Chapter 17: Breasts and Regional Lymphatics – Flashcards
Unlock all answers in this set
Unlock answersquestion
Non pregnant Breasts
answer
change with ebb & flow of hormones during menstrual cycle. Modularity increases --> mid cycle up to menstruation. 3-4 days before menstruation --- breasts full, tight, heavy, or sore. breasts smallest --- on day 4-7 go cycle.
question
Pregnant women
answer
*breast change in 2nd month --> early sign of pregnancy. *pregnancy stims expansion of ductal system & fatty tissue & development of true secretory alveoli. *breasts enlarge & more nodular. *nipples-- larger, darker. tubercules more prominent (The brown color fades after lactation, but the areolae never return to the original color.) A venous pattern is prominent over the skin surface
question
Colostrum
answer
starts after 4th month. -thick, yellow fluid. -precursor to milk. -same amt. of protein & lactose, but little fat. -produced for 1st few days after delivery. -antibody rich--> protect from infection.
question
Lactation "milk production"
answer
starts 1-3 days after delivery. white --> from fat & calcium caseinate.
question
Aging Women
answer
*after menopause: -ovary secretion of estrogen & progesterone decreases --> causes breast gland tissue to atrophy. -replaced with fibrous tissue. -fat atrophies -->start in Middle years & marked @ 70s & 80s. **breast drooping accentuated by Kyphosis in some older women. -decrease breast size & elastic --> droop & sag. flat & flabby -The decreased breast size makes inner structures more prominent. -A breast lump may have been present for years but is suddenly palpable. -around the nipple the lactiferous ducts are more palpable and feel firm and stringy because of fibrosis and calcification. -The axillary hair decreases.
question
Male Breast
answer
- is a rudimentary structure consisting of a thin disk of undeveloped tissue underlying the nipple. -areola is well developed, but nipple is small. ****During adolescence it is common for the breast tissue to enlarge temporarily, producing gynecomastia. - temporary, but reassurance is necessary for the adolescent male, whose attention is riveted on his body image. ***Gynecomastia may reappear in the aging male ---> testosterone deficiency.
question
Culture & Genetics
answer
*puberty influence: genetics & environment. **African-American before whites. -puberty: 1-1.5 yrs -Menstruation: 8.5 months earlier Breast development: -8.87 y/o = black -10 y/o = white Menses (start): -12.16 y/o = black 13 y/o = white **obesity contributes to breast development -- environmental factor. girls with early onset of breast budding have higher BMI scores than age-matched girls without budding.21 Among normal-weight girls, signs of puberty occurred before 8 years in fewer than 5% of White girls, 12% of Black girls, and 19% of Mexican-American girls.33 But girls with overweight or obese BMI levels had a significantly higher occurrence of early breast budding and early menarche. Thus the epidemic of childhood obesity is a major determinant of early-age pubertal milestones.
question
Breast Cancer
answer
We all have certain tumor suppressor genes termed BRCA1 and BRCA2; women who inherit a mutation on one or both have a significantly increased risk of developing breast or ovarian cancer. Evidence now shows that the prevalence of these mutations is about the same (at 1% to 4%) among breast cancer patients of African, Asian, White, and Hispanic descent.26 However, worldwide there exists significant racial and ethnic variation among the prevalence of these mutations, the access to genetic testing, and the recommended risk-management interventions. White women have a higher incidence of breast cancer than African-American women starting at 45 years of age. In contrast, African-American women have a higher incidence before age 45 years, and they are more likely to die of their disease at every age.2 Women from Asian-American, Hispanic, and American Indian groups have a lower incidence and lower death rates from breast cancer than Whites and African Americans have. Between 1992 and 2005 U.S. breast cancer rates rose and then started falling, reflecting the trend in hormone replacement therapy in certain perimenopausal women. In July 2002 the results of the Women's Health Initiative (WHI) study confirmed that long-term use of combined estrogen and progestin therapy increased the risk of developing breast cancer. A dramatic reduction