Anesthesia Boards+True Learn – Flashcards
Unlock all answers in this set
Unlock answersquestion
EKG leads corresponding to RCA territory? The RCA supplies which part of the heart?
answer
II, III, aVF RA, the entire RV except for the APEX, posterior/inferior LV, posterior 1/3rd of interventricular septum, SA (50%) & AV (90%) node, posteromedial pappillary muscle
question
EKG leads corresponding to LAD territory The LAD supplies which part of the heart?
answer
V1, V2, V3, V4 LAD supplies anterior LV, anterior 2/3rds of IV septum, Bundles
question
EKG leads corresponding to Circumflex territory The LCx supplies which part of the heart?
answer
I, V5, V6 LCx provides for posterior and lateral LV wall, and anterolateral papillary muscle
question
Nerve supply for Cricothyroid Muscle
answer
External Branch of Superior Laryngeal Nerve
question
Nerve supply for everything but Cricothyroid Muscle
answer
Recurrent Laryngeal Nerve
question
Postoperative Complications of Thyroid Surgery
answer
1) Airway obstruction due to laryngeal edema (PACU) 2) Airway obstruction due to hematoma (can present in PACU if arterial or within 24 hours if venous - this is the most common cause of airway obstruction) 3) Airway obstruction due to bilateral damage to RLN (results in laryngospasm immediately post extubation) 4) Hypoparathyroidism (24-96 hours later) - laryngeal stridor leading to laryngospasm
question
Posterior Pituitary produces which hormones
answer
Vasopressin and Oxytocin
question
MELD Score
answer
INR, Bilirubin, Creatinine, Sodium; Determines who has the highest priority to receive a liver transplant. The higher the number, the more elevated the risk. "CRIB NA"
question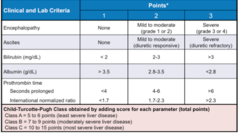
Child Pugh Score
answer
INR, Bilirubin, Albumin, Ascites, Encephalopathy; Useful to determine prognosis in patients with cirrhosis. Class A (5-6 points) low risk, Class C (10-15) high risk. "HI ABA"
question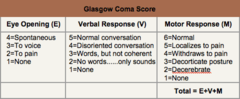
Glascow Coma Scale
answer
Eye response (4), Verbal (5), Motor (6); Extra value Meal costs $4.56
question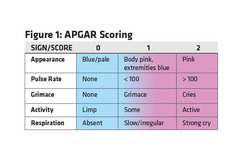
APGAR
answer
Appearance, Pulse, Grimace, Activity, Respiration
question
CVP waveform

answer
ACXVY a wave = atrial contraction c wave = ventricular contraction x descent = pulmonic valve opening v wave = venous return of flow with tricuspid closed y descent = TV opens, atrium empties into the ventricle (diastasis)
question
Innervation of Larynx (sensory)
answer
Anterior Tongue --> Vallecula (includes soft palate and oropharynx): CN IX Vallecula/Hypopharynx --> Vocal cords: Internal Branch of SLN Vocal cords --> Trachea --> RLN
question
Innervation of Larynx (motor)
answer
Cricothyroid Muscle: External Branch of SLN Everything else: RLN
question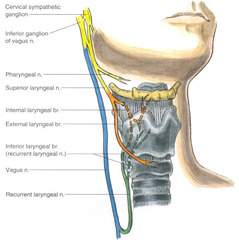
Regional Anesthesia for FOI (3 blocks)
answer
1) Anterior Tonsillar Pillar - Glossopharyngeal 2) Inferior Aspect of Greater Cornu of Hyoid - Internal Branch of SLN 3) Transtracheal - RLN
question
Atracurium metabolite
answer
Laudanosine (excreted renally). Can cause seizures and hypotension in patients with renal failure. Side effect of atracurium: can cause histamine release (transient flushing, hypotension, tachycardia) Metabolism: Eliminated via Hoffman Elimination and Ester Hydrolysis
question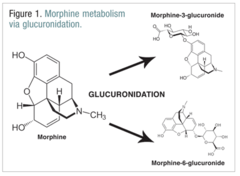
Morphine active metabolite
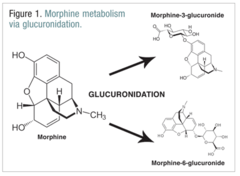
answer
Morphine-6 Glucuronide - accumulates in patients with kidney failure causing respiratory depression. THERE ARE 6 LETTERS IN THE WORD 'ACTIVE'
question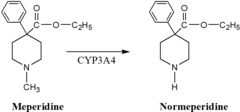
Meperidine active metabolite
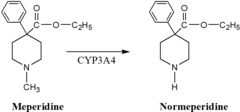
answer
Normeperidine (excreted renally) - accumulates in patients with renal failure causing seizures
question
Hydromorphone active metabolite
answer
Hydromorphone 3 Glucuronide (excreted renally) - accumulates in patients with renal failure causing cognitive dysfunction and myoclonus
question
Free Water Deficit equation **corrected**
answer
(0.6 x Kg) x (Serum Na/140 - 1)
question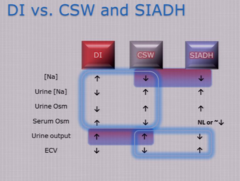
Diabetes Insipidus vs Cerebral Salt Wasting vs SIADH
answer
Tx of Central DI - Desmopressin Tx of Nephrogenic DI - HCTZ (counterintuitive) Tx of SIADH - fluid restriction + demeclocycline (interferes with the action of ADH) Tx of Cerebral Salt wasting - replacing urinary loses of sodium + free water with fluids **Do not correct hypernatremia too fast (no more than 0.5mEq/L/hr)
question
Plavix Mechanism of Action

answer
Blocks ADP receptor (Activation of ADP leads to surface expression of IIb/IIIa receptor on platelets - where fibrinogen and vWF binds). It is non competitive and irreversible.
question
Warfarin Mechanism of Action
answer
Blocks Vit K epoxide reductase. Leads to depletion of clotting factors II, VII, IX, X, protein C and protein S. Factor VII will be depleted first
question
Argatroban Mechanism of Action
answer
Direct Thrombin Inhibitor. Hepatic clearance. t1/2: 40-50mins
question
Bivalrudin Mechanism of Action
answer
Direct Thrombin Inhibitor. Cleared by plasma proteases - can be used in patients undergoing CPB who cannot be given heparin; it is monitored by ACT levels
question
Hirudin Mechanism of Action
answer
Direct Thrombin Inhibitor. Renal elimination.
question
Fondaparinux Mechanism of Action
answer
Factor Xa inhibitor. Renal elimination.
question
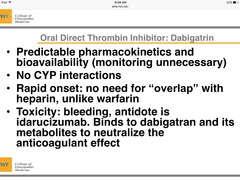
Dabigatran mechanism of action?
answer
Direct thrombin inhibitor; renally cleared
question
Rivaroxiban (xarelto) mechanism of action?
answer
Direct Xa inhibitor, use with caution in hepatic and renal insufficiency
question
DDAVP
answer
Antagonizes V2 receptor. Regulates water reabsorption and can cause a release of vWF. Indicated in DI and vWD and mild hemophilia A.
question
TXA and Aminocaproic Acid Mechanism of Action
answer
Binds to plasminogen and blocks the activation of plasmin (pro-thrombotic)
question
HIT Type I vs Type II
answer
Type 1: Non immune mediated. Seen after 1st day of exposure. Transient and insignificant Type 2: Immune mediated. IgG binds to PF4, activates platelets and causes aggregation. Seen 5-10 days after exposure. Management: switch to direct thrombin inhibitors (bivalrudin, argatroban, fondaparinux
question
vWD Type 1 vs Type 2 vs Type 3
answer
Type 1: Quantitative decrease in vWF. AD. Tx: Desmopressin Type 2: Qualitative abnormality in vWF. AD Type 3: Rare, undetectable levels of vWF. Body does not produce it.
question
Lambert Eaton Syndrome sensitive/resistant to Succinylcholine/NMBDs?
answer
Sensitive to both Succinylcholine and NMBDs.
question
Myasthenia Gravis sensitive/resistant to Succinylcholine/NMBDs?
answer
Resistant to Succinylcholine but sensitive to NMBDs.
question
How to tell the difference between Myasthenic Crisis vs Cholinergic Crisis?
answer
Give Edrophonium --> Increased weakness points to cholinergic crisis; Improvement or Decreased weakness points to Myasthenic crisis
question
Tx of Myasthenia Gravis
answer
Anticholinesterase inhibitors - Pyridostigmine
question
Malignant Hyperthermia Diagnosis
answer
Gold standard - Halothane-caffeine Test
question
Treacher Collins Syndrome

answer
Difficult airways, autosomal dominant, genetic mutation, 1:50,000 live births - Mandibular/Maxillary Hypoplasia (micrognathia, absent cheekbones) - Cleft or Arched Palate - Macrostomia - Fish like facies - Choanal Atresia - Cor Pulmonale - OSA - Conductive hearing loss, malformed ears
question
Pierre Robin Sequence

answer
Triad (Disappears after 2 years of age): 1) Hypoplastic Mandible 2) Glossoptosis - posterior displacement of the base of the tongue over epiglottis 3) Cleft palate Associated with Cor pulmonale, OSA Can be seen in Stickler syndrome, Velocardiofacial syndrome, Treacher-Collin syndrome
question
1cm elevation = what change of mmHg?
answer
0.74mmHg; Example 10cm elevation = reading will be 7.5mmHg higher than baseline
question
Types of Heat Loss? #1 cause of intraop heat loss?
answer
Convection, Conduction, Evaporation, Radiation. Radiation is the #1 cause of heat loss intraoperatively
question
Anterior/Posterior Ischemic Optic Neuropathy Associations
answer
Associated with: Prone surgeries Spine cases Cardiopulmonary Bypass cases Males Hypotension Anemia, >6hr Surgery, Increased Venous/Eyeball pressure Less Colloids
question
Vessel Rich Organs vs Vessel Poor Organs
answer
Rich = Brain, Kidney, Heart, Liver, Adrenals (does NOT include lungs because normally the lungs receive 100% of CO) Med = Muscle, Skin Poor = Bone, Cartilage, Ligaments
question
Meperidine Facts
answer
- Meperidine is a strong anticholinergic, causes tachycardia - Causes Histamine Release - Metabolite Normeperidine - accumulates in renal patients potentially causing seizures - MAO inhibitor + Meperidine can lead to serotonin syndrome (confusion, hyperthermia, shivering, myoclonus, and hyperreflexia) - Kappa receptor agonism to oppose shivering - Potency 0.1 compared to Morphine
question
Baclofen binds to which receptor
answer
GABA-B. Benzodiazepines bind to GABA-A.
question
Opioid Receptors
answer
Mu1: analgesia, skeletal muscle rigidity Mu2: respiratory depression Kappa: sedation, dysphoria, miosis. Antagonizes shivering
question
Venous systems that bypass the R Heart
answer
Thesbian, bronchiolar and pleural veins
question
Full term newborn's Total Blood Volume Premature neonate's Total blood volume
answer
Fullterm: 90cc/kg Premature: 100cc/kg
question
Neonatal Airway Differences The Larynx is positioned at ____ level. The epiglottis is long/short? The tongue is smaller/larger? The narrowest part of the airway is the ____. Occiput is larger/smaller?
answer
- C3-C4 in children. C5-C6 in adiults - Longer, floppy, omega/u shaped - Larger - Cricoid cartilage; it is conically shaped. The narrowest part in adults is the glottis - Larger occiput - may benefit from shoulder roll
question
Neonates are more likely to drop temperature intraop due to:
answer
Increased surface to body ratio
question
When does the Foramen Ovale close? Ductus Arteriosus? Ductus Venosus?
answer
Functionally: FO: Immediately, DA: 1 day, DV: 1 week Anatomically: FO: 3 months, DA: 1 month, DV: 1-3 weeks Note: Foramen Ovale remains patent in 25% of population
question
Adult SPINAL CORD ends at what level? Infant spinal cord ends at what level?
answer
Adult spinal cord ends at L1-2 Infant (<12 months) spinal cord ends at L3-4. After 12 months it is similar to that of an adult.
question
Adult DURAL SAC ends at what level? Infant dural sac ends at what level?
answer
Adult dural sac ends at S2 Infant dural sac ends at S4
question
Where would you place a pulse oximeter in a newborn?
answer
The R Hand is the only preductal choice and it is recommended to place it on the R hand to monitor lung function.
question
Delay ambulatory/elective surgery in infants after what age?
answer
Post conceptual age >50weeks. Delay surgery because of increased risk of post anesthesia apnea. Risk of apnea can be decreased with IV caffeine or aminophylline.
