Epidemiology Lecture 7-8 – Confounding and Control of Confounding – Flashcards
Unlock all answers in this set
Unlock answersquestion
Confounding
answer
Addresses the interpretation of observational data - The presence of confounding weakens the case for a CAUSAL relationship between exposure and outcome - May be multiple confounding factors
question
Confounding Example
answer
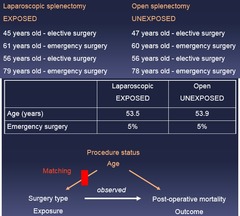
Laparoscopic splenectomy patients actually had lower post-op mortality compared to open splenectomy patients However, laparoscopic splenectomy patients also more likely to undergo elective surgery, which has lower mortality
question
Confounding: Example 1: Cohort study of laparoscopic versus open splenectomy Patients identified through international surgical registry Data abstracted from splenectomies 2008-2009 *Identified*: - 874 patients who underwent laparoscopic splenectomy - 907 patients who underwent open splenectomy Followed for all-cause mortality
answer
12/874 patients in laparoscopic group died within 30 days of surgery *Incidence 30 day post-op mortality* = 12/874 x 100% = *1.4%* 42 / 907 patients in open group died within 30 days of surgery *Incidence 30 day post-op mortality* = 42/907 x 100% = *4.6%* *Relative risk *= 1.4% / 4.6% = *0.3* comparing laparoscopic to open surgery *Laparoscopic splenectomy associated with 70% lower post-operative mortality compared to open splenectomy* Questions: 1.) Is laparoscopic splenectomy ASSOCIATED w/ lower postoperative mortality? YES: YES, lap splenectomy associated with 70% lower risk of post-op mortality 2.) *Does laparoscopic splenectomy REDUCE post-operative mortality?* Possible. Also possible that other characteristics linked with laparoscopic splenectomy responsible for observed lower post-operative mortality
question
Example 1: Does laparoscopic splenectomy REDUCE post-operative mortality? --> *Are there other characteristics possibly linking laparoscopic splenectomy w/observed lower post-operative mortality?*
*Are there other characteristics possibly linking laparoscopic splenectomy w/observed lower post-operative mortality?*" alt="Example 1: Does laparoscopic splenectomy REDUCE post-operative mortality? --> *Are there other characteristics possibly linking laparoscopic splenectomy w/observed lower post-operative mortality?*">
answer
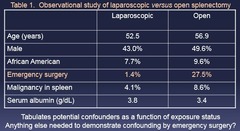
Observational vs Randomized studies: Observational Study: Laparoscopic surgery patients a little younger, less likely to have emergency surgery, less likely to have malignancy, have better nutrition *Randomization eliminates other characteristics by balancing them*
question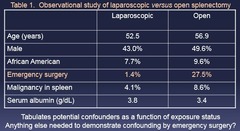
Example 1: Step 1
answer
*Tabulate Potential Confounders as a Function of Exposure Status* - Pts who had Emergency surgery were far more likely to undergo open surgery than lap
question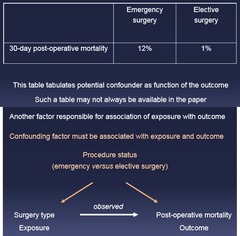
Example 1: Step 2
answer
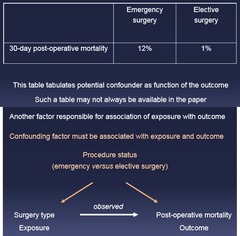
*Tabulate Potential Confounders as a Function of Outcome* - Pts who had emergency surgery had a higher rate of death (regardless of exposure) *Confounding factor must be associated with exposure AND outcome*
question
Confounding Factors: P Values

answer
*Irrelevant to whether or not a factor is confounding* - P-values make an inference to a larger population of similar pts
question
Association with with exposure AND outcome: Confounding vs Non-Confounding
answer
*Confounding*: factor leads to more exposure and more outcome *Non-Confounding*: exposure leads to factor, factor leads to outcome *Non-Confounding*: Factor not related to both exposure and outcome
question
Confounding Factors: Steps
answer
1.) Tabulate Potential Confounders as a Function of Exposure Status 2.) Tabulate Potential Confounders as a Function of Outcome 3.) Confounding factor must be associated with exposure AND outcome (Relative Risk) 4.)