in hormone use followed. Since 2006 studies in the United States, Europe, and Australia have shown an annual decline in breast cancer incidence of around 39010%.25 But the decreased incidence in the United States occurred only among White non-Hispanic women living in high-income counties who had estrogen receptor-positive tumors and were 50 years of age and older. The declines did not occur among Black, Hispanic, or Asian women; this may reflect the social pattern of hormone therapy use,25 i.e., women of color may have had decreased access to hormone replacement therapy, and this may have spared them the increase in breast cancer rates in the 1990s. Screening mammography can discover small, potentially curable breast cancers, and the American Cancer Society recommends beginning annual screening at 40 years of age. The percentage of women 40 years of age and older who report having a mammogram in the last 2 years was 66.5% in 2010.2 This included higher rates of cancer screening for women of color in recent years: 67% of non-Hispanic Whites, 66% of African Americans, 64.4% of Hispanics/Latinas, and 62% of Asians reported mammography. However, women least likely to have had a recent mammogram include those with less than a high school education, with no health insurance, or who are recent immigrants.2 Low-income women have multiple barriers to screening mammography, including lack of insurance coverage, lack of access to care, not having a regular health care provider, and lack of comprehensive breast cancer knowledge, not merely screening awareness.1 Lifestyle factors relate to breast cancer risk. Many studies have associated alcohol drinking with breast cancer risk in a dose-dependent measure. Recent evidence using the Nurses' Health Study cohort show that even low levels of drinking (3 to 6 drinks per week) were associated with a small increase in breast cancer risk, although the strongest risks were seen with cumulative consistent alcohol use through adult life.9 Recreational physical activity at any intensity level may reduce breast cancer risk, especially during the reproductive years and after menopause. However, postmenopausal weight gain may eliminate the profits of regular physical activity.28 Two dietary patterns have been studied: (1) "alcohol/Western" (meat products, French fries, appetizers, rice/pasta, potatoes, pizza, pies, canned fish, eggs, alcohol, cakes, mayonnaise, butter/cream); and (2) "healthy/Mediterranean" (vegetables, fruits, seafood, olive oil, sunflower oil). The first pattern has a modest positive association with breast cancer risk, especially with estrogen or progesterone receptor-positive tumors. The healthy Mediterranean diet has a modest protective effect.
question
Subjective Data
answer
Breast 1. Pain 2. Lump 3. Discharge 4. Rash 5. Swelling 6. Trauma 7. History of breast disease 8. Surgery or radiation 9. Medications 10. Patient-centered care Perform breast self-examination Last mammogram Axilla 1. Tenderness, lump, or swelling 2. Rash In Western culture the female breasts signify more than their primary purpose of lactation. Women are surrounded by excessive media influence that feminine norms of beauty and desirability are enhanced by and depend on the size of the breasts and their appearance. Women leaders have tried to refocus this attitude, stressing women's self-worth as individual human beings, not as stereotyped sexual objects. The intense cultural emphasis shows that the breasts are crucial to a woman's self-concept and her perception of her femininity. Matters pertaining to the breast affect the body image and generate deep emotional responses. This emotionality may take strong forms that you observe as you discuss the woman's history. One woman may be acutely embarrassed talking about her breasts, as evidenced by lack of eye contact, minimal response, nervous gestures, or inappropriate humor. Another woman may talk wryly and disparagingly about the size or development of her breasts. A young adolescent is acutely aware of her own development in relation to her peers. Or a woman who has found a breast lump may come to you with fear, high anxiety, and even panic. Although many breast lumps are benign, women initially assume the worst possible outcome (i.e., cancer, disfigurement, and death). While you are collecting the subjective data, tune in to cues for these behaviors that call for a straightforward and reasoned attitude.
