Hematology Exam 3 Week 12 – Flashcards
Unlock all answers in this set
Unlock answersquestion
Chronic Myeloproliferative Disorders (CMPD)
answer
- heterogeneous group of acquired clonal disorders - excessive proliferation of progenitor cells - associated increase in corresponding cell types in peripheral blood - splenomegaly, extramedullary hematopoiesis - associated w/ genetic abnormalities features: hyperplasia, most common in adults
question
4 major types of CMPD
answer
► Chronic myelogenous leukemia (CML) - Granulocytic hyperplasia ► Polycythemia vera (PV) - Erythroid hyperplasia - already covered ► Essential thrombocythemia (ET) - Megakaryocyte increases ► Chronic idiopathic myelofibrosis (IMF) *each are associated w/ hyperplasia of a specific cell type, except IMF
question
Chronic Idiopathic Myelofibrosis (IMF)
answer
- NO hyperplasia of a specific cell type - instead, there is early increase in all cell types - but as an unexplained fibrosis takes over the bone marrow in later disease, pancytopenia can result
question
CMPD transitions between diseases and reason why
answer
- CML can convert to AML or ALL - ET is precursor of AML or PV - PV convert to AML or IMF - most likely because the hematopoietic stem cells that have the genetic abnormality can change their developmental or lineage decisions to give rise to a different cell type as the disease progresses *hematopoietic stem cell is target of genetic mutation*
question
Chronic Myelogeneous Leukemia (CML)
answer
- correlates with Philadelphia chromosome - Abnormal chromosome 22 - t(9;22) translocation - unique fusion gene called BCR-ABL - marked increase in PB granulocytes - granulocyte hyperplasia of the bone marrow - 20% of adult leukemia cases - always acquired, never congenital *basophilia is hallmark BCR-ABL always in present, but Ph22 isn't diagnostic bc found in ALL and AML
question
BCR-ABL
answer
- protein that is the result of a fusion between the ABL-1 gene on chromosome 9 and the BCR, which stands for break cluster region, on chromosome 22 - induces clonal stem cell disorder - novel fusion protein with tyrosine kinase activity - aberrant activation of cell signaling pathways - induces abnormal cell growth
question
3 phases to CML
answer
- chronic phase -most patients diagnosed at this stage - responsive to chemotherapy - accelerated phase - worsening symptoms but not "blast crisis" - blast phase - increase in blasts in BM or PB, >20% - aggressive form of acute leukemia - AML 60-70% of cases; ALL 25% of cases - difficult to treat *patient can either undergo all three phases or skip directly from the chronic phase to the blast phase - treatment for this disease is a drug, called Imatinib or Gleevec. treats all phases, inhibits BCR-ABL and the tyrosine kinase - bone marrow transplant also cure
question
Lab features of CML
answer
Peripheral blood ►Very high WBC count ►Granulocytes with immature forms ►Basophilia ►Thrombocytosis ►Blasts <10% ►Decreased LAP ►Increased LDH, vitamin B 12, uric acid Bone marrow ►Myeloid hyperplasia ►Blasts <10% ►Increase megakaryocytes ►Myelofibrosis ►Monocyte usually <3% *normocytic anemia common RBCs pushed out
question
CML vs leukemoid reaction
answer
- both have neutrophils with immature forms- CML demonstrates basophilia/eosinophilia + "myelocyte bulge" (leuk will have metamyelocytes and bands) - CML: Philadelphia chromosome/BCR-ABL + - toxic granulation and vacuolation: + in leukemoid reaction; rare in CML - döhle bodies: + in leukemoid reaction; rare in CML - LAP: - in CML, positive in leuk
question
Essential Thrombocythemia (ET)
answer
CMPD characterized by ^ in platelets and abnormal function, risk of thrombosis (clotting) and hemorrhage - platelet count: >600 X 10^9/L - megakaryocyte hyperplasia in BM - absence of reactive thrombocytosis - absence of Ph chromosome - normal red cell mass - absence of significant marrow fibrosis - presence of iron in BM; failure to respond to oral iron ONLY INCREASE IN PLATELETS OBSERVED
question
PB smear of ET
answer
