27 – Antineoplastics – Flashcards
Unlock all answers in this set
Unlock answersquestion
Overview of Antineoplastic Agents (picture)

answer
- all inhibit DNA synthesis in some way
question
Characteristics of Cancer Cells
answer
- Uncontrolled proliferation - *Dedifferentiation with loss of function* - Invasiveness - Metastases
question
The log-kill hypothesis (chart)

answer
dash line - have cancer, don't do anything about - symptoms - tx will prolong survival, but you will die younger - you MUST eradicate all cancer cells to get rid of the disease - surgery + radiation ; shorter tx time
question
CHEMOTHERAPY
answer
- Primary treatment for hematologic and diffuse cancers eg leukemias - *Adjuvant chemotherapy* after surgery ; radiation of solid tumors - *Neoadjuvant chemotherapy* before surgery improves surgical results eg in osteogenic sarcoma / breast cancer (CA) to downstage tumor - *Chemoprotection* to prevent cancer in high risk individuals
question
Concepts Related to Chemotherapy
answer
- Selective toxicity - Cell kinetics: cycle time, growth fraction - Cell cycle phases - Cell phase and cycle specificity for drug action - Cancer growth
question
Cell cycle of cancer cell

answer
- most drugs work in S phase M phase: vincristine S + G2: etoposide G2: Bleomycin
question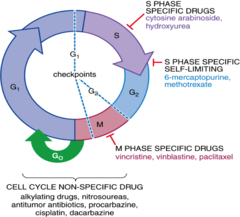
Cell cycle ; site of action of antineoplastic agents
answer
- cell cycle agents vs. non specific drugs (these have the MOST ADRs, aggressive)
question
Common Toxicities
answer
- Bone marrow suppression (BMS), infections (blood cells divide everyday) - Damage to GI epithelium, ulcerations, mucositis, stomatitis - Skin damage / sores - Loss of hair (alopecia) - Sterility / teratogenicity / *carcinogenicity (mainly alkylators)* - cancer tax's that cause cancer - Nausea / vomiting (N/V)
question
*Drug resistance*
answer
- Decreased permeation/* increased drug efflux via P-glycoprotein transporter* (e.g., *methotrexate and vincristine*) - Increased intracellular conc. of thiols - Increased activity of DNA repair pathways - Increased rates of metabolism
question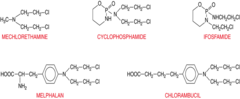
Chemical structure of nitrogen mustards
answer
- cyclophosphamide, ifosfamide, + mechlorethamin are important
question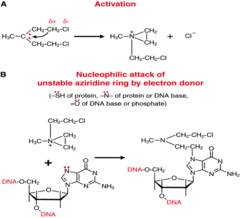
Mechanism of action of alkylating agents
answer
- alkylating action that attaches to DNA; eventually will cause cell death which you want in cancer (example of *meclorethamine*)
question
Meclorethamine: Clinical indication
answer
- Most commonly used as a component of the mechlorethamine, vincristine, prednisone, procarbazine (MOPP) regimen in Hodgkin's disease (nitrogen mustard - alkylating agent)
question
Meclorethamine: Pharmacokinetics
answer
- IV, rapid action/short duration, spontaneously converts to reactive metabolite; potent vesicant, extravasation causes severe pain / necrosis - lots of pain at injection site (nitrogen mustard - alkylating agent)
question
Meclorethamine: ADRs
answer
- Highly reactive, do not mix with any other drugs, decomposes within 30 minutes - Myelosuppression (BMS) dose-limiting; severe nausea/vomiting, alopecia (nitrogen mustard - alkylating agent)
question
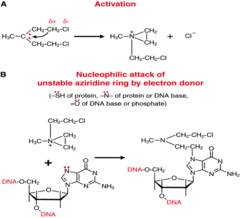
Cyclophosphamide: Mechanism of action/clinical indications, pharmacokinetics and adverse effects
answer
- Broad-spectrum alkylator, PO / IV - Prodrug, activated by liver P-450 enzymes - Phosphoramide mustard - the alkylator - Use for lymphomas and lymphocytic leukemia, ovarian cancers and solid tumors in children - *Acrolein (cytotoxic) - hemorrhagic cystitis* - cause blood in urine - Predrug hydration use of mesna disulfide - Severe N/V, dose-limiting BMS, alopecia, mucocutaneous, cystitis, amenorrhea/ azoospermia
question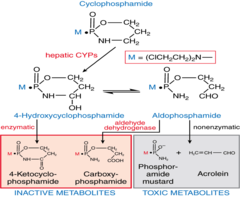