question
Examiner Asks **BREAST** 1. Pain. Any pain or tenderness in the breasts? When did you first notice it? • Where is the pain? Localized or all over? • Is the painful spot sore to touch? Do you feel a burning or pulling sensation? Is the pain cyclic? Any relation to your menstrual period? • Is the pain brought on by strenuous activity, especially involving one arm; a change in activity; manipulation during sex; part of underwire bra; exercise? **LUMP** Ever noticed a lump or thickening in the breast? Where? • When did you first notice it? Changed at all since then? • Does the lump have any relation to your menstrual period? • Noticed any change in the overlying skin: redness, warmth, dimpling, swelling? **DISCHARGE** Any discharge from the nipple? • When did you first notice this? • What color is the discharge? • Consistency—thick or runny? • Odor? **RASH** Any rash on the breast? • When did you first notice this? • Where did it start? On the nipple, areola, or surrounding skin? **SWELLING** Any swelling in the breasts? In one spot or all over? • Related to your menstrual period, pregnancy, or breastfeeding? • Any change in bra size? **TRAUMA** Any trauma or injury to the breasts? • Did it result in any swelling, lump, or break in skin? **H/O BREAST DZ** Any history of breast disease yourself? • What type? How was it diagnosed? • When did it occur? • How is it being treated? • Any breast cancer in your family? Who? Sister, mother, maternal grandmother, maternal aunts, daughter? How about your father's side? • At what age did this relative have breast cancer? **SURGERY/RADIATION** Ever had surgery on the breasts? Was it a biopsy? What were the biopsy results? • Mastectomy? Mammoplasty—augmentation or reduction? • Ever had radiation to chest? What was it for? At what age? **MEDS** Have you taken oral contraceptives? For how long? • Hormone replacement therapy? (HRT) Estrogen and progestin? Estrogen only? For how long? 10. Patient-centered care • Have you ever been taught breast self-examination (BSE)? • How often do you perform it? What helps you remember? • Ever had mammography, a screening x-ray image of the breasts? When was the last mammogram? • The American Cancer Society recommends that women 20 to 39 years of age have a clinical breast examination (CBE) every 3 years; women 40 years of age and older have an annual mammogram and an annual CBE conducted close to the same time. **AXILLA** 1. Tenderness, lump, or swelling. Any tenderness or lump in the underarm area? • Where? When did you first notice it? 2. Rash. Any axillary rash? Please describe it. • Seem to be a reaction to deodorant? **Additional History for the Preadolescent** 1. Have you noticed your breasts changing? • How long has this been happening? 2. Many girls also notice other changes in their bodies that come with growing up. What have you noticed? • What do you think about all this? **Additional History for the Pregnant Woman** 1. Have you noticed any enlargement or fullness in the breasts? • Is there any tenderness or tingling? • Do you have a history of inverted nipples? 2. Are you planning to breastfeed your baby? ***Additional History for the Menopausal Woman** 1. Have you noticed any change in the breast contour, size, or firmness? (NOTE: Change may not be as apparent to obese women or to women whose earlier pregnancies already have produced breast changes.) **Risk Factor Profile for Breast Cancer** Breast cancer is the second major cause of death from cancer in women. However, early detection and improved treatment have increased survival rates. The 5-year survival rate for localized breast cancer has increased from 78% in the 1940s to 98% today. If the cancer has spread regionally, the survival rate is 84%.2
answer
Rationale -MASTALGIA: occurs with trauma, inflammation, infection, and benign breast disease. -Cyclic pain is common with normal breasts, oral contraceptives, and benign breast (fibrocystic) disease. Is pain related to specific cause? Carefully explore the presence of any lump. A lump present for many years and exhibiting no change may not be serious but still should be explored. Approach any recent change or new lump with suspicion. -GALACTORRHEA: . Note medications that may cause clear nipple discharge: oral contraceptives, phenothiazines, diuretics, digitalis, steroids, methyldopa, calcium channel blockers. -Bloody or blood-tinged discharge always is significant. Any discharge with a lump is significant. -Paget disease starts with a small crust on the nipple apex and spreads to areola (see Table 17-6, Abnormal Nipple Discharge, p. 410). -Eczema or other dermatitis rarely starts at the nipple unless it is caused by breastfeeding. It usually starts on the areola or surrounding skin and then spreads to the nipple. A lump from an injury (seat belt injury, direct blow) is caused by local hematoma or edema and resolves shortly. Past breast cancer increases the risk for recurrent cancer (see