question
Confounding Factor: Definition
answer
Confounding occurs when another factor is responsible for at least part of an association of exposure with outcome - A confounding factor is associated with both exposure and outcome and does not reside on the causal pathway of association
question
Classical evaluation of a confounder:
answer
1.) *Use the study data* to decide whether a potential confounding factor is associated with both the exposure and the outcome - Data for association of potential confounder with the study outcome may not be available in a paper - Sometimes have to guess --> 2.) *Use biologic plausibility* to decide whether a potential confounding factor resides on the causal pathway of association
question
Confounding Example 2: Oral erythromycin use and sudden cardiac death - Erythromycin used to treat bacterial upper respiratory infections - Prolongs cardiac repolarization - Associated with V-Tach in case reports *Study*: Large sample of Tennessee Medicaid population - Use versus non-use of erythromycin identified by pharmacy records - Sudden cardiac deaths adjudicated by record review What are the Questions?
answer
1.) *Is current erythromycin use ASSOCIATED with cardiac death?* Yes, relative risk = 2.01 compared to non-users 2.) *Is current erythromycin use a CAUSE of cardiac death?* - If yes, may considering new warning label for erythromycin Current erythromycin users compared to non users: - A little bit older - More likely to take other medications - More likely to have previous encounters for CV disease
question
Confounding Example 2: Current erythromycin users compared to non users: - A little bit older - More likely to take other medications - More likely to have previous encounters for CV disease *Is there any pattern to the confounding factors in this case?*
answer
These are all indications for the use of Erythromycin
question
Confounding by Indication
answer
A special case of confounding in which indications for medication or procedure confound the association - Confounding-by-indication occurs when the indication for a medication or procedure specifically confounds the association - The presence of confounding weakens the case for causality *Solution* = Compare with another drug or procedure w/ similar indication
question
Example 2: Confounding by Indication Solution

answer
Incidence rate erythromycin users = 10/5,305 = 1.89 per 1,000 person-yrs Incidence in amoxi users = 8/6,846 = 1.17 per 1,000 person-yrs Relative Tisk = 1.89/1.17 = 1.61 comparing current erythromycin use to current of amoxicillin use ==> Current erythromycin users associated w/ 61% greater risk of death compared to amoxicillin use *Strengthens case for causal association of erythromycin*
question
Evaluation of Different Confounding Factors
answer
Classical evaluation of a confounder: *Asses using Study Data if*: - Associated with the exposure - Associated with the outcome *Asses using own knowledge/biological plausibility if*: - Not on the causal pathway
question
Methods to control for confounding
answer
- Randomization - Restriction - Stratification - Matching - Regression
question
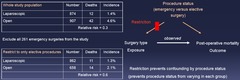
Control Example 1: Cohort study of laparoscopic versus open splenectomy 30 day post-operative mortality Relative risk = 0.3 comparing laparoscopic to open splenectomy Concerned that these results might be confounded by other factors Procedure status (emergency vs elective surgery) meets classic definition of a confounder: Associated w/ exposure and outcome and not on the causal pathway *What can we DO about this?*
answer
1.) *Randomization* 2.) *Restriction* prevents confounding by procedure status; However: - Lose 261 study participants - reduces study power - Study results now apply to only elective splenectomies - May still be confounding by other characteristics 3.) *Stratification* 4.) *Matching* 5.) *Regression* - Modern approach for handling multiple confounders; Topic of future lecture
question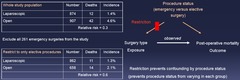
Restriction
answer
Prevents confounding by procedure status (prevents procedure status from varying in each group)
question
Advantages and Limitations of Restriction to control for confounding
answer
*Advantages*: - Simple and easy to understand - Can control for one or possibly a few major confounders *Limitations*: - Lose study subjects and study power - Reduced applicability of study findings - Difficult to deal with multiple confounders
question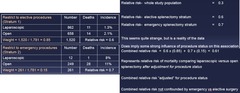
