USMLE Step 2 CK OBGYN" and secrets – Flashcards
Unlock all answers in this set
Unlock answersquestion
Embryologic origin of uterus
answer
Fusion of the 2 Mullerian ducts
question
When is transvaginal transducer ultrasound used? Transabdominal transducer?
answer
Transvaginal transducer: ("pie shaped image") - lower pelvic masses - not influenced by thickness of maternal abdominal wall Transabdominal transducer: - entire pelvis as well as abdomen imaging Ultrasound works best when adjacent tissues have differing echodensities, particularly fluid/tissue interfaces
question
Average age range of menarche? Thelarche?
answer
menarche: 10-16.5y thelarche: breast development; 8~11y
question
What is the average age for Tanner II stage of breast development? Presentation?
answer
Tanner II: Breast development - 8-13 yrs - Breast buds begin
question
ASCUS?
answer
Atypical Squamous Cells of Uncertain Significance misreadings on Pap smears due to mechanical errors (drying, etc.)
question
Major structures of the uterus (3)
answer
Corpus (body) - Cornu (uterus join with fallopian tubes) Isthmus Cervix
question
Describe satisfactory colposcopy vs. unsatisfactory colposcopy
answer
Satisfactory colposcopy 1. T-zone does NOT extend into the endocervical canal 2. No lesions visualized within T-zone Unsatisfactory is the opposite..
question
Tanner stages: Pubic Hair
answer
Male + Female Tanner I: None (prepubertal state) Tanner II: small amount of long, downy hair with slight pigmentation on the labia majora Tanner III: hair becomes more coarse and curly and begins to extend laterally Tanner IV: adult-like hair quality, extending across pubis but sparing medial thighs Tanner V: hair extends to medial surface of the thighs
question
What are the risks of cone biopsy? (3)
answer
1. incompetent cervix (cutting too much) 2. cervical stenosis (can cause amenorrhea) 3. preterm birth
question
Traditional Pap vs. Liquid-based Pap
answer
Traditional Pap: - spatula for ectocervix* - cyto-brush for endocervical canal* (rotating in 1 direction 360°) - both specimens are smeared onto a glass slide, fixed with formalin, then stained *Potential problems* - ASCUS (atypical squamous cells of uncertain significance) cannot be diagnosed - insufficient smearing, air-drying artifacts if process is delayed, mechanical problems makes traditional technique obsolete Liquid-based Pap: - cervical broom* to collect specimens (rotated 5 times in same direction) - broom is placed into "formalin" solution and rotated 10 times to release collected material - this method is more preferred vs. traditional Pap due to absence of mechanical errors - ASCUS can also be used for HPV-DNA typing
question
What is special about Tanner IV stage of breast development?
answer
Papilla and areola forms a 2' mound not contour with surrounding breast
question
LEEP (loop electrosurgical excision procedure) description, procedure, followup, risks
answer
A thin low-voltaged loop cuts out abnormal cervical tissue identified with colposcopy advantage: visual confirmation lesions have been removed; no anesthesia needed followup Pap smear every 3-6 months for 2 years to ensure dysplastic changes to not return long-term risks of LEEP include - cervical stenosis - cervical insufficiency
question
What type of blood supply do oviducts receive? From where?
answer
Dual blood supply* Receives blood from the uterine artery and ovarian artery
question
What is the average age range for Tanner V stage of breast development?
answer
Tanner V: Breast development - 12.5~18.5 yrs - development is complete
question
What does the ovarian stroma produce?
answer
androgen Important for libido after menopause
question
Dilation and Curettage (D&C) procedure
answer
under anesthesia examines histology of endometrial lesions similar to endometrial biopsy; dilation of cervix is required to introduce curette can collect large amounts of endometrial tissue (>endometrial biopsy)
question
What are the 4 segments of the oviducts?
answer
Proximal → Distal "INTERcourse IS AMP and FUN" 1. Interstitium 2. Isthmus 3. Ampulla 4. Infundibulum
question
American Cancer Society recommendations
answer
1. initial study at age 34 if there are risk factors (breast cancer in first degree relative, BRCA genes, etc.) 2. routine screening at age 40 if there are no risk factors
question
Explain the formation of the T-zone
answer
at puberty the vaginal pH falls (due to estrogen dominance) the "native" columnar epithelium goes through metaplasia and becomes the transformation zone; normal-appearing "metaplastic" stratified squamous epithelium Old→New squamocolumnar junction (outer-to-inner)
question
Procedure associated with assessment of Asherman's syndrome
answer
HSG hysterosalpingogram
question
Cryotherapy description, procedure, followup, risks
answer
Destroys dysplastic cervical tissue identified by colposcopy and cervical biopsy; no anesthesia needed Cryo probe at -50℃ with liquid nitrogen Freeze and destroy tissue; 3 minutes intervals of freezing Watery discharge will occur over next few weeks as destroyed tissue sloughs off Followup Pap smears every 3-6 months for 2 years; disadvantage of not knowing if lesions are destroyed until followups Risks: cervical stenosis
question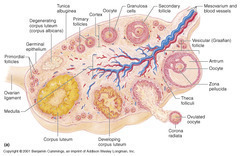
Phases of development: Folliculogenesis
answer
Primordial: - dormant, small - 1 layer of flat granulosa cells Primary: - Mitotic cells - cuboidal granulosa cells Secondary: - Theca cells - Multiple layers of granulosa cells Tertiary: - Fully formed antrum Graafian (vesicular) follicle: - preovulatory follicle; fully mature
question
Tanner stages: Breast development
answer
Tanner I: no glandular tissue; areola follows skin contours of the chest (prepubertal) Tanner II: breast bud forms with small area of surrounding glandular tissue; areola beings to widen - 8-13yrs Tanner III: breast begins to become more elevated and extends beyond borders of areola; remains in contour with surrounding breast Tanner IV: increased breast size and elevation; areola and papilla form a secondary mound projecting from the contour of the surrounding breast Tanner V: adult size; areola returns to contour of the surrounding breast, with projecting central papilla (nipple) - 12.5-18.5yrs
question
Colposcopy description
answer
"binoculars into the vagina" 1. *visually* identify where abnormal Pap smear cells originated 2. biopsy that area to send for histologic diagnosis
question
Average length of a vagina
answer
8-9cm
question
What is the lymphatic drainage of the ovaries?