Table 17-2, Breast Cancer Risk Factors in Women, p. 393). presence of benign breast disease makes the breasts harder to examine; the general lumpiness conceals a new lump. Breast cancer occurring before menopause in certain family members increases risk for this woman (see Table 17-2). Biopsy-confirmed atypical hyperplasia increases breast cancer risk. Between ages 10-30 years, chest radiation exposure has greatest risk of breast cancer later in life. Oral contraceptives may control symptoms of benign ("fibrocystic") breast disease. Combined HRT after menopause increases risk of BC, even with 2 years' use. -Increased risk applies only for current ; recent users. -Use of estrogen alone does not increase risk of breast cancer. Awareness that BSE, CBE, and mammograms are complementary screening measures. With good BSE practice, a woman knows how her breasts normally feel and can detect any change more easily. Mammography can reveal cancers too small to be detected by the woman or by the most experienced examiner. However, interval lumps may become palpable between mammograms. Breast tissue extends up into the axilla. The axilla also contains many lymph nodes. Developing breasts are the most obvious sign of puberty and the focus of attention for most girls, especially in comparison with peers. Assess each girl's perception of her own development, and provide teaching and reassurance as indicated. Breast changes are expected and normal during pregnancy. Assess the woman's knowledge and provide reassurance. Inverted nipples may need special care in preparation for breastfeeding. Breastfeeding alone for 6 months provides the perfect food and antibodies for the baby, decreases risk for ear infections, promotes bonding, and provides relaxation. It is also protective against breast cancer. Decreased estrogen level causes decreased firmness. Rapid decrease in estrogen level causes actual shrinkage. The best way to detect a person's risk for breast cancer is by asking the right history questions. Table 17-2 highlights risk factors for breast cancer and, from these, you can fashion your questions. Be aware that most breast cancers occur in women with no identifiable risk factors except sex and age. Just because a woman does not report the cited risk factors does not mean that you or she should fail to consider breast cancer seriously.
question
Breast Cancer Risk Factors -- Women >4.0 2.1-4.0 1.1-2.0 *Relative risk compares the risk of disease among people with a particular exposure to the risk to the risk among people without that exposure. If the relative risk is above 1.0, risk is higher among exposed than unexposed persons.
answer
• Age (65+ vs. <65 years, although risk increases across all ages until age 80) • Biopsy-confirmed atypical hyperplasia • Certain inherited genetic mutations for breast cancer (BRCA1 and/or BRCA2) • Lobular carcinoma in situ • Mammographically dense breasts • Personal history of early onset (<40 years) breast cancer • Two or more first-degree relatives with breast cancer diagnosed at an early age • Personal history of breast cancer (40+ years) • High endogenous estrogen or testosterone levels (postmenopausal) • High-dose radiation to chest • One first-degree relative with breast cancer • Alcohol consumption • Ashkenazi Jewish heritage • Diethylstilbestrol (DES) exposure • Early menarche (30 years) • Late menopause (>55 years) • Never breastfed a child • No full-term pregnancies • Obesity (postmenopausal)/adult weight gain • Personal history of endometrial, ovarian, or colon cancer • Recent and long-term use of menopausal hormone therapy containing estrogen and progestin • Recent oral contraceptive use
question
Objective Data Preparation: The CBE screens for breast masses and abnormalities, evaluates any presenting symptoms, and presents an opportunity for you to teach breast self-awareness and examination. Some have listed that harms of screening could be false-positive results and overdiagnosis.29 However, these are mitigated by using proper technique and spending an adequate amount of time. Plan to take a few minutes for a careful examination of the average size breast.8 Begin with the woman sitting up and facing you. You may use a short gown, open at the back, and lift it up to the woman's shoulders during inspection. During palpation when the woman is supine, cover one breast with the gown while examining the other. Be aware that many women are embarrassed to have their breasts examined; use a sensitive but matter-of-fact approach. After your examination be prepared to teach the woman BSE.
answer
Equipment Needed Small pillow Ruler marked in centimeters Pamphlet or teaching aid for BSE
question
Normal Range of Findings Inspect Breasts General Appearance: -symmetry of size ; shape. -common for slight asymmetry in size. (left breast commonly larger than right)
answer
Abnormal Findings -sudden increase in the size of one breast signifies inflammation or new growth.