question
Apnea of Prematurity
answer
- Defined as >10s of apnea or 15s of apnea with desaturations or bradycardia - Risk factors: 1) Prematurity (<37 week gestation) 2) HCT < 30% 3) GA 4) Preoperative apnea - Tx Caffeine 10mg/kg IV
question
Omphalocele vs Gastroschesis
answer
Omphalocele - Midline defect - Covered in membranous sac - More likely to be associated with other defects (75% of time - VSDs [most common], Trisomy 21, Beckwith Wiedmann syndrome Gastroschisis - Off midline defect - Usually not associated with anything besides prematurity - Not covered by membranous sac - If surgeon cant close, consider leaving abdomen open with silo
question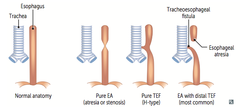
Tracheoesophageal Fistula
answer
- Most common type is Type C - Associations: 1. Prematurity 2. CHD 3. GI abnormalities 4. VACTERL 5. Renal/GU Abnormalities - Intraop management 1. Rapid sequence or awake intubation 2. Avoid N2O 3. Spontaneous breathing until fistula is ligated 4. Murphy's eye facing anteriorly
question
How much ml/kg of pRBC can raise a patient's Hgb by 1?
answer
4mL/kg
question
Do muscle relaxants cross the placenta?
answer
No, both succinylcholine and NMBDs do not cross the placenta because they are charged particles.
question
Anesthesia Dolorosa
answer
Pain in an area that lacks sensation
question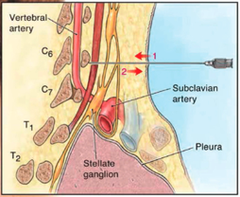
Chassiaignac's Tubercle
answer
C6
question
A successful Stellate Ganglion Block should cause what?
answer
- Ipsilateral Horner's Syndrome (anhidrosis, miosis, ptosis, nasal stuffiness) - Increased temperature of ipsilateral arm - Hyperemia of ipsilateral arm
question
Celiac Ganglion Block at what level?
answer
L1
question
1st Stage of Labor (Latent and Active) is covered at what dermatome?
answer
Covered by T10-L1. Latent Stage = 2-3cm dilated Active stage = 3cm-complete dilation
question
2nd Stage of Labor is covered by what?
answer
Covered by S2-S4. It is due to distention of the pelvic floor. Covered by Epidural, Spinal, Caudal and Pudendal nerve blocks
question
Why would you need avoid NSAIDS in the pregnant population?
answer
It can cause closure of the Ductus Arteriosus in the fetus which can be fatal.
question
Acute Intermittent Porphyria can be triggered by?
answer
Avoid barbiturates, BZDs, glucocorticoids, etomidate, toradol, alcohol, stress/dehydration. AIP can be exacerbated by inducers of the CYP450 system Present with confusion, anxiety, autonomic instability, abdominal pain and emesis. Porphyria cutanea tarda is not affected by anesthetic medications.
question
Fetal Heart Monitoring: Early, Variable and Late Decels?
answer
Early could be due to head compression due to uterine contractions (reassuring) Variable could be due to uteroplacental cord compression (reversible) Late due to uteroplacental insufficiency (not resassuring, needs OB evaluation). Deceleration >30secs after contraction LATE DECELs "The onset and nadir of late fetal heart rate (FHR) decelerations occur after the onset and peak of the associated uterine contraction. Late decelerations are caused by delivery of deoxygenated blood to the chemoreceptors in the fetus. Activation of chemoreceptors in the aortic arch and in the carotid sinus due to hypoxia activates the vagal response. The circulation time from placenta to chemoreceptors appears to delay the onset of the deceleration, so it is referred to as "late" deceleration. Deoxygenated blood from the placenta also depresses the fetal heart. Therefore, it is suggested that both activation of chemoreceptor reflex as well as direct myocardial depression are responsible for late FHR decelerations. Late decelerations, when accompanied by decreased or absent FHR variability, are indicative of fetal hypoxia, and steps to initiate emergent delivery of the baby should be considered."
question
Mild Preeclampsia? Severe Preeclampsia? Ecclampsia?
answer
Mild preeclampsia: BP >140/90, proteinuria (>300mg/day), edema (Management: IF TERM, INDUCE; IF NOT, BEDREST) Severe preeclampsia: BP >160/110, proteinuria, edema, HA, blurry vision, RUQ pain, hyperactive reflexes, HELLP syndrome (Management: DELIVER IMMEDIATELY) Ecclampsia: Severe preeclampsia + SIEZURES
question
Magnesium Toxicity
answer
Loss of DTRs, Resp depression, complete heart block, VASODILATION (Tx: Calcium gluconate, lasix + isotonic fluids, dsialysis). Additional info for reference: - Normal serum Mg concentration is 1.5-2.5. - Therapeutic levels for preeclampsia is 5-9. - DTRs are reduced >5, lost at >12. Skeletal muscle weakness begins at 7-10. Respiratory muscle/diaphragm weakness can start to occur >15. - Cardiac symptoms can be seen >5 (prolonged PR and widened QRS) with asystole at >25. **Remember that magnesium potentiates NMBDs and LA and can prolong succinylcholine.
question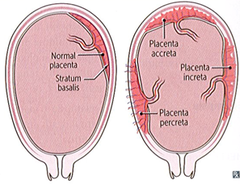
Define Placenta Accreta, Increta and Percreta What conveys the highest risk of abnormal placentation?
answer
Accreta — chorionic villi attach to the myometrium, rather than being restricted within the decidua basalis. Increta — chorionic villi invade into the myometrium. Percreta — chorionic villi invade through the PERImetrium, sometimes invading the bladder or rectum Risk factors include advanced maternal age, prior CS, and placenta previa. Placenta previa carries the highest risk.
question
Placenta Previa
answer
Positioning of the placenta at or near the cervical os. Causes painless bright red bleeding. If it is non-obstructing, trial of labor can be allowed
question
Abruptio Placenta
answer
Separation of the placenta from the uterus. Causes mild to severe pain with dark red blood (venous bleeding). Risk factors: chronic HTN, cocaine, preeclampsia, multiparity, smoking, trauma.
question
Calculating depth of ETT?
answer
3 x Diameter of ETT
question
Croup aka laryngotracheobronchitis

answer
- MCC Parainfluenza, RSV, Influenza A/B - Well looking patient - Slow onset - Mild-moderate stridor - Barking Cough - Able to swallow - Hoarse voice - "Steeple sign" on XR - Treatment: Racemic epinephrine, no intubation needed
question
Epiglotitis

answer
- MCC H. Influenzae, Staph, Strep - Toxic and unwell apperance - Abrupt onset - High fever - Moderate-severe stridor - Unable to speak - Unable to swallow - "Thumb print sign" on XR - Treatment: Intubate in the OR with ENT available, no time for XR or any imaging, Give ABx. Do not give racemic epi (its contraindicated)
question
Racemic Epinephrine
answer
Helpful in Croup, Bronchiolitis or post intubation croup in the PACU
question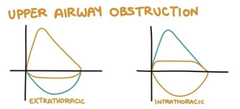
Flow volume Loops
answer
EXPiratory Blunting is due to INTRAthroacic Obstruction (i.e. Mediastinal mass, lower tracheomalacia, lower tracheal mass) INSPiratory Blunting is due to EXTRAthoracic Obstruction (i.e. Vocal cord paralsis, thyroid mass, laryngomalacia, epiglotitis) INSP- & EXPiratory Blunting is due to a FIXED lesion (i.e. Tracheal stenosis or choanal atresia)
question
DiGeorge Syndrome
answer
CATCH-22 Cardiac disease (TOF) Abnormal Facies Thymic Atresia Cleft Palate Hypocalcemia Due to Deletion of Chromosome 22
question
Rigidity associated with Neuroleptic Malignant Syndrome OR Malignant Hyperthermia resolves after administration of muscle relaxant?
answer
NMS
question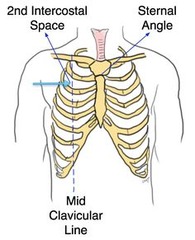
Where do you perform a needle thoracotomy?
answer
Second intercostal space, midclavicular line (below 2nd rib)
question
True or False? Factor 7 administration can overcome a relative deficiency of factors in the intrinsic pathway?
answer
True. Factor 7 couples with tissue factor to activate the common pathway (10--5-->2-->1--->Fibrin clot). The main job of the intrinsic pathway is to synergistically support the continued formation of thrombin once the extrinsic pathway is started.
question
Vitamin K is needed for production of which factors?
answer
Factors 2, 7, 9, 10, protein C and protein S
question
Fat Embolism Syndrome presents how and when?
answer
SOB, respiratory failure, RHF, mental status changes, coagulopathic changes, petchiae (pathognomic). It usually occurs 1-3 days postop. Diagnosis of exclusion but BAL can show fat droplets in macrophages.
question
Oculocardiac Reflex Pathway?
answer
Afferent: Ciliary nerves/Trigeminal Nerve - Ophthalmic division (through ciliary ganglion and gasserian ganglion) Efferent: Vagus Nerve
question
Following administration of Sulfur hexafluoride, what anesthetic should you avoid intraoperatively and for how many days after should this be avoided?
answer
Nitrous oxide; Lasts 10 - 28 days! But avoid for 4-6 weeks after use (per UK anesthesia)
question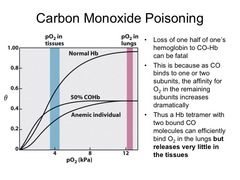
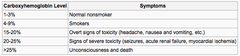
Carbon Monoxide Poisoning Affect on Pulse oximetry? Tx?
answer
COHgb will overestimate SpO2 showing slightly low to normal oxygen levels. Diagnosis to be made with ABG co-oximetry. Treatment with 100% oxygen.
question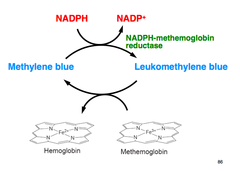
Methemoglobinemia affect on Pulse oximetry/ABG? Tx?
answer
MetHgb will overestimate SpO2 showing O2 levels in the 80%s. ABG will show normal PaO2 levels but the patient will be cyanotic (highly suggestive of MetHgbemia). Definitive diagnosis is to be made with co-oximetry. Treatment with Methylene Blue.
question
Functional Residual Capacity = what?
answer
ERV + RV
question
What factors decrease FRC?
answer
Restrictive lung disease, obesity, pregnancy, posture (FRC greatest to least: standing > sitting > prone > supine > trendelenberg) Not obstructive lung disease
question
Laminar flow is directly related to ____ where as turbulent flow is directly related to ____.
answer
Viscosity; Density "Las Vegas is Too Dense"
question
Laminar flow is seen in the ____ airways whereas turbulent flow is seen in the ____ airways.
answer
Distal; proximal/larger
question
A high Reynolds number (>2000) is more consistent with turbulent or laminar flow?
answer
Turbulent Flow R = (Velocity x Diameter x Density) / Viscosity
question
Heliox will reduce work of breathing how?
answer
Helium has decreased density compared to air so it will decrease the resistance caused by turbulent flow.
question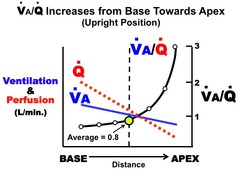
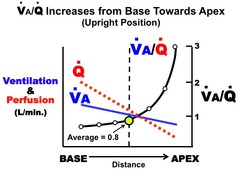
Ventilation and perfusion are maximal at what part of the lungs?
answer
Both are maximal at the base of the lungs. Perfusion is higher than ventilation at the base. Ventilation is higher than perfusion at the apex.
question
What is the Alveolar gas equation?
answer
Palv = FiO2 (Patm - Ph2o) - PaCO2/RQ. This equation can explain why elevated PaCO2 can cause hypoxemia.
question
Cushing's Triad?
answer
Response to elevated intracranial pressures which involves: 1) Elevated BP 2) Bradycardia 3) Irregular respirations (slow and irregular)
question
What EKG changes would you see during a massive pulmonary embolism?
answer
You would see ischemic changes in the anterior leads, esp V1 and V2 indicating R heart strain. RBBB could also be seen with V1-V2 RR' complexes. The classic finding is S1Q3T3 (S wave in lead I, Q wave in lead III, and inverted T wave in lead III) but is rarely seen.
question
Absolute Contraindications to Extracorporeal Lithotripsy?
answer
Absolute: 1) Pregnancy 2) Coagulation disorder/Anticoagulation 3) Distal Obstruction of Renal Calculi Relative Contraindication: 1) Large Calcified Aorta 2) UTI 3) Pacemaker/AICD 4) Morbid obesity 5) Intraabdominal aortic Aneurysm
question
What is Autonomic Dysreflexia?
answer
In a patient with spinal cord injury (usually T6 or above), noxious stimulus below the level of injury causing an amplified sympathetic response below the level. There will be a strong parasympathetic response to follow. The patient will be hypertensive and bradycardic. You will see flushing above the lesion and pale, white skin due to vasoconstriction below. It can be caused by surgical stimulation, bladder distension, or fecal impaction. Consider spinal anesthesia, arterial line and sodium nitroprusside available.
question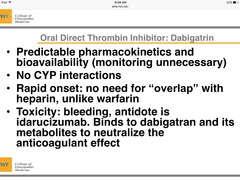
Dabigatrin reversal?
answer
Idarucizumab
question
Major side effect of CYCLOSPORINE
answer
Nephrotoxicity
question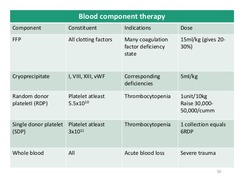
Cryoprecipitate contains what?