answer
Pelvic nodes Para-aortic nodes
question
What are the organ systems we need to consider involving pelvic pain/pelvic mass?
answer
GI (colons) Uterus Bladder
question
What is the most common anatomical position of the uterus?
answer
Anteverted (50%) mid-position (25%) retroverted (25%)
question
Endometrial biopsy
answer
examines histology of endometrial lesions hollow suction cannula is placed into uterine cavity and suction is applied; rotation of cannula before fixing with formalin
question
Which portion of the cervix is most concerned for scrapings during a Pap smear?
answer
Transformation zone (T-zone) - 95% of cervical dysplasia and cancer develops here - screening for squamous cell carcinoma (most common cancer of the cervix 80%) - area between old (outer, "O") squamocolumnar junction and new (inner) squamocolumnar junction
question
Risks of mammography
answer
high radiation (0.7 mSv) same as background radiation in 3 months 1 rad = 10 mSv
question
What is the specimens required for a Pap smear? What diseases are they mostly screening for?
answer
2 areas 1. T-zone of the ectocervix (squamous cell carcinoma; most common cancer of cervix 80%) 2. columnar epithelium of endocervical canal (adenocarcinoma; 2nd most common cancer of cervix 15%)
question
Hysterosalpingogram (HSG) description and procedure
answer
procedure performed without anesthesia, radio-opaque fluid injected at endocervical canal allowing assessment of uterine malformations and Asherman's syndrome dye is supposed to spill into pelvic cavity; non-spillage can be a sign of fallopian tube occlusion or blockage
question
Vulvar biopsy
answer
done with punch biopsy or scalpel performed under local anesthesia, histology of vulvar lesions
question
Hysterectomy types
answer
removal of uterus "hyster" root comes from the misled belief women are crazy because of their uterus 1. subtotal: removes only teh corpus, leaving cervix in place 2. total: removes both corpus and cervix of uterus (aka simple hysterectomy) 3. radical hysterectomy: performed for early stage CIN, involves removal of the uterus, cervix, and surrounding tissues, including cardinal ligaments, uterosacral ligaments, and the upper vagina (can involve removing lymph nodes depending on stages of CIN)
question
What is the term for the surgery of removing ovaries?
answer
removal of ovaries Salpingo-oophorectomy
question
Cone biopsy: wide-shallow cone vs. narrow-deep cone
answer
Cone biopsy; both procedures need anesthesia Wide-shallow cone: - performed if Pap smear shows changes more severe than the colposcopically directed biopsy Narrow-deep cone: - performed if a lesion extends from the exocervix into teh endocervical canal
question
The pelvic floor is made up of which diaphragms? What structures do they hold?
answer
Pelvic diaphragm: - levator ani (puborectalis, pubococcygeus, ileococcygeus) - coccygeus muscles Perineal membrane (urogenital diaphragm): - triangular sheet of dense fibromuscular tissue "anterior triangle" that spans the anterior half of the pelvic outlet - vagina and urethra pass through the perineal membrane
question
Most common cause of uterine prolapse?
answer
childbirth
question
Uterine prolapse classification
answer
Grade I: cervix descends half way to introitus Grade II: cervix descends to introitus Grade III: cervix extends outside the introitus Grade IV or procidentia: entire uterus, as well as the anterior and posterior vaginal walls, extends outside the introitus
question
What is procidentia?
answer
Grade IV Uterine prolapse entire uterus + anterior and posterior vaginal walls extends outside the introitus
question
Vaginal prolapse classification
answer
Cystocele (most common): anterior vaginal wall prolapse; contains the bladder Rectocele (2nd most common): posterior vaginal wall prolapse; contains the rectum Enterocele (3rd): rectouterine pouch/pouch of Douglas prolapse
question
What is the triad for rectocele diagnosis?
answer
1. postmenopausal woman 2. Posterior vaginal wall protrusion 3. Digitally assisted removal of stool "digital splitting"
question
Management of pelvic relaxation: non-surgical
answer
Non-surgical: - Kegel exercises (learning to control pubococcygeus muscle; "magazine for better sex"; kegel weights) - Estrogen replacement in postmenopausal women - Pessaries (mechanical method)
question
Management of pelvic relaxation: surgical
answer
Surgical: when conservative methods fail - vaginal hysterectomy (with vagina vault suspension) + anterior/posterior vaginal repair - anterior and posterior colporrhaphy: uses endopelvic fascia that supports bladder and rectum
question
Diagnosis of prolapse in pelvic relaxation is done how?
answer
Tell the patient to perform Valsalva in lithotomy position
question
Average age of menopause?
