Hematology NCLEX style questions – Flashcards
Unlock all answers in this set
Unlock answersquestion
In evaluating a young woman, the following laboratory result the nurse recognizes as abnormal is a. hemoglobin 13 g/dl. b. platelet count 20,000/mm3. c. red blood cell count 5 million/mm3. d. white blood cell count 6000/mm3.
answer
ANS: B Normal platelet count is 150,000/mm3.
question
A client has a hematocrit (Hct) of 30%. The nurse interprets this to mean a. 30% of the blood will be plasma and plasma products. b.bleeding disorders are possible. c. the blood is viscous and concentrated. d. the individual has fewer red blood cells than normal.
answer
ANS: B Hematocrit measures the percent volume of red cells in whole blood. The normal value in adult women is 37% to 45%.
question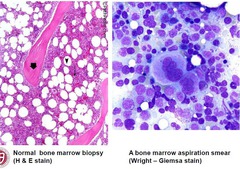
A nurse is explaining that a bone marrow biopsy is done to evaluate??
answer
The biopsy reveals the number, size, and shape of the RBCs, WBCs, and platelet precursors. This can diagnose disorders such as aplastic anemia, leukemia, pernicious anemia, and thrombocytopenia.
question
The laboratory test result that would be most helpful to the nurse in the assessment of a client with a bleeding disorder is
answer
Platelet count--it is a key role in blood clotting. An abnormal platelet count would indicate bleeding problems originating from a platelet disorder.
question
A client has severe anemia and is being treated with transfusion therapy. The nurse should be alert for a complication of transfusion, such as a. flank pain. b. hearing loss. c. liver damage.
answer
ANS: A Reactions to blood products include fever, chills, back or flank pain, shock, wheezing, headache, vomiting, or urticaria (hives).
question
The nurse is monitoring the laboratory test results for a client receiving anticoagulation therapy. The nurse is aware that the International Normalized Ratio (INR) for most clinical conditions requiring anticoagulation is (NOTE: keywords "receiving anticoag therapy!) a.less than 1. b. 1 to 2. c. 2 to 3.5.
answer
ANS: C For most clinical conditions that necessitate anticoagulation, the recommended INR is 2 to 3.5.
question
A nurse is conducting a wellness seminar on healthy eating and prevention of iron deficiency anemia. The food the nurse would describe as being high in iron is a.citrus fruits. b.grains. c.green leafy vegetables. d.milk products.
answer
ANS: C Encourage foods cooked in iron pots and ingestion of foods such as liver (the richest source), oysters, lean meats, kidney beans, whole wheat bread, kale, spinach, egg yolk, turnip tops, beet greens, carrots, apricots, and raisins.
question
The nurse recognizes that the laboratory finding indicative of polycythemia vera is a. erythrocyte count of 5 million/mm3. b. hemoglobin level of 22 g/100 ml. c. leukocyte count of 6000/mm3. d. platelets of 50,000/mm3.
answer
ANS: B Diagnostic findings include RBC count as high as 8 to 12 million/mm3, hemoglobin level of 18 to 25 g/dl, and a hematocrit level greater than 54% in men and 49% in women. **break down the word poly=many, cy=cell, emia=blood vera=vicous---think ALOE VERA!***
question
The nurse assessing a client with sickle cell anemia would recognize the common manifestation of the disease is a. confusion. b. diarrhea. c. hypertension. d. leg ulcers.

answer
ANS: D Leg ulcers are found in about 75% of older children and adults with the disease. Diarrhea is not seen. The most common cardiovascular manifestation is heart failure. Stroke is a common neurologic outcome.
question
The nursing intervention that is the priority when preparing to administer blood is a. administration of pretransfusion antihistamines. b. asking a second health care professional to confirm blood acceptability. c. establishing baseline vital signs. d. obtaining a written order for the transfusion.
answer
ANS: B All options are reasonable. Baseline vitals are important to compare against subsequent ones. There will be a written order for the transfusion at some point; either the physician or the nurse will write the order. Some clients will need premedication before a transfusion, but the most critical phase of transfusion is confirming product compatibility and verifying client identity. Most transfusion reactions can be traced to improper product-to-patient identification. Two professional nurses are required to perform that task.
question
The nurse can decrease the danger of transfusion reactions in a client by a. adding sterile saline to the blood transfusion. b.forcing fluids. c.infusing the blood slowly during the first 15 minutes. d.monitoring the urine output.
answer
ANS: C It is recommended that the transfusion begin slowly and that the client be closely monitored. If no evidence of a reaction is noted within the first 15 minutes, flow can then be increased to the prescribed rate.