Metabolism of cyclophosphamide
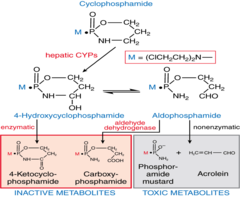
answer
- Prodrug, liver converts it to active aldophosphamide - phosphoramide mustard = alkylating agent
question
Ifosfamide: Mechanism of action/clinical indications, pharmacokinetics and adverse effects
answer
- Related to cyclophosphamide,~ uses/toxicity - Slower hepatic activation to ifosfamide mustard, need larger doses, more acrolein, - Dose-limiting toxicity *hemorrhagic cystitis*, mesna usu. mandatory - CNS toxicity, thought to be due to formation of chloracetaldehyde - decreased arousal, somnolence, coma, seizures ; death - Advantage: Less bone marrow suppression (BMS)
question
Chlorambucil: Mechanism of action/clinical indications, pharmacokinetics and adverse effects
answer
- Alkylator, PO adm, good bioavailability - Main use: chronic lymphocytic leukemia (CLL), and non-Hodgkin's lymphoma (NHL) - Usually well tolerated on daily basis - Lower toxicity on bone marrow and more easily reversed - N/V usually @ higher doses, amenorrhea/ azoospermia, sterility, secondary acute leukemias with prolonged use
question
Chronic Myeloid Leukemia (CML)
answer
- Genetic defect in Phila chromosome that inc abn enzyme BCR-ABL causing *unregulated tyrosine kinase* >excessive production white blood cells (WBCs) - Bone marrow transplant only cure - *Busulfan* - sulfonate alkylator, decs mainly granulocytes; pulmonary fibrosis, skin pigmentation - *Imatinib mesylate* - small organic molecule that inhibits ABL portion of abnormal enzyme; mild side effects, allows pts to live relative comfort for years
question
Nitrosoureas: Carmustine - Mechanism of action/clinical indications, pharmacokinetics and adverse effects
answer
- Nitrosourea, highly lipid soluble *crosses BBB* - Nonenzymatic conversion to alkylator - Particularly indicated for CNS /GI tumors, meningeal leukemias, NHL, Hodgkin's disease - Drug is a vesicant (i.e., local irritation) - Minimal cross resistance with nitrogen mustard alkylators - Delayed bone marrow toxicity - (N-V), BMS, mucocutaneous, hepato- / renal toxicity, pulmonary fibrosis at higher doses
question
*Cisplatin*: Mechanism of action/clinical indications, pharmacokinetics and adverse effects
answer
- Platinum metal salt, acts as an alkylator - Intra strand cross-linking of double-stranded DNA - *Wide use in solid tumors; testicular, lung, ovarian, breast* (aggressive - pancreatic) - ;90% bound to plasma proteins, 25% is excreted by 24 hours, 45% by 5 days - Usually severe/persistent nausea/vomiting - Dose-limiting *nephrotoxicity* (renal tubular damage); use hydration / diuretics (mannitol); amifostine - Ototoxicity/high tone loss/tinnitus; *peripheral neuropathy* - BMS usually mild
question
*Oxaliplatin*: Uses, ADRs
answer
- uses - colorectal, pancreatic cancers/combined w/5-FU and leucovorin (FOLFOX regimen); *BMS*, peripheral neuropathy, diarrhea
question
Carboplatin
answer
- similar uses as cisplatin - less hydration is needed; more BMS, less nephrotoxic
question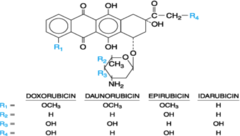
Chemical Structures of Anthracyclines
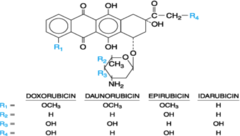
answer
- know doxorubin
question
Anthracyclines: Doxorubicin - Mechanism of action/clinical indications, pharmacokinetics
answer
- Anthracycline antibiotic acts by DNA intercalation, inhibits topoisomerase II, free radical formation;DNA scissions,; a vesicant - Isolated from the soil microbe: Streptomyces - Widely used lymphomas, leukemias, and many solid tumors (e.g.,osteosarcomas, lung/testicular/ ovarian/ breast cancers), - Converted to active alcohol intermediate, drug is cleared by hepatic metabolism and biliary excretion
question
Anthracyclines: Doxorubicin - ADRs
answer
- BMS dose-limiting, stomatitis, EKG changes, tachycardia / cardiac arrhythmias - *Chronic cumulative dose-dependent cardiomyopathy irreversible CHF*
