Postural imbalance and short leg syndrome – Flashcards
Unlock all answers in this set
Unlock answersquestion
What is Short Leg Syndrome?
answer
A condition in which an anatomical or functional leg length discrepancy results in - sacral base unleveling - vertebral sidebending and rotation - innominate rotation
question
what is a functional Short leg?
answer
One leg appears shorter than the other due to somatic dysfunction in sacrum, pelvis, lumbar spine, cranium or anywhere
question
What is an Anatomic Short leg?
answer
It is an actual discrepancy in the lengths of the femurs or tibia
question
what can cause a Anatomic Short leg?
answer
- childhood trauma with fracture or growth plate injury (often) - polio, cerebral palsy, major illness, osteomyelitis, surgery (hip replacement) - basically any illness that affects the metabolic growth rate of bone
question
What is the typically presentation of a pt with Short Leg Syndrome?
answer
- back pain - SI joint pain (usually on the side of the longer leg) - Hip pain - Knee pain - Pelvic pain - Dysmenorrhea/menorrhagia - Chronic constipation
question
what might be in the history of a pt with Short Leg Syndrome?
answer
- more often chronic pain that has gradually worsened over time - occasionally discovered after an injury from which the pt never recovered - pt may tell you that the wear out their shoe at different rates or that their pants hang unevenly
question
what are the signs of short Leg Syndrome, that would be seen during a physical exam?
answer
- Standing exam (with feel level and pointed straight forward) - discrepancy in crest heights, ASIS, PSIS, ischial tuberosities - Difference in feet - pronation vs supination - One leg flexed at hip, more forward or externally rotated at hip - may have mild or even moderate-severe scoliosis dont forget to also examine: angle between the thigh and leg, and angle between the leg and foot
question
How does pronation of the foot affect leg length? What does pronation of the foot involve?
answer
Pronation *shortens* the leg pronation of the foot involves: *abduction, dorsiflexion, and eversion*
question
How does supination of the foot affect leg length? What does supination of the foot involve?
answer
Supination *lengthens* the leg supination of the foot involves: *adduction, plantar flexion, and inversion*
question
How can you tell the difference between a functional and anatomic short leg?
answer
Functional - resolves with OMT and postural correction - re-evaluation of findings and malleoli shows no further asymmetry Anatomic - regardless of whether dysfunction is resolved, leg remains short OR now appear shorter after removal of compensations
question
what are the two possible signs of Anatomic short leg syndrome when examining the pt in the supine position?
answer
One - leg lengths are *asymmetric* at malleoli - pelvis and sacrum ect. may or may not show somatic dysfunction but more likely to *appear balanced*, especially if the patient uses a lift Two - leg lengths are *symmetric* at malleoli - pelvis and sacrum extra may or may not show somatic dysfunction but more likely to *appear unbalanced*
question
Which leg is more likely to be short in Anatomic Short leg syndrome? What is the common presentation of Anatomical short leg syndrome?
answer
- *Right* is more common - Somatic dysfunctions resemble common compensatory pattern - L-spine SlRr - Left on left torsion - Right innominate anterior/ left posterior
question
what is the compensatory fascial pattern seen in anatomical short right leg syndrome?
answer
OA - left (r-to-l) → RTM diaphragm CT - right (l-to-r) → thoracic inlet diaphragm TL - left (r-to-l) → abdominal diaphragm LS - right (l-to-r) → pelvic diaphragm these are transitional regions - areas where anatomic structure changes create the potential for the greatest functional change
question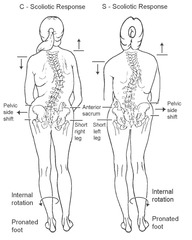
describe the biomechanics of somatic dysfunctions caused by short leg syndrome
answer
- when the sacral base is unlevel, the body compensates to try to keep the eyes level - early in the process the thoracic and lumbar side form a long *C-shaped curve* that is *concave on the long leg side* and *convex on the short leg side* - with more time compensatory mechanism redistribute an *S-shaped curve forms* with the *lumbar concavity away from the short leg* and the *thoracic concavity towards the short leg*
question
early in the biomechanical process what shapes does the thoracic and lumbar spine form?
answer
a C shaped curve
question
what side of the C shaped curve is concave and convex?
answer
Concave = on the long leg side Convex = on the short leg side
question
late in the biomechanical process what shape does the thoracic and lumbar spine form?
answer
S-shaped curve
question
what direction does the lumbar and thoracic concavity face in the S-shaped curved spine?