question
The nurse is caring for a patient with chronic kidney disease. On reviewing the patient's laboratory results, the nurse finds that the red blood cell (RBC) count is greatly reduced. Which drug does the nurse anticipate the health care provider prescribing?
answer
The patient will likely be prescribed a synthetic erythropoietin like epoetin alfa to stimulate the production of RBCs. The patient has chronic kidney disease and is unable to produce adequate amounts of the hormone erythropoietin.
question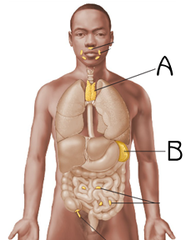
The spleens functions by....
answer
destroying old or imperfect red blood cells (RBCs), breaks down hemoglobin released from these destroyed cells, stores platelets, and filters antigens.
question
A patient with leukemia has a platelet count of 7000/mm3. Which intervention does the nurse implement to prevent injury?
answer
Patients with low platelet counts are at risk for bleeding; the patient should not have rectal temperatures, strain at stool, or retain hard stool. If injured, the patient should apply ice to promote vasoconstriction and lessen bleeding.
question
What does a high reticulocyte count indicate in regards to red blood cells (RBCs)?
answer
A high reticulocyte count indicates that immature RBCs are being released from the bone marrow to overcome blood loss. A high reticulocyte count is desirable in a patient after hemorrhage.
question
The nurse is reinforcing information about genetic counseling to a patient with sickle cell disease (SCD) who has a healthy spouse. What information does the nurse include?
answer
The children of the patient with sickle cell disease will inherit the sickle cell trait, but may not inherit the disease. If both parents have the sickle cell trait, their children could get the disease.
question
What should be a major focus in a teaching plan for a teenager with sickle cell anemia? a. Limit tobacco use to no more than two cigarettes a day. b. Eat foods high in iron and vitamin B. c. Maintain environmental temperature at 65° F to 68° F. d. Maintain adequate hydration.
answer
ANS: D The maintenance of adequate fluid intake (4-6 L/day) prevents hemoconcentration. The use of alcohol and tobacco are contraindicated for the patient with sickle cell anemia as the cause vasoconstriction. Warm environments are more therapeutic as warm environments do not cause vasoconstriction.
question
Which is considered an approximate normal hematocrit value?
answer
Hematocrit is approximately three times the hemoglobin value.
question
What is the rationale for administering injections of vitamin B12 to patients with pernicious anemia? a. The patient's body does not normally manufacture enough vitamin B12. b. The patient may lack the intrinsic factor necessary for vitamin B12 absorption. c. Vitamin B12 is found in very small quantities in the patient's body.
answer
ANS: B The patient with pernicious anemia lacks the intrinsic factor, found in the stomach, which is essential for vitamin B12 absorption. (common in gastric bypass pt due to that portion of stomach being removed-they need b12 the rest of their life!)
question
Which foods should a nurse include in a nutrition teaching plan for a patient with iron-deficiency anemia? a. Beans and dried fruit b. Apples and white rice c. Yogurt and cooked carrots d. Yellow squash and tortillas
answer
ANS: A Iron-rich foods include beans, dried fruit, liver, red meat, fish, and whole-grain breads.
question
A 35-year-old man is examined in an urgent care clinic. His presenting symptoms suggest polycythemia vera. Which extreme laboratory value would confirm this possible diagnosis? a. High hemoglobin level b. Low white cell count c. Low platelet count d. High iron level
answer
ANS: A The symptoms of polycythemia vera are extremely high hemoglobin and hematocrit values because of the excessive production of red blood cells. Patients with polycythemia vera have 1 pint of blood taken from them until the blood values become more normal. The blood is collected as it would be for a blood donation, but it cannot be used for transfusion purposes.
question
What should a nurse be careful to observe for when assessing a patient with thrombocytopenia? a. Distended neck veins and skin discoloration b. Discoloration of the nails and sclera c. Petechiae on the skin and bleeding gums
answer
ANS: C Symptoms of thrombocytopenia include petechiae, purpura, bleeding gums, and epistaxis.
question
A nurse is assessing a patient 20 minutes after a bone marrow biopsy. Which statement by the patient is cause for the most concern? a. "There is fresh blood on my dressing." b. "I am thirsty." c. "My hip feels bruised where they stuck the needle." d. "I had a sharp pain in my leg when they pulled the needle out."
answer
ANS: A Fresh blood on the pressure dressing 20 minutes after the aspiration needs to be addressed. Usually, redressing with a pressure dressing and an ice pack is sufficient. Feelings of bruising and pain on extraction are to be expected. Thirst is of no clinical significance.
