Pharmacotherapy of Pneumonia – Flashcards
Unlock all answers in this set
Unlock answersquestion
Identify pathogens commonly associated with community- acquired pneumonia.
answer
S. pneumoniae—most common Mycoplasma pneumoniae Chlamydia pneumoniae respiratory viruses (e.g., influenza, parainfluenza, respiratory syncytial virus)
question
Hospital-Acquired Pneumonia (HAP)
answer
Hospital-acquired (or nosocomial) pneumonia (HAP) is pneumonia that occurs 48 hours or more after admission and did not appear to be incubating at the time of admission. Hospital-acquired pneumonia (HAP) is the second most common hospital-acquired infection in the U.S., with high associated morbidity and mortality. The presence of HAP increased both hospital length of stay (by 7-9 days) as well as hospital costs ($40,000 per patient). HAP is responsible for up to 25% of ICU infections and more than 50% of the antibiotics prescribed. HAP is further classified based on time of onset and presence of these risk factors.
question
Identify pathogens commonly associated with hospital-acquired pneumonia.
answer
Streptococcus pneumoniae Haemophilus influenzae Methicillin-susceptible Staphylococcus aureus
question
Identify risk factors for drug resistance to S. pneumoniae.
answer
Age >65 years Beta-lactam, macrolide, or fluoroquinolone therapy within the past three to six months—macrolide resistance is more than 25% in the some regions of US. Do not use as monotherapy in those areas. Alcoholism Medical comorbidities Immunosuppressive illness or therapy Exposure to a child in a daycare center
question
multidrug-resistant pathogens
answer
• The definition of multidrug resistance in gram-negative bacilli, which are an important cause of HAP, VAP, and HCAP, is variably defined as resistance to at least two, three, four, or eight of the antibiotics typically used to treat infections with these organisms. • Extensively drug-resistant (XDR) gram-negative bacilli are defined by resistance to all commonly used systemic antibiotics except colistin, tigecycline, and aminoglycosides. • Awareness of local resistance patterns is critical for decisions regarding empiric therapy for HAP, VAP, and HCAP.
question
Identify risk factors for infection with multidrug-resistant pathogens in hospital-acquired pneumonia.
answer
Antimicrobial therapy in preceding 90 days Current hospitalization ≥ 5 days High frequency of antibiotic resistance in community or hospital unit Presence of risk factors for HCAP: Hospitalization for ≥ 2 days in the preceding 90 days Residence in nursing home or extended care facility Home infusion therapy (including antibiotics) Chronic dialysis within 30 days Home wound care Family member with multidrug-resistant pathogen Immunosuppressive disease and/or therapy
question
Select appropriate empiric antibiotic therapy for community- and hospital-acquired pneumonia based on clinical practice guidelines.
answer
Treatment (see algorithm at the end of the handout) • Treatment of uncomplicated pneumonia who do not require hospitalization, patients with no comorbidities, no recent antibiotic use and low rate of resistance use a macrolide antibiotic or doxycycline as monotherapy: • Azithromycin - • Clarithromycin • Clarithromycin XL • Doxycycline
question
Treatment of uncomplicated pneumonia who do not require hospitalization, patients with no comorbidities, no recent antibiotic use and low rate of resistance use a macrolide antibiotic or doxycycline as monotherapy:
answer
• Azithromycin • Clarithromycin • Clarithromycin XL • Doxycycline
question
Treatment of complicated pneumonia with comorbidities, recent antibiotic use, or high rate of resistance
answer
A respiratory fluoroquinolone (levofloxacin, moxifloxacin, or gemifloxacin) for five days. Combination therapy with a beta-lactam effective against S. pneumoniae (high-dose amoxicillin OR amoxicillin-clavulanate OR cefpodoxime OR cefuroxime PLUS either a macrolide (azithromycin OR clarithromycin OR clarithromycin XL) OR doxycycline. Treatment should be generally be continued for five days.