answer
51-52
question
Physiology: continence vs. micturition
answer
balance between urethral closure & detrusor muscle (bladder muscle) activity urethral sphincter pressure normally > bladder pressure = urine continence urethral pressure decreases < bladder pressure = micturition/voiding Normally proximal urethra + bladder both within the pelvis (prolapse can alter this state leading to incontinence); intraabdominal pressure increases (valsalva) are transmitted equally to both, leaving the pressure difference unchanged; continence detrusor muscle spontaneous contractions are normally easily suppressed
question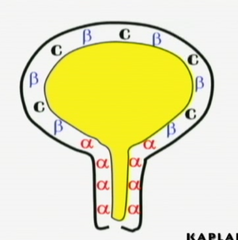
Pharmacology: bladder receptors innervation
answer
α-adrenergic receptors: Sympathetic nervous system - "Sympathetic SHOOTS" hence urethral sphincters contract to inhibit incontinence during ejaculation - primarily found in urethra - *prevent* micturition; *contraction* of urethral - Drugs agonists: ephedrine, imipramine, estrogens - Drugs antagonists: phenoxybenzamine β-adrenergic receptors: Sym. nervous system - *prevents micturition*; relaxation of bladder detrusor muscles hence prevents urination - primarily in the detrusor muscle - Drugs agonists: flavoxate, progestins Cholinergic receptors: Parasympathetic innervation - *enhances micturition* - primarily also in detrusor muscle; *contraction* - Drugs agonists: bethanecol, neostigmine - Drugs antagonists: oxybutynin, propantheline
question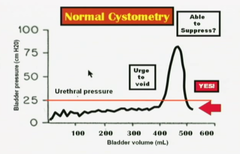
Cystometry Volume Measurements
answer
Post-void residual volume = <50mL Sensation of fullness = 200-225mL Urge to void = 400-500mL Normally a patient should be able to suppress the urge to void. (shown on graph) Involuntary contractions can be seen by watching saline level in the syringe rise/fall; normally there should not be any involuntary contractions
question
Sensory Irritative Incontinence: etiology, history, examination, investigative studies, management
answer
Etiology: - involuntary rises in bladder pressure - results in detrusor contractions - possible causes: infection, stone, tumor, foreign body History: - loss of urine occurs with *urgency, frequency and dysuria* - can take place *day or night* Examination: - suprapubic tenderness may be elicited - pelvic examination normal (no prolapse of any sort) - neurological exam normal (anal contraction reflex normal, S2-3-4; by stimulating labia majora we get a anal contraction) Investigative study: *urinalysis* - bacteria and WBC (infection) - RBC (stone, foreign body, tumor) - positive urine culture (infection) - normal cystometric studies (normal RV with involuntary detrusor contractions present) Management: - antibiotics (infections) - cystoscopy to diagnose and remove stones, foreign bodies, tumors
question
Inhibit voiding Tx: bladder relaxants/antispasmodics
answer
oxybutynin (Ditropan) flavoxate (Urispas)
question
Inhibit voiding Tx: bladder relaxant/anticholinergics
answer
Pro-Banthine
question
Inhibit voiding Tx: bladder relaxant/tricyclics
answer
Imipramine (Tofranil)
question
Inhibit voiding Tx: vesical neck contraction/alpha adrenergics
answer
ephedrine Imipramine Estrogen stimulates alpha receptors Progesterone stimulates beta receptors
question
Which receptors do estrogen stimulate? progesterone?
answer
Estrogen stimulates alpha receptors Progesterone stimulates beta receptors
question
Promote voiding Tx: bladder contraction/cholinergics
answer
Bethanechol (Urecholine) Neostigmine (Prostigmin)
question
Promote voiding Tx: vesicle neck relaxants/alpha antagonists
answer
methyldopa phenothiazines
question
Genuine Stress Incontinence: Etiology, history, examination, investigative studies, management
answer
Etiology: - most common form of true urinary incontinence - rises in bladder pressure because of intraabdominal pressure increase - not transmitted to proximal urethra due to pelvic relaxation and not being a part of pelvic structures anymore - *loss of bladder support* History: - loss of urine occurs in small spurts simultaneously with coughing or sneezing - *Does NOT* take place when patient is sleeping Examination: - cystocele may be seen - Neurologic examination is normal - Q-tip test is positive (q-tip placed within the urethra and patient increases intraabdominal pressure, the q-tip will rotate >30 degrees) Investigative studies: - urinalysis + culture are normal - cystometric studies are normal - *no* involuntary detrusor contractions seen Management: Mostly similar to pelvic relaxation management - Kegel exercises - estrogen replacement (stimulates alpha receptors) - surgical therapy aims to elevate the urethral sphincter (Burch procedure, MML, tension-free vaginal tape procedure)
question
What is the most common form of true urinary incontinence?
answer
Genuine stress incontinence
question
What is the only incontinence that does not result in voiding during the night?
answer
Genuine stress incontinence
question
What is the triad of stress incontinence?
answer
Involuntary loss of urine (large) with coughing and sneezing (increase abdominal pressure) No urine lost at night
question
Motor Urge (Hypertonic) Incontinence: etiology, history, examination, investigative studies, management
answer
Etiology: 'Itty-Bitty Bladder Syndrome' - involuntary rises in bladder pressure from idiopathic detrusor contractions that cannot be voluntarily suppressed History: - loss of urine occurs in large amounts; often without warning - day + night - most common symptom is urgency Examination: - pelvic examination shows normal anatomy - neurologic examination is normal Investigative studies: - urinalysis + culture normal - cystometric studies show normal residual volume - *involuntary detrusor contractions are present even with small volumes of urine in the bladder* Management: - anticholinergic medications - NSAIDS to inhibit detrusor contractions - tricyclic anti-depressants - calcium-channel blockers
question
What is the triad for hypertonic bladder?