answer
Lumbar concavity away from the short leg Thoracic concavity towards the short leg
question
what are the consequences of Short leg syndrome
answer
Muscle imbalance - *hypertonic muscles in long leg - weak muscles in short leg* *Ligaments* (such as the iliolumbar ligament) will *calcify* in under prolonged stress *Bone will remodel* when under stress - within the compensatory curve, wedging of the vertebrae will occur Joint degeneration will occur with *arthritis* of the hip/SI on the *long leg side*
question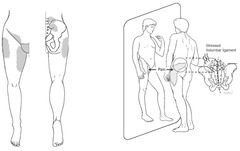
describe the referral pattern of pain from the iliolumbar ligament
answer
ipsilateral groin, and sometimes into the testicle or the labia and the upper medial thigh (gluteus medius, minimus area, and greater trochanter)
question
What is the medical management for Short leg syndrome
answer
- Treat with OMT 2-3 times to see how the patient response before adding a lift or doing x-rays - Postural x-rays (sacral base unleveling is the most important criterium) - Lift therapy - Exercise
question
How do you take measurement from a postural X-ray review
answer
1. make a reference line (RL) using a plumb line 2. make a line from the top of each femur to the RL 3. make a line from the top of each iliac crest to the RL
question
when/how to use a lift for short leg syndrome
answer
Acute: usually after trauma or joint replacement surgery - cna replace entire amount of sacral base unleveling Chronic - start with the lowest level of lip - gradual increase - usually only increase half (or a little more) of sacral base unleveling Lifts must be used at all times so that the body is not constantly trying to accommodate to changing leg lengths
question
when would short leg syndrome not require a lift?
answer
if unleveling of the sacral bases is less than 5 mm
question
what should you do if a lift greater that 12 mm is needed?
answer
must apply lift to outside of shoe to *avoid achilles contracture*
question
Swayback posture also called ____ is part of the clinical presentation of what?
answer
also called *increased lumbar lordosis* is part of the clinical presentation of *Lower Cross syndrome*
question
what is Levitor
answer
- it transfers pressure to cushioned pads, one over the superior portion of the pubic symphysis and the other on the posterior part of the sacral apex below the S2 middle transverse axis - it is designed to resist the counter-rotation of the sacrum and innominates that occur under the influence of the strain of gravity - *used for sagittal plane dysfunction, makes the sacrum move toward extension*
question
what exercises are useful for short leg syndrome?
answer
- Knee/chest stretches - Quadratus lumborum and psoas stretches - Hamstring stretches - Pelvic clock
question
how do knee/chest stretches help in the treatment of short leg syndrome?
answer
helps general SI mobility and can help the piriformis - if knee is bought up to the opposite shoulder it will stretch the piriformis
question
what are the pelvic clock exercises best used for?
answer
best for addressing *lumbar sagittal plane postural decompression*
question
what is the stork test?
answer
pt stands on one leg while your hands are on their iliac crests - observe if the pelvis remains even
question
How do you test/fit a lift?
answer
- Do a gentle side shift (try to push your patient gently off balance)→ if they have a short leg → more unstable - Then give the lift→ do a pelvic shift again (or a little bit of rotation) - Also do a standing flexion test and a stork test (pick up 1 leg and evaluate stability) - Once again, give a lift and check again - This tells you how stable and how good the lift is - If the lift is good→ pt will be stable and leveled out - Another way to know if the lift is working after they've had it for a while: when supine, you want the legs to be asymmetrical legs and a balanced pelvis because that means that they are no longer having to compensate -If the pelvis is off →the lift is not high enough
question
what is the definition of a Structural model?
answer
the goal of the structural model is *biomechanical adjustment and the mobilization of joints*. This model also seeks to *address problems in the myofascial connective tissues, as well as in the bony and soft tissues, to remove restrictive forces and enhance motion*. This is accomplished by the use of a wide range of osteopathic manipulative techniques such as high velocity-low amplitude, muscle energy, counterstrain, myofascial release, ligamentous articular techniques and functional techniques.
question
what is the definition of a Respiratory-circulatory model?
answer
the goal of the respiratory-circulatory model is to* improve all of the diaphragm restrictions in the body*. Diaphragms are considered to be "transverse restrictors" of motion, venous and lymphatic drainage and cerebrospinal fluid. The techniques used in this model are *osteopathy in the cranial field, ligamentous articular strain, myofascial release and lymphatic pump techniques*.
question
what is the definition of a Metabolic model?
answer
the goal of the metabolic model is to *enhance the self-regulatory and self-healing mechanisms*, to foster energy conservation by balancing the body's energy expenditure and exchange,and to enhance immune system function, endocrine function and organ function. The osteopathic considerations in this area are *not manipulative in nature except for the use of lymphatic pump techniques*. Nutritional counseling, diet and exercise advice are the most common approaches to balancing the body through this model.
question
what is the definition of a Neurogenic model?
answer
the goal of the neurologic model is to *attain autonomic balance and address neural reflex activity, remove facilitated segments, decrease afferent nerve signals and relieve pain*. The osteopathic manipulative techniques used to influence this area of patient health include *counterstrain and Chapman reflex points*
question
what is the definition of a Behavioral model?