question
At 1000 a nurse receives 2 units of blood for a patient to be transfused. What is the most appropriate nursing action? a. Set up 1 unit for the infusion to start by 1030 and send the other unit back until the first one has infused b. Set up both units to infuse at the same time and to start at 1100. c. Set up one unit for infusion and place the other in the refrigerator for the later infusion. d. Send both units back and ask for a reissue of 1 unit only.
answer
ANS: A Blood must be started within 30 minutes of its receipt after it has been checked by two licensed staff members. In many settings, licensed practical nurses do not start the blood but can set up the infusion. The best option is to send the second unit back immediately, with an explanation that it will be called for later. One unit of blood usually takes about 2 to 4 hours to infuse.
question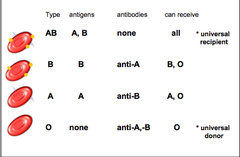
"The client with O+ blood is in need of an emergency transfusion but the lab does not have any O+ blood available. Which potential unit of blood could be given to the client?
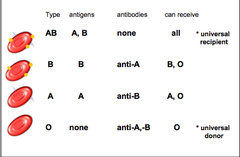
answer
O- negative blood is considered the universal donor because it does not contain the antigens A, B, or Rh. (AB+ is considered the universal recipient because a person with this blood type has all the anti-gens on the blood).
question
Red blood cells only live about _____ days.
answer
approximately 120 days.
question
When the patient with pernicious anemia says, "I don't know why I am so tired," the nurse can clarify by saying that the fatigue is related to:
answer
The fatigue experienced by people with anemia is related to the lack of oxygenation due to the lack of RBCs to carry the oxygen.
question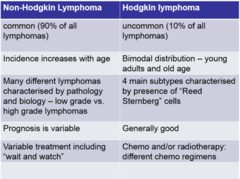
Non Hodgkins Lymphoma
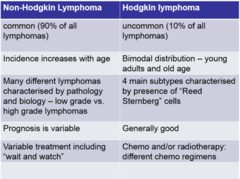
answer
Associated with auto immune disorders, HIV, transplants or from immunosuppressive drugs Enlarged spleen It can orginate in any lymph node tissue, it tends to spread early and unpredicably ot other lymph node tissues. (Considered non-treatable!)
question
What are the manifestations of hodgkins disease? **more common in teens and young adults and adults in 50s and 60s)
answer
Large painless nodes, fever >105, drenching night sweets, unexplained wt. loss. Most treatable & potentially curable (vs non Hodgkins) Reed-Sternberg cells occur with Hodgkin's disease.
question
A patient with anemia asks, "Why am I feeling tired all the time?" How does the nurse respond? "How many hours are you sleeping at night?" "You are not getting enough iron." "You need to rest more when you are sick." "Your cells are delivering less oxygen than you need."
answer
"Your cells are delivering less oxygen than you need." The single most common symptom of anemia is fatigue, which occurs because oxygen delivery to cells is less than is required to meet normal oxygen needs. Although assessment of sleep and rest is good, it does not address the cause related to the diagnosis. While it may be true that the patient isn't getting enough iron, it does not relate to the patient's fatigue. The statement about the patient needing rest because of being sick is simply not true.
question
The nurse is conscientious in the care of the feet and legs of a patient with sickle cell anemia because: a. stasis ulcers are a constant threat. b. bleeding may occur on the soles of the feet. c. edema of the feet increases activity intolerance.
answer
ANS: A Because of the sluggish flow of blood, stasis ulcers are a constant threat and are very difficult to heal.
question
The nurse is teaching a client with vitamin B12 deficiency anemia about dietary intake. Which type of food does the nurse encourage the client to eat? Dairy products Grains Leafy vegetables Starchy vegetables
answer
Dairy products such as milk, cheese, and eggs will provide the vitamin B12 that the client needs. Grains, leafy vegetables, and starchy vegetables are not a source of vitamin B12.
question
Which client is at greatest risk for having a hemolytic transfusion reaction? A 34-year-old client with type O blood A 42-year-old client with allergies A 58-year-old immune-suppressed client
answer
34 year old=. Type O is considered the universal donor, but not the universal recipient. Hemolytic transfusion reactions are caused by blood type or Rh incompatibility. When blood that contains antigens different from the client's own antigens is infused, antigen-antibody complexes are formed in the client's blood The client with allergies would be most susceptible to an allergic transfusion reaction. The immune-suppressed client would be most susceptible to a transfusion-associated graft-versus-host disease.