answer
Involuntary loss of urine cannot suppress urge to void urine loss day + night
question
Hypertonic incontinence vs. Hypotonic incontinence
answer
Hypertonic: - large volume urine loss - idiopathic detrusor muscle contraction - day + night Hypotonic: - small volume urine loss (until urethral sphincter = bladder pressure) - bladder never empties; detrusor muscle relaxation - day + night
question
Overflow/Neurogenic (Hypotonic) Incontinence: etiology, history, examination, investigative studies, management
answer
etiology: - Rises in bladder pressure occur gradually from over-distended, hypotonic bladder - voiding occurs only when bladder pressure > urethral sphincter pressure - *bladder never empties*; voiding occurs only until bladder pressure = urethral sphincter pressure - may be due to denervated bladder (diabetic neuropathy, MS, or systemic medication) history: - loss of urine occurs intermittently in small amounts* - day + night - pelvic fullness is a common symptom examination: - pelvic examination may show normal anatomy - *decreased pudendal nerve sensation* investigative studies: - urinalysis and culture usually normal; may show infection - cystometric studies show markedly increased residual volume - involuntary detrusor muscle contractions do NOT occur management: - intermittent self-catheterization may be necessary - discontinue the offending systemic medications - bladder contraction stimulation (alpha receptor blocker; cholinergic drugs)
question
What is the triad for hypotonic bladder?
answer
involuntary loss of urine detrusor muscle not contracted urine loss day + night
question
Types of urinary incontinence with irregular detrusor muscle contractions
answer
Hypertonic incontinence
question
Types of urinary incontinence with no involuntary detrusor muscle contractions
answer
Stress incontinence Hypotonic incontinence
question
Fistula incontinence: etiology, history, examination, investigative studies, management
answer
etiology: - normal urethral-bladder mechanism is intact - bypassed by urine leaking out through a fistula from urinary tract history: - *radical pelvic surgery* or *pelvic radiation therapy* - loss of urine occurs continually in small amounts - day + night examination: - normal anatomy and normal neurologic findings investigative studies: - urinalysis and culture are normal - IVP (intravenous pyelogram) will demonstrate dye leakage from urinary tract fistula management: - surgical repair of the fistula
question
Triad for bypass incontinence
answer
involuntary loss of urine history: radical pelvic surgery or radiation urine loss day + night continuously* (small amounts)
question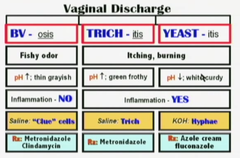
Vaginal discharge: BV, parasitic, yeast
answer
BV; bacterial vaginosis (most common) - fishy odor - pH↑; thin grayish exudate - no inflammation; endogenous transmission - diagnostic: clue cells - Rx: metronidazole; clindamycin Trichomonas vaginalis - itching, burning "strawberry cervix" - inflammation prominent; pH↑ - green/yellowish frothy discharge - Methylene blue wet mount; mobile flagellates - Rx: Metronidazole Candida albicans - itching, burning - inflammation not as prominent as Trichomonas vaginalis; white "cottage cheese" discharge - pH stays same or ↓ - KOH: pseudohyphae/hyphae - Rx: fluconazole; azole cream Note: metronidazole is safe to use in all trimesters of pregnancy; class B
question
Most common cause of vagina discharge? 2nd? 3rd?
answer
Bacterial vaginosis (50%) Candidiasis (30%) Trichomonas (15%)...STD's
question
What is the predominant bacteria in the vagina?
answer
Lactobacillus Normal flora (70%) in BV it decreases to 15%
question
What is the normal pH of the vagina?
answer
pH < 4.5 estrogen dominance
question
Diagnostic Test: Vaginal Discharge
answer
Visual inspection: the vulva and vagina should be examined for evidence of inflammatory response; check vaginal discharge on speculum Vaginal pH: normal <4.5 Microscopic examination 2 drops of vaginal discharge are placed on glass slide (saline on one side, KOH on the other) looking for clue cells, hyphae, flagellates, WBC's
question
What is a positive "whiff" test in BV?
answer
when KOH is placed on the discharge, releasing a fishy odor KOH is for Candida albicans diagnostics; but it dissolves tissue
question
How does BV most commonly present as?
answer
asymptomatic 50%
question
Rx: Bacterial vaginosis
answer
Metronidazole - safe to use in all 3 trimesters of pregnancy - 250mg - t.i.d. for 7 days - no alcohol for 24-48 hrs Clindamycin - 300mg - b.i.d. for 7 days
question
Trimethylamineuria
answer
Fish odor syndrome AR a rare clinical entity where the patient has an offensive persistent odor that no amount of bathing can correct differential diagnosis with BV
question
What is associated with bubbly vaginal discharge?
answer
Trichomonas vaginalis
question
Trichomoniasis: Men vs. Woman symptoms
answer
Men: 90% asymptomatic Woman: 50% asymptomatic Both needs treatment despite presentations
question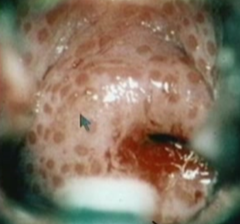
What is associated with strawberry cervix?