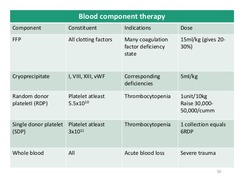
answer
Factor VIII vWF Factor XIII Fibrinogen Fibronectin FFP contains all the plasma proteins that is found in whole blood including all factors. Cryoprecipitate is prepared by thawing FFP and allowing the larger molecules to precipitate which is the centrifuged and frozen.
question
Major side effect of CISPLATIN
answer
Nephrotoxicity
question
Major side effect of DOXORUBICIN
answer
Cardiotoxicity
question
Major side effect of VINCRISTINE
answer
Neurotoxcity
question
Major side effect of BLEOMYCIN
answer
Pulmonary fibrosis
question
Type 1 Error
answer
False Positive
question
Type 2 Error
answer
False Negative
question
To measure ICP the correct level to place the transducer is the _____.
answer
External auditory meatus
question
TV = ___mL/kg
answer
7mL/kg
question
FRC = ___mL/kg
answer
30mL/kg
question
Vital Capacity = ___mL/kg
answer
60mL/kg
question
Total lung capacity = ___ mL/kg
answer
90mL/kg
question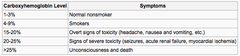
At what % of CO would you give supplemental oxygen?
answer
>10%; 10% or less is normal for smokers
question
Which antibiotic has the potential to prolong neuromuscular blockade?
answer
Aminoglycosides (i.e. gentamycin, amikacin, tobramycin, stretomycin, neomycin). NOT erythromycin, PCN or cephalosporins.
question
The carotid sinus Function? Location? Manipulation can cause what? Afferent limb? Injecting local anesthetic at the sinus can cause what?
answer
It is a baroreceptor that is located at the base of the internal carotid artery that functions as a baroreceptor. Manipulation of the carotid sinus can lead to profound bradycardia and hypotension that is ameliorated during a carotid artery surgery by injecting local anesthetic at the carotid bifurcation. The afferent limb of this reflex is mediated by the Glossopharyngeal nerve. Injecting local anesthetic can actually cause significant hypertension intra- and postoperatively.
question
The carotid body Function? Location? Afferent limb? Inhibited by? Bilateral CEA would cause what?
answer
Chemoreceptor cells that are located at the bifurcation of the ECA and ICA. They function mainly to respond to decreases in O2 tension <60mmHg by increasing ventilation. Afferent impulses are sent via the glossopharyngeal nerve (CN IX). It is inhibited by volatile anesthetics, BZDs or opioids. Note that a bilateral carotid endarterectomy would result in significant impairment of the hypoxic drive.
question
What would you see on an ABG in a third trimester pregnant woman?
answer
Mild, chronically compensated respiratory alkalosis. They would have elevated ventilatory rates due to an elevation in progesterone. PaCO2 would be around 30mmHg
question
Normal ABG values? Normal Cl?

answer
pH: 7.35-7.45 PaO2: 80-100mmHg PaCO2: 35-45 (45 respiratory acidosis) HCO3: 22-28 (28 metabolic alkalosis) Cl: 96-106
question
Methadone Mechanism of action? Major side effect?
answer
NMDA recepter antagonist and NE+Serotonin Reuptake inhibitor QTc prolongation, can lead to Torsades de point High doses of methadone (>60mg daily) can put you at increased risk for Torsades
question
Transplanted Heart Patient What medications act directly on a transplanted heart? What are some examples of medications that do not? Baseline heartrate?
answer
- Any medication that acts on B receptors directly such as Dobutamine, Isoprotenernol, Epinephrine, Norepinephrine. However, the heart rate response may be exaggerated because there is no parasympathetic innervation to counter the increased heart rate - Indirect drugs that affect rate will not be effective (antimuscarinics, anticholinesterases, pancuronium, digoxin). Use direct acting agents (isoproterenol, epinephrine). - Lack of vagal tone will result in baseline rate of 90-100. About 25% of patients will develop a bradycardia that will require implantation of a permanent pacemaker.
question
How does laryngoscopy affect a patient with a transplanted heart?
answer
You will not see a vagal response to laryngoscopy. Vagal bradycardic reflexes will also be absent due to denervation of parasympathetics (laryngoscopy, hypertension, carotid sinus massage).
question
Pacemaker Settings What is position 1? what is position 2? What is Position 3? What is asynchronous mode?
answer
Position 1 = Chamber paced (A, V, Dual or O[None]) Position 2 = Chamber sensed (A, V, Dual or O [None]) Position 3 = what the device does in response to the sensing (Inhibited, Triggered, Dual [both] or O [None]) Asynchronous mode = AOO, VOO or DOO
question
Two ways of stopping the heart during EVAR?
answer
Adenosine and rapid right ventricular pacing.
question
Phantom pain Occurrence following amputation? Definition Difference between phantom pain and stump pain?
answer
Occurs in 90% of patients in the first 6 months following amputation surgery Defined as unpleasant or painful sensation in the missing body part. It is usually intermittent with intervals between 1 day - several weeks. Phantom pain that lasts > 6 months is usually refractory to treatment. Stump pain is different from phantom pain in that stump pain is usually due to local processes such as soft tissue infection, skin lesions or provoked by traction or pressure on the remaining body part.
question
Keys for treating LVAD patient?
answer
Maintain preload, reducing afterload and preserving R heart function. This means: Avoid hypovolemia. Recommend MAPs between 60 and 80mmHg. Preserve R heart function by avoiding elevations in pulmonary artery pressures (avoid hypercapnia)
question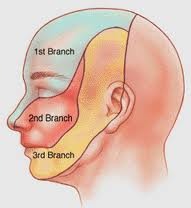
Trigeminal Neuralgia (tic dolereaux) R or L side affected more? Men or women more?
answer
R >> L side Women >> Men Pain is self limited Treatment: Anticonvulsants are first line. Baclofen and Neurontin can help as well. Surigcal treatments are available for patients who have failed medical management. Microvascular decompression (MVD), nerve lesion techniques and motor cortex stimulation are available. Question sample: A woman presents with recurrent flashes of severe pain at the junction of her R upper lip and the nasolabial fold despite normal facial appearance and neurologic exam. Brushing her upper molars triggers these attacks. Most likely diagnosis? Classical Trigeminal Neuralgia
question
What is allodynia?
answer
It is he triggering of a pain response from stimuli which do not normally provoke pain.
question
What is the difference between CRPS Type 1 vs Type 2?
answer
CRPS Type 1 (RSD) is a syndrome where chronic pain (normally in an extremity) appears to be associated with sympathetic nervous system dysfunction. It can be the result of a trivial injury (ie burn, ankle sprain, cut) on that extremity CRPS Type 2 (Causalgia) is a syndrome where chronic pain is the result of prior nerve injury. Management: Step 1: physical therapy Step 2: medical management with TCA, gabapentin, mild opioid if needed for physical therapy Step 3: diagnostic sympathetic block Step 4: somatic block of sympathetic block Step 5: spinal cord stimulator / intrathecal medications
question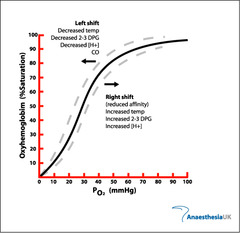
What are some things that cause R shift on the Oxyhemoglobin dissociation curve?
answer
Increase in Temp, PaCO2, BPG, H ions Decrease in pH
question
What causes a L shift on the oxyhemoglobin dissociation curve?
answer
Decrease in Temp, PaCO2, BPG, H ions Increase in pH Increase in CO Increase in MetHgb Increase in HbF
question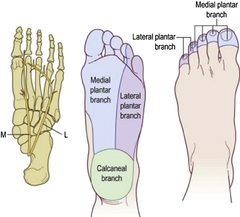
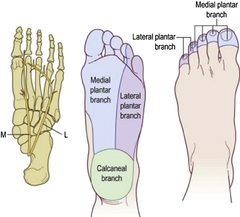
Explain the sensory nerve distribution of the foot/ankle.
answer
The POSTERIOR TIBIAL NERVE covers the heel and plantar surface of the foot. The medial ankle is covered by the Saphenous (femoral nerve) and the lateral surface is covered by the Sural Nerve. The superior portion of the foot is covered by the common peroneal nerve. Only thing to note is that the webbing between the 1st and 2nd toe is covered by the deep peroneal nerve while the rest is covered by the superficial peroneal nerve.
question
What metabolizes codeine, oxycodone and hydrocodone?
answer
CYP2D6 Codeine is active and undergoes O-demethylation by CYP2D6 to create morphine.
question
Alfentanil has a higher or lower volume of distribution?
answer
It has a lower volume of distribution which means that it has a shorter duration of action. It also has a lower pKA so it has the fastest onset and crosses the BBB quickly. It has a brief duration of action due to redistribution.
question
Naloxone Onset? Dose? Half life?
answer
Onset 1-2 mins Dose 0.01-0.1mg/kg; 0.04mg q 3-6 mins and then infuse 4-5mcg/kg/hr t1/2 = 30-60mins
question
What is the reason for the hypercoagulable state in pregnant women?
answer
Increased fibrinogen and factor VII levels and decreased anticlotting factors.
question
Non ionized = lipophilic or hydrophilic?
answer
Lipophilic (lipid soluble).
question
pKa definition
answer
pH at which a compound exists as 50% ionized and 50% unionized The lower the pKA, the more the nonionized form (the more lipid soluble and therefore the faster the onset)
question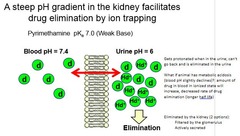
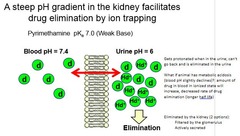
Explain ion trapping.
answer
If there is a pH gradient, ionized substances are trapped on the side that the pH favors ionization. For weak bases, the drug will accumulate on the acidic side of the membrane. For example, the nonionized fraction of a local anesthetic agent (weak base) crosses the placenta, where it is changed to the ionized form in the relatively acidic fetus. The ionized form cannot leave the placenta. Further, the nonionized drug continues to enter fetal circulation.
question
A patient on enoxaparin for DVT ppx, when is it appropriate to remove or place an epidural? What about in a patient receiving "treatment" dosing of lovenox?
answer
12 hours for DVT ppx 24 hours for "Treatment"
question
A patient who is receiving subQ heparin for DVT ppx, when is it appropriate to perform neuraxial anesthesia? What about a patient receiving IV heparin?
answer
There are no contraindications if the daily dose is <10,000units. IV heparin - delay needle/catheter placement 4 hours after last dose and document a normal aPTT. Restart after 1 hour.
question
Tumescent Liposuction Lidocaine dose? Epinephrine dose? Toxic range of lidocaine? Why is it so high compared to IV toxic range? Peak levels of lidocaine occurs when?
answer
- Lidocaine 0.05%, - Epinephrine 1:1,000,000 - Dose range: 35- 55 mg/kg of lidocaine injected. - The range is higher because the adipose tissue acts as a resevoir (lidocaine is highly lipophilic). Also the epinephrine vasoconstricts. - 12-14 hours after
question
Specificity = ? Sensitivity = ?
answer
Specificity = TN / TN + FP Sensitivity = TP / TP + FN
question
FA/FI Ratio notes
answer
FA = Alveolar end tidal concentration FI = Inspired concentration The larger blood:gas partition coefficient means a lower FA/FI ration (due to increased uptake). The lower the FA/FI ratio the slower the onset.
question
Onset of anesthesia is faster in volatile agents with lower/higher blood:gas coefficients?
answer
Lower. Desflurane 0.42 N2O 0.47 Sevo 0.63 Iso 1.4 The more soluble the gas, the higher the blood:gas coefficient, and the slower the onset
question
How do the following affect FA/FI? Ventilation? Cardiac output? Children vs Adults?
answer
Increased ventilation, increases FA/FI Decreased CO, increasees FA/FI Children have a more rapid
question
Surgical emergency: Aortic dissection type A or type B?
answer
Type A - involves the ascending aorta and possibly the AV Type B - can be managed medically with combined a and B blockers. SBP goal < 110mmHg
question
Why is there a resistance to NMDBs in burn patients?
answer
It is attributed to the proliferation of extrajunctional receptors.
question
When is it unsafe to use succinylcholine in burn patients?
answer
After 24 hours, for up to one year afterwards. It can result in fatal hyperkalemia.
question
Treatment of Transient Neurologic Symptoms? Increased risk of TNS with what? How is this different from neuraxial hematoma or cauda equina syndrome?