question
Anthracyclines: Doxorubicin - Administer this drug along with:
answer
- *Dexrazoxane- chelates Fe prevents iron-mediated free radical generation, used to reduce cardiotoxicity*
question
Anthracyclines: Daunorubicin
answer
- used in acute myelocytic leukemia (AML), acute lymphoblastic leukemia (ALL), acute nonlymphocytic leukemia (ANLL) - synthetic
question
Anthracyclines: Mitoxantrone
answer
- synthetic analog of doxorubicin, less cardiac toxicity, used ANLL, breast cancer, others
question
Anthracyclines: Idarubicin
answer
- a semisynthetic derivative with similar uses as daunorubicin, AML/ALL, claim of less cardiotoxicity
question
Bleomycin: Mechanism of action/clinical indications, pharmacokinetics
answer
- Glycopeptide antibiotic intercalator, binds Fe DNA to form free radicals that cause DNA strand breaks, a.k.a. scissions, Cell cycle G2 phase - Isolated from Streptococcus verticillus - Uses: Headneck, testicular, cervix, esophagus, lung, Hodgkin's NHL - Admin. I.V. or I.M./inj. into bladder (i.e., bladder cancer), T1/2: 3 hours, 70% is excreted in urine
question
Bleomycin: ADRs
answer
- *Dose-related pulmonary pneumonitis* with progression to fibrosis (most serious toxic effect - life threatening); mucositis, hyperpigmentation (hands) - Minimal BMS
question
Antimetabolites: Methotrexate (MTX) - Mechanism of action/clinical indications, pharmacokinetics
answer
- Binds with great affinity to dihydrofolate reductase, prevents activation of folic acid; requires transport into cells - Polyglutamated within cells, long t1/2 in liver/kidney (months); MTX elim. by renal mech.(t1/2 = 2/10 hrs.); *increased P-glycoprotein transporter in cancer cells leads to resistance - Wide use: ALL, NHL, choriocarcinoma, solid tumors; also Rheumatoid arthritis and psoriasis*
question
Leucovorin
answer
- *Leucovorin "rescue"* (activated folate) adm with high dose MTX (weak acid), administered within 24-36 hr; ? dose if plasma MTX remains elevated; *nephrotoxicity* /alkalinize urine and hydrate person to minimize toxicity
question
Antimetabolites: Methotrexate (MTX) - ADRs
answer
- *nephrotoxicity* - *BMS, GI tract/ulcers*, skin, hepatic/pulmonary fibrosis, teratogen - Drug interactions - highly plasma protein bound drugs can displace MTX to inc toxicity, e.g. warfarin, sulfonamides, tetracyclines; also drugs that compete for tubular secretion, e.g. pens, cephs or reduce renal blood flow, e.g. NSAIDS
question
Methotrexate/mechanism of action

answer
- build up of methotrexate polyglutamase in cells is a major mechanism of inhibitions
question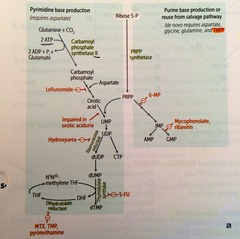
5 - Fluorouracil (5-FU)
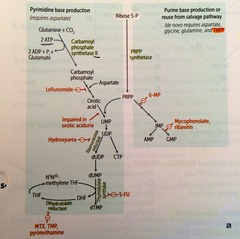
answer
- Activated to FdUMP, complexes with tetrahydrofolate (FH4) to *irreversibly inhibit thymidylate synthetase "thymineless death" and synthesis of DNA*, methotrexate also enhances activation of 5-FU, adm IV due severe GI toxicity - *Catabolized by dihydropyrimidine dehydrogenase (DPD); 5% of CA patient are deficient leads to increased BMS.* - FUMP >Triphosphate into RNA and miscoding - Carcinomas : used mostly in solid tumors of GI (esp colon), bladder, breast, head and neck, skin (topical application) - Capecitabine, related drug forms 5-FU, adm. PO - *BMS*, GI mucositis stomatitis, *skin hyperpigmentation*
question
5-fluorouracil/mechanism of action

answer
- don't need to know enzymes
question
Mercaptopurine: Mechanism of action/clinical indications, pharmacokinetics and adverse effects

answer
- Purine-related analog, forms fraudulent nucleotides that inhibits purine synthesis - Also forms fraudulent bases in DNA that lead to miscoding ; faulty translation - *Use: childhood acute leukemia* - Bioavailability- only 10-50%, metabolized by HGPRT to 6-thioinosinic acid (active metabolite) increased when combined with methotrexate - Typical toxicity: BMS (usually mild), n-v, GI ulcer, hyperuricemia, long term use associated with risk of hepatotoxicity - Drug interaction with *allopurinol Xanthine Oxidase*