answer
Trichomonas vaginalis
question
Rx: Vaginal Trichomoniasis
answer
Metronidazole - 24~48hrs no liquor - recommended: 2g orally in a single dose - alternative: 500mg b.i.d for 7 days - pregnancy: 2g orally in a single dose
question
Rx: Vaginal Candidiasis
answer
Oral fluconazole - 150mg single dose azole cream
question
Physiologic discharge: Sx, risk factors, speculum exam, management
answer
Sx: - most common complaint is increased watery vaginal discharge - no burning or itching Speculum: - columnar epithelium of endocervical canal extends over a wide area of the ectocervix, producing abundant mucus discharge - thin and watery - pH is normal (<4.5) Risk factors: - chronic anovulatory conditions - PCOS, etc. (polycystic ovarian syndrome) Management: - steroid contraception with progestins - convert watery thin discharge into thick sticky progestin-dominant mucus
question
Most common symptom of benign/malignant vulvar lesions
answer
Vulvar itching
question
Premalignant vulvar dermatosis
answer
benign lesions with malignant predisposition - most common symptom is vulvar itching, most lesions are asymptomatic Diseases: - Squamous hyperplasia - Lichen sclerosis - Squamous dysplasia - CIS
question
Squamous hyperplasia : appearance, palpation, histology, management
answer
premalignant vulvar dermatosis Appearance: - lesions appear whitish focal or diffuse areas Palpation: - firm and cartilaginous on palpation Histologically: - thickened keratin - epithelial proliferation Management: - fluorinated corticosteroid cream
question
Lichen sclerosis: appearance, palpation, histology, management
answer
premalignant vulvar dermatosis Appearance: - lesions are bluish-white papula that can coalesce into white plaques Palpation: - thin and parchment-like Histology: - epithelial thinning Management: - Clobetasol cream
question
Vulvar squamous dysplasia: appearance, histology, management
answer
premalignant vulvar dermatosis Appearance: - lesions are white, red, or pigmented, often multifocal in location - almost identical to cervical dysplasia Histology: - cellular atypia restricted to the epithelium without breaking through the basement membrane Management: - surgical excision
question
CIS: appearance, histology, management
answer
premalignant vulvar dermatosis Appearance: - indistinguishable from vulvar dysplasia - white, red, or pigmented, often multifocal lesions Histology: - cellular atypia is full thickness but does not penetrate the basement membrane Management: - laser vaporization and vulvar wide local excision
question
Malignant vulvar lesions
answer
uncommon gynecologic malignancy (4th most common gynecologic malignancy) mean age 65 risk factors: old age, cigarette smoking, HIV, premalignant vulvar dermatosis Diseases: - squamous cell - melanoma - Paget disease
question
Squamous cell (malignant vulvar lesion)
answer
most common type of invasive vulvar cancer (90%) association with HPV Pathogenesis is chronic inflammation (for older woman) and HPV infection (for younger women) Most common stage at diagnosis is Stage 1
question
Melanoma (malignant vulvar lesion)
answer
second most common histologic type of vulvar cancer (5%) most important prognostic factor is the depth of invasion Any dark or black lesion in vulva should be biopsied and considered for melanoma
question
Paget disease (malignant vulvar lesion)
answer
Characteristics: - red lesion - most common in postmenopausal white women Any patient with red vulvar lesion must be considered for the possibility of Paget disease Most common form of Paget disease is intraepithelial process 18~20% of cases invasion of basement membrane is identified association with other cancers (mainly GI, urinary, and breast)
question
Malignant vulvar lesions: diagnosis
answer
Biopsy
question
Malignant vulvar lesions: pattern of spread
answer
starts with local growth and extension that embolizes to inguinal lymph nodes and finally, hemtogenous spread to distant sites
question
Malignant vulvar lesions: staging
answer
Staging is surgical Stage 0: CIS (basement membrane is intact) Stage I: - tumor confined to vulva with size </= 2cm - nodes not palpable Stage IA: invasion 1mm deep Stage II: - tumor confined to the vulva with size >2cm - nodes not palpable Stage III: - Tumor any size with spread to lower urethra, vagina, or anus - unilateral nodes Stage IV: widespread metastasis Stage IVA: involves upper urethra, bladder or rectum, pelvic bone, bilateral nodes Stage IVB: distant metastasis
question
Malignant vulvar lesions: management
answer
1) Wide local excision 2) Modified radical vulvectomy 3) Radical vulvectomy 4) Pelvic exenteration 5) Radiation therapy
question
Management for stage IA malignant vulvar lesions
answer
Wide local excision only
question
Malignant vulvar lesions management: wide local excision
answer
Stage IA only risk of metastasis is negligible No lymphadenectomy is needed
question
Malignant vulvar lesions management: Modified radical vulvectomy
answer
involves radical local excision - Ipsilateral inguinal dissection is used only if stage is IB and unifocal lesion > 1cm from midline AND no palpable nodes (less sexual morbidity) - Bilateral inguinal dissection is used if at least stage IB or a centrally located lesion OR palpable inguinal nodes or positive ipsilateral nodes (lower-extremity edema)
question
Malignant vulvar lesions management: radical vulvectomy
answer
involves removal of labia minora + majora, clitoris, perineum, perineal body, mons pubis seldom performed due to high morbidity sexual dysfunction may result
question
Malignant vulvar lesions management: pelvic exenteration
answer
radical vulvectomy + removal of cervix, vagina, ovaries + lower colon, rectum + bladder create appropriate stomas if necessary seldom indicated or performed due to high morbidity
question
Malignant vulvar lesions management: radiation therapy
answer
only used for patients who cannot undergo surgery
question
Benign vulvar lesions: diseases
answer
1) Mulluscom contagiosum 2) Condylomata acuminata 3) Bartholin cyst
question
Mulluscom contagiosum: at risk group, Sx, transmission, management
answer
Benign vulvar lesion Children, sexually active adults, immunodeficient patients Sx: - spontaneously regressing, umbilicated tumors of skin Transmission: - direct skin contact Management: - observation - curettage - cryotherapy
question
Condylomata acuminata: causative agent, Sx, management
answer
Benign vulvar lesions HPV 6, 11 (no malignant predisposition) Sx: - cauliflower-like vulvar lesions Management: - treat clinical lesions only
question
Bartholin cyst: pathogenesis, management
answer
Benign vulvar lesions obstruction of the Bartholins gland duct may occur due to infection (GC) After immune defenses overcome, duct remains obstructed resulting in cystic dilation of the gland aspiration of the cyst yields sterile fluid Management: - conservative unless pressure symptoms due to size
question
gynecologic cancer rankings 1~4 and age relevance
answer
1. endometrium (61) 2. ovaries (69) 3. cervix (45) 4. vulva (65)
question
What is the type of gynecological cancer occurs earliest in life? Oldest?