question
Skin -skin normally is smooth and of even color. Note any localized areas of redness, bulging, or dimpling. Also note any skin lesions or focal vascular pattern. A fine blue vascular network is visible normally during pregnancy. Pale linear striae, or stretch marks, often follow pregnancy. Normally no edema is present. Edema exaggerates the hair follicles, giving a "pigskin" or "orange-peel" look (also called peau d'orange).
answer
*Hyperpigmentation. Redness and heat with inflammation. Unilateral dilated superficial veins in a nonpregnant woman. Edema. Signs of retraction & inflammation.
question
Nipple -The nipples should be placed symmetrically on the same plane on the two breasts. Nipples usually protrude, although some are flat and some are inverted. They tend to stay in their original condition. Distinguish a recently retracted nipple from one that has been inverted for many years or since puberty. Normal nipple inversion may be unilateral or bilateral and usually can be pulled out (i.e., it is not fixed). -Note any dry scaling, fissure or ulceration, and bleeding or other discharge. -A supernumerary nipple is a normal and common variation. An extra nipple along the embryonic "milk line" on the thorax or abdomen is a congenital finding. Usually it is 5 to 6 cm below the breast near the midline and has no associated glandular tissue. It looks like a mole, although a close look reveals a tiny nipple and areola. It is not significant; merely distinguish it from a mole.
answer
-Deviation in pointing. Recent nipple retraction signifies acquired disease -Explore any discharge, especially in the presence of a breast mass. -Rarely additional glandular tissue, called a supernumerary breast, is present.
question
Maneuvers to Screen for Retraction -Direct the woman to change position while you check the breasts for skin retraction signs. First ask her to lift her arms slowly over her head. Both breasts should move up symmetrically -Next ask her to push her hands onto her hips and to push her two palms together. These maneuvers contract the pectoralis major muscle. A slight lifting of both breasts occurs. -Ask the woman with large, pendulous breasts to lean forward while you support her forearms. Note the symmetric free-forward movement of both breasts
answer
-Retraction signs are caused by fibrosis in the breast tissue, usually caused by growing neoplasms. The fibrosis shortens with time, causing contrasting signs with the normally loose breast tissue. Note a lag in the movement of one breast. Note a dimpling or a pucker, which indicates skin retraction - Note fixation to chest wall or skin retraction
question
Inspect & palpate axillae -Examine the axillae while the woman is sitting. Inspect the skin, noting any rash or infection. Lift the woman's arm and support it yourself so her muscles are loose and relaxed. Use your right hand to palpate the left axilla (Fig. 17-12). Reach your fingers high into the axilla. Move them firmly down in four directions: (1) down the chest wall in a line from the middle of the axilla, (2) along the anterior border of the axilla, (3) along the posterior border, and (4) along the inner aspect of the upper arm. Move the woman's arm through range of motion to increase the surface area that you can reach. -Usually nodes are not palpable, although you may feel a small, soft, nontender node in the central group. Expect some tenderness when palpating high in the axilla. Note any enlarged and tender lymph nodes.
answer
-Nodes enlarge with any local infection of the breast, arm, or hand and with breast cancer metastases.