question
Indication to hospitalize
answer
The decision to hospitalize a child with CAP is individualized based upon age, underlying medical problems, and clinical factors including severity of illness. Hospitalization generally is warranted for infants younger than three to six months of age, unless a viral etiology or Chlamydia trachomatis is suspected and they are normoxemic and relatively asymptomatic. Hospitalization is also warranted for a child of any age whose family cannot provide appropriate care and assure compliance with the therapeutic regimen. Additional indications for hospitalization include: • Hypoxemia (oxygen saturation 70 breaths per minute for infants 50 breaths per minute for older children; retractions; nasal flaring; difficulty breathing; apnea; grunting • Toxic appearance (more common in bacterial pneumonia and may suggest a more severe course) • Underlying conditions that may predispose to a more serious course of pneumonia (e.g., cardiopulmonary disease, genetic syndromes, neurocognitive disorders), may be worsened by pneumonia, even viral pneumonia (e.g., metabolic disorder) or may adversely affect response to treatment (e.g., immunocompromised host) • Complications (e.g., effusion/empyema) • Suspicion or confirmation that CAP is due to a pathogen with increased virulence, such as Staphylococcus aureus or group A streptococcus • Failure of outpatient therapy (worsening or no response in 48 to 72 hours)
question
Infants younger than three to six months of age with suspected bacterial CAP or who are hypoxemic should be treated how?
answer
They should be admitted to the hospital for management. Afebrile infants one to four months of age who are thought to have afebrile pneumonia of infancy (e.g., Chlamydia trachomatis) can be treated in the outpatient setting if they are not hypoxemic and remain afebrile.
question
Empiric antibiotic therapy for CAP in children six months to five years of age who are thought to have bacterial pneumonia (e.g., abrupt onset, moderate to severe respiratory distress, and supportive laboratory data if obtained include coverage for what?
answer
Streptococcus pneumoniae
question
Identify groups at high risk for complications due to influenza infection.
answer
Rates of infection with influenza are highest among children. Rates of influenza complications, hospitalizations, and death are higher among those aged 65 and older, young children, and patients with medical conditions that predispose them to such complications (any age).
question
In infants and children six months and older, the usual duration of antimicrobial therapy is how long?
answer
five days for azithromycin and 7 to 10 days for other agents
question
Children who are treated for CAP as outpatients should have follow-up within what amount of time?
answer
24 to 48 hours Those whose condition has worsened at follow-up should be evaluated for potential complications and hospitalized.
question
Treatment of Children <5 years with CAP ---One to four months of age
answer
• In afebrile infants one to four months of age with CAP, the most likely bacterial pathogen is C. trachomatis. Infants who are thought to have afebrile pneumonia of infancy can be treated in the outpatient setting if they are not hypoxemic and remain afebrile • Erythromycin 50 mg/kg/d in 4 doses for 14 days • Azithromycin 20 mg/kg/day given 1 per day for 3 days
question
Treatment Six months to five years Viral:
answer
Suspected viral etiology — Viral etiologies very common during early childhood. Viral pneumonia (suggested by gradual onset, preceding upper respiratory tract symptoms, diffuse findings on auscultation, lack of toxic appearance should not be treated with antibiotics. Antiviral agents generally are not used for viral pneumonia in the outpatient setting. • Infants and young children with known or suspected chronic disease (e.g., cardiopulmonary disease, neuromuscular disease) are at increased risk for severe or complicated viral lower respiratory tract infection. If such children are not admitted to the hospital, they merit close monitoring in the outpatient setting. ● Suspected influenza - In children with suspected influenza who are at increased risk of complications, initiation of antiviral treatment is recommended as soon as possible.
question
What is the most frequent cause of "typical" bacterial pneumonia in children of all ages?
answer
Streptococcus pneumoniae is the most frequent cause of "typical" bacterial pneumonia in children of all ages
question
For children younger than five years who are thought to have bacterial CAP based upon clinical presentation, examination findings but do not require inpatient therapy, what is the recommended therapy?
answer
For children younger than five years who are thought to have bacterial CAP based upon clinical presentation, examination findings but do not require inpatient therapy, high dose amoxicillin is usually considered the drug of choice. Amoxicillin is preferred because it is effective against the majority of bacterial pathogens for CAP in this age group, is well tolerated, and is inexpensive. The higher dose of amoxicillin is suggested because of the concern for antibiotic-resistant S. pneumoniae isolated from patients with community-acquired respiratory tract infections. Twice daily dosing for pneumonia due to a S. pneumoniae isolate with an MIC of 2 mcg/mL is predicted to achieve a clinical and microbiologic cure in only 65 percent of children, whereas the same total daily dose divided in three equal portions is predicted to achieve a cure in 90 percent.