answer
Cervical cancer (45) Ovaries (69)
question
Cervical polyps: description, cause, at risk group, findings, management
answer
Description: fingerlike growths that start on the surface of the cervix or originate within endocervical canal/columnar epithelium (more common), can extend out of the cervical os. Cause: - Idiopathic - Associated with chronic inflammation - Associated with increased levels of estrogen (ex: pregnancy) - Associated with thrombosed cervical blood vessels At risk group: - relatively common - older multiparous women more common Findings: - vaginal bleeding, often after intercourse - bleeding occurs between normal menstrual periods - speculum examination: smooth, red/purple, fingerlike projections from cervical canal - biopsy typically reveals mildly atypical cells and signs of infection Management: - polyps can be removed by gentle twisting or by surgical string removal method (electrocautery/laser) - due to infected polyps being common, antibiotic may be given after the removal even if there are no or few signs of infection - although most polyps are benign, pathology exam of biopsy should still be done - regrowth of polyps is uncommon
question
What are cervical polyps associated with?
answer
Associations: - chronic inflammation - increased estrogen levels (pregnancy, etc.) - thrombosed cervical blood vessels - idiopathic
question
What do people with cervical polyps most commonly present with?
answer
vaginal bleeding, mostly after intercourse bleeding between normal menstrual cycles
question
What is the management of cervical polyps?
answer
polyps can be removed by gentle twisting or by surgical string removal method - electrocautery - laser antibiotics given after procedure due to common association of polyps with infection biopsy sent to pathology regardless of nature of polyps
question
Which group of people are at risk for developing cervical polyps?
answer
older women multiparous women
question
Nabothian cysts: description, cause, findings, management
answer
Description: mucus-filled cyst on the surface of the uterine cervix. These endocervical glands can become *covered* by squamous epithelium through metaplasia. Cause: - during the metaplasia and formation of the T-zone, columnar epithelium morphs into squamous epithelium; if the columnar cells beneath did not completely go through metaplasia, they can secrete mucus which can push the squamous epithelium outwards. Findings: - benign condition; rarely large enough to cause clinically relevant problems - pelvic examination reveals small, smooth, rounded lump (or collection of bumps) - rarely, colposcopic exam can be used to distinguish nabothian cysts from other types of cervical lesions Management: - no treatment necessary - Nabothian cysts do not clear spontaneously - Easily cured through electrocautery or cryotherapy
question
The cervical canal is lined by what type of cells? Function?
answer
Glandular cells / columnar epithelium secrete mucus
question
What does the Nabothian cyst present as? How do you treat it?
answer
small, smooth, rounded lump or collection of bumps caused by mucus-fileld cysts on the surface of the cervix (ectocervix) due to incomplete metaplasia of columnar epithelium beneath the T-zone during transformation benign condition No treatment necessary - electrocautery or cryotherapy can easily cure cyst
question
Cervicitis: symptoms, examination, investigative findings, management
answer
Symptoms: - no symptoms most common - vaginal discharge Examination: - most common finding is mucopurulent cervical discharge - friable cervix: endocervical bleeding easily induced by cotton swab palpation of cervical os - No pelvic tenderness noted - Patient is afebrile Investigative findings: DNA probe - Routine cervical cultures are positive for chlamydia or gonorrhea - STDs - WBC and ESR normal (no inflammation) Management: - Oral azithromycin in single dose - Oral doxycycline BID for 7 days
question
What is the most common finding in cervicitis?
answer
mucopurulent discharge from cervix friable cervix no pelvic tenderness or febrile condition
question
How do you manage cervicitis?
answer
Oral azithromycin single dose or Oral doxycycline BID for 7 days
question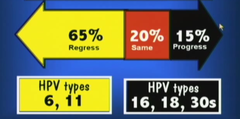
Cervical neoplasia: presentation, etiology, risk factors
answer
Presentation: - usually asymptomatic - progression from premalignant to invasive cancer has been reported to be approximately 8~10 yrs (good prognosis for early detection and slow progression) - Most regress (young women) Etiology: - most common* etiology of cervical cancer is HPV - Over 75 subtypes - most common HPV types: 16, 18, 31, 33, 35, 45 - most common for condyloma accuminata: 6, 11 risk factors: - early age intercourse - multiple sexual partners* (strong positive correlation) - cigarette smoking - immunosuppression
question
What is the most common presentation of cervical cancer? What is the most common progression? Associated age groups and types?
answer
most common presentation is asymptomatic progression is most commonly regression, especially in young women - age 14~19 has 33% HPV risk - age 20~29 has 28% HPV risk 65% regress, associated with HPV 6, 11 - young women most commonly regress, 61% within 1 yr, and 91% within 3 years 20% same + 15% progress - associated with HPV 16, 18, 30s
question
What are the risk factors for developing cervical cancer?
answer
early age of intercourse cigarette smoking multiple sex partners immunosuppression
question
What are the most common HPV types for cervical cancer? Order of malignancy? Condyloma accuminata?
answer
CIN: HPV-16, 18, 31, 33, 35, 45 (16>18>45>31>33) Condyloma accuminata: HPV-6, 11
question
What is the most effective medically cancer screening test ever developed?