answer
NSAIDS Increased risk of TNS include: - Lidocaine OR Mepivacaine spinal anesthesia (7 fold increase compared to other LAs) - Lithotomy position - Outpatient surgery - Knee arthroscopy - Obesity **LA concentration, baricity, w/ or w/o epinephrine, and technique do not contribute to TNS*** It's different from an epidural hematoma and CE in that the patient will not have bowel or bladder dysfunction. There will only be back pain with possible radiation to the legs.
question
Myotonic Dystrophy
answer
- Patient presents with persistent muscle contraction after voluntary contraction ie unable to let go of a handshake - Autosomal dominant - Likely due to intracelluar ATP system that fails to return Ca to SR. - Contractions are not relieved by NMBDs or deep anesthesia - Avoid succinylchoine - can be severe enough to impair ventilation Coexisting disease: - Cardiac abnormalities - conduction defects and CMP - Respiratory - restrictive lung disease and OSA Triggers: - Succinylcholine - Shivering - Excessive stimulation - Hypothermia
question
In hypothermic patients, the MAC increases/decreases?
answer
Decreases
question
Lithotomy position is associated with which nerve injury, most commonly? How would the patient present
answer
Common peroneal. Loss of the ability to dorsiflex (footdrop) and evert the ankle.
question
Cardiac Tamponade
answer
Equalization of the DIASTOLIC pressure in all 4 chambers of the heart with the pressure inside the pericardium. You would see pulsus paradoxus - abnormally large decrease in SBP on inspiration. During inspiration there is increased R sided filling which causes the interventricular septum to shift to the left causing a decrease in BP. You would also see electrical alterans. Clinically you would see dyspnea, hypotension, tachycardia, distant heart sounds, orthopnea, and JVD. "FAST FULL AND TIGHT" FAST CO is HR dependent FULL SV is dependent on adequate preload TIGHT vascular tone should be tight
question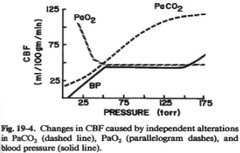
Cerebral blood flow is influenced by what?
answer
MAP, PaCO2, PaO2, and local brain metabolic activity.
question
HERBAL SUPPLEMENTS SIDE EFFECTS :( Ginger? Garlic? Ginko? Ginseng? Green Tea? Saw Palmetto? Fish Oil?? Kava? Ephedra? St. Johns Wart?
answer
- Ginger - inhibits thromboxane synthetase. - Garlic - Inhibits platelet aggregation. Discontinue for 7d prior - Ginko - inhibits platelet aggregation. Discontinue 36h prior - Ginseng - inhibits platelet aggregation and decreases blood sugar. Discontinue 24h prior - Green tea - inhibits platelet aggregation. Discontinue 7d prior - Saw Palmetto - can cause increased bleeding intraop - Fish Oil - can cause increased bleeding intraop - Kava - anxiolytic, causes sedation, decreases MAC, can cause HEPATOTOXICITY - Valerian - causes sedation, decreases MAC. - Ephedra - HTN , tachycardia, seizures - St. Johns Wart - SNRI inhibitor; also EZYME INDUCER of cytochrome P450 systems
question
Chronic opioid use can lead to increase or decrease of cortisol levels, testosterone/estrogen/LH/FSH levels?
answer
Decrease.
question
NMDA Receptor is blocked by what 5 medications?
answer
Ketamine, N2O, Methadone, Xenon and Magnesium
question
Fenoldopam mechanism of action?
answer
Antihypertensive. Selective D1 agonist. Direct renal vasodilator. Causes naturesis and diuresis. Effective in hypertensive crisis
question
Effect on MAC: Hyponatremia? Hypercarbia? Hypothermia? a2 agonists? Acute EtOH? Chronic EtOH? Red hair? Pregnancy?
answer
HypoNa - decreases MAC Hypercarbia - decreases MAC Hypothermia - decreases MAC Lithium - decreases MAC a2 agonists - decreases MAC Acute EtOH - decreases MAC Chronic EtOH - increases MAC Red hair - increases MAC Pregnancy - decreases MAC
question
Intraoperative awareness vs Dreaming vs Explicit Memory vs Implicit Memory
answer
Intraoperative awareness - postoperative recall of events while under general anesthesia Dreaming - experiences that patients are able to remember postoperatively that they believe to be dreaming and that they think occurred during general anesthesia Explicit Memory - conscious recollection of prior experiences Implicit Memory - unconscious memory of an experience that produces a change in performance or behavior. It can usually be accessed by hints or using a word stem
question
How long must you wait for elective surgery after a bare metal stent? After a drug eluding stent? After a CABG? Are you allowed to take care of a patient with a new stent in the surgery center?
answer
BMS - 4-6 weeks DES - 12 months CABG - 30 days PCI/Balloon angioplasty - 2 weeks If out of the window, continue dual antiplatelet medications PERIoperatively unless the elective procedure is with a high risk of bleeding. Then d/c plavix 5 days prior and reload postop. Alphabetical order: Balloon angio (2 wks) ; BMS (4-6 wks) ; DES (12 mo) NO; send to a facility that has cardiology service
question
Dantrolene will increase or decrease MAC?
answer
Decrease
question
Sentinel Event is defined as?
answer
Any event that is unanticipated or with an unintended outcome that has the potential to cause patient harm. A near miss can qualify as a sentinel event. A patient complaint or an error in judgement cannot be considered a sentinel event.
question
Some indications of Hyperbaric Oxygen? Absolute Contraindication of HBO?
answer
- Carbon Monoxide Levels ; 25% - Air or Gas embolism - Soft tissue necrosis - Decompression sickness - Diabetic Wound treatment Absolute contraindication = untreated Pneumothorax
question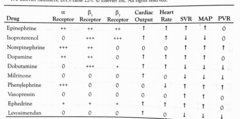
Dobutamine affect on PVR, SVR and MAP? What about HR and Cardiac output? Receptors?
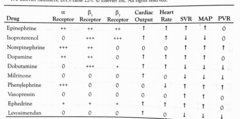
answer
Dobutamine decreases SVR, MAP and PVR because of its affect on B2 receptors. It increases HR and CO because of its affect on B1. B1: +++ B2: +
question
Milrinone affect on SVR and PVR? What about CO? Mechanism?
answer
Milrinone causes decrease in SVR and PVR. It causes increase in CO. Mechanism of Action: PDE III Inhibitor (decreased cAMP breakdown --> increased Ca breakdown in myocardium)
question
Aortic Stenosis Anesthetic plan in a patient with Aortic stenosis? Normal valve area? Classic symptoms?
answer
- Maintain HR 60-90. Bradycardia can be devastating as they are HR dependent. Maintain afterload by avoiding hypotension. Treat hypotension with small doses of phenylephrine. - Normal valve area 2.5-3.5cm2; Symptomatic stenosis occurs at 0.8-0.9cm2 and critical AS when valve area ;0.7cm2 - Angina, syncope, and angina. 50% mortality at 5, 3 and 2 years respectively.
question
Aortic Dissection Risk factors?
answer
Predisposing conditions include - male sex - age greater than 60 years - HTN - Marfan syndrome or other connective tissue disease - congenital heart disease, including coarctation of the aorta and bicuspid aortic valve - pregnancy
question
What is likely being compressed during a medistinoscopy and what side should you monitor SpO2 and BP?
answer
The inominate artery. You should put the Aline and SpO2 on the R side so that you dont have undetected hypotension.
question
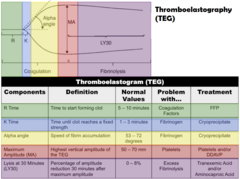
TEG

answer
Thromboelastogram components shown in Figure 2 include: Reaction time (R) measures the time to initial clot formation. R can be prolonged when clotting factors are deficient or in the presence of heparin, low molecular weight heparin, direct thrombin inhibitors, warfarin, etc. Kinetics (K) represents the rate at which fibrin strands form and begin to cross-link to form the fibrin meshwork. Angle (?) represents the rate of clot formation and reflects fibrinogen activity. Maximum amplitude (MA) represents whole clot strength and reflects many aspects of clot formation, including platelet number and function as well as the fibrin contribution to clot strength. G is derived from the MA and is also a measure of overall clot strength. The G value is used to discuss platelet function and clot strength. Estimated percent lysis (EPL) represents clot breakdown as seen in patients with disseminated intravascular coagulation or hyperfibrinolysis.
question
Sodium Nitroprusside Mechanism? Toxicity?
answer
Mechanism of Action: Increases cGMP Toxicity: 1) Thiocyanate 2) Cyanide 3) Methemoglobinemia
question
SSEP Usually measure which nerves (which correlate to which cerebral distribution?) What qualifies as a significant change? False positives can be caused by what? Do NMDBs block SSEPs?
answer
- Posterior tibial nerve (ACA) and Median nerve (MCA) - Significant changes: 50% drop in amplitude and 10% increase in latency - False positives can be due to anesthetics, hypothermia, hypotension, and anemia - Volatile anesthetics and N2O are most suppressive - NMDBs do not affect SSEPs.
question
What part of the spinal cord do SSEPs test and what is the spinal blood supply for these territories?
answer
- SSEPs for the upper extremity test the dorsal column which is supplied by the Posterior Spinal Artery. For the lower extremity, it will test the dorsal lateral funiculus which is supplied by the Anterior Spinal Artery.
question
Medications that undergo ester hydrolysis?
answer
- Succinylcholine (Plasma cholinesterase) - Remifentanil (non specific esterases) - Esmolol (nonspecific esterases) - Mivacurium - Atracurium - Cisatricurium - All ester local anesthetics i.e. 2-Chloroprocaine, Procaine, Cocaine
question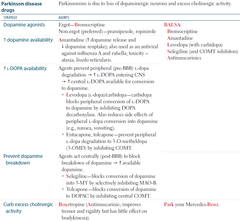
Parkinson's Disease Due to a deficiency in what neurotransmitter? This causes excessive amounts of ____? What medications should you avoid? What medications are ok to use?
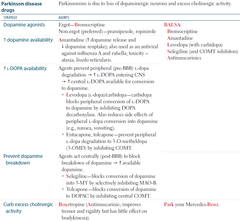
answer
- Dopamine (due to loss of substantia nigra) - Acetylcholine - Avoid dopamine blocking medications such as: 1) Droperidol 2) Metaclopromide 3) Antipsychotics (haldol, chlropromazine, etc) - OK to use: 1) Ondansetron 2) Antihistamines 3) Cannabinoids (Dronabinol)
question
Familial Hypokalemic Periodic Parlysis
answer
- HypoK+ periodic paralysis is a disorder characterized by episodes of weakness when serum K drops - Lasts anywhere from hours to days - Spares muscles of respirations - Avoid glucose containing solutions, hypothermia, or any medications that cause intracellular shifts of K+ (such as B blockers) - Remember, insulin causes K to move into the cells - Muscle relaxants (including succinylcholine) are OK Triggers: - Exercise followed by rest, high carbohydrate meals, high sodium meals, sudden changes in temperatures - Low dose acetazolamide may prevent attacks
question
Familial Hyperkalemic Periodic Paralysis
answer
Management: - Give glucose and insulin - Give Calcium - Give diuretics - Avoid succinylcholine
question
Innervation of the abdominal viscera?

answer
Distal esophagus to the Transverse colon is supplied by the CELIAC PLEXUS Descending colon to the rectum is supplied by the SUPERIOR HYPOGASTRIC PLEXUS (which also covers GU and perineum)
question
Conditions that will increase DLCO? Conditions that will decrease DLCO?
answer
Conditions that increase DLCO: - Asthma - Exercise - Polycythemia - L-->R shunt Conditions that decrease DL CO will be anything that impairs gas exchange across the alveolar membrane. - COPD - Heart failure - Anemia - TB, Asbestos, Sarcoid
question
In a patient who is in her third trimester, are you expected to find an increase or decrease in the following: Minute ventilation (due to what hormone?) Tidal volume Respiratory rate Vital Capacity FEV1 FRC ERV RV
answer
Minute ventilation - increased due to progesterone Tidal volume - increased Respiratory rate - more or less the same Vital Capacity - more or less the same FEV1 - more or less the same FRC - decreased ERV - decreased RV - decreased
question
Cytochrome P450 inducers or inhibitors?