- increase platelets, platelet anisocytosis - platelets aggregating - normocytic, normochromic anemia - bleeding can be a problem bc of platelets, making MCHC and MCV decrease
question
Idiopathic Myelofibrosis (IMF)
answer
CMPD with.. - fibrosis of the marrow - satchy at first; widespread leader - extramedullary hematopoiesis - spleenomegaly and liver involvement - leukoerythroblastosis - clonal defect in the CD34+ hematopoietic stem cell - myeloblasts and NRBC in PB - teardrop poikilocytosis *associated with proliferation of granulocytes, megakaryocytes, and fibroblasts - patients may be asymptotic before diagnosis
question
Lab findings in IMF
answer
fibrosis -> BM failure, can show pancytopenia in some patients - normocytic normochromic anemia - evidence of hemolytic anemia/ reticulocytosis (DAT + or -) - abundant NRBC, immature granulocytes, teardrop cells - WBC and platelet count variable (normal to increased most common) - bone marrow aspirates "unsuccessful"
question
Chronic lymphoproliferative disorders
answer
- clonal proliferations of morphologically and immunophenotypically mature B or T lymphocytes - disorders affecting bone marrow and blood are called leukemias - those affecting lymph nodes and other lymphoid tissues are called lymphomas
question
Chronic lymphocytic leukemia (CLL)
answer
- most common leukemia in adults - extensive accumulation of lymphocytes (most small lymphocytes, some more immature) - chromatin is very condensed in the nuclei of many of these cells and it often takes on a "soccer-ball" pattern that can be very helpful in identifying these cells as leukemic - can see smudge cells (bare nuclei) - most often malignancy of B lymphocytes, T rare - B vs T can't be distinguished morphologically have to use cytogenetics, etc.
question
characteristics of CLL
answer
- disease of age, rare <50 y.o. ► Most frequently a malignancy of B cells ► Proliferative forms create the pool of small, non-dividing CLL cells that accumulate ► Accumulating lymphocyte mass in BM causes neutropenia, anemia, thrombocytopenia ► Lymphadenopathy, splenomegaly can be present ► patient can become immune compromised/autoimmunity - hypogammaglobulinemia, that is a decrease in Ab concentration
question
Etiology of CLL
answer
► No specific agent or cause known ► Gradual accumulation of B cells ► Chromosomal translocations rare ► Accumulate anti-apoptotic protein Bcl-2 ► Inhibition of apoptosis ► Abnormal cell cycle: blocked in early G1 phase ► Can respond rapidly to proliferative signals
question
Cell surface molecules that identify B cell lineage
answer
- surface immunoglobulin, CD19 and CD20 - CD23 and CD45?? (CD5 marks T cells, but is positive in CLL)
question
Flow cytometry
answer
- identifies lymphocytic leukemic cells, since they can't be determined morphologically - used with graphs plotting dots representing cells - plotted on axes of chains and surface markers
question
T cell prolymphocytic leukemia (T-PLL)
answer
- T cell malignancies rare - cells positive for CD3, usually CD4, CD7 and CD5 - negative for CD8 - most T cell leukemias are from the CD4 bc human T- cell leukemia virus or HTLV-1infects CD4 positive T cells and transforms them ....causes adult T cell leukemia aka ATL
question
CLL bone marrow patterns of lymphocyte accumulation
answer
- nodular - interstitial - diffuse *nodular and interstitial is better because the bone marrow is not completely replaced with lymphocytic cells *no room for hematopoiesis in diffuse BM, even fat tissue is replaced
question
Prognostic factors/clinical course of CLL
answer
- chromosomal abnormalities: trisomy 12, 13q14 deletions - slowly progressive, good 5 year survival rate for >50% - 10 year survival for 30%, 1-2 years for 20% ►Best prognosis: lymphocyte doubling time (LDT) >12 months, non-diffuse pattern in BM, Rai stage of 0-2 ►Worse prognosis: LDT <12 months, diffuse pattern in BM, Rai stage 3-4, elevated serum beta2 and elevated CD23 ►Infection or unrelated disease most common causes of death (patients older) ►Expression of zap-70, p53 mutations- worse prognosis -transformation to acute leukemia is rare
question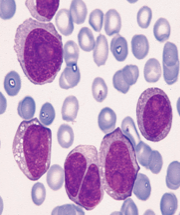
B prolymphocytic leukemia or B-PLL
answer
- >55% or even >70% of WBCs will be prolymphocytic - these are less mature than cells in CLL - nuclear chromatin is not as condensed - priminent nucleolus observed - extreme leukocytosis observed in this disease
question
Small Lymphocytic Lymphoma (SLL)
answer
- the counterpart of CLL, cells more in lymph node rather than PB - also called "diffuse non-Hodgkin lymphoma" - approximately 80% of cases of SLL contain trisomy 12 (20%), 13q14 abnormalities (50%) and deletions in chromosome 11 (20%) just like is seen in CLL - in leukemic phase, cells have left nodes and migrated to pb
question
Mantle Cell Lymphoma (MCL)
answer
- a type of SLL - disease arises from a particular lymphocyte type found in lymphoid tissue - always B cells - extremely high levels WBCs in blood (>200 billion) - distinguished from CLL bc they are CD23 negative - in 70% MCL, specific translocation detected t(11:14), -> increased cyclin D1 expression
question
Small Cleaved cell lymphoma (SCCL)
answer
- cleavage seen in nucleus - is a non-Hodgkin lymphoma consisting of B cells it can be nodular (in the lymph nodes) or diffuse - can progress to a leukemic phase and appear in blood
question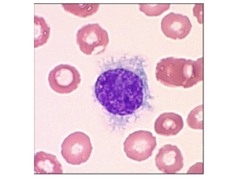
Hairy Cell Leukemia
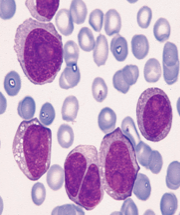
answer
- cells are so named because of the uneven, irregular, hair-like cytoplasmic projections that are observed in almost all of the leukemic cells - this disease results in a fibrosis of the bone marrow and is often associated with pancytopenia. - a disease of B cells but its etiology is for the most part unknown
question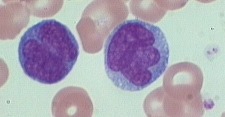
Sezary syndrome
answer
- the leukemic phase of the most common type of cutaneous T cell lymphoma, which is known as *mycosis fungoides* - name from the skin lesions observed (bc T cells accumulate in the skin) HALLMARK - T cells have nuclei that stain very dark and have numerous folds - nucleus is also cribriform - unknown cause
question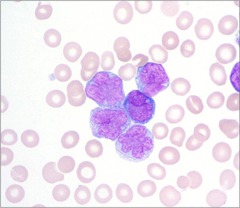
Adult T cell leukemia lymphoma (ATLL)
answer
- caused by a retrovirus known as human T-cell leukemia virus or HTLV-1 - common in Japan and Caribbean - the abnormal lymphocytes that have a highly convoluted nucleus - variation of cell size/morphology - high WBC count - disease can be acute, chronic, or smoldering - cells most often CD4 positive - rare cases CD8 positive
question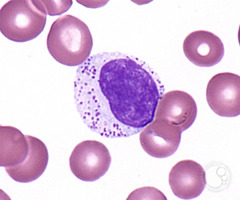
T cell large granular lymphocytic leukemia (LGL)
answer
- lymphocytosis with large granular lymphocytes that have azurphilic granules in the cytoplasm
question
3 types LGL
answer
- T-gamma lymphocytosis: cells are T cells with large granular lymphocytes, chronic neutropenia and autoimmunity observed - When cells are NK cells: disease aggressive and many organs involved - most ppl have 3rd type LGL: slower progression and the cells are CD3 negative (means they aren't T cells, but they don't have the NK phenotype either)
question
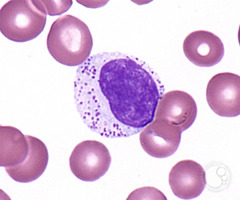
reactive lymphocytes
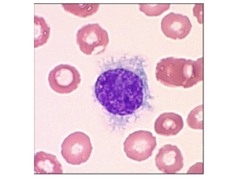
answer
- caused by viral infections with EBV, CMV and viral hepatitis - infectious mononucleosis characterized by these - cells mostly T cells - indentions of cytoplasm by RBCs characteristic, NOT seen in leukemic cells atypical = leukemic reactive = non leukemic lymphocytes
question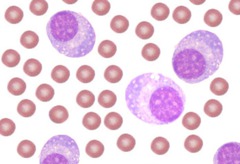
the 3 plasma cell dyscrasia's
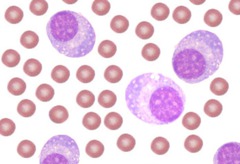
answer
- Waldonstrom's macroglobulinemia, multiple myeloma, and plasma cell leukemia - these cells are circulating plasma cells and they are not observed in normal peripheral blood smears - STRIKING FACTOR: nucleus is almost always eccentric, or to one side - cytoplasm is very blue because of the abundance of RNA and reticulum being used to manufacture Ig - "perinuclear clear zone" = - this zone near the nucleus contains the extensive Golgi apparatus the cell needs to secrete its Ig molecules