answer
PAP smear 70~80% decrease of death rate
question
Which HPV is most associated with squamous cell carcinoma of cervix?
answer
HPV-16
question
Which HPV is most associated with adenocarcinoma of the cervix?
answer
HPV-18
question
Rank the most common malignant HPV types that causes cancer in the cervix + association
answer
HPV-16 (squamo)....59% HPV-18 (adeno)....12% HPV-45>31>33....squamo
question
Why do we NOT start PAP smear before age of 21?
answer
Most cases of HPV infection regresses (65%) More so, most cases of HPV infection in young woman regresses completely in 3 years (91%) HPV infection is correlated with sexual intercourse at young age if HPV is going to regress mostly in 3 years there isn't a point of starting PAP smears until after 21yrs old
question
When doing a Pap smear on pregnant women what should you use?
answer
spatula for T-zone *cotton swab for endocervical canal
question
Pap smear should be started at the following ages:
answer
Age < 21: - NO Pap test or screening for HPV, regardless of sexual activity Age 21: start Pap test with cytology alone *without HPV testing; the recommendation is the same whether HPV vaccinated or not
question
What is the frequency of recommended Pap smear for Age groups 21-29? 30-65?
answer
Age 21-29: - repeat Pap every 3 years with cytology alone; do not perform HPV testing in this age group (due to slow progression of the disease) Age 30-65: - Pap every 3 years with cytology but no HPV testing OR - repeat Pap every 5 years if both cytology + HPV (recommended choice)
question
When should Pap smears be discontinued?
answer
After age 65 - if negative cytology and/or HPV tests for past 10 years AND no history of CIN-2, 3, or cervical carcinoma Any age if total hysterectomy and no history of CIN
question
What is the system used to classify Pap smears in the U.S.?
answer
Bethesda system
question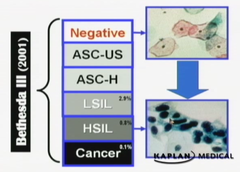
Classification os Bethesda system
answer
Negative: No intraepithelial lesions - may report trichomoniasis, candida, BV, HSV, atrophy, etc. Abnormal squamous cells (99% of abnormal Pap smears) ASCUS: (5%~20%) - atypical squamous cells of undetermined significance - suggestive of LSIL but not adequate - decrease ASCUS findings by making a thinner prep ASCH: - atypical squamous cells can't rule out HSIL - suggestive of but not adequate to label HSIL LSIL: - low-grade squamous intraepithelial lesion - biopsy is expected to show histologic findings of HPV, mild dysplasia, or CIN 1 HSIL: - high-grade squamous intraepithelial lesion - biopsy is expected to show histologic findings of moderate-severe dysplasia, CIN 2, 3, CIS Squamous cell carcinoma: - biopsy expected to show histologic findings of invasive cancer Abnormal endocervical cells (1% of abnormal Pap smears) AGC-NOS: - atypical glandular cells, not otherwise specified AGC-neoplastic: - atypical glandular cells, can't rule out neoplasia - changes suggestive of but not adequate to call AIS or cancer AIS: - adenocarcinoma in situ Adenocarcinoma
question
Describe ASCH on Bethesda system
answer
atypical squamous cells can't rule out HSIL - changes suggestive of but not adequate to label HSIL
question
Describe ASCUS on Bethesda system
answer
atypical squamous cells of undetermined significance - changes suggestive of but not adequate to label LSIL
question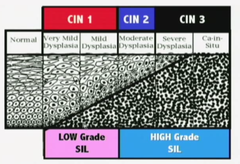
Describe LSIL on Bethesda system
answer
low-grade squamous intraepithelial lesion - biopsy is expected to show histologic findings of HPV, mild dysplasia, CIN1
question
Describe HSIL on Bethesda system
answer
high-grade squamous intraepithelial lesion - biopsy is expected to show histologic findings moderate-severe dysplasia, CIN2, CIN3, CIS
question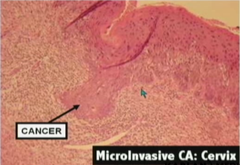
Squamous cell carcinoma on Bethesda system
answer
Invasive carcinoma will enter staging instead of CIN numbers Stage 1 is after CIS - <2cm lesion (1a = 1mm deep lesion)
question
Describe AGC-NOS on Bethesda system
answer
atypical glandular cells not otherwise specified
question
Describe AGC-neoplastic on Bethesda system
answer
atypical glandular cells can't rule out neoplasia
question
Describe AIS on Bethesda system
answer
adenocarcinoma in situ
question
High-grade squamous intraepithelial lesions are associated with which histologic findings?
answer
moderate-severe dysplasia CIN-2 CIN-3 CIS
question
Low-grade squamous intraepithelial lesions are associated with which histologic findings?
answer
mild dysplasia HPV CIN 1
question
How often does ASCUS show up on Pap smears? How do you decrease ASCUS diagnosis? What is the management of ASCUS?