answer
Carbamazepine - inducer St. Johns Wort - inducer Omeprazole - inducer Phenytoin - inducer Phenobarbital - inducer "OCPPS" Nicardipine - inhibitor Grapefruit - inhibitor Isoniazid - inhibitor Cimetidine - inhibitor Erythromycine - inhibitor "NICE-G"
question
Diseases linked to MH?
answer
Central core disease, King-Denborough syndrome, and Evans myopathy are clearly linked to MH.
question
Best preoperative tests prior to thoracotomy to assess LUNG PARENCHYMAL FUNCTION? To assess CARDIOPULMONARY RESERVE? To assess RESPIRATORY MECHANICS? (include minimum values that would result in pulmonary complications)
answer
Lung Parenchymal Function: DLCO (ppo >40%) Cardiopulmonary Reserve: VO2max (>15mL/kg/min) Respiratory Mechanics: FEV1 (ppo >40%)
question
What are some examples of medications that cause uterine smooth muscle relaxation?
answer
Terbutaline, magnesium sulfate, nitroglycerine, and inhaled inhalation anesthetics relaxes uterine smooth muscle.
question
What are some medications that cause uterine smooth muscle contraction?
answer
Oxytocin, Carboprost (Hemabate), Methergine, Cytotec Oxytocin - causes hypotension Hemabate - avoid in asthmatics Methergine - avoid in hypertensives and CAD/CVA pts
question
What is Hepatopulmonary Syndrome?
answer
Hepatopulmonary syndrome (HPS) is defined by the presence of liver dysfunction, unexplained hypoxemia, and abnormal vasodilation of intrapulmonary vessels. There is also a phenomena called orthodeoxia which is manifested by hypoxia when standing that improves when lying supine. This resolves following liver transplantation.
question
Opioid Induced Pruritis treatment?
answer
Zofran Propofol Nalbuphine (Nubain) Butorphanol (Stadol)
question
Opioids other effects? Immune Effects?
answer
Opioids suppress resistance to infection by modulation of immune cellular activity (T Cells, macrophages, NK cells)
question
Which medications do you dose using Ideal Body Weight? Total Body Weight? Lean Body Weight?
answer
Ideal Body Weight: NMDBs Total Body Weight: Succinylcholine and Propofol (infusion) Lean Body Weight: Opioids and Propofol (induction)
question
E Cylinder Volume Pressure O2 ?? ?? Air ?? ?? N2O ?? ??
answer
E Cylinder Volume Pressure O2 625L 2000psi Air 625L 2000psi N2O 1590L 750psi N20 will only start to drop in pressure at ~400L. Only way to reliably estimate the volume is to weight the cylinder PSI / (200x flow) x 60
question
Most common serious adverse event following a celiac plexus block?
answer
Paraplegia
question
Maternal Physiologic Changes Hematologic: Blood volume? Plasma volume? RBCs? Hgb? Hct? Factor VII and Fibrinogen?
answer
Blood volume? Up Plasma volume? Up RBCs? Up Hgb? Down Hct? Down Factor VII and Fibrinogen? Up vWF Up
question
Maternal Physiologic Changes Electrolytes: RBF/GFR? Serum Cr/BUN? HCO3? Na? K? Cl?
answer
RBF/GFR? Up Serum Cr/BUN? Down HCO3? Down to compensate for resp alk Na? Down K? Down Cl? Down
question
Maternal Physiologic Changes Respiratory: Rate? Tidal volume? ERV? FRC?
answer
Rate? No change Tidal volume? Up by 50% (due to progesterone) ERV? Down by 25% RV? Down by 15% FRC? Down by 20-80% TLC, VC, CC unchanged
question
Maternal Physiologic Changes Cardiac: Rate? SV? CO? SVR/MAP?
answer
Rate? Up SV? Up CO? Up (up 40% to meet metabolic demands of mom and baby) SVR/MAP? Down CVP? No change
question
What neuromonitoring technique is most affected by volatile anesthetics?
answer
MEP > SSEP > VEP > BAER They are not altered by narcotics. EMG and nerve stimulation are not affected by volatiles but avoid NMBDs
question
Subq Fentanyl Patch Time to therapeutic onset? Systemic effects after removal?
answer
Type to therapeutic onset? 12 hours Time after removal? 16 hours - 3 days
question
Weight change side effects: TOPAMAX LYRICA NEURONTIN
answer
TOPAMAX = weight loss LYRICA, NEURONTIN = weight gain
question
Bainbridge Reflex
answer
Increase in heart rate in response to increase venous return. The reflex is mediated by stretch receptors in the walls of the atria. Stimulation of sympathetic fibers and inhibition of vagal outflow from the medulla is thought to be the primary efferent pathway in the Bainbridge reflex to produce an increase in heart rate.
question
Reverse Bainbridge Reflex
answer
Decrease in venous return results in bradycardia, occurs during spinal anesthesia. Otherwise known as Bezold Jarisch Refelx
question
Of the IV anesthetics, the only medications to cause BURST SUPPRESSION are what?
answer
Etomidate, Propofol and Barbiturates. Inhaled anesthetics also can induce burst suppression
question
Critical Illness Myopathy
answer
Distal weakness and muscles of respiration first. Depressed DTRs and slightly elevated CKs. More prevalent in patients who are receiving NMBDs + steroids in the ICU
question
Amitryptiline Mechanism of action with what side effects.
answer
TCA with anticholiergic effect.
question
Postpartum Foot drop due to
answer
Lumbosacral Nerve Injury
question
NPO Guidelines for the following?
answer
Clear liquid 2h Breast milk 4h Formula 6h Non human milk 6h Light non fatty food 6h Fried food 8h
question
Bupivicaine Toxicity in Infants
answer
2.6
question
Urinary specific gravity for a patient who is hypovolemic/dehydrated?
answer
>1.010 = dehydration/hypovolemia
question
Strong ion difference =
answer
SID= [Na + K + Ca + Mg]-[Cl+Lactate] Disturbances that increase SID increase the blood pH causing alkalosis; also dehydration can cause increase in SID Disturbances that lower SID cause acidosis Normal SID = 40
question
Hyperkalemia - diagnosis and treatment?
answer
Classic EKG changes include peaked T waves, shortened QT intervals, long PR Severe - most rapidly treated by hemodialysis Mild/moderate: 1) insulin/glucose to facilitate intracellular transfer of potassium 2) Calcium to stabilize the cardiac membrane 3) Kayexelate and loop diuretics to eliminate potassium 4) B agonists
question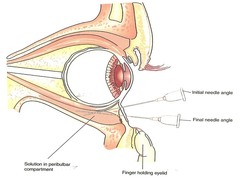
Are peribulbar blocks safer than retrobulbar blocks? Why?
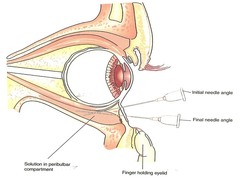
answer
Peribulbar blocks are generally safer because the needle transverses a shallower path without directly advancing the needle towards the optic nerve or the central retinal artery
question
Aldosterone effects on sodium and potassium? How would a Conns syndrome patient present? What medicine would directly counter aldosterone?
answer
Aldosterone is released following activation of renin angiotensin pathway in response to hypovolemia or renal hypoperfusion. Aldosterone works on the distal tubules and collecting ducts to upregulate Na/K pumps. It promotes the reabsorption of Na and excretion of K. Supraphysiologic aldosterone secretion leads to HTN and hypokalemia. Spirinolactone is an aldosterone receptor antagonis.
question
Sodium deficit formula? ***skip
answer
(140 - serum sodium) x (kg x 0.6) Typically, 50% of the Na deficit should be corrected in the first 24hrs and the rate of hypertonic saline should never be higher than 100mL/hr.
question
Magnesium toxicity levels and symptoms Treatment of toxicity?
answer
5-6: Hypotension and bradycardia 6-12: Prolonged PR 12: DTR loss, weakness, can progress to respiratory depression 18: SA/AV node block 20-25: Asystole Tx of Toxicity with IV Calcium
question
Celiac plexus block
answer
Innervates the stomach, small bowel, proximal large bowel, spleen, gallbladder, pancreas, kidneys, and adrenal glands T12-L1 Complications include orthostatic hypotension (MOST COMMON), back pain, retroperitoneal hematoma, hiccups, diarrhea, abdominal aortic dissection, paraplegia (due to subarachnoid injection).
question
In a patient receiving heparin for 5 days or more, what study should be done prior to neuraxial anesthesia?
answer
Platelet count in case of HIT.
question
Differences between aortic and radial arterial waveforms?

answer
A radial waveform will have: 1) a higher systolic pressure 2) a wider pulse pressure 3) a more pronounced diastolic wave 4) a more delayed and slurred dicrotic notch
question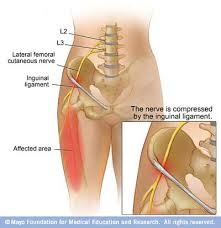
What is meralgia paresthetica?
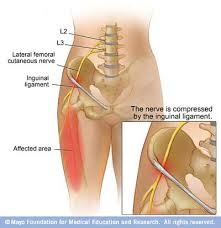
answer
Entrapment of the lateral femoral cutaneous nerve.
question
VACTERL stands for?
answer
Vertebral defects Anal atresia Cardiac defects TEF Renal anomalies Limb abdmormailties Typically infants undergo repair of TEF first. Then, if there are cardiac abnormalities they will be repaired next. Imporforate anus is repaired next. Prior to considering a caudal for this procedure, consider a lumbosacral MRI to evaluate for neural tube defects (the v in vacterl). These defects are contraindications for caudal anesthesia. CHD are the most common defect associated with TEF, occurring in up to 75%
question
Hyperalimentation is commonly associated with what lab abnormalities?
answer
Hypophosphatemia Hypo-/hyper glycemia Acute liver injury/elevated PTT - usually requiring vitamin K supplementation
question
Pregnancy effects on coagulation? Which factors increase? Which factors decrease?
answer
Factors that increase include I (fibrinogen), VII, VIII, IX, X, XII and vWF. Factors that decrease include XI, XIII, antithrombin III, tPA and protein S Factors that develop resistance = Protein C Dilutional thrombocytopenia usually results in a decrease in platelets by 10%.
question
The first presenting sign of an intrathecal injection in an infant is what?
answer
Apnea. Not hypotension because infants' have a relatively underdeveloped sympathetic nervous system. You would not see bradycardia until late hypoxemia.
question
Confirmatory tests for brain death
answer
Positive apnea test, EEGs (2 isoelectric tests 24 hrs apart) and determination of the absence of blood flow (via cerebral angio, MRI/MRA, transcranial Doppler). All reversible tests must be ruled out. Note: Brain death is a clinical diagnosis and confirmatory testing is not mandatory
question
List neuromonitoring that is least to most sensitive to volatile anesthetics
answer
Least to most sensitive to anesthesia: BAEP ; SSEP ; MEP ; VEP (BAEP = BArely affected, SSEP = Somewhat affected, MEP = Mostly affected, VEP = VEry affected
question
Changes in physiology in response to altitude? Acute changes? Chronic changes?
answer
The most important immediate adaptation is increased HR and then hyperventilation and thus increase in minute ventilation due to the decrease in PaO2, this via stimulation of the peripheral chemoreceptors (central chemoreceptors are not sensitive to falls in PaO2). This results in a respiratory alkalosis. This would normally suppress ventilation but in the next 48-96 hours, the pH of the CSF compensates via bicarbonate loss and bicarbonate is further excreted by the kidneys to return blood to normal pH. In the first 12-24 hours also note that there is a right shift in the OH curve caused by an increase in 2-3 DPG. Over 1-3 weeks, the body further compensates by increasing EPO secretion causing an increase in hematocrit. The increased minute ventilation remains increased as long as the person remains at a higher altitude
question
Peripheral chemoreceptors (carotid and aortic bodies) sense/respond to ____ while central chemoreceptors (medullary) sense/respond to _____.
answer
Peripheral receptors respond to hypoxemia and hypercarbia. Body needs oxygen and makes co2 Central receptors respond to hypercarbia.
question
What do you do for hypoxemia during OLV?
answer
First give CPAP to the nondependent (nonventilated) lung to allow ventilation to the down lung. Second, you can give PEEP to the dependent (ventilated) lung or increasing FiO2. If still hypoxemic consider unclamping the down lung. If this is not possible at the time, clamping of the branch PA on the non-dependent side to decrease intrapulmonary shunting. If absolutely necessary, institution of CPB would be the final option.
question
ACA stroke would present how? MCA stroke would present how?
answer
MCA - upper extremity and facial weakness ACA - lower extremity weakness
question
Conn's syndrome/Hyperaldosteronism affect on: Sodium? Potassium? H ions?
answer
Hyperaldosteronism causes hyernatremia, hypokalemia, metabolic alkalosis. Aldosterone causes sodium reabsorption in exchange for potassium and hydrogen ions. It's net effect is an expansion in ECF volume caused by fluid retention. It is stimulated by RAS. They should be on spirinolactone.
question
What is the most common congenital heart defect?
answer
Perimembranous VSDs - VSDs are the most common and perimembranous VSDs represent 70% of all VSDs
question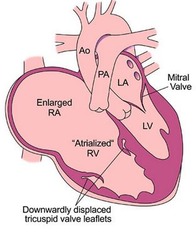
What is Ebstein's Anomaly?