question
Cytarabine - mechanism of action/clinical indications, pharmacokinetics and adverse effects
answer
- Cytosine analog, activated to CTP, inhibits DNA polymerase, incorporated into DNA, is an S-phase specific antimetabolite - Very active for adult AML - 20% bioavailability due to cytidine deaminase in GI tract and liver - BMS, GI, neurotoxicity - Liposomal IT injection for lymphomatous meningitis; may cause seizures/altered mental states
question
*Gemcitabine*
answer
- new analog of cytarabine, less toxicity; an influenza-like syndrome, mild BMS; used in *pancreatic*, ovarian, bladder ; lung cancers
question
Alkylators vs Antimetabolites - Summary of effects and adverse reactions
answer
Alkylators: - CCNS - Damage preformed DNA - Action on rapid ; slow/G? proliferating cells - Greater ability to kill BM stem cells/ cause secondary lymphomas /leukemias - Greater mutagenic, teratogenic, carcinogenic potential Antimetabolites: - CCS (S phase) - interfere with synthesis new DNA - action just on rapidly proliferating cells
question
Vincristine (plant derivative) - Mechanism of action/clinical indications and adverse effects
answer
- M phase drugs metaphase arrest, binds tubulin, prevents microtubule formation - *P-glycoprotein transporter is increased and leads to resistance dev. in cancer cells - Plant alkaloid derivative of Vinca rosea* - Indications ALL, *Hodgkins/NHL lymphomas*, Wilms tumor - Vesicant action with extravasation, alopecia common, BMS usu. mild - *Neurotoxicity* dose-dependent/limiting (paresthesias, areflexia, neuritis, paralytic ileus/constipation, muscle weakness)
question
*Vinblastine*
answer
- dose-limiting toxicity *BMS* (leukopenia), vesicant action, GI; use testicular CA, lymphomas
question
Vinorelbine
answer
- used in non-small cell lung cancer (NSCLC), less toxicity
question
Topoisomerase Inhibitors - Mechanism of Action
answer
- Topoisomerase I breaks and reseals single-stranded DNA. Inhibited by camptothecin analogues: *irinotecan and topotecan*, S-phase specific drugs - Topoisomerase II breaks and reseals double-stranded DNA. Inhibited by podophyllotoxins: *etoposide and teniposide* , S-G2 phase action
question
Camtothecin Analogues - Mechanism of action/clinical indications, pharmacokinetics and adverse effects
answer
- Inhibits DNA topoisomerase I - Large lactone ring structure, adm IV, bioavailability 20-35% - *Irinotecan* - adm IV rapidly metabolized in liver to highly active SN-38 metabolite. - Main use recurrent colorectal CA with 5FU/leucovorin (FOLFIRI), and with cisplatin in advanced small-cell lung cancer - *Topotecan* - active against glioma, sarcoma, lung, ovarian CA - ADRs (both), BMS, N-V-diarrhea (severe with irinotecan), alopecia
question
Podophyllotoxins - Mechanism of action/clinical indications, pharmacokinetics and adverse effects
answer
- *Etoposide (broad-spectrum use)* and Teniposide (primarily used in combination drug regimens for lung (small cell), prostate, and testicular carcinoma) - Inhibit topoisomerase II, forms complex with DNA that causes permanent DNA strand breakage, active in S / G2 phases; etoposide also can cause metaphase arrest - Bioavailability 50% after P.O. adm., excreted in urine - Common toxicities: BMS, N-V, alopecia, mucocutaneous/GI, hypotension when infused to rapidly, secondary leukemias (etoposide)
question
Paclitaxel - Mechanism of action/clinical indications, pharmacokinetics and adverse effects
answer