answer
<5% but up to 20% Decrease ASCUS findings by: - make a thinner prep or HPV/DNA typing: - if 6, 11 it will most likely regress (low-risk) but repeat Pap within 1 year - if 16, 18, 30s it is high-risk and need colposcopy and biopsy
question
If you find ASCUS on Pap smear, what are the tests you could run? (3)
answer
Accelerate repeat Pap: - 4~6 month intervals until 2 consecutive negative Paps - if a repeat Pap is again ASCUS or worse, this is an indication for colposcopy HPV-DNA testing: - if liquid-based cytology was used on initial Pap smear, it can be used for DNA testing (100% diagnostic) - indications for colposcopy: high-risk HPV types Colposcopy: - uses acetic acid to make vascular patterns more visible - 10~12 times magnification - satisfactory/non-satisfactory - unsatisfactory = t-zone invading into endocervical canal
question
What if you find cells other than ASCUS on a Pap smear, what tests should you run?
answer
Colposcopy and biopsy
question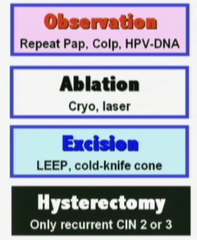
If you find cells others than ASCUS (ASC-H, LSIL, etc.) on a Pap smear, what is your plan of management?
answer
Colposcopy Endocervical curettage (ECC) - not in pregnancy - ***colposcopy shows T-zone extending into endocervical canal, etc. Ectocervical biopsy - lesions identified on ectocervix by colposcopy*** - mosaicism, punctation, white lesions, abnormal vessels - biopsy and send for histology Compare Pap smear and biopsy - ensure level of severity is comparable with colposcopy - *Pap smear should not be worse than biopsy; means you missed the more malignant area on biopsy Diagnostic Cone biopsy indications: - Pap smear is worse than biopsy - ECC: abnormal cells - Lesions entering endocervical canal*** - Biopsy: microinvasive carcinoma Manage by histology: - observation: CIN1, repeat Pap in 6~12 months, colposcopy and repeat Pap in 12 months, or HPV/DNA testing in 12 months - ablation: CIN1, 2, 3 (cryotherapy, laser vaporization, electrofulguration) - resection: CIN1, 2, 3 (LEEP, cold-knife conization) - hysterectomy: biopsy-confirmed, recurrent CIN2 or 3 only
question
What are the risk of cone biopsy?
answer
incompetent cervix cervical stenosis
question
When Pap smear shows worse dysplasia than ASCUS, you use colposcopy examination and you see metaplastic epithelium entering the endocervical canal, what will you do next?
answer
ECC endocervical canal curettage
question
When Pap smear shows worse dysplasia than ASCUS, you use colposcopy examination and you see ectocervical lesions, what will you do next?
answer
Ectocervical biopsy
question
When Pap smear shows worse dysplasia than ASCUS, you use colposcopy examination and you see lesions entering the endocervical canal, what will you do next?
answer
Narrow cone biopsy
question
What are follow-up options for CIN1?
answer
Observation (repeat Pap, colposcopy and Pap, HPV-DNA) Ablative therapy (cryotherapy, laser, electrofulguration) Excisional procedure (LEEP, cold-knife)
question
What are follow-up options for CIN2?
answer
Ablative therapy (cryotherapy, laser, electrofulguration) Excisional procedure (LEEP, cold-knife cone) Hysterectomy (recurrent CIN2 only)
question
What are follow-up options for CIN3?
answer
Ablative therapy (cryotherapy, laser, electrofulguration) Excisional procedure (LEEP, cold-knife cone) Hysterectomy (recurrent CIN3 only)
question
When is hysterectomy indicated in CIN?
answer
recurrent CIN2, 3
question
CIN follow-up management: Observation
answer
Indicated for CIN1 Repeat Pap in 6~12 months Colposcopy and repeat Pap in 12 months HPV-DNA testing in 12 months
question
CIN follow-up management: Ablative therapy
answer
Indicated for CIN1, 2, 3 Cryotherapy Laser vaporization Electrofulguration Follow-up: repeat Pap smears, colposcopy and Pap smear, or HPV-DNA testing every 4~6 months for 2 years
question
CIN follow-up management: Excision/Resection
answer
Indicated for CIN1, 2, 3 LEEP cold-knife conization Follow-up: repeat Pap smears, colposcopy and Pap smear, or HPV-DNA testing every 4~6 months for 2 years
question
CIN follow-up management: hysterectomy
answer
CIN2, 3 only indicated in recurrent infections
question
What follow-up procedures are required for ablative therapy and excisional procedure patients for CIN?
answer
Follow-up: repeat Pap smears, colposcopy and Pap smear, or HPV-DNA testing every 4~6 months for 2 years
question
If cytologic findings of Pap smear reveals HSIL, what is the next step for patients ages 25-64?
answer
colposcopy + biopsy immediate LEEP**
question
Invasive Cervical Cancer definition
answer
cervical neoplasia that has penetrated through the basement membrane >CIS
question
Cervical cancer: definition, presentation, epidemiology, diagnostic findings
answer
Definition: cervical neoplasia penetrated through the basement membrane Presentation: - normal menstrual cycles - postcoital vaginal bleeding - irregular vaginal bleeding - lower extremity pain and edema in advanced stages Epidemiology: - 3rd most common gynecological carcinoma - ~45 years of age (youngest occurrence) - 250,000 deaths/yr world wide; 10,000/yr in U.S. Diagnostic Tests/Findings: - Cervical biopsy* - Metastatic workup: pelvic examination, chest x-ray, intravenous pyelogram, cystoscopy, sigmoidoscopy - Imaging studies: invasive cervical cancer is the ONLY gynecological cancer staged clinically (CT and MRI cannot be used for clinical staging)
question
What is the only gynecological carcinoma that uses clinical staging?
answer
Cervical cancer
question
Common presentation of cervical carcinoma?
answer
normal menstrual cycle postcoital vaginal bleeding irregular vaginal bleeding
question
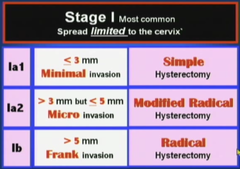
Cervical cancer: staging
answer
CLINICAL (only gynecological carcinoma staged clinically) Stage 0: CIS (basement membrane is intact) Stage I: Spread limited to the cervix. *most common* - