Co-existing Disease; Ann – Flashcards
Unlock all answers in this set
Unlock answersquestion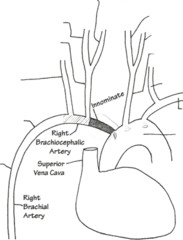
Vertebral arteries arise from the _______ ?
answer
The vertebral arteries arise from the subclavian arteries
question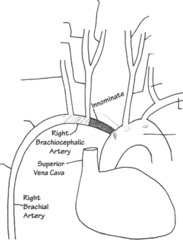
The subclavian arises from the __________ ?
answer
aortic arch
question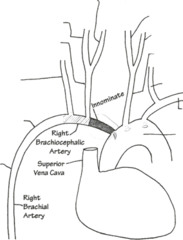
The carotids arise from the ________ ?
answer
The carotids arise from the aortic arch
question
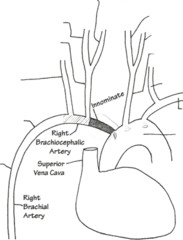
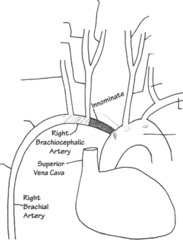
The vessels that can be most easily compressed during mediastinoscopy are the _______ ?
answer
The vessels that can be most easily compressed during mediastinoscopy are the innominate, right brachiocephalic and right common carotid.
question
Mediastinoscopy - Where is incision site?
answer
Mediastinoscopy This procedure can either be done via a transverse incision just above the suprasternal notch or in the second or third rib interspace. The mediastinoscope is inserted between the rib cage and the lungs.
question
Most common complication for Mediastinoscopy is _________ ? Name two other complications.
answer
Most common complication is hemorrhage and second is pneumothorax (primarily on right side). • May have air embolism if spontaneously breathing (Trendelenburg position) • May have vagal response due to stretching of vagal nerve or trachea
question
Mediastinoscopy is most useful for _______ ?
answer
Most useful for right lung tumors
question
If spontaneously breathing (Trendelenburg position) during Mediastinoscopy, what complication may happen?
answer
May have air embolism if spontaneously breathing (Trendelenburg position)
question
Mediastinoscopy what should you look for in these patients?
answer
• Myasthenic syndrome • Tracheal deviation • Thoracic inlet obstruction (lymph) • Type and cross for blood
question
What nerves should you be aware of during Mediastinoscopy?
answer
Left recurrent laryngeal nerve and phrenic nerve are around aortic arch
question
What anesthestic considerations for Mediastinoscopy?
answer
Anesthesia Application • Arterial line in right radial artery to monitor compression of innominate and right brachiocephalic arteries. • Monitor blood pressure in left arm. • Should pulse oximeter be placed on right or left hand? opposite art line • Large venous tear may mandate starting IV in leg. • Endotracheal intubation • Muscle paralysis • Positive pressure ventilation (decrease likelihood of air embolism)
question
Contraindications of Mediastinoscopy?
answer
Contraindications • Previous mediastinoscopy (scarring) • Superior vena cava obstruction • Tracheal deviation • Aneurysm of thoracic aorta
question
Complications of Mediastinoscopy?
answer
Complications: • Hemorrhage • Air embolus • Nerve injury • Pneumothorax • Esophageal injury • Thoracic duct injury • Tracheal compression
question
Where do you place art line in mediastinoscopy and why?
answer
Arterial line in right radial artery to monitor compression of innominate and right brachiocephalic arteries.
question
A body mass index greater than _______ are obese. Pts. who weigh _______ % more than their ideal body weight are obese .
answer
Anesthesia for Morbid Obesity Patients who weigh 20% above their ideal body weight or have a body mass index greater than 28 are obese.
question
Morbid obesity occurs when the patient's body weight is more than ________ above ideal body weight or when weightor his or her body mass index (BMI) exceeds ______.
answer
Morbid obesity occurs when the patient's body weight is more than 45 kg above ideal body weight, or his or her body mass index (BMI) exceeds 35 .
question
Respiratory changes in obesity (resembles ________ disease):
answer
Respiratory changes (resemble restrictive disease): O Basal metabolic rate (unchanged) O Chest wall compliance decreased O Expiratory reserve volume decreased O Inspiratory capacity decreased O Vital capacity decreased O Functional residual capacity decreased O Diaphragm is elevated O Work of breathing increased O Diaphragm breather O Pa02 decreased (arterial hypoxemia) O PaC02 normal O Restrictive ventilation defect O Sleep apnea O Be careful with the head down position.
question
Chest wall compliance decreased or increased in obesity?
answer
Chest wall compliance decreased
question
Functional residual capacity decreased or increased in obesity?
answer
Functional residual capacity decreased
question
Diaphragm is elevated or depressed in the obese?
answer
Diaphragm is elevated
question
How are Pa02 and PaC02 in the obese?
answer
Pa02 decreased (arterial hypoxemia) PaC02 normal
question
Cardiovascular changes in obesity:
answer
Cardiovascular changes O Cardiac output is increased O Congestive heart failure may occur O Pulmonary and systemic hyperperfusion O Blood volume increased (50 ml/kg) O Hypercholesterolemia O Hypertriglyceridemia O Diabetes mellitus O Ischemic heart disease O Cardiomegaly O Pulmonary hypertension
question
Cardiac output is increased or decreased in obesity?
answer
Cardiac output is increased
question
Blood volume increased or decreased?
answer
Blood volume increased: (50 ml/kg)
question
Anesthesia concerns:
answer
Anesthesia concerns: O Use caution for aspiration (rapid sequence induction, RSI) O Be aware that halothane hepatitis is a possibility due to increased fatty infiltrates in the liver O Assess your airway O Calculate drug dose on ideal rather than actual body weight O Regional anesthesia may be difficult due to obscured bony landmarks-osteoarthritis O Monitor ABGs O Mechanical ventilation with high tidal volumes O Prone to nerve stretch injuries due to difficulty in positioning; watch brachial plexus O Need to wake up quickly; extubate awake - sleep apnea
question
Anesthesia concerns: postop
answer
Postoperative O Semi-sitting position O Oxygen per mask for 2-3 days O Need early ambulation to decrease risk of deep vein thrombosis and pulmonary emboli O Use narcotics with caution due to respiratory depression O Use correct size blood pressure cuff
question
In the obese, Calculate drug dose on ideal or actual body weight?
answer
Calculate drug dose on ideal rather than actual body weight
question
Management of ventilation in the obese:
answer
Management of ventilation ■ Large tidal volume ■ Prone and head-down position may further decrease Pa02 O
question
Compared with a nonobese person, what happens to functional residual capacity (FRC) in the morbidly obese patient while upright (standing or sitting)
answer
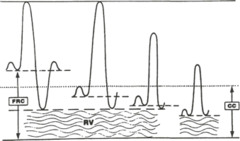
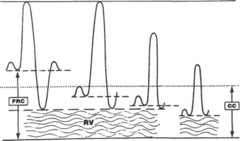
Compared with a nonobese person, what happens to functional residual capacity (FRC) in the morbidly obese patient while upright (standing or sitting), supine, or prone? In the upright position, FRC is decreased compared with that of the nonobese person. Tidal ventilation may fall within the closing capac¬ity (CC) (see figure). In the supine position, FRC falls further and tidal breathing continues to occur with some airways closed (within the range of closing capacity). If the patient is positioned so that the abdomen hangs free, FRC is decreased less in the prone than in either the supine or the lateral positions, so events in the morbidly obese, prone patient would be between the obese upright and obese supine positions
question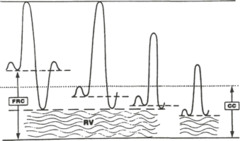
Compared with a nonobese person, what happens to functional residual capacity (FRC) in the morbidly obese patient while upright (standing or sitting)
answer
Effects of position on lung volumes (Labeled left to right: Nonobese; obese upright; obese supine; obese trendelenburg) In the upright position, FRC is decreased compared with that of the nonobese person. Tidal ventilation may fall within the closing capac¬ity (CC) (see figure).
question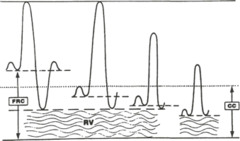
Compared with a nonobese person, what happens to functional residual capacity (FRC) in the morbidly obese patient while supine?