question
Treatment For children with non-type 1 hypersensitivity reactions to penicillin:
answer
For children with non-type 1 hypersensitivity reactions to penicillin a second- or third-generation cephalosporin (e.g., cefdinir) is an acceptable alternative to amoxicillin. • For the infant or child who is suspected to have bacterial CAP and is unable to tolerate liquids at the time of presentation, a single initial dose of ceftriaxone (50 to 75 mg/kg) may be administered intramuscularly or intravenously before starting oral antibiotics
question
Treatment for children with type 1 hypersensitivity reactions to penicillin:
answer
For children with type 1 hypersensitivity reactions to penicillin, clindamycin or a macrolide may be used.
question
Suspected atypical pneumonia — in children
answer
Mycoplasma pneumoniae and Chlamydophila pneumoniae are less common than S. pneumoniae in children younger than five years with CAP. However, they can occur in this age group and should be considered in children without a pneumonia-associated complication who fail to improve after 48 to 72 hours of empiric therapy for S. pneumoniae (e.g., amoxicillin), at which time a macrolide could be added or substituted
question
Treatment of Children ≥5 years with CAP
answer
A. Suspected typical or atypical bacterial etiology — S. pneumoniae is the most frequent cause of "typical" bacterial pneumonia in children of all ages. However, in otherwise healthy children five years and older with CAP who are not ill enough to require hospitalization, M. pneumoniae and C. pneumoniae are the most likely pathogens • Macrolide antibiotics for initial empiric therapy for CAP in children older than five years who are treated as outpatients • Among the macrolide antibiotics, clarithromycin and azithromycin have a more convenient dosing schedule and fewer side effects than erythromycin • Macrolide antibiotics may provide coverage for S. pneumoniae, which is the most frequent typical bacterial pathogen for all age groups. However, approximately 40 to 50 percent of S. pneumoniae isolates are resistant to macrolides. Failure to respond to macrolide therapy may indicate the development of a complication, a macrolide-resistant pathogen, and/or the need to alter therapy to provide better pneumococcal coverage. • Given the significant resistance of S. pneumoniae to macrolides, fluoroquinolones (e.g., levofloxacin, moxifloxacin) are another reasonable alternative for the outpatient treatment of CAP.
question
Empiric antibiotic therapy for CAP in children ≥5 years should include coverage for what?
answer
atypical bacteria
question
What is the most frequent cause of "typical" bacterial pneumonia in children of all ages?
answer
Streptococcus pneumoniae
question
Identify candidates for prevention and/or treatment of influenza with antiviral drugs (oseltamivir [Tamiflu®], zanamivir [Relenza®], or peramivir [Rapivab®]).
answer
— Initiation of antiviral treatment for influenza (e.g., oseltamivir) as soon as possible is recommended for children with suspected influenza who are at high risk for complications of influenza pneumonia; laboratory confirmation should not delay initiation of antiviral therapy.
question
Identify candidates for the influenza vaccine and select the most appropriate vaccine formulation.
answer
Annual vaccination is recommended for all persons 6 months or older (in the absence of contraindications) Children younger than 8 years old may require 2 vaccine doses
question
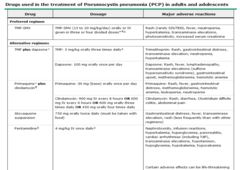
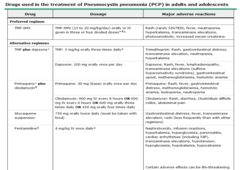
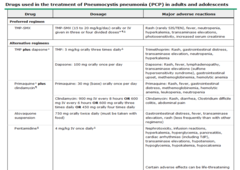
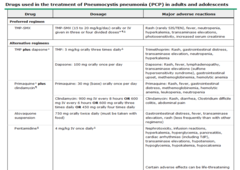
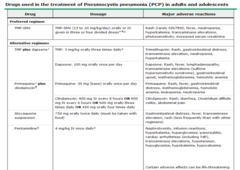
Given a patient with PCP pneumonia with mild, moderate or severe disease, choose the appropriate antibiotic and whether or not corticosteroids are indicated.
answer
Corticosteroids • Corticosteroids should be administered concurrently with anti-Pneumocystis therapy in this setting to decrease the incidence of mortality and respiratory failure associated with PCP. • Administer to patients with moderate to severe disease
question
Given a patient with PCP pneumonia select the appropriate timing of ART
answer
For patients with PCP who are not receiving ART at the time of their diagnosis, ART (anti-retroviral therapy) should be initiated within two weeks of PCP treatment. Early ART (versus starting therapy after PCP treatment) can reduce the risk of AIDS progression and death in patients presenting with PCP.