question
Palpate Breasts -Help the woman to a supine position. Tuck a small pad under the side to be palpated and raise her arm over her head. These maneuvers flatten the breast tissue and displace it medially. Any significant lumps then feel more distinct (Fig. 17-13). For pendulous breasts, to distribute the tissue medially across the chest wall, ask the woman to rotate her hips opposite to the side you are palpating. -Use the pads of your first 3 fingers and make a gentle rotary motion on the breast. Vary your pressure so you are palpating light, medium, and deep tissue in each location. The vertical strip pattern (Fig. 17-14) is the best way to detect a breast mass, but two other patterns are in common use: from the nipple palpating out to the periphery as if following spokes on a wheel and palpating in concentric circles out to the periphery. ***Vertical strip pattern of palpation. -For the vertical strip pattern, start high in the axilla and palpate down the midaxillary line just lateral to the breast down to the bra line. Proceed medially in overlapping vertical lines ending at the sternal edge. Take care to palpate every square inch of the breast and examine the tail of Spence high into the axilla. This should take a few minutes with each breast. Be consistent and thorough in your approach to each woman. -In nulliparous women normal breast tissue feels firm, smooth, and elastic. After pregnancy the tissue feels softer and looser. Premenstrual engorgement is normal from increasing progesterone. This consists of slight enlargement, tenderness to palpation, and generalized nodularity; the lobes feel prominent, and their margins more distinct. -In addition, normally you may feel a firm transverse ridge of compressed tissue in the lower quadrants. -This is the inframammary ridge, and it is especially noticeable in large breasts. Do not confuse it with an abnormal lump. -What about the occasional woman with breast implants? Correctly placed implants are located behind the breast tissue. Therefore follow the same steps for CBE as shown for the woman without implants. -After palpating over the four breast quadrants, palpate the nipple (Fig. 17-15). Note any induration or subareolar mass. With your thumb and forefinger gently depress the nipple tissue into the well behind the areola. The tissue should move inward easily. If the woman reports spontaneous nipple discharge, press the areola inward with your index finger; repeat from a few different directions. If any discharge appears, note its color and consistency. -For the woman with large, pendulous breasts, you may palpate by using a bimanual technique (Fig. 17-16). The woman is in a sitting position, leaning forward. Support the inferior part of the breast with one hand. Use your other hand to palpate the breast tissue against your supporting hand. -If the woman mentions a breast lump that she has discovered herself, examine the unaffected breast first to learn a baseline of normal consistency for this woman. If you do feel a lump or mass, note the following characteristics. 1. Location—Using the breast as a clock face, describe the distance in centimeters from the nipple (e.g., "7:00, 2 cm from the nipple"). Or diagram the breast in the woman's record and mark in the location of the lump. 2. Size—Judge in centimeters in 3 dimensions: width × length × thickness. 3. Shape—State whether the lump is oval, round, lobulated, or indistinct. 4. Consistency—State whether the lump is soft, firm, or hard. 5. Movable—Is the lump freely movable, or is it fixed when you try to slide it over the chest wall? 6. Distinctness—Is the lump solitary or multiple? 7. Nipple—Is it displaced or retracted? 8. Note the skin over the lump—Is it erythematous, dimpled, or retracted? 9. Tenderness—Is the lump tender to palpation? 10. Lymphadenopathy—Are any regional lymph nodes palpable? -Premenopausal women at midcycle often have tissue edema and mastalgia (pain) that make it hard to detect a lesion. If your findings are in question, consider asking this woman to return for a follow-up examination the first week after her menses, when hormone levels are lower and edema is not present. The woman with a healing or healed mastectomy needs special consideration. She may be very concerned about a recurrence of cancer and be anxious for your findings. Inspect and palpate as described previously. Be gentle around the scar area because these tissues are quite sensitive. There should be no inflammation or infection. Lymphedema of the upper arms is a common sequela because of interruption of lymphatic drainage and removal of nodes.
answer
Heat, redness, and swelling in nonlactating and nonpostpartum breasts indicate inflammation. -Except in pregnancy and lactation, discharge is abnormal (see Table 17-6). Note the number of discharge droplets and the quadrant(s) producing them. Blot the discharge on a white gauze pad to ascertain its color. Test any abnormal discharge for the presence of blood. Breast Lumps, and Table 17-5, Differentiating Breast Lumps, for a description of common breast lumps with these characteristics. Screening measures aim to detect breast lumps when small and potentially curable. The acronym BREAST lists physical signs associated with more advanced cancer: Breast mass, Retraction, Edema, Axillary mass, Scaly nipple, Tender breast.
question
Male Breast -Your examination of the male breast can be abbreviated, but do not omit it. Combine the breast examination with that of the anterior thorax. Inspect the chest wall, noting the skin surface and any lumps or swelling. -Palpate the nipple area for any lump or tissue enlargement (Fig. 17-19). It should feel even, with no nodules. Palpate the axillary lymph nodes. -The normal male breast has a flat disk of undeveloped breast tissue beneath the nipple. Gynecomastia is a benign growth of this breast tissue, making it distinguishable from the other tissues in the chest wall (Fig. 17-20). It feels like a smooth, firm, movable disk. This occurs in about one half of adolescent boys at 13 or 14 years of age. -It can be unilateral or bilateral and is temporary. The adolescent is acutely aware of his body image and feels distressed. Reassure him that this change is normal, common, and temporary.