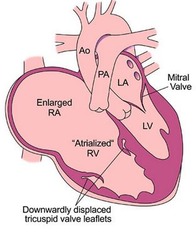
answer
It is a rare congenital anomaly characterized by downward displacement of the tricuspid valve. It is basically atrialization of a portion of the R ventricle causing a larger RA and a hypoplastic RV. The baby would present with cyanosis. It is associated with Wolff-Parkinson White syndrome.
question
How to differentiate between DIC and Liver disease?
answer
Factor VIII because VIII will be normal in cirrhotics.
question
Acute Epiglottitis management?
answer
Transport to the OR immediately and perform an inhaled induction. It is crucial to maintain spontaneous ventilation with PPV. Avoid N2O because of the potential for air trapping in the lungs via a ball-valve effect (meaning that air can go in but not out)
question
Surfactant is produced when and by what cells?
answer
It is made primarily after 32 weeks gestation. It is produced by type II pneumocytes. Infants born prematurely are at risk for RDS because of surfactant deficiency. Treatment with exogenous surfactant may reduce intrapulmonary shunting in RDS and hypoxemia.
question
Absolute contraindications for TEE? Relative contraindications for TEE?
answer
ABSOLUTE: Esophageal webs/rings Esophageal tumor Esophageal trauma Scleroderma Mallory Weiss Tear Zenker Diverticulum Active/Recent Variceal Bleed Esophagectomy Recent GI surgery RELATIVE: AAJ instability Symptomatic Hiatal Hernia Hx of Varices Hx of GI surgery PUD Coagulopathy
question
Tourniquets - how much do you inflate them?
answer
Upper extremity: 50mmHg above SBP Lower extremity: 100mmHg above SBP
question
B2 agonists (ritodrine and terbutaline) affect on uterine muscle?
answer
B2 agonists are tocolytics and relax uterine contractions and increase uterine blood flow. Other uterine relaxants: magnesium sulfate, nitroglycerine, and inhaled inhalation anesthetics
question
Treatment for uterine atony?
answer
(Don't need to know doses) Pitocin/Oxytocin: 10-20 U infusion over 10 mins - causes hypotension Methergine/Methylergonovine: 0.2 mg IM, contraindicated in preeclampsia, avoid in HTNives Hemabate/Carboprost (Prostaglandin F2?): 0.25 mg IM, may increase airway resistance so avoid in asthmatics. HEMAbate - Omar has Asthma, likes CARs Cytotec/Misoprostol (prostaglandin E1 analog) - avoid in maternal fever
question
Treatment for Cyanide toxicity?
answer
Hydroxocobalamin (first line) ; Amyl nitrate Elevated cyanide levels can be seen with smoke inhalation from residential or industrial fires. Elevated cyanide and thiosulfate levels can also be seen with administration of sodium nitroprusside. Thiosulfate is seen in long term administration of SNP, especially in pts with renal insufficiency. You would see elevated SvO2 and metabolic acidosis (cyanide will decrease utilization of O2 for ATP production and decrease VO2 thus increasing SvO2)
question
ARDS Severity
answer
P/F = PaO2/FiO2 ratio Mild: P/F ratio 200-300 Moderate: P/F ratio 100-200 Severe: P/F ratio 60mmHg with adequate Hgb 2) PEEP (up to 20mmHg) 3) Minimize FiO2 (;50%) 4) Minimize tidal volumes (6mL/kg)
question
Does atropine cross the placenta?
answer
Yes. It is a tertiary amine and is used if fetal bradycardia is a concern. It is usually given with neostigmine in the pregnant population.
question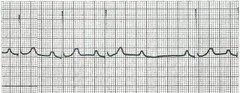
Pacemakers placement is indicated in which AV node blocks?
answer
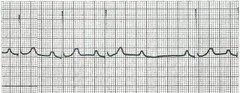
Second degree, Mobitz Type II ; Third degree block First degree = prolonged PR Second Degree, Mobitz Type 1 (Wenkebach) = progressive lengthening of PR interval with eventual dropped beat Second Degree, Mobitz Type 2 = intermittent nonconducted P wave not proceeded by PR lengthening (see picture) - the P waves will march at the same length Third degree = "two rhythms at the same time"; the P-P intervals are constant and the R-R intervals are constant irrespective of each other
question
Simple HR determination

answer
300, 150, 100, 75, 60, 50 etc
question
Median Nerve
answer
- C5-C7 - Motor: flexors of the wrist except for flexor carpi ulnaris - Sensory: palmar side of thumb, index, middle finger, and half of ring finger - Rescue block at the elbow - medial to the brachial artery in the AC fossa - It runs through the carpal tunnel and compression causes CTS
question
Use of Fetal Heart Rate Monitoring is feasible at the earliest when?
answer
The soonest you can do FHR monitoring is at 18-20 weeks gestation. Prior to this, the fetus is too small to monitor.
question
Treatment of stable SVT in patients with WPW?
answer
Procainamide is the drug of choice for patients with AVRT. Patients with AVNRT can be treated with adenosine, verapamil, B blockers, Diltiazem
question
Alkalosis does what to potassium? Insulin does what to potassium?
answer
Alkalosis drives potassium into cells. So less hydrogen ions = less potassium ions Insulin drives potassium into cells.
question
Neuraxial Block ASRA guidelines? - For the patient on ASA? - For the patient on Plavix? - For the patient on Heparin subQ? - For the patient on Unfractioned Heparin IV? - For the patient on prophylactic Lovenox? - For the patient on therapeutic Lovenox? - For the patient on Coumadin?
answer
- ASA? No contraindications - Plavix? Should be discontinued 7 days - Heparin SQ? No contraindications if dose is ;10,000 units - Unfractioned Heparin IV? Heparin gtt must be stopped 2-4 hours before needle placement with aPTT documented to be normal, can be restarted 1 hour after procedure - Lovenox ppx? Delay procedure for 12 hours from last prophylactic dose - Therapeutic Lovenox? Delay procedure for 24 hours, removal should be 12 hours after last dose - Coumadin? Should be discontinued for 4-5 days and check an INR
question
Lidocaine with epi toxic dose?
answer
7mg/kg of lidocaine with epi
question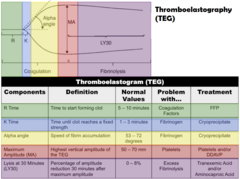
TEG What do you give for the following: Prolonged R? Prolonged K? Decreased MA? "Teardrop" configuration?
answer
Prolonged R = FFP Prolonged K = Cryo Decreased MA = platelets Teardrop = Antifibrinolytics ie TXA, eproetin
question
HOCM intraop strategy?
answer
1) Maintain preload 2) Optimize diastolic time by decreasing heartrate (beta blockers) 3) Maintain afterload (phenylephrine)
question
Alveolar gas equation? Which energy substrate is most effective for a ventilator wean?
answer
PAO2 = FiO2 x (Patm - PH2O) - CO2/RQ RQ = 0.8 Carbs = 1.0 Protein = 0.8 Lipids = 0.7 Lipids result in the lowest increase in CO2 production. So they would be most ideal for ventilator weaning by reducing the amount of CO2 that needs to be removed by ventilation.
question
Mixed Venous Oxygen (SvO2) - what causes an increase in SvO2? What causes a decrease?
answer
SvO2 is a measure of global oxygen delivery. Increase: - Increasing Hgb concentration - Increased SaO2 (via increased FiO2) - Increased CO (eg Sepsis) - Decreased VO2 (eg cyanide, sepsis, CO, MetHgb, Hypothermia) Decrease: - Increased O2 Consumption (eg hyperthermia, shivering, pain) - Decreased CO (eg MI, hypovolemia) - Decreased Hgb - Decreased SaO2
question
Causes of Metabolic Acidosis GAP metabolic acidosis? NONGAP metabolic acidosis?
answer
Normal Anion gap = 8-12 GAP: "MUDPILES" Methanol, Uremia, DKA, Propylene glycol, INH/Infection, Lactic acidosis, Ethanol/Ethylene glycol, Salicylates NONGAP: "FUSEDCARS" Fistula, Uretero-enterostomy, Saline admin, Endocrine (hyperPTH), Diarrhea, Carbonic anhydrase inhibitors, Ammonium chloride, RTA, Spirinolactone There are three major etiologies of nongap acidosis: 1) Chloride containing solutions (NS or TPN) 2) Increased HCO3 loss (diarrhea, ostomy output, GI fistula) 3) Decreased acid excretion (ie hypoaldosteronism, ARF/CRF
question
Afferent vs Efferent
answer
Afferent is the nerve arriving to the spinal cord, efferent is the nerve exiting the spinal cord. Afferent ARRIVES, Efferent EXITS.
question
In a patient with muscular dystrophy who receives succinylcholine, why would they have hyperkalemic cardiac arrest?
answer
Not because of extrajunctional receptors but because of rhabdomyolysis. Patients with Duchenne or Becker would present with muscle weakness, pseudohypertrophy of calves, and elevated CK. They might also have dilated CMP. They are not more susceptible to MH.
question
Tumescent Liposuction dose/kg of lidocaine?
answer
35-55mg/kg is allowed because the majority is aspirated during the procedure, because it is not absorbed, and because it is given with Epi. Concentrations peak at 12 hours. 0.05% Lidocaine with Epi 1:1,000,000
question
ABGs are generally run at ___ degrees C. To correct for colder patients
answer
37 degrees C For each degree Celcius temperature decrease, the pH of the blood increases by 0.02. For example, a sample on a patient who was at 32 degrees came back with a pH of 7.20, what would the corrected pH be? 7.30
question
Reflexes: What is the Bezold Jarisch Reflex? What is the Bainbridge Reflex? What is the normal Baroreceptor Reflex?
answer
Bezold Jarisch - hypotension sensed in the LV leads to bradycardia and further hypotension Bainbridge - paridoxical tachycardia in response to fluid bolus Baroreceptor - stretch receptors in the carotid results in decreased HR and decreased BP
question
Risk factors for Post Dural Puncture Headaches (PDPH)?
answer
Age ; 40 Prior PDPH BMI ; 30 Hx of Air Travel Multiple Attempts The use of Cutting Needles (Quincke, Pitkin, Rovenstine) Puncture with a large bore needle
question
Inhaled Nitric Oxide can cause what?
answer
Methemoglobinemia and a left shift on the oxygen disassociation curve. It will improve VQ mismatch by decreasing PVR, thus increased PaO2 NO is endogenously secreted by the vascular epithelium to inhibit platelet aggregation.
question
ECT Autonomic Effects?
answer
Initially following seizure activity, there is an increase in parasympathetic stimulation which can manifest as increased secretions, bradicardia and sometimes transient asystole. The increased parasympathetic stimulation is quickly followed by an increase in sympathetic stimulation which will present as hypertension and tachycardia. You can sometimes see ST changes which is usually transient.
question
B2 agonism effect on: Glucose? Potassium?
answer
B2 agonists causes HYPERglycemia and HYPOkalemia. It also is used off label as a tocolytic/uterine relaxation. "B SWEET" Also, remember that B agonists are a treatment for hyperkalemia
question
Goals for Aortic and Mitral Insufficiency?
answer
Decrease afterload Augment contractility Avoid bradycardia - any medication that would decrease heart rate is not recommended because it will allow for more time for regurgitant flow. A mnemonic for Aortic Insufficiency and Mitral Insufficiency is "fast, full and forward" - avoid bradycardia, optimize preload, and minimizing afterload. Can use nitroprusside to decrease afterload
question
Goals for Aortic Stenosis?
answer
Avoid hypotension Maintain sinus rhythm avoiding both bradycardia and tachycardia Optimize intraventricular filling Avoid sudden increases or decrases in SVR
question
Goals for MV Stenosis?
answer
Avoid sinus tachycardia or Afib with RVR Avoid marked increases in CVP Avoid drug induced decreases in systemic vascular resistance Avoid hypoxemia or hypoventilation which might precipitate increases to PVR and eventual right sided failure
question
Goals for HOCM?
answer
1) Ensuring adequate preload and CO, 2) Reduce contractility - halothane used in the past but no longer because of arrhythmogenicity 3) Maintain SVR Etomidate is a good choice for induction because of its ability to maintain SVR.
question
Neonatal Fluid management - Things to Keep in Mind
answer
1) Neonates have reduced GFR and are prone to fluid overload because their nephrons are immature and underdeveloped. 2) Neonates are sodium wasters because they do not respond as strongly to aldosterone. 3) TBW is highest in preterms and lowest in adults. 4) A high body surface area:body weight ratio pre disposes neonates to increased evaporative losses. 5) Immature sympathetic nervous system and baroreceptors are the reason for a reduced response to low BP 6) Infants and neonates have a higher volume of distribution. 7) Infants and neonates have a LOW plasma protein content which means that they have increased plasma concentration of unbound/active molecules/hormones/medications. 8) Enzyme immaturity leads to slower metabolism but remember that they have a higher volume of distribution
question
The best medicine to improve CPP?
answer
Vasopressin is actually better at improving CPP compared to phenylephrine or NE. Not only does vasopressin increase MAPs but it also reduces ICP. CPP = MAP - ICP
question
Coronary Perfusion pressure = ?