question
The nurse is educating a group of young women who have sickle cell disease (SCD). Which comment from a class member requires correction? **KEY WORDS-require correction** "Frequent handwashing is an important habit for me to develop." "Getting an annual 'flu shot' would be dangerous for me." "I must take my penicillin pills as prescribed, all the time." "The pneumonia vaccine is protection that I need."
answer
** "Getting an annual 'flu shot' would be dangerous for me." ** would require correcting the SCD patient. The client with SCD SHOULD receive annual influenza and pneumonia vaccinations; this helps prevent the development of these infections, which could cause a sickle cell crisis. Handwashing is a very important habit for the client with SCD to develop because it reduces the risk for infection. Prophylactic penicillin is given to clients with SCD orally twice a day to prevent the development of infection.
question
The nurse understands that the client with pernicious anemia will have which distinguishing laboratory findings?

answer
Lack of the intrinsic factor, which results from atrophy of the stomach wall or surgery to the stomach. Without the intrinsic factor, vitamin B12 cannot be absorbed in the small intestines, and folic acid needs vitamin B12 for DNA synthesis of RBCs **Vitamin B12 combines with intrinsic factor in the stomach and is then carried to the ileum, where it is absorbed in the bloodstream. So if there is removal of ileum you will have the same issue as it cannot be absorbed!)
question
The nurse devises a teaching plan for the patient with aplastic anemia. Which of the following is the most important concept to teach for health maintenance? aplastic anemia is a RARE condition in which the body stops producing enough new blood cells. Aplastic anemia decreases the bone marrow production of RBCs, WBCs, and platelets.
answer
Clients with aplastic anemia are severely immunocompromised and at risk for infection and possible death related to bone marrow suppression and pancytopenia. Strict aseptic technique and reverse isolation are important measures to prevent infection.
question
A client comes into the health clinic 3 years after undergoing a resection of the terminal ileum complaining of weakness, shortness of breath, and a sore tongue. Which client statement indicates a need for intervention and client teaching? "I have been drinking plenty of fluids." "I have been gargling with warm salt water for my sore tongue." "I have 3 to 4 loose stools per day." "I take a vitamin B12 tablet every day."
answer
"I take a vitamin B12 tablet every day." Vitamin B12 combines with intrinsic factor in the stomach and is then carried to the ileum, where it is absorbed in the bloodstream. In this situation, vitamin B12 cannot be absorbed regardless of the amount of oral intake of sources of vitamin B12 such as animal protein or vitamin B12 tablets. Vitamin B12 needs to be injected every month, because the ileum has been surgically removed.
question
A client is to receive epoetin (Epogen) injections. What laboratory value should the nurse assess before giving the injection? Hematocrit Partial thromboplastin time Hemoglobin concentration INR
answer
**Hematocrit**: Epogen is a recombinant DNA form of erythropoietin, which stimulates the production of RBCs and therefore causes the hematocrit to rise. The elevation in hematocrit causes an elevation in blood pressure; therefore, the blood pressure is a vital sign that should be checked
question
When a client is diagnosed with aplastic anemia, the nurse monitors for changes in which of the following physiological functions? Bleeding tendencies Intake and output Peripheral sensation Bowel function
answer
The client is at risk for bruising and* bleeding tendencies*
question
Of the following blood components, WHAT is decreased? Anemia Granulocytopenia Leukopenia Thrombocytopenia
answer
Anemia is defined as a decreased number of erythrocytes (red blood cells). Leukopenia is a decreased number of leukocytes (white blood cells). Thrombocytopenia is a decreased number of platelets. Granulocytopenia is a decreased number of granulocytes (a type of white blood cells)
question
Which of symptoms are expected with hemoglobin of 10 g/dl?
answer
Mild anemia usually has no clinical signs. Palpitations, SOB, and pallor are all associated with severe anemia.
question
Which of the following diagnostic findings are most likely for a client with aplastic anemia? Decreased production of T-helper cells Decreased levels of white blood cells, red blood cells, and platelets Increased levels of WBCs, RBCs, and platelets Reed-Sternberg cells and lymph node enlargement
answer
*Decreased levels of white blood cells, red blood cells, and platelets*In aplastic anemia, the most likely diagnostic findings are decreased levels of all the cellular elements of the blood (pancytopenia). T-helper cell production doesn't decrease in aplastic anemia. Reed-Sternberg cells and lymph node enlargement occur with Hodgkin's disease.