- Derived from pacific/European yew tree - *Acts in M phase, inc polymerization of mitotic spindle, blocks disassembly* - Advanced breast and ovarian CA , lung - Inactivated by hepatic metabolism, CYP enzymes (Taxanes) - *Neutropenia *(BMS), thrombocytopenia, *peripheral neuropath*y (myalgia/sensory disturbances) are dose-limiting toxicities;
question
Docetaxel

answer
- paclitaxel analog, used advanced breast/ovarian CA, ADRs: neutropenia, neurotoxicity (Taxanes)
question
L-Asparaginase - Mechanism of action/clinical indications, pharmacokinetics and adverse effects

answer
- Enzyme derived originally from E. coli - Inhibition of protein synthesis - Some leukemic (ALL)/lymphoma cells lack asparagine synthetase and require asparagine as an essential amino acid - Asparaginase metabolizes asparagine to the inactive aspartic acid - Allergic /hypersensitivity rxs, hyperglycemia, bleeding, hepatotoxicity, pancreatitis
question
Pegaspargase
answer
- modified form for patients sensitive to L-asparaginase - conjugated with polyethylene glycol (PEG)
question
Hormonal agents - Summary of mechanism
answer
- Many tumors of reproductive organs possess receptors for sex and steroid hormones that regulate growth - Removal of endocrine gland (outdated) - Administer opposite sex hormone (generally outdated) - Hormonal antagonists to block receptors, this has become the preferred method - Glucocorticoids (agonists); *prednisone *- suppresses lymphocyte mitosis; used in lymphomas/leukemias
question
Tamoxifen - Mechanism of action/clinical indications, pharmacokinetics and adverse effects
answer
- Blocks cytoplasmic estrogen receptors (anti-estrogenic) - Originally developed as oral contraceptive - Cytostatic action, not tidal *less toxic; - Primary indication for breast cancer in node+ postmenopausals, trials underway for chemoprevention in high risk women - Adverse effects similar to post-menopausal : hot flashes, menstrual irregularities/bleeding, n-v, risk of endometrial cancer/uterine agonist
question
Toremifene:
answer
- new analog (of Tamoxifen) /advanced breast CA
question
Aromatase Inhibitors
answer
(e.g., anastrozole): advanced breast cancer
question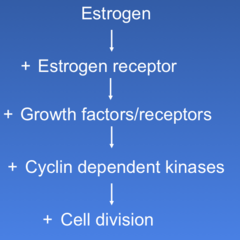
Signaling of estrogen
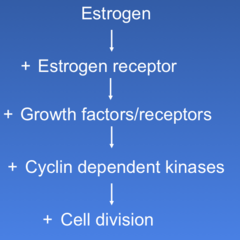
answer
- receptor are tyrosine kinase
question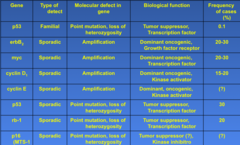
Table 1 Principal genetic alterations in breast cancer
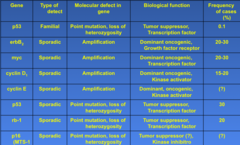
answer
*erb B2*
question
Oncogenes/Tumor suppressor genes and the cell cycle

answer
CDK inhibitors
question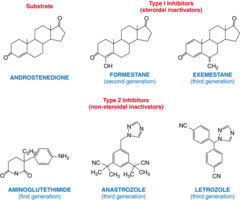
Aromatase inhibitors/chemical structures
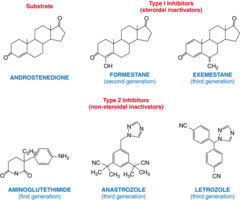
answer
- *lestrozole + anastrozole*
question
Aromatase Inhibitors - Specific Drugs ; Mechanisms of action
answer
- Aromatase - responsible for the conversion of androstenedione and testosterone to estrone and estradiol, respectively - *Letrozole* - Inhibits estrogen synthesis from androstenedione and testosterone - *Anastrozole* - similar to letrozole - Exemestane - steroid, irreversible inhibitor of aromatase
question
Aromatase Inhibitors - clinical indications and adverse effects
answer
- Indicated for treatment advanced breast cancer postmenopausal women with disease progression following tamoxifen therapy - ADRs: fatigue, n-v/GI, headache, muscle pain, estrogen-deficiency symptoms - Drugs contraindicated in pregnancy
question
Gonadotropin-Releasing Hormone Agonists: Mechanism of action and clinical indications
answer
- *Leuprolide *- Buserelin - Goserelin - Peptide analogs of LH-RH that initially stimulate hormone production, but *chronically *inhibit FSH / LH secretion, (pharmacologic castration) monthly IM injections - Decreases gonadal production of both estrogen and testosterone - Use: prostate cancer
question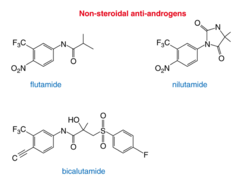
Androgen receptor antagonists/chemical structures