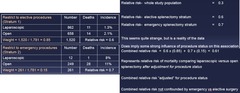
Stratification Example 1
answer
1.) Separate into 2 groups (emergency vs elective) = *Stratum* - w/in each stratum, procedure status is not confounding 2.) Compare Relative Risk of each group - example: implies that there was some confounding since both RR's are closer to 1 3.) Combine the results to calculate and overall RR - weight the RR by % of the study population in each group - e.g. (RR1*weight1) +(RR2*weight2)
question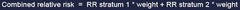
Combined Relative Risk Equation
answer
Combined relative risk = RR stratum 1 * weight + RR stratum 2 * weight
question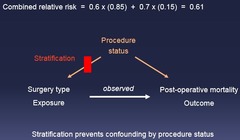
Stratification
answer
Prevents confounding by procedure status 1.) Separate into Stratum based on factor 2.) Compare Relative Risk of each group 3.) Combine the results to calculate and overall RR Combined relative risk = RR stratum 1 * weight + RR stratum 2 * weight
question
Stratification Results Example 1
answer
Relative risk Unadjusted = 0.3 Relative risk Adjusted for procedure status = 0.61 (stratification) "After adjustment for procedure status laparoscopic splenectomy associated with 39% lower risk of death compared to open splenectomy" *Could this association still be confounded by other factors?* YES
question
Stratification for More than One Factor

answer
Divide into more stratum, works best with a really large study group then weight and combine RR across all strata
question
Advantages and Limitations of Stratification to control for confounding
answer
*Advantages*: - Uses all of the study data - Works well for naturally binary confounding factors (procedure status, gender, past history of diabetes) *Limitations*: - Difficult to deal with multiple confounders at the same time - "Residual confounding" for continuous variables (age, serum albumin level)
question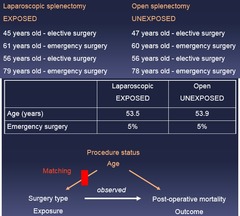
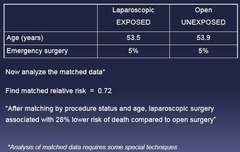
Matching: Example 1 Step 1
answer
For each study patient undergoing laparoscopic splenectomy, find one or more similar pts undergoing open splenectomy with: - Same procedure status (elective vs emergency surgery) - Similar age (for example, within ±3 years
question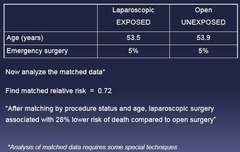
Matching: Example 1 Step 2
answer
Now analyze the matched data Find matched relative risk = 0.72 "After matching by procedure status and age, laparoscopic surgery associated with 28% lower risk of death compared to open surgery"
question
Matching
answer
Breaks association between confounder and exposure - Varies by Study Design 1.) For each patient, match with another pt according to confounders 2.) Find Matched Relative Risk
question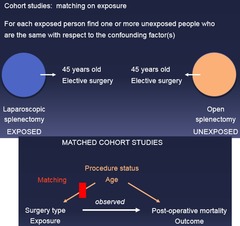
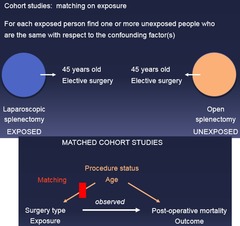
Matching Cohort
answer
*Matching on exposure* - For each exposed person find one or more unexposed people who are the same with respect to the confounding factor(s)
question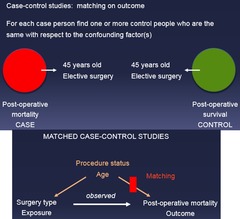
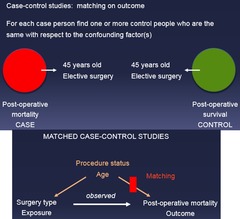
Matching Case Control Study
answer
*Matching on outcome* (case and control) - For each case person find one or more control people who are the same with respect to the confounding factor(s)
question
Advantages and Limitations of Matching to control for confounding
answer
*Advantages*: - Easy to understand - Possible to deal with multiple confounders *Limitations*: - Must be performed in the Design - before the analysis - May be difficult to control for multiple confounders - Alters generalizibility to matched population
question
Interpretation of Adjusted Results Example 1: Relative risk 30 day mortality comparing laparoscopic to open surgery: - 0.30 unadjusted - 0.61 adjusted for procedure status (stratification method) *What do these findings imply about procedure status as a confounder?*
answer
Change to adjusted RR implies that the factor that was adjusted for was a confounder *Alternative definition of a confounding factor = "Meaningful" change in association after adjustment for that factor*
question
Alternative definition of a confounding factor
answer
"Meaningful" change in association after adjustment for that factor - No consensus on "meaningful" - 5%, 10%, 20% change proposed - No statistical test for "meaningful" either *Can use 10% for this class*
question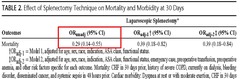
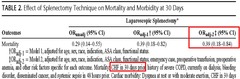
Example: Interpretation of the unadjusted odds ratios
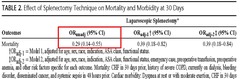
answer