answer
-Male breast cancer is rare (see Table 17-8, Male Breast Abnormalities, p. 411) but usually presents with painless, firm, retroareolar lump. Also note less frequent signs: nipple discharge (clear or bloody), ulceration, retraction, axillary lymphadenopathy. Nipple discharge is rare but strongly associated with cancer; thus it demands detailed evaluation. -Gynecomastia also occurs with use of anabolic steroids, some medications, cirrhosis, and other disease states.
question
Abnormal Findings Signs of Retraction ; inflammation

answer
Dimpling The shallow dimple (also called a skin tether) shown here is a sign of skin retraction. Cancer causes fibrosis, which contracts the suspensory ligaments. The dimple may be apparent at rest, with compression, or with lifting of the arms. Also note the distortion of the areola here as the fibrosis pulls the nipple toward it.
question
Nipple Retraction.

answer
The retracted nipple looks flatter and broader, like an underlying crater. A recent retraction suggests cancer, which causes fibrosis of the whole duct system and pulls in the nipple. It also may occur with benign lesions such as ectasia of the ducts. Do not confuse retraction with the normal long-standing type of nipple inversion, which has no broadening and is not fixed.
question
Edema (Peau d'Orange)

answer
Lymphatic obstruction produces edema. This thickens the skin and exaggerates the hair follicles, giving a pigskin or orange-peel look. This condition suggests cancer. Edema usually begins in the skin around and beneath the areola, the most dependent area of the breast. Also note nipple infiltration here.
question
Fixation
answer
Asymmetry, distortion, or decreased mobility with the elevated arm maneuver. As cancer becomes invasive, the fibrosis fixes the breast to the underlying pectoral muscles. Here note that the right breast is held against the chest wall.
question
Deviation in nipple pointing

answer
An underlying cancer causes fibrosis in the mammary ducts, which pulls the nipple angle toward it. Here note the swelling behind the right nipple and that the nipple tilts laterally.
question
BREAST LUMPS Benign ("Fibrocystic") Breast Disease
answer
-Multiple tender masses that occur with numerous symptoms and physical findings: • Swelling and tenderness (cyclic discomfort) • Mastalgia (severe pain, both cyclic and noncyclic) • Nodularity (significant lumpiness, both cyclic and noncyclic) • Dominant lumps (including cysts and fibroadenomas) • Nipple discharge (including intraductal papilloma and duct ectasia) • Infections and inflammations (including subareolar abscess, lactational mastitis, breast abscess, and Mondor disease) -Many women have some form of benign breast disease. Nodularity occurs bilaterally; regular, firm nodules are mobile, well demarcated, and feel rubbery like small water balloons. Pain may be dull, heavy, and cyclic as nodules enlarge. Some women have nodularity but no pain and vice versa. Cysts are discrete, fluid-filled sacs. Dominant lumps and nipple discharge must be investigated carefully. Nodularity itself is not premalignant but produces difficulty in detecting other cancerous lumps.
question
Cancer
answer
Solitary, unilateral, nontender mass. Single focus in one area, although it may be interspersed with other nodules. Solid, hard, dense, and fixed to underlying tissues or skin as cancer becomes invasive. Borders are irregular and poorly delineated. Grows constantly. Often painless, although the person may have pain. Most common in upper outer quadrant. Found in women 30 to 80 years of age; increased risk across all ages until age 80 years. As cancer advances, signs include firm or hard irregular axillary nodes; skin dimpling; nipple retraction, elevation, and discharge.
question
FIBROADENOMA
answer
Benign tumors; most commonly present as self-detected in late adolescence. Solitary nontender mass that is solid, firm, rubbery, and elastic. Round, oval, or lobulated; 1 to 5 cm. Freely movable, slippery; fingers slide it easily through tissue. Usually no axillary lymphadenopathy. Diagnose by triple test (palpation, ultrasound, and needle biopsy). Because of risk of deformity of surgery to a growing breast, excisional surgery is reserved for masses >5 cm; for continuously enlarging, well-circumscribed, multiple masses; or with suspicious ultrasound findings.