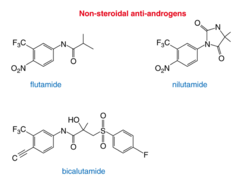
answer
*flutaminde*
question
*Flutamide*
answer
(Antiandrogens) - androgen receptor blocker; non-steroidal; used in prostate cancer ; initial leuprolide therapy; side effects: diarrhea, nausea reversible liver abnormalities ? Interrupt negative feedback of testosterone to pituitary-hypothalamic axis - attenuating impotency and loss of libido
question
Cyproterone
answer
(Antiandrogens) - steroidal inhibitor of androgen receptor; used to treat prostate cancer antiandrogen side effects: hot flushes, impotency/loss of libido, gynecomastia
question
*Procarbazine and Dacarbazine*:
answer
- methylation of DNA thereby inhibiting DNA synthesis (these agents primarily used in drug regimens of Hodgkin's lymphoma; e.g., doxorubicin, bleomycin, vinblastine, dacarbazine (ABVD)) and brain tumors
question
Gefitinib
answer
- small molecule, binds epidermal growth factor receptor; use NSCLC (non-small cell non lung carcinoma)
question
Erlotinib:
answer
- blocks epidermal growth factor receptor that instructs cells to grow/divide, use NSCLC
question
Hydroxyurea:
answer
- inhibits DNA synthesis in S phase; used in CML, but largely replaced by imatinib; still used to treat sickle cell anemia
question
Mitotane:
answer
- adrenal necrosis adrenal tumors
question
*Trastuzumab*
answer
(Monoclonal Antibodies) - binds, blocks, down-regulates human epidermal growth factor receptor HER 2, *approved in breast tumors that over express HER 2 (~ 30% of cases)* - Serious hypersensitivity and pulmonary reactions have resulted in deaths - ADRs: chills, fever, mouth sores, cardiac disturbances/CHF WILL BE ON TEST
question
*Bevacizumab *
answer
(Monoclonal Antibodies) - binds vascular endothelial growth factor, starves tumors of blood supply needed for growth, used in colorectal/lung cancer
question
Rituximab
answer
(Monoclonal Antibodies) - murine antibody that binds CD20 receptor normal/malignant B lymphocytes, used in NHL, induces complement-mediated lysis, apoptosis; ADR: can cause serious infusion-rx, fever/chills/bronchospasm/angioedema
question
Tositumomab
answer
(Monoclonal Antibodies) - anti-B-cell (binds CD20 receptor) lymphoma antibody conjugated to an iodine 131 isotope, NHL
question
Alemtuzumab
answer
(Monoclonal Antibodies) - human antibody against CD52 antigen on B and T-cell lymphomas; used in CLL
question
A 32-year-old woman underwent segmental mastectomy for a breast tumor of 3 cm diameter. Lymph node sampling revealed 2 involved nodes. She underwent postoperative treatment with antineoplastic drugs. The chemotherapy regimen was fluorouracil, doxorubicin, cyclophosphamide & vincristine. Six cycles 1 mo apart of this chemotherpy regimen were planned. Adjunctive drugs included tamoxifen because the tumor cells were hormone receptor positive. The chemotherapy undertaken by this patient caused acute hemorrhagic cystitis. Which drug was most likely responsible for this toxicity? A. Cyclophosphamide B. Doxorubicin C. Fluorouracil D. Tamoxifen E. Vincristine
answer
A. Cyclophosphamide
question
Which of the following best describes the mechanism of anticancer action of cellular metabolites of fluorouracil? (A) Cross-linking of double-stranded DNA (B) Inhibition of DNA-dependent RNA synthesis (C) Interference with the activity of topoisomerase I (D) Irreversible inhibition of thymidylate synthase (E) Selective inhibition of DNA polymerases
answer
(D) Irreversible inhibition of thymidylate synthase
question
After several cycles of chemotherapy, the patient was found to have a high resting pulse rate. A noninvasive radionuclide scan revealed evidence of cardiomyopathy. The drug that is most likely responsible for the cardiac toxicity is: A. Cyclophosphamide B. Doxorubicin C. Fluorouracil D. Tamoxifen E. Vincristine
answer