Laparoscopic surgery associated with 71% lower unadjusted odds of post-operative mortality compared with open splenectomy BUT Post-operative mortality after splenectomy relatively uncommon (Rare) sooo.... - Laparoscopic surgery associated with ≈71% lower unadjusted risk of post-operative mortality compared with open splenectomy
question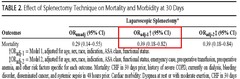
Example: Interpretation of the adjusted odds ratios1
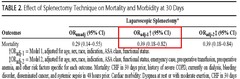
answer
Laparoscopic surgery associated with 61% lower risk of post-operative mortality compared with open splenectomy after adjustment for age, sex, race, indication, ASA class, functional status
question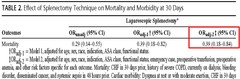
Example: Interpretation of the adjusted odds ratios2
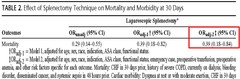
answer
After further adjustment for all the rest of that stuff: laparoscopic surgery associated with 61% lower risk of post-operative mortality compared with open splenectomy
question
Example Odds Ratios: 1.) Laparoscopic surgery associated with ≈71% lower unadjusted risk of post-operative mortality compared with open splenectomy 2.) Laparoscopic surgery associated with 61% lower risk of post-operative mortality compared with open splenectomy after adjustment for age, sex, race, indication, ASA class, functional status 3.) After further adjustment for all the rest of that stuff: laparoscopic surgery associated with 61% lower risk of post-operative mortality compared with open splenectomy *What do these Findings Imply?*
answer
These findings imply Some degree of confounding by age, sex, race, indication, ASA class, and/or functional status - No further confounding by a large number of other factors
question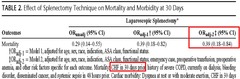
Example: Two final important considerations when evaluating confounding #1
answer
Model includes adjustment for heart failure: Back to the methods section to check how heart failure was measured - Heart failure assessed using diagnosis codes - Diagnosis codes have poor accuracy for capturing heart failure *What happens when you adjust for a poorly measured confounding factor?* NOTHING = "*Imprecise ascertainment of comorbidity*" - An important consideration when evaluating confounding
question
Imprecise ascertainment of comorbidity
answer
Just bc you adjusted for something doesn't mean you actually adjusted for "it" you adjusted for something that represents "it" - and it may respresent it poorly - if you are worried results are still confounded after adjustments, look at how the factor was measured
question
Example: Two final important considerations when evaluating confounding #2: Cohort study of laparoscopic versus open splenectomy Relative risk 30 day mortality comparing laparoscopic to open surgery - 0.30 unadjusted - 0.39 adjusted for age, sex, race, indication, functional status - 0.80 adds adjustment for intra-operative blood loss --> where does that fit? It is a Mechanism, not a confounder, so why are they adjusting it and how do we interpret it?
where does that fit? It is a Mechanism, not a confounder, so why are they adjusting it and how do we interpret it?" alt="Example: Two final important considerations when evaluating confounding #2: Cohort study of laparoscopic versus open splenectomy Relative risk 30 day mortality comparing laparoscopic to open surgery - 0.30 unadjusted - 0.39 adjusted for age, sex, race, indication, functional status - 0.80 adds adjustment for intra-operative blood loss --> where does that fit? It is a Mechanism, not a confounder, so why are they adjusting it and how do we interpret it?">
answer
Part of the lower post-operative mortality observed for laparoscopic splenectomy is likely mediated via less intra-operative bleeding *Over-adjustment* - An important consideration when evaluating confounding
question
Over-adjustment
answer
Studies often over adjust by adjusting for things that are part of the causal pathway (mechanisms) - relative risks become falsely LOW - reporting an association that is falsely low, "shoot yourself in the foot"
question
Control of Confounding: Summary
answer
- Procedures to control for confounding include randomization, restriction, stratification, matching, and regression - Break bonds between confounder and exposure or outcome - Alternative definition of confounding factor is a "meaningful" change in the association after adjustment for that factor - Two important considerations when evaluating confounding include imprecise ascertainment of co-morbidity and over adjustment



