
answer
-does the client have a useful method of relieving pain? -range of muscular activities, verbal methods (praying and cursing), concentration exercises help reduce intensity of oncoming pain -get identification of practitioners whose services are being used
question
Associated factors
answer
N, HA, dizziness, urge to urinate, constipation, restlessness
question
Physiologic Responses
answer
onset of acute pain -HR, RR, BP increase -palpation or manipulation of the site may increase pain -cues (posturing or guarding of the area may occur) -physical exhaustion if unrelieved
question
Behavioral indicators of effects of pain
answer
1. vocalizations (may be involuntary) 2. facial expressions 3. body movement 4. social interaction
question
Influence of Pain on DA
answer
-assessment of daily activities reveals the extent of disability and adjustments necessary to help in self-care routines 1. sleep interruptions? 2. normal hygiene? 3. sexual relations? 4. ability to work? 5. daily chores? 6. social activities? 5. neurological functions?
question
Special populations
answer
-children -older adults -developmentally delayed or clients who are psychotic -critically ill -cognitively impaired pt -clients with dementia -non-english speakers
question
Pain Assessment Tools for children
answer
-oucher (2 separate scales) -wrong baker faces -behavior indicators of pain
question
Pain as a problem (d)
answer
pain (acute or chronic) related to... -fear -inadequate pain management
question
pain as an etiology (d)
answer
-anxiety -ineffective coping -compromised health maintenance -ineffective health maintenance -fatigue -self care deficit -impaired physical mobility
question
Outcome Identification/Planning (p)
answer
-pt will have decreased level of pain (3/10) within one hour -pt will identify 3 emotional factors that precipitate pain by the end of the shift
question
Implementation (I)
answer
-be the patient advocate! -nurses role is to: 1. administer and monitor interventions ordered by physician for pain relief 2. independently use pain relief measurers that complement those prescribed by the physician
question
CAM pain-relief interventions (non pharmacological)
answer
1. include cognitive behavioral and physical approaches 2. agency for health care policy and research (AHCPR) cite non pharmacological interventions as appropriate to clients when they: -find them to be appealing -express anxiety or fear -may benefit from avoiding or reducing drug therapies -are likely to experience and need to cope with a prolonged interval of post op pain -have incomplete pain relief after use of pharmacological interventions
question
Distraction (I)
answer
-distraction directs a client's attention to something else and reduces awareness of pain -the reticular activating system inhibits painful stimuli if a person receives sufficient or excessive sensory input *w/ meaningful stimuli: can become unaware of pain *pleasurable stimuli: causes release of endorphins -most appropriate for short intense pain lasting a few minutes (while waiting for analgesia to work)
question
Music
answer
effective distraction that produces an altered state of consciousness through sound, silence, space and time -to be therapeutic listen to for at least 15 minutes -decreases physiological pain, stress, and anxiety by diverting there person's attention away from pain and creating a relaxation response -should match client's mood
question
Relaxation (I)
answer
relaxation: mental and physical freedom from tension or stress -relaxation techniques provide individuals with self-control when discomfort or pain occurs *reverses the physical and emotional stress of pain
question
Guided Imagery (I)
answer
-client creates an image in the mind, concentrates on the image and gradually becomes less aware of pain -nurse coaches in formation of image and concentrating on sensory experience -client describes image -STOP if signs of agitation or restlessness occur
question
Effective Relaxation
answer
-particiaption and cooperation are necessary -explain the technique in detail and describe common sensations -nurse is the coach, guiding through the exercise -environment should be free of noises -sit in a comfortable chair or lie in a bed -a light sheet or blanket for warmth = comfortable
question
Effects of Relaxation
answer
-decreased pulse, BP, RR -decreased O2 consumption -decreased muscle tension -decreased metabolic rate -heightened global awareness -lack of attention to environmental stimuli -no voluntary change of position -sense of peace and well-being -deep, wakeful, restful period of alertness
question
Progressive Relaxation
answer
-involves combination of controlled breathing exercises and series of contractions and relaxation of muscle groups -attention is paid to body and areas of tension are noted -success: when full relaxation is achieved -> pain perception and anxiety is lowered
question
Cutaneous Stimulation (CS)
answer
-stimulation of the skin to relieve pain *touch and massage are sensory integration techniques that influence autonomic nervous system activity -massage -applying heat (dry & moist) -applying cold (dry & moist)
question
Applying heat
answer
dry: hot water bags, electric heating pads, aquathermia pads, hot packs moist: sterile moist compress, sitz baths, warm soaks
question
Applying cold
answer
dry: ice bags, cold packs, hypothermia blankets moist: cold compress
question
Acupressure
answer
-based on asian theory that a life force in the form of energy, circulates throughout the body in well-defined cycles -acupressure opens congested energy pathways to promote a healthier state (takes about an hour) -nurse therapists apply pressure over particular points along pathways
question
TENS
answer
transcutaneous electrical nerve stimulation -stimulation of skin with mild electric current passed through external electrodes -REQUIRES PHYSICIAN ORDER -consists of a battery powered transmitter, lead wire, electrodes (placed over or near the site of pain) -when client feels pain: transmitter is turned on, and a tingling sensation is created. -intensity and quality of skin stimulation may be adjusted -tingling sensation applied until pain relief occurs -useful: post surgical pain control and reduction of pain caused by post op procedures
question
Self-Hypnosis
answer
-useful self-suggestion and images of relaxation and peace -helps to alter pain perception through the influence of positive suggestion
question
Biofeedback
answer
-learns voluntary control over autonomic function such as HR, muscle tension -produces deep relaxation - effective for muscle tension and migraine HA (place electrodes externally over each temple) -requires extensive training (takes several weeks to learn)
question
Meditation
answer
-person focuses on a single thought or sound -yoga is meditation with stretching exercises
question
basic nursing interventions for controlling painful stimuli
answer
-tighten & smooth wrinkled bed linens -position tubing on which client is lying -loosen constricting bandages -change wet dressings and linens -position in anatomical alignment -check temp or hot or cold application -lift client up in bed -position correctly on bed pan -avoid exposing skin or mucous membranes to irritants -prevent urinary retention -prevent constipation with fluids, diet and exercise -remove or prevent painful stimuli -anticipate procedures' effects