answer
the goal of this model is to *improve the biological, psychological and social* components of the health spectrum. This includes *emotional balancing and compensatory mechanisms*. Reproductive processes and behavioral adaption are also included under this model.
question
what is structural/bioenergetic?
answer
free motion of the associated structures allows for greater physiologic function Key point: *improving structural relationships actually decreases the physiologic work (energy expenditure) of breathing* - small studies have shown increased compliance, increased tidal volume and distribution of gas throughout the lung example: you can eliminate some of the work required for the pt to breath by eliminating structural somatic dysfunctions which can prolong the time before the pt needs to go on a ventilator
question
Respiratory circulation
answer
- the *diaphragm acts as a the piston* in the thoraco-abdomino-pelvic cylinder - descent of the diaphragm creates a relative negative intrathoracic pressure, causing the inflow of air as well as fluids in the low pressure circulatory system, bringing venous and lymphatic fluid back to central circulation
question
what does shallow breathing lead to?
answer
leads to ineffective movement of fluid in this low pressure circulatory system - *venous and lymphatic stasis* results in increased metabolic waste remaining in the tissues - *"Cellular Constipation"*
question
what is the function of the Cisterna Chyli? how does the diaphragm affect the function of the cisterna chyli?
answer
it *collects the lymph from the lower abdomen, pelvis and lower extremities* and is located just below the diaphragm - the *motion of the diaphragm helps to draw lymph superiorly* into the thoracic duct which then traveses the thoracic inlet - the motion of the abdominal viscera also promotes this fluid movement into the thorax
question
what lymphatic treatments are available and what lymphatic treatment should you start with?
answer
- typically start with the *thoracic inlet* to open the door before you try to start pushing fluid through it - rib raising - diaphragm doming - pedal pump - upper thoracic lymphatic pump - pectoral traction
question
Neurological model
answer
- autonomic imbalance plays a role in almost every disease process - don't think of sympathetic and parasympathetic systems as a see-saw
question
what is function OMT treatment of the autonomic nervous system, such as rib raising?
answer
Treatment is not aimed at "turning the system up or down" but at *providing a stimulus that allows the body to regulate itself*
question
Sympathetic influence
answer
mucosal and parenchymal irritation stimulate visceral afferents - *T2-T7* bombarded with info, facilitated to discharge easily - Bronchodilation is good, but local vasoconstriction is not
question
what does long term sympathetic hypertonia lead to?
answer
leads to increase goblet cells that make thicker more tenacious mucus
question
where are the sympathetic chain ganglia located?
answer
on the heads of the ribs - SD in that region will have direct effect on sympathetic activity
question
what can affect the sympathetic input?
answer
the sympathetic chain ganglia are covered with fascia that blends with the *radiate ligaments* over the rib heads - this fascial restriction can alter the functional environment of the sympathetic chain
question
Parasympathetic influence
answer
this is normally the dominant state - creates a higher ratio of ciliated cells - produces a thinner mucous which is more easily cleared
question
Facilitation
answer
Adaptive homeostasis mechanisms can go out of control, especially when there is chronically increased sympathetic tone and viscerosomatic reflexes - once a *segment become facilitated, its threshold for stimulation is much lower*, so that normal stimuli can trigger a disproportional response, long after the original insult is gone
question
what is the goal of neurogenic treatment?
answer
- reduce parenchyma congestion - reduce mechanical impediments to respiratory motion - restore balance to the autonomic nervous system and reduce sympathetic hyperreactivity to the lung tissues
question
Restoration of Autonomic balance
answer
- thinking in terms of the neurologic model, consider addressing this first prior to instituting any other treatment techniques - without down-regulating sympathetics, providing more stimulation to facilitated area of the cord may further increase sympathetic ton - *Start with gentle inhibition to upper thorax*
question
Primary trigger point
answer
contain nociceptor activity in the center of a muscle or a group of muscles, and is mainly responsible for the development of the myofascial pain
question
Secondary trigger point
answer
develops in synergist muscle of the affected muscle. An imbalance tension in the primary muscle, due to shortening muscle fibers, and compensatroy overload of teh synergist muscles cause secondary Tp sides to develop. secondary Tps can also form at muscle attachment sites in highly sensitized connective tissue
question
Satellite trigger point
answer
forms within the pain referral zone of another muscle containing a primary Tp. According to davies and davies "long term chronic pain is often a compound effect from a chain of satellite trigger points, cascading from muscle to muscles". Satellite trigger points can sometimes resolve independently if the primary Tp site is deactivated
question
Latent trigger pooint
answer
a site where nociceptors have become activated but not sensitized enough to cause pain. However, these area are painful and produce a 'jump sign' when the tissue is compressed above the latent site