answer
Effects of position on lung volumes (Labeled left to right: Nonobese; obese upright; obese supine; obese trendelenburg) In the supine position, FRC falls further and tidal breathing continues to occur with some airways closed (within the range of closing capacity).
question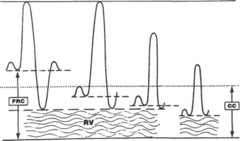
What happens to functional residual capacity (FRC) in the morbidly obese patient while prone?
answer
Effects of position on lung volumes (Labeled left to right: Nonobese; obese upright; obese supine; obese trendelenburg) If the patient is positioned so that the abdomen hangs free, FRC is decreased less in the prone than in either the supine or the lateral positions, so events in the morbidly obese, prone patient would be between the obese upright and obese supine positions
question
Pheochromocytoma :
answer
It is a tumor of the adrenal medullary or chromaffin tissue of the paravertebral sympathetic chain that has excessive catecholamine secretion (usually norepinephrine).
question
Where does Pheochromocytoma originate and where is it found?
answer
A tumor of the adrenal medullary or chromaffin tissue of the paravertebral sympathetic chain that has excessive catecholamine secretion (usually norepinephrine). It is found in the abdominal cavity most of the time (95%) and originates in the adrenal medulla about 90% of the time.
question
The diagnostic triad for Pheochromocytoma is:
answer
The diagnostic triad is: O Diaphoresis O Tachycardia O Headaches
question
Symptoms of Pheochromocytoma are:
answer
paroxysmal hypertension, sweating, tremulousness, tachycardia headache, palpitations, orthostatic hypotension. The diagnostic triad is: O Diaphoresis O Tachycardia O Headaches
question
Causes of death in pts with Pheochromocytoma are:
answer
When not diagnosed and treated in a timely manner, the patient may die from: O Congestive heart failure O Myocardial infarction O Intracerebral hemorrhage
question
Treatment (pre-operative) preparation) in pts with Pheochromocytoma are:
answer
• Alpha adrenergic blockade O Phenoxybenzamine: start with 20-30 mg/day and increase to 60-250 mg/day in order to control the blood pressure. O Prazosin • Beta block O Primarily for treatment of tachycardia • Patient will need fluid status assessed and hypovolemia will be corrected (may use Neosynephrine)
question
Treatment (intra-operative) care) in pts with Pheochromocytoma are:
answer
Anesthesia • Do not stimulate the sympathetic nervous system. Use caution and sedate during line placement, induction, laryngoscopy, and skin incision. You must have anesthesia in place before any stimulation occurs. • Continue pre-operative therapy, invasive monitors, opioids and Forane/Ethrane • Control tachycardia with esmolol, labetalol and propranolol.
question
Absolute and relative indications for one Lung Anesthesia-Ventilation
answer
Absolute indications: O Prevent contamination of healthy lung O Control distribution of ventilation Relative indications: O Surgical exposure
question
What kind of tubes should be used for one Lung Anesthesia-Ventilation?
answer
O Carlens tube is a left-sided double lumen tube with a carinal hook O White tube is a right-sided Carlens tube O Robert Shaw is a double lumen tube available in right or left clear plastic that does not have a carinal hook
question
How to Place the Robert Shaw tube in one Lung Anesthesia-Ventilation?
answer
Placing the Robert Shaw tube: • Concave curve of tube is anterior (12:00 noon) • After the tip of the tube passes the cords the tube is turned 90 degrees to the left (9 o'clock) and advanced until resistance is met.
question
How to verifying placement of Robert Shaw tube in one Lung Anesthesia-Ventilation :
answer
Verifying placement of Robert Shaw tube: • Inflate tracheal cuff and confirm bilateral and equal breath sounds • Inflate bronchial cuff (how much air?) and confirm bilateral and equal breath sounds • Confirm one lung ventilation by clamping each lumen
question
The goal of one lung ventilation is
answer
The goal of one lung ventilation is to optimize arterial oxygenation.
question
ASA Class 1
answer
Healthy patient, no organic, physiologic, bio¬chemical, or psychiatric disturbance
question
ASA Class 2
answer
Patient with mild systemic disease (disturbance) that may or may not be related to the reason for surgery
question
ASA Class 2 examples:
answer
Essential hypertension, heart disease that only slightly limits activity, diabetes, anemia, extremes of age, morbid obesity, and chronic bronchitis
question
ASA Class 3
answer
Patient with severe systemic disease (disturbance) that limits activity but is not incapacitating and may or may not be related to surgery
question
ASA Class 3 examples
answer
Heart disease that limits activity, poorly controlled essential hypertension, diabetes with vascular complications, chronic pulmonary disease that limits activity, history of prior myocardial infarction and angina pectoris
question
ASA Class 4
answer
Patient with an incapacitating systemic disease that is a constant threat to life with or without surgery
question
ASA Class 4 examples
answer
Congestive heart failure (CHF), persistent angina pectoris, any advanced kidney, liver or pulmonary disease
question
ASA Class 5
answer
Moribund patient not expected to live 24 hours with or without surgery. Submitted to surgery as resuscitative effort
question
ASA Class 5 examples:
answer
Pulmonary embolus, cerebral trauma or ruptured AAA (uncontrolled)
question
ASA Class 6
answer
A brain-dead patient whose organs are being harvested
question
ASA Class 6 examples
answer
Organ donation
question
Emergency Operation (E)
answer
Any patient requiring emergency (not elective) surgery
question
Emergency Operation (E) examples:
answer
appendicitis, dilation and curettage for bleeding, or any surgery required on a non-elective basis
question
Muscular Dystrophy:
answer
Painless degeneration and atrophy of skeletal muscles (associated with mental retardation)
question
Most common and most severe Muscular Dystrophy:
answer
Duchenne's muscular dystrophy
question
Duchenne's muscular dystrophy
answer
• X-linked recessive (boys) • Early childhood • Early childhood • Kyphoscoliosis and hip and knee contracture are common
question
What ECG changes do you see with Duchenne's muscular dystrophy?
answer
• ECG changes include prolonged PR and QRS interval, ST segment abnormalities, bundle branch block, Q waves, tall R waves
question
How are total lung capacity and residual volume affected with Duchenne's muscular dystrophy?
answer
• Total lung capacity and residual volume are reduced
question
Anesthetic considerations with Duchenne's muscular dystrophy:
answer
• Recurrent pulmonary infections • Increased incidence of malignant hyperthermia, so avoid succinylcholine • Neuromuscular monitoring is mandatory
question
The most significant anesthesia concern with Duchenne's muscular dystrophy:
answer
• Increased incidence of malignant hyperthermia, so avoid succinylcholine
question
Pseudohypertrophic muscular dystrophy:
answer
Pseudohypertrophic muscular dystrophy ■ Congestive heart failure ■ Recurrent pneumonia ■ Kyphoscoliosis ■ Hyperkalemia with succinylcholine ■ May be susceptible to malignant hyperthermia
question
Limb-girdle muscular dystrophy:
answer
(relatively benign disease)
question
Facioscapulohumeral muscular dystrophy :
answer
(heart not involved)
question
Nemaline rod muscular dystrophy:
answer
■ Micrognathia ■ Bulbar palsy
question
Multiple Sclerosis
answer
Characterized by random and multiple sites of demyelination of corticospinal tract neurons in the brain and spinal cord, exclusive of the peripheral neurons.
question
Multiple Sclerosis signs and symptoms:
answer
O Visual disturbances 0 Ataxia O limb paresthesia and weakness O Spastic paresis of skeletal muscles O Exacerbations and remission
question
How to diagnose Multiple Sclerosis:
answer
Diagnosis O Somatosensory evoked responses O Computed tomography O Immersion in hot water O Examination of CSF
question
Treatment (palliative) of Multiple Sclerosis:
answer
Treatment (palliative): O Corticosteroids O Avoid stress O Avoid marked temperature changes O Dantrolene O Carbamazepine
question
Management of anesthesia for Multiple Sclerosis:
answer
O Exacerbation of symptoms may occur, SUBARACHNOID BLOCK IS A QUESTIONABLE SELECTION. O Hyperkalemia in response to succinylcholine O Prevent increased body temperature post-operatively.
question
Myasthenia Gravis:
answer
A chronic autoimmune disease involving the neuromuscular junction. It is characterized by weakness and rapid exhaustion of skeletal muscles with repetitive use; there is some recovery with rest.
question
Signs and Symptoms of Myasthenia Gravis:
answer
O Ptosis and diplopia - most common initial symptoms O Weakness of pharyngeal and laryngeal muscles - aspiration risk O Asymmetric extremity skeletal muscle weakness - atrophy absent O Cardiomyopathy O Hypothyroidism
question
Most common initial symptoms of Myasthenia Gravis:
answer
O Ptosis and diplopia - most common initial symptoms
question
Anesthesia concern with Myasthenia Gravis:
answer
O Weakness of pharyngeal and laryngeal muscles - aspiration risk
question
Treatment of Myasthenia Gravis:
answer
Treatment O Anticholinesterase drugs (Neostigmine Edrophonium) O Corticosteroids O Cyclosporine ***O Plasmapheresis O Thymectomy - most likely elective operation
question
Anesthesia for Myasthenia Gravis:
answer
O Preoperative preparation ■ Avoid opioids ■ Inform patient of possible mechanism ventilation postoperative O Muscle relaxants NDMB - very sensitive; DMB unpredictable. ■ Expect altered response O Induction ■ Short acting IV drug ■ Tracheal intubation without muscle relaxants O Maintenance ■ Volatile drugs ■ Short or intermediate-acting muscle relaxants O Postoperative ■ Skeletal muscle strength may decrease abruptly
question
Avoid muscle relaxants in Myasthenia Gravis. T or F
answer
True Tracheal intubation without muscle relaxants if possible Short or intermediate-acting muscle relaxants
question
Parkinson's Disease
answer
Parkinson's Disease • Degenerative disease of the CNS characterized by loss of dopaminergic fibers in the basal ganglia of the brain. Dopamine is an inhibitory neurotransmitter acting on the extrapyramidal motor system.
question
Parkinson's Disease Signs and symptoms:
answer
O Signs and symptoms ■ Skeletal muscle rigidity ■ Resting tremor ■ Diaphragmatic spasms ■ Mental depression
question
Parkinson's Disease Treatment:
answer
Treatment (increase concentration of dopamine) ■ Levodopa - combines with decarboxylase inhibitor; side effects reflect dopamine effects on the CNS, heart and GI tract ■ Anticholinergic drugs ■ Antihistamine drugs - Benadryl.
question
Management of anesthesia with Parkinson's Disease:
answer
Management of anesthesia O Continue levodopa therapy O Labile blood pressure and cardiac dysrhythmias possible ***O Avoid drugs with antidopaminergic effects (droperidol, possibly opioids, and Reglan)
question
What drugs should you avoid with Parkinson's Disease? Why?
answer
Avoid drugs with antidopaminergic effects (droperidol, possibly opioids, and Reglan) Degenerative disease of the CNS characterized by Joss of dopaminergic fibers in the basal ganglia of the brain.
question
RHEUMATOID ARTHRITIS:
answer
Chronic inflammatory disease characterized by symmetric polyarthropathy and significant systemic involvement. • Has cervical vertebral involvement but no sacroiliac involvement. • Most common in females 30-50 years old. What following cardiac changes:
question
What cardiac changes do you see in RHEUMATOID ARTHRITIS?
answer
O May see the following cardiac changes: ■ Pericardial effusion ■ Aortic regurgitation ■ Cardiac conduction abnormalities ■ Cardiac valve fibrosis ■ Coronary artery arteritis
question
Airway evaluation in RHEUMATOID ARTHRITIS?
answer
Airway evaluation (restrictive disease) O Head movement and position O Hoarseness or stridor - cricoarytenoid joint involvement (May present already with hoarseness) O May need fiberoptic intubation O Pulmonary function studies and ABGs O Postoperative ventilation
question
Keratoconjunctivitis sicca: What condition do you see this in?
answer
(a condition marked by hyperemia of the conjunctiva, lacrimal deficiency, thickening of the corneal epithelium, itching and bruising of the eye, and often reduced visual acuity)
question
RHEUMATOID ARTHRITIS pulmonary concern?
answer
Pulmonary fibrosis, pleural effusion
question
RHEUMATOID ARTHRITIS symptoms :
answer
Consider multiple organ involvement Cardiac changes Anemia Rheumatoid factor is positive Keratoconjunctivitis sicca Pulmonary fibrosis, pleural effusion Cricoarytenoid involvement
question
Treatment for RHEUMATOID ARTHRITIS:
answer
■ Aspirin ■ Gold ■ Surgery ■ Corticosteroids (stress dose)
question
Osteoarthritis: .
answer
• Degenerative process that affects the articular cartilage and differs from rheumatoid arthritis due to lack of (or minimal) inflammatory reaction. • Degenerative changes are primarily in the middle to lower cervical spine and in the lower lumbar area.
question
Osteoarthritis:
answer
Treatment O Aspirin O Reconstructive joint surgery O No corticosteroids (because not inflamatory chronically)
question
SCOLIOSIS:
answer
• Lateral curvature of spine • Idiopathic scoliosis is most common type • Restrictive pattern of breathing with thoracic scoliosis • Chest wall deformity
question
SCOLIOSIS lung changes:
answer
Vital capacity (60-80% of predicted), total lung capacity decrease inspiratory volume decrease functional residual capacity decrease inspiratory capacity decrease expiratory reserve volume decrease. Residual volume may be normal. FEV₁/FVC is normal. ***(Because it is restrictive) Chest wall deformity
question
What would you see with ABGs and SCOLIOSIS:
answer
O Thoracic scoliosis associated with arterial desaturation, but PaC02 and pH are normal. O Arterial hypoxemia O Alveolar ventilation is normal
question
SCOLIOSIS and cardiovascular system:
answer
May develop elevated pulmonary vascular resistance and pulmonary hypertension leading to right heart failure. Mitral valve prolapse is most common abnormality.
question
Anesthetic technique with SCOLIOSIS:
answer
Preoperative medication: O Avoid heavy premedication O Antisialagogue Avoid succinylcholine (muscle disease) Author favors nitrous oxide - narcotic infusion - relaxant technique O Prepare for blood loss (15-25 ml/kg): Patients with neuromuscular scoliosis may lose 75 ml/kg. O Deliberate hypotension—do not want to compromise spinal cord blood flow (MAP 60-65 mm Hg)
question
Parameters for extubation for pt with SCOLIOSIS:
answer
Need to be breathing well Vital capacity > 10 ml/kg ***Tidal volume >3ml/kg Spontaneous respiration rate -30 cm H20.
question
Complications seen with SCOLIOSIS: .
answer
Complications: O Pneumothorax O Atelectasis O Pleural effusion O Hemothorax O Neurologic injury
question
What is most common abnormality with scoliosis? .
answer
Mitral valve prolapse is most common abnormality.
question
What type blood loss can you see with SCOLIOSIS?
answer
Prepare for blood loss (15-25 ml/kg): in patients with neuromuscular scoliosis may lose 75 ml/kg.
question
What type vital capacity will you see with scoliosis?
answer
Vital capacity (60-80% of predicted), Total lung capacity decreased.
question
What type of breathing pattern is seen with with thoracic scoliosis?
answer
Restrictive pattern of breathing with thoracic scoliosis
question
_________ scoliosis is most common type. .
answer
Idiopathic scoliosis is most common type.
question
Number 1 and 2 complications seen with mediastinoscopy. .
answer
1. Hemorrhage 2. Pneumothorax
question
Inominate gives rise to .
answer
Inominate gives rise to RCA and RVC .
question
ASA 3 or ASA 4 :
answer
Look for the word incapacitating.
question
Muscular Dystrophy
answer
Psdohypertrophy especially of calves due to fatty infiltration of muscles
question
Multiple Sclerosis and central blocks
answer
No central blocks; No spinals; epidurals are controversial.
question
Duchenne's muscular dystrophy and Succ: .
answer
Hyper K with Succ.
question
Eaton Lambert
answer
Myasthemic syndrome associated with carcinoma.