answer
Coronary Perfusion Pressure = Aortic DBP - LVEDP
question
What factors increase in pregnancy?
answer
1, 7-10, 12 and vwf 11, 13 and at3 decrease
question
Substrates that are metabolized by butrylcholinesterase
answer
Heroin Cocaine Other ester local anesthetics ASA Mivacurium Succinylcholine **Remifentanil and esmolol are not metabolized by butylcholinesterase
question
Malignant Hyperthermia Pathophys? Earliest signs? Triggers? Associated with? Confirmation test?
answer
Caused by mutation in the ryanodine receptor (normally responsible for release of calcium into muscle cell) that causes prolonged release of calcium. Earliest signs are masseter muscle rigidity, tachycardia and hypercarbia. Hyperthermia and myoglobinuria is a late sign. Triggers: Volatile anesthetics only (NOT nitrous) and succinylcholine Clear associations with Central Core Disease, Multi-minicore myopathy and King Denborough syndrome. Confirmation test: Muscle biopsy - caffeine-halothane contracture test (10-20% false positive rate but near 0% false negative rate - it is 100% sensitive)
question
Malignant Hyperthermia Intraoperative management?
answer
Call for help 1) Stop triggering agent 2) 100% O2 - high flows 3) Dantrolene 2.5mg/kg - give early and ok to give rapidly 4) Change circuit tubing, soda lime 5) Get Arterial access for lab draws - ABG q5 mins, check BMP and clotting studies 6) Bicarbonate 1-2mEq/kg 7) Treat symptoms - cool if necessary, antiarrhythmics (procainamide), diuretics (furosemide 1mg/kg or mannitol 0.25mg/kg) Dantrolene + CCBs are contraindicated because myocardial depression has been demonstrated in animal studies
question
What is the earliest most sensitive sign for MH? What is the earliest most specific sign for MH?
answer
Earliest most sensitive: Hypercarbia Earliest most specific: Muscle rigidity
question
Known Triggers for post op OSA in Pediatric Population
answer
Severe OSA on Polysomnography Age ; 3 years old Hx of prematurity Neuromuscular disorders URI in the past 4 weeks Nasal pathology Systemic HTN Obstruction during Inhaled Induction Hx of Snoring, Frequent awakenings, Daytime restlessness Cor Pulmonale
question
Do hyper-/hypothyroidism affect MAC?
answer
NO
question
Pheochromocytoma Management? What to expect in the PACU?
answer
Alpha blockade first followed by beta blockade. If you do beta blockade first, you will get unopposed alpha causing hypertension. Treat first with phenoxybenzamine (irreversable alpha blocker) or phentolamine or prazosin (alpha 1 blocker). Combination of phenoxybenzamine, prazosin, beta blocker, ACEi, CCBs, and magnesium sulfate to attain HD stability. In the PACU, they will be hypotensive, sedated, hypertensive (if part of the tumor persists), and hypoglycemic. Not hyperglycemic.
question
Smoking Cessation
answer
12-24 hours to decrease CO levels and decrease sympathetic outflow caused by nicotine (t1/2 of 1-2hrs) 1-2 weeks to decrease sputum production, normalization of mucociliary function 3-4 weeks to decrease wound healing complications ;4 weeks to decrease respiratory complications (ie bronchospasm or pneumonia)
question
Hepatic Blood Flow is derived from?
answer
The portal vein provides about 75% of total hepatic flow and the hepatic artery only provides about 25%.
question
In obesity, what changes would you see in lung mechanics?
answer
Decreased FRC (due to decreased ERV) Decreased VC Decreased TLC RV and closing capacity are unchanged FEV 1 and FVC are usually normal.
question
Which lung volumes remain constant from infancy to adulthood?
answer
FRC (30mL/kg) and Tidal volume (7mL/kg)
question
Pierre Robin vs Apert Syndrome vs Klippel-Feil syndrome vs Beckwith-Wiedeman syndrome vs Hurler syndrome
answer
Pierre Robin: Micrognathia/mandibular hypoplasia, glossoptosis and cleft palate Apert: MAXillary hypoplasia and choanal stenosis = mouth breathers but not a difficult airway Klippel-Feil: limited neck extension due to fused cervical vertibrae Beckwith-Wiedeman: macroglossia; associated with CHD and omphalocele Hurler: airway difficulty due to infiltration of mucopolysaccharide into pharyngeal and laryngeal soft tissue
question
Tet Spell Management
answer
Knee-chest position (increases SVR) Phenylephrine (increases SVR) Fluid bolus (increases preload) Morphine (decrease agitation and decrease RVOT obstruction) B blocker (decreases RVOT obstruction)
question
Uptake of volatile agents is faster in infants why?
answer
Because they have a higher alveolar ventilation:FRC ratio. Infants also have a larger proportion of vessel rich tissues such as brain, liver and heart which also contributes to a more rapid uptake. This explains why an inhaled induction is faster in infants, compared to adults.
question
Umbilical Vein Blood Gas Umbilical Artery Blood Gas
answer
7.35 / 40 / 30 7.20-7.30 / 50-55 / 18-25
question
Estimated Allowable Blood Loss equation?
answer
EABL = EBV (Hcti-Hctf/Hcti) EBV = 80mL/kg infants, 70mL/kg adults
question
Risk factors for developing Preeclampsia?
answer
Advanced maternal age African Americans Nulliparity Family history of Preeclampsia Placental Abruption Obesity Diabetes Renal disease Vascular disease HTN NOT CIGARETTES or TABACCO
question
How does magnesium affect the NMB and the NM junction?
answer
It inhibits the release of ACh at the NMJ It decreases sensitivity at the NMJ to ACh It depresses the excitability of the muscle fiber membrane It increases potency and duration of NMDBs
question
Meds that do/do not cross the placenta
answer
Do not: Heparin, glycopyrrolate, muscle relaxants (minimal placental transfer) Do: Atropine, scopalamine, thiopental (highly lipid soluble), opiates (morphine the most, fentanyl the least), volatile anesthetics, local anesthetics (depend on pKA, maternal/fetal pH, degree of protein binding) - mainly lidocaine will cross, bupi and ropi have high protein binding and chlorprocaine is metabolized quickly.
question
P50 of neonates? P50 of 10 month old? P50 of adult Hgb?
answer
neonate - 20mmHg, left shift because of decreased interaction between HbF and 2,3 DPG 10mo - 30mmHg, the P50 decreases to adult values at about 10-12yo adult - 27mmHg
question
Beginning at what week gestation should you start to implement left uterine displacement? When can you start monitoring fetal heart tones?
answer
18-20 weeks for both
question
Up to what month can you use NSAIDs during pregnancy?
answer
Up to the end of the 2nd trimester
question
Avoid elective surgery when during pregnancy? When is the optimal time for elective surgery?
answer
Avoid it in the 1st trimester because of organogenesis (occurs between days 30-70). The second trimester is the optimal time to perform surgery
question
t-test vs ANOVA?
answer
t-test is used for comparing continuous outcomes in 2 groups. ANOVA is used to compare more than 2 groups
question
What is the leading cause of mortality in pregnant women?
answer
Pulmonary embolism - due to an increase in factor I, 7-10, 12 and vWF and a decrease in protein S (mainly hypercoagulable state is due to increased VII and fibrinogen) Risk of venous thromboembolism in pregnancy increases with the following additional risk factors: obesity, smoking, multiple gestations, advanced maternal age, increased parity, cesarean section, as well as the presence of a concomitant thrombophila.
question
Preservatives in LA solutions possible toxicity? Sulfites? EDTA? Methylparabens?
answer
Sulfites - added to 2-chloroprocaine is associated with arachnoiditis or anaphylaxis. Pts who have had accidental large intrathecal volume injection can develop bilateral lower extremity paralysis EDTA - added as a chelating agent that can cause back pain at the injection site Methylparaben - bacteriostatic agent that has a chemical structure similar to PABA and can cause anaphylaxis.
question
Absorption of LA from greatest to least?
answer
IV, Tracheal, Intercostal, Caudal, Epidural, Brachial plexus, Sciatic, SubQ "IT ICE BS"
question
Lidocaine max dose?
answer
4-5mg/kg without epi 7mg/kg with epi
question
Bupivicaine/Ropivicaine max dose?
answer
3mg/kg
question
Cocaine mechanism of action?
answer
1) Na channel blocker 2) NE reuptake inhibitor 3) Stimulates presynaptic NE + dopamine release Metabolized by butrylcholinesterase
question
Interscalene Block What part of the brachial plexus? Surgical applications? What side effects or complications?
answer
Upper and middle trunks mainly, the lower trunk is often spared Blocks the entire brachial plexus with occasional ulnar sparing Good for shoulder or proximal - mid humerus surgery Phrenic nerve paresis in 100% of patients, unsuitable for COPDs or elderly who cannot tolerate 25% reduction in pulmonary function
question
Supraclavicular Block What part of the brachial plexus? Surgical applications? What side effects or complications?
answer
Trunks/divisions Blocks the Radial, ulnar, median, musculocutaneous and axillary nerves so good for surgeries of the mid humerus, elbow, forearm and hands Risk of PTX requires caution. Phrenic nerve paresis in 30%
question
Infraclavicular Block
answer
Blocks at the level of the cords
question
Axillary Block What part of the brachial plexus? Surgical applications? What side effects or complications?
answer
Terminal branches/peripheral nerves Blocks the radial, ulnar, median and musculocutaneous (unreliably blocked) Good for operations of the forearm and hand Supplimental intercostobrachial nerve block needed for TNQT pain
question
The intercostobrachial nerve is responsible for what nerve distribution?
answer
The medial surface of the arm in the axilla
question
What formation of Bupivicaine is the most cardiotoxic? R+, S- or Racemic?
answer
R+ isomer is 7 times more potent than S- Levobupivicaine is the same as S-
question
Why do you get decreased HR in a high neuraxial block?
answer
1) you could have blockage of the cardioaccelerator fibers (T1-T4) 2) unoposed vagal tone from high sympathectomy 3) Reverse bainbridge reflex/Bezold Jarisch reflex (decresaed HR due to decreased intracardiac stretch receptors)
question
What effects on lung mechanics do you get from neuraxial anesthesia?
answer
TV is not impaired as long as C3-C5 are not blocked VC is decreased due to decreased ERV from abdominal muscle weakness Apnea during spinal is due to medullary ischemia from hypotension rather than motor block of the phrenic
question
In cases of MRI equipment malfunction, the liquid helium (which is used to cool the superconducting materials) can boil off in what is known as a _____. If the helium does not escape through the safety valve, the large amount of helium can pose a risk for_____.
answer
Quench Asphyxiation to personal and patients due to displacement of O2 in the room.
question
WPW - what are the two types of tachyarrhythmia? What are the pathways of the two types? What are the treatments of the two types?
answer
AVNRT is the most common tachyarrhythmia seen in pts with WPW. AVNRT is classified as either ORTHODROMIC or ANTIDROMIC. Orthodromic is more common and has a narrow QRS - the impulse is conducted from atrium to AV node to His to Purkinje and then return from ventricle to atria using an accessory pathway. Treatment should begin with vagal maneuver. If unsuccessful give B blockers, verapamil, adenosine or amio. Antidromic has a wide QRS - impulse is conducted from the atrium to the ventricle through the accessory pathway and returns from the ventricles to the atria via the normal AV node. Treatment with PROCAINAMIDE. Meds that slow AV node conduction such as adenosine, CCBs, B blockers, lidocaine and digoxin can actually increase conduction through the accessory pathway and are contraindicated. Cardiovert if unstable
question
Treatment of Long QT syndrome
answer
B-blockers, potassium supplementation, Mexilitine, ICD placement
question
Neurolysis for cancer pain: what are the two methods?
answer
1) Alcohol - burns on injection 2) Phenol - does not burn
question
Celiac plexus block is used for what?
answer
Cancer of organs from the distal esophagus to the transverse colon
question
Superior Hypogastric Plexus is used for what?
answer
Bladder ca, cervical Ca, prostate Ca
question
What is the caudal block dose in infants?
answer
0.5-1mL/kg of 0.25% bupi or ropi with or without epi 0.5mL/kg covers sacral dermatomes 1mL/kg covers low thoracic dermatomes 1.25mL/kg covers mid thoracic dermatomes
question
Signs of Uterine rupture?
answer
Atypical abdominal pain, shoulder pain, vaginal bleeding, uterine tenderness, hypotension, tachycardia, shock.
question
What type of nerve fibers are the most susceptible to LA blockade?
answer
Small myelinated B fibers
question
What is the anesthetic site of action for lipophilic opioid epidural infusions? Lipophilic epidural bolus?
answer
Opiate epidural infusions site of action = systemic Opiate epidural bolus site of action = spinal
question
Neuraxial hydrophilic opioids move cephalad or caudad?
answer
Hydrophilic opioids (ie morphine dilaudid) meds move more cephalad compared to fentanyl
question
Lidocaine Bier Block dose?