question
Given a patient with PCP pneumonia with mild disease, choose the appropriate antibiotic and whether or not corticosteroids are indicated.
answer
• A-a O2 gradient <35 mmHg and/or a partial pressure of arterial oxygen ≥70 mmHg -- Oral antibiotic therapy with trimethoprim-sulfamethoxazole (TMP-SMX) unless there is a concurrent infection or comorbidity that would impact absorption -- Standard dose TMP-SMX is 15-20 mg/kg/day orally or IV in 3 to 4 divided doses for 21 days. -- Alternative antibiotics (See Table at the end of handout): -- trimethoprim-dapsone, -- clindamycin-primaquine, -- atovaquone—used only in mild disease. -- Test for glucose-6-phosphate dehydrogenase (G6PD) deficiency when using a regimen that contains dapsone or primaquine since patients with G6PD deficiency are at risk for developing hemolytic anemia when exposed to these agents. Patients with G6PD deficiency and mild disease should receive atovaquone. For those with G6PD deficiency and moderate disease, the decision to use atovaquone, desensitize to TMP-SMX, or switch to IV therapy with pentamidine depends upon the severity of their disease and their past reaction to TMP-SMX. Although it is best if G6PD results are available prior to initiating treatment, therapy may be initiated simultaneously with testing as the risk for this deficiency is quite low. --- Corticosteroids are not required
question
Given a patient with PCP pneumonia with moderate disease, choose the appropriate antibiotic and whether or not corticosteroids are indicated.
answer
• A-a O2 gradient ≥35 and <45 mmHg and/or a partial pressure of arterial oxygen ≥60 and <70 mmHg --Oral antibiotic therapy with trimethoprim-sulfamethoxazole (TMP-SMX) unless there is a concurrent infection or comorbidity that would impact absorption -- Alternative antibiotics (See Table at the end of handout): -- trimethoprim-dapsone, -- clindamycin-primaquine -- Clindamycin can be administered intravenously at a dose of 600 mg every six hours or 900 mg every eight hours. Primaquine base is given orally at a dose of 30 mg daily. Patients should be tested for G6PD when initiating this regimen since patients with G6PD deficiency are at risk for developing hemolytic anemia when exposed to primaquine. -- Corticosteroids ARE required
question
Given a patient with PCP pneumonia with severe disease, choose the appropriate antibiotic and whether or not corticosteroids are indicated.
answer
-- A-a O2 gradient is ≥45 mmHg, the partial pressure of arterial oxygen is <60 mmHg, and/or there is potential for fatigue leading to respiratory failure (e.g., a high respiratory rate or a partial pressure of arterial carbon dioxide that is normal or higher than normal in a patient with hypoxia). -- IV antibiotic therapy with trimethoprim-sulfamethoxazole (TMP-SMX) unless there is a concurrent infection or comorbidity that would impact absorption. Continue until patient is clinically stable (PaO2 ≥60 mmHg, respiratory rate <25) and able to take oral antibiotics. -- Alternative antibiotics (See Table at the end of handout): -- Pentamidine for patient who have a sulfa allergy -- IV dose of 4 mg/kg daily -- Avoid in patients with renal insufficiency CrCl <60 mL/min -- Avoid in patients with concurrent pancreatitis -- Corticosteroids required
question
Given a patient with PCP pneumonia select the appropriate timing of secondary prophylaxis.
answer
After completing their initial 21-day course of treatment, patients should continue to receive antimicrobial therapy at a reduced dose to prevent recurrent infection (i.e., secondary prophylaxis). Secondary prophylaxis can be discontinued in patients receiving ART if they have an undetectable viral load and a rise in their CD4 count to ≥200 cells/microL for at least three months.
question
Select the correct statement regarding the need for G6PD testing in patients needing dapsone or primaquine therapy and the possible adverse reactions.
answer
-- Test for glucose-6-phosphate dehydrogenase (G6PD) deficiency when using a regimen that contains dapsone or primaquine since patients with G6PD deficiency are at risk for developing hemolytic anemia when exposed to these agents. Patients with G6PD deficiency and mild disease should receive atovaquone. For those with G6PD deficiency and moderate disease, the decision to use atovaquone, desensitize to TMP-SMX, or switch to IV therapy with pentamidine depends upon the severity of their disease and their past reaction to TMP-SMX. Although it is best if G6PD results are available prior to initiating treatment, therapy may be initiated simultaneously with testing as the risk for this deficiency is quite low.