question
A client with iron deficiency anemia is scheduled for discharge. Which instruction about prescribed ferrous gluconate therapy should the nurse include in the teaching plan? "Take the medication with an antacid." "Take the medication with a glass of milk." "Take the medication with cereal." "Take the medication on an empty stomach."
answer
Preferably, ferrous gluconate should be taken on an empty stomach. Ferrous gluconate should not be taken with antacids, milk, or whole-grain cereals because these foods reduce iron absorption.
question
The nurse explains that, in the event of a massive hemorrhagic episode, the _____ contracts and adds blood to the circulating volume.
answer
spleen
question
When doing discharge teaching for a patient who has had an emergency splenectomy following an automobile accident, the nurse will teach the patient about the increased risk for a. infection. b. lymphedema. c. chronic anemia. d. prolonged bleeding.
answer
ANS: A Splenectomy increases the risk for infection, especially with gram-positive bacteria. The risks for lymphedema, bleeding, and anemia are not increased after splenectomy.
question
Which clinical manifestation is common to all types of anemia regardless of cause or pathologic mechanism? a. Jaundiced sclera and roof of the mouth b. Hypertension and peripheral edema c. Tachycardia at basal activity levels d. Increased PaCO2
answer
ANS: C The client with anemia has some degree of tissue hypoxia. A compensatory mechanism to increase tissue oxygenation is to increase cardiac output by increasing heart rate.
question
Which laboratory value in a client alerts the nurse to the probability of sickle cell disease? a. Hgb A1: 97% b. Hgb F: 1.5% c. Hgb C: 0% d. Hgb S: 65%
answer
ANS: D Normal values for Hgb S should be 0%. Clients with an Hgb S value higher than 43% are considered to have sickle cell disease.
question
The client in sickle cell crisis has effective pain management. What is now the priority nursing diagnosis? a. Deficient Knowledge related to contraception and pregnancy options b. Deficient Knowledge related to prevention of crisis episodes c. Risk for Injury related to decreased tissue oxygenation d. Risk for Infection related to decreased spleen function
answer
ANS: C During sickle cell crisis, when cells are sickled, blood flow is obstructed in the microcirculation and macrocirculation. Depending on which tissue is hypoxic or anoxic, ischemia can lead to tissue injury and cell death.
question
Which intervention for the client with sickle cell disease prevents vascular occlusion? a. Assessing pulse oximetry every 2 hours b. Administering morphine sulfate every 6 hours c. Keeping the room temperature at or below 68o F. d. Maintaining an oral fluid intake of at least 4500 mL/day
answer
ANS: D Venous stasis causes vascular occlusion. Maintaining hydration prevents venous stasis and vascular occlusion
question
In adults, bone marrow is usually aspirated from which area? a. post iliac crest b. sternum c. rib d. vertebrae
answer
a. post iliac crest
question
A client with anemia has been admitted to the medical-surgical unit. Which assessment findings are characteristic of iron deficiency anemia? a. night sweats, weight loss, diarrhea b. nausea, vomiting, anorexia c. itching, rash, jaundice d. dyspnea, tachycardia, pallor
answer
d. Dyspnea, tachycardia, and pallor
question
A client is seen in the emergency department with severe pain related to a sickle cell crisis. What does the nurse understand is occurring with this client? a. decreased pain tolerance b. overhydration c. Vascular occlusion in small vessels decreasing blood and oxygen to the tissues.
answer
Vascular occlusion in small vessels decreasing blood and oxygen to the tissues.
question
James is a 25-year-old African American male, hospitalized with sickle cell anemia on the hematology floor where you practice nursing. You are preparing a teaching plan to review with James and his family. Which of the following interventions will you include? Select all that apply. Never exceed the recommended dosages of analgesics. Dress warmly in cold temperatures. While participating in physical exercise, wear constrictive clothing to support circulation. Decrease fluid intake
answer
Never exceed the recommended dosages of analgesics. Dress warmly in cold temperatures. (due to vasoconstriction in cold weather!) While participating in physical exercise, wear constrictive clothing to support circulation. **pt with SCD must increase fluid intake of at least 4500 mL/day**
question
A patient with abdominal injuries from a motor vehicle crash is scheduled for surgery to remove the spleen. What bodily function will be affected by the removal of this organ? a. Filtration of waste products b. Removal of old red blood cells from circulation c. Clearance of mucous in the tracheobronchial tree d. Facilitation of glucose to be used by the cell for energy
answer
b. Removal of old red blood cells from circulation
question
Hemophilia A is a deficiency of Factor ___ and accounts for __% of cases?
answer
Factor VIII (a clotting protein in protein) 80%