answer
3mg/kg of 0.5% Lidocaine will provide anesthesia for up to 90 mins
question
Most common cause of transfusion related mortality?
answer
TRALI - caused by recipient antibodies to donor HLA causing an influx of neutrophils into the lungs with subsequent activation causing inflammatory response and increased pulmonary microvascular permeability
question
Hemophilia A is a deficiency in ___? Hemophilia B is a deficiency in ___?
answer
A = factor eight B = factor nine A8, B9
question
In regards to local anesthetics: Lipid solubility is the determinant of what? pKA is a determinant of what? Protein binding is a determinant of what?
answer
Lipid solubility is the primary determinant of intrinsic local anesthetic potency (increased lipid solubility indicates increased potency) Speed of onset is related to the pKa (lower pKA indicates shorter onset of action) Protein binding is implicated in the duration of action (high protein binding indicates longer duration of action)
question
CEA Normal regional cerebral blood flow? Ischemia seen with what cerebral blood flow? EEG changes seen with what cerebral blood flow? Cerebral tissue death is seen with what CBF?
answer
Normal 50mL/min/100g Ischemia 20mL/min/100g EEG changes 15-20mL/min/100g Cell death 10mL/min/100g 16 lead EEG is the gold standard
question
Paired t-test Unpaired t-test Chi-Square Fisher-test
answer
Paired t-test: compare study subjects means at 2 different times Unpaired t-test: compares means of two different subjects Fisher test: compares 2 proportions Chi-square: compares ;2 proportions
question
SVR formula? PVR formula?
answer
SVR = 80 * (MAP-CVP) / CO PVR = 80 * (mPAP - PCWP) / CO
question
Abdominal compartment syndrome: When do you see it? What bladder pressures would you see?
answer
- Can be the result of major abdominal surgery or following massive fluid resuscitation for massive trauma or burns. This is because of massive intra-abdominal edema secondary to shock induced inflammatory mediators or surgical manipulation - ;20-25mmHg
question
Alpha stat vs pH stat
answer
During pH stat the patient's pH is maintained my managing the pH at the current temperature. ***pH stat infuses extra CO2 into the blood causing improved CBF*** During alpha stat the patient's pH management is not temperature corrected. Just remember that in a cold patient, the patient's PaCO2 will be LOWER than what is seen on the alpha stat.
question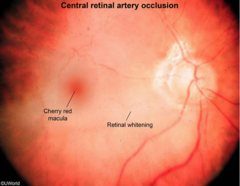
In the prone head/neck case, patient wakes up with unilateral blindness, proptosis and retinal exam shows a cherry red spot, what is the diagnosis?
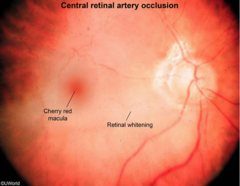
answer
Central retinal artery occlusion "Prone case with pressure on the eyeball" This is different from Posterior/Anterior IOP in that the optic disc is normal.
question
Extracorporeal Membrane Oxygenation VA ECMO VV ECMO AV ECMO
answer
VA ECMO = can provide near full support of heart and lungs VV ECMO = gas exchange of 80% of cardiac output, does not provide any cardiovascular support AV ECMO = gas exchange is driven by arterial flow through extracorporeal membrane
question
Vaporizer output at alitutde
answer
Modern conventional vaporizers are temperature compensated variable bypass vaporizers. This means that these vaporizers divert a certain amount of FGF through the liquid volatile anesthetic. Therefore the amount of volatile exiting the vaporizer is subject to change based on the atmospheric pressure. They automatically compensate for changes in altitude. However, the desflurane vaporizer is different in that it is heated to 39 degrees C. No FGF flows through a desflurane sump, rather a certain volume of desflurane is released into the circuit based on the percentage set on the control dial. Therefore, the output of desflurane from the anesthesia circuit will be the SAME weather at sea or at altitude. An example of a question: If a machine is set at 6% in two operating rooms. One machine is set at sea level (Patm 760mmHg) and the other is set at 8000ft above sea level (Patm 570mmHg), what would be the expected anesthetic depth of the patient at 8000 feet? Deeper? Lighter? The same? Answer: Relatively lighter because the partial pressure of desflurane in the sea level pt would be 760 x 0.06 = 45.6mmHg and the partial pressure of the desflurane in the 8000ft pt would be 570 x 0.06 = 34.2mmHg. So the 8000ft pt would be getting less desflurane.
question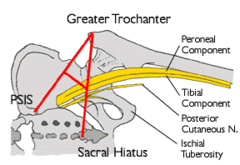
For a sciatic nerve block, what three anatomical landmarks are required?
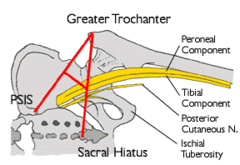
answer
1) Greater trochanter of the femur 2) PSIS 3) Sacral Hiatus
question
What is the most common congenital cardiac anomaly?
answer
Bicuspid aortic valve
question
Cirrhosis: increased or decreased? Intravascular volume? ECF? Total body water? Intracellular volume? Cardiac output? SVR? SvO2?
answer
Intravascular volume decreased ECF increased Total body water increased Intracellular volume unchanged CO increased - cirrhosis causes a hyperdynamic state SVR decreased SvO2 increased
question
Amniotic Fluid Embolism risk factors?
answer
Multiparity Placenta previa Abruptio placenta Uterine rupture Cervical laceration
question
GI changes in 3rd trimester: increased or decreased? - Gastric pH? - Gastric emptying? - Gastric volume? - LES tone
answer
Gastric pH down due to increased gastrin Gastric emptying decreases in active labor Gastric volume up due to increased gastrin LES tone decreases due to progestin & upward displacement of the stomach
question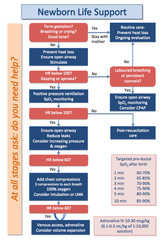
Neonatal resuscitation
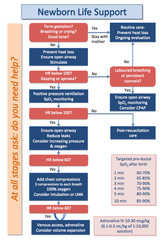
answer
Not breathing or crying? Dry, warm, stimulate, clear airway secretions HR <100, gasping or apneic? PPV HR < 60 after 30 seconds of PPV? Continue PPV - intubate, start chest compressions HR still < 60 after 60 secs? GIVE EPI 10-30mcg/kg IV, IT, or via umbilical artery For meconium: If adequate RR, HR and activity, do NOT intubate, just suction If not adequate HR, irregular RR, poor tone - intubate and suction
question
Conditions associated with Meconium
answer
Postmaturity (>42 weeks) Uteroplacental insufficiency IUGR Maternal conditions (ie HTN, Placenta previa, PHTN, Abruptio placenta)
question
Arrhythmia associated with SAH? Also, in the setting of SAH an echo might show what?
answer
QT prolongation Global LV hypokinesis
question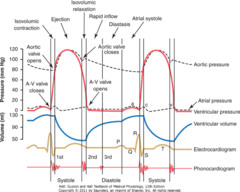
What period of the cardiac cycle is most shortened in sinus tachycadia? When does most of the LV filling occur?
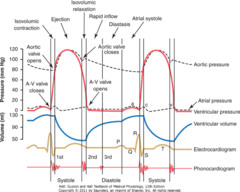
answer
Diastasis (slow filling prior to atrial contraction, the y descent) Early diastole upon opening of the mitral valve. Atrial systole is responsible for 15% of LV filling
question
How does hetastarch affect anticoagulation?
answer
It binds to Factor VIII and vWF.
question
Aspirin Toxicity Laboratory findings? Clinical presentation? Treatment?
answer
First you will get direct stimulation of respiratory centers leading to respiratory alkalosis due to hyperventilation Metabolic acidosis to follow with an increased anion gap acidosis due to accumulation of lactate and excretion of bicarb (the kidneys have been wasting bicarb to compensate for resp alkalosis) Clinically, TINNITIS, tachypnea, hyperthermia, nausea/vomiting, seizures, CV collapse Tx: Activated charcoal within 1-2 hours, gastric lavage, bowel irrigation; sodium bicarb, HD, IV fluids
question
Congenital Long QT syndrome Medications to avoid? Acute management of torsades? Chronic management of LQTS?
answer
Avoid quinidines, procainamide, amio, macrolides, TCAs, SSRIs, ondansetron, methadone, volatile anesthetics Acute management: Magnesium, correct electrolytes Chronic management: B blocker and possibly a pacemaker
question
Separation anxiety does not begin until what age?
answer
6 months
question
What ETTs are the most flammable?
answer
PVC > silicone > red rubber
question
If a patient presents with MI and is found to have severe mitral regurg, what happened?
answer
There was likely posteromedial papillary muscle rupture due to RCA infarction.
question
Renal failure electrolytes?
answer
Elevated Electrolytes: potassium, phosphate, and magnesium Decreased Electrolytes: sodium, calcium Other Increases: urea, creatinine, uric acid, sulfate, phosphorus, lipids, cholesterol Other Decreases: albumin Acid/Base: anion gap metabolic acidosis
question
IE prophylaxis
answer
Previous IE Prosthetic valve CHD Heart transplant pts with valve issues
question
Most likely cause of intraop anaphylaxis?
answer
NMBDs
question
Elderly PFTs/Age related changes Closing pressure Residual volume Elasticity Gas exchange Dead space Chest wall rigidity Response to hypercapnia/hypoxia MAC CO Volume of distribution Hepatic function Recovery from anesthesia Levels of catecholamines Sensitivity to B receptor
answer
Closing pressure increased Residual volume increased Elasticity decreased Gas exchange decreased due to collapse of smaller airways and decreased alveolar surface area Dead space increased Chest wall rigidity increased Response to hypercapnia/hypoxia blunted MAC decreased CO decreased Volume of distribution increased Hepatic function decreased Recovery from anesthesia due to increased Vd and decreased hepatic function There is increased levels of catecholamines but decreased sensitivity to B receptor
question
Amiodarone Affect on SVR? Affect on HR?
answer
Decreases SVR and HR.
question
Tetanus toxin mechanism?
answer
Tetanus - travels retrograde up the motor neuron to the spinal cord where it enters the inhibitory interneurons and blocks the release of glycine.
question
Botulism toxin mechanism?
answer
Botulism inhibits the release of ACh at the NMJ by cleaving SNARE proteins - this stops the fusion of vesicular ACh.
question
FENa values
answer
1% = intrinsic (ATN or AIN) >4% = post renal
question
Acetazolamide
answer
Wastes sodium and HCO3 Cl reabsorption Clinical use: Acute mountain sickness (to compensate for resp alkalosis), glaucoma, urinary alkalinization Can in hyperchloremic metabolic acidosis
question
Etomidate/Ketamine affect on evoked potentials?
answer
Increased amplitude
question
Cyanide toxicity
answer
Hydroxocobalamin: combines with cyanide, forming cyanocobalamin (vitamin B12), which is renally excreted; few side effects, well-tolerated by critically ill Amyl nitrite: inhaled formulation, rapidly enters circulation generating methemoglobin which has higher affinity for CN than cytochrome oxidase Sodium Nitrite: slower onset, longer lasting nitrite, as above frees up cytochrome oxidase to resume aerobic metabolism Sodium Thiosulfate: regenerates sulfur-dependant rhodanese activity; this enzyme converts CN to thiocyanate, which is renally excreted; recommended co-administration with hydroxocobalamin or nitrites, especially in prolonged exposures
question
Fibromyalgia Diagnosis? Treatment?
answer
1) WPI score >7 OR SS scale score of >5 OR WPI 3-6 + SS scale of >9 2) Symptoms >3 months 3) No other explanation of pain Treatment CBT, sleep hygeine, strength training, meds - fda approved meds = Cymbalta, Lyrica or Savella
question
Facet arthropathy Nerve supply? Presentation?
answer
Each facet joint is innervated by the MEDIAL BRANCH of the posterior rami of the spinal nerves above and below Pain may be near midline and can radiate to gluteal region, thigh and knee. Worse with hyperextension and lateral rotation of spine Diagnostic medial branch block Tx Medial branch rhizotomy
question
Herniated Disc What level? Worse with? Better with? Associated symptoms? Initial tx?
answer
90% of the time it is L4-L5 or L5-S1. Occurs from flexion injuries or heavy lifting Aggravated by bending, lifting, sitting. Relieved by lying down +/- numbness or weakness or DTRs L4-L5 = weakness in dorsiflexion L5-S1 = weakness in plantar flexion Acute back pain tx: NSAIDs and APAP
question
Spinal stenosis
answer
Progressive narrowing of neural foramina and spinal canal. It is improved with flexion of the spine (squatting) and worsened with extension of the spine (walking up a hill)
question
Sciatic nerve is derived from what?
answer
L4-S3
question
Obesity
answer
Decrease in TLC Decrease in FRC (due to loss of ERV)
question
CHARGE syndrome
answer
Coloboma Heart defects Atresia, choanal Retardation of growth or development Genital abnormalities Ear abnormalities/deafness