question
Abnormal Nipple Discharge Mammary Duct Ectasia

answer
Pastelike matter in subareolar ducts produces sticky, purulent discharge that may be white, gray, brown, green, or bloody. A light green, single duct discharge is shown here. Caused by stagnation of cellular debris and secretions in the ducts, leading to obstruction, inflammation, and infection. Usually occurs in perimenopause. Itching, burning, or drawing pain occurs around nipple. May have subareolar redness and swelling. Ducts are palpable as rubbery, twisted tubules under areola. May have palpable mass, soft or firm, poorly delineated. Not malignant but needs biopsy.
question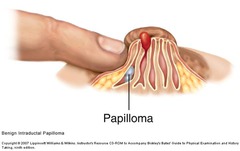
Intraductal Papilloma
answer
These are discrete benign tumors that arise in a single or multiple papillary duct(s). May have serous or serosanguineous discharge. Often there is a palpable nodule in underlying duct (highlighted here). Most common in women ages 40 to 60 years. Most are benign, although multiple papillomas have a higher risk of subsequent cancer than do solitary ones.30 Requires core needle biopsy and possible excision.
question
Carcinoma
answer
Bloody nipple discharge that is unilateral and from a single duct requires further investigation. Although there was no palpable lump associated with the discharge shown here, mammography revealed a 1-cm, centrally located, ill-defined mass.
question
Paget Disease (Intraductal Carcinoma)
answer
Early lesion has unilateral, clear, yellow discharge and dry, scaling crusts, friable at nipple apex. Spreads outward to areola with erythematous halo on areola and crusted, eczematous, retracted nipple. Later lesion shows nipple reddened, excoriated, and ulcerated with bloody discharge, and an erythematous plaque surrounding the nipple. Symptoms include tingling, burning, itching. Except for the redness and occasional cracking from initial breastfeeding, any dermatitis of the nipple area must be explored carefully and referred immediately.
question
DISORDERS DURING LACTATION MASTITIS

answer
This is uncommon; an inflammatory mass before abscess formation. Usually occurs in single quadrant. Area is red, swollen, tender, very hot, and hard, here forming outward from areola upper edge in right breast. The woman also has a headache, malaise, fever, chills, sweating, increased pulse, flulike symptoms. May occur during first 4 months of lactation from infection or from stasis from plugged duct. Treat with rest, local heat to area, antibiotics, and frequent nursing to keep breast as empty as possible. Must not wean now, or the breast will become engorged, and the pain will increase. Mother's antibiotic not harmful to infant. Usually resolves in 2 to 3 days.
question
BREAST ABSCESS
answer
rare complication of generalized infection (e.g., mastitis) if untreated. A pocket of pus that feels hard, looks red, and is quite tender accumulates in one local area. Here there is extensive nipple edema, and abscess is "pointing" at 3 o'clock position on areolar margin. May nurse depending on location of abscess, associated pain, and type of medicine. Continue to nurse on unaffected side. Treat with antibiotics, surgical incision, and drainage.
question
PLUGGED DUCT
answer
This is common when milk is not removed completely because of poor latching, ineffective suckling, infrequent nursing, or switching to second breast too soon.3 There is a tender lump that may be reddened and warm to touch. No infection. It is important to keep breast as empty as possible and milk flowing. The woman should nurse her baby frequently on affected side first to ensure complete emptying and manually express any remaining milk. A plugged duct usually resolves in less than 1 day.
question
MALE BREAST ABNORMALITIES GYNECOMASTIA

answer
Benign enlargement of male breast that occurs when estrogen concentration exceeds testosterone levels. It is a mobile disk of tissue located centrally under the nipple-areola. At puberty it is usually mild and transient. In older men it is bilateral, tender, and firm but not as hard as breast cancer. Gynecomastia occurs with Cushing syndrome, liver cirrhosis (because estrogens cannot be metabolized), adrenal disease, hyperthyroidism, and numerous drugs: alcohol and marijuana; estrogen treatment for prostate cancer; antibiotics (metronidazole, isoniazid); spironolactone, digoxin, angiotensin-converting enzyme (ACE) inhibitors; psychoactive drugs (diazepam, tricyclic antidepressants).