question
Clinical Overview
answer
Pneumonia results from microorganism invasion of the lower airways with associated local and systemic symptoms. Organisms gain entry into this normally sterile environment via inhalation of aerosolized microorganisms, aspiration, or spread from the blood to the lungs. Pneumonia is classified based on site of acquisition and/or patient risk factors.
question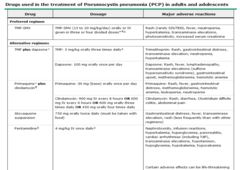
Given patient with PCP pneumonia, match the adverse reaction with the patient's antibiotic therapy. --TMP-SMX
answer
- Adverse reactions to TMP-SMX are common in patients being treated for PCP . Reactions can range from mild to severe and include gastrointestinal intolerance, photosensitivity, rash, and fever. Laboratory testing can reveal leukopenia and marked hyperkalemia, as well as evidence of acute kidney injury and hepatotoxicity . Sulfonamides should be immediately discontinued if any of the following conditions are present: -- Persistent rash and/or fever for more than five days -- Absolute neutrophil count <500 cells/mm3 -- Hypotension -- Intractable hyperkalemia -- Fever and flu-like symptoms, followed by conjunctival irritation, mucous membrane involvement, painful skin, target lesions, blistering, or desquamation of the skin
question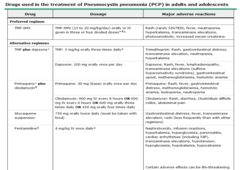
Atovaquone — side effects
answer
The most common side effect is gastrointestinal distress. Other adverse reactions include fever and transaminase elevations. Rash may also occur, but is less common than with other regimens.
question
Community-Acquired Pneumonia (CAP)
answer
an acute infection of the pulmonary parenchyma in a patient who has acquired the infection in the community.
question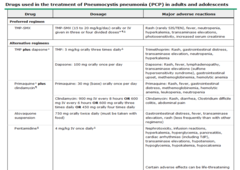
Given patient with PCP pneumonia, match the adverse reaction with the patient's antibiotic therapy. --TMP-dapsone -
answer
Side effects of TMP-dapsone include gastrointestinal upset, rash, fever, hemolytic anemia, and methemoglobinemia. Laboratory testing can also reveal neutropenia, hyperkalemia, and transaminase elevations. An interaction between trimethoprim and dapsone appears to increase the levels of both drugs in patients being treated for PCP, and this may increase the risk of side effects such as anemia and methemoglobinemia
question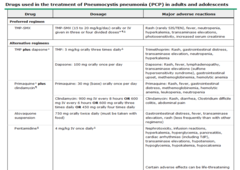
Clindamycin-primaquine - Side effects
answer
include rash, fever, diarrhea (including Clostridium difficile-associated colitis), hemolytic anemia, neutropenia, and methemoglobinemia.
question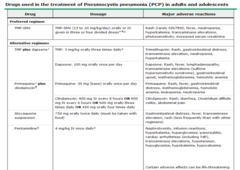
Pentamidine — Adverse reactions
answer
occur in up to 70 percent of patients and include nausea, taste disturbance, cardiac arrhythmias, hyperkalemia, nephrotoxicity, pancreatitis, hypokalemia, hypocalcemia, hypoglycemia, and hyperglycemia. Patients can develop permanent insulin-requiring diabetes mellitus after treatment with pentamidine. The nephrotoxicity of pentamidine is cumulative and is usually evidenced by a gradual increase in the creatinine concentration over the course of therapy. Concomitant use of other nephrotoxic drugs such as amphotericin B and aminoglycosides potentiate the renal toxicity of pentamidine. Certain adverse events, particularly hypoglycemia and hypotension, may be life threatening.
question
Identify the monitoring parameters to detect or to prevent adverse reactions due to antibiotic treatment for PCP pneumonia.
answer
-- Outpatient monitoring: after one week of therapy schedule follow up for clinical assessment and obtain laboratory testing. At that visit, we measure the oxygen saturation; obtain a complete blood count, and measure renal function, electrolytes, and aminotransferase levels. -- Hospitalized patients: monitor complete blood counts, electrolytes, and liver function tests at least two to three times per week. -- Individuals receiving pentamidine should have renal function, glucose, calcium, and electrolyte concentrations monitored daily; such patients should be switched to a less toxic regimen as soon as they can tolerate oral therapy.