B. Doxorubicin If asked to reverse toxicity - know chelating agent
question
Which of the following is a cell cycle specific anticancer drug that acts mainly in the M phase of the cell cycle? A. Bleomycin B. Cisplatin C. Etoposide D. Methotrexate E. Paclitaxel
answer
E. Paclitaxel
question
An adult patient is being treated for acute leukemia with a combination of anticancer drugs that includes cyclophosphamide, mercaptopurine, methotrexate, vincristine and prednisone. The patient complains of "pins and needle" sensations in the extremities and muscle weakness. He is not able to execute a deep knee bend or get up out of a chair without using his arm muscles. If these problems are related to the chemotherapy, which of the following is the most likely causative agent? (A) Cyclophosphamide (B) Mercaptopurine (C) Methotrexate (D) Prednisone (E) Vincristine
answer
(E) Vincristine
question
Which of the following is a drug that is used in combination therapy for testicular carcinoma and is also associated with nephrotoxicity? (A) Bleomycin (B) Cisplatin (C) Etoposide (D) Leuprolide (E) Vinblastine
answer
(B) Cisplatin
question
A cancer cell that is resistant to the effects of both vincristine and methotrexate probably has developed that resistance as a result of (A) Changes in properties of a target enzyme (B) Decreased activity of an activating enzyme (C) Increase in expression of a P-glycoprotein transporter (D) Increase in proteins that are involved in DNA repair (E) Increase in production of drug-trapping molecules
answer
(C) Increase in expression of a P-glycoprotein transporter
question
A 23-year-old man with Hodgkin's disease was treated unsuccessfully with the MOPP regimen (mechlorethamine, vincristine, prednisone, procarbazine). He subsequently underwent a successful course of therapy with the ABVD regimen (doxorubicin, bleomycin, vinblastine, dacarbazine) Which of the following classes of anticancer drugs used in the treatment of this patient is cell cycle specific (CCS) and is used in both the MOPP and ABVD regimens? (A) Alkylating agents (B) Antibiotics (C) Antimetabolites (D) Glucocorticoids (E) Plant alkaloids
answer
(E) Plant alkaloids (Vincristine ; vinblastine)
question
During the second course of drug treatment (ABVD regimen), this patient developed dyspnea, a nonproductive cough, and intermittent fever, Chest x-ray film revealed pulmonary infiltration. If these problems are due to the anticancer drugs to which has been exposed, the most likely causative agent is (A) Bleomycin (B) Dacarbazine (C) Doxorubicin (D) Prednisone (E) Vinblastine
answer
(A) Bleomycin
question
All of the following agents have been used in drug regimens for the treatment of breast carcinoma. Which one has specific activity in a subset of female breast cancers? (A) Flutamide (B) Doxorubicin (C) Fluorouracil (D) Methotrexate (E) Trastuzumab
answer
(E) Trastuzumab
question
A 55-year-old man presents with increasing fatigue, 15-pound weight loss, and a microcytic anemia. Colonoscopy identifies a mass in the colon and biopsy reveals colon cancer. The mass is surgically removed and the patient receives FOLFOX regimen (5-FU, leucovorin and oxaliplatin) for his adjuvant therapy. After the first weekly cycle of the therapy, which of the following adverse effects are likely for the patient to experience? (A) Shortness of breath (B) Swelling of hands (C) Skin rash (D) Myelosuppression (E) Brain pain
answer
(D) Myelosuppression
question
A 28-year-old woman presents with a 1-cm mass in the right supraclavicular fossa. Biopsy reveals nodular sclerosing Hodgkin's disease that is advanced. Which of the following drugs are useful in Hodgkin's lymphoma? (A) Paciltaxel (B) Methotrexate (C) 5-fluorouracil (D) Vincristine (E) Cisplatin
answer
Comes down to two - best choice: (D) Vincristine



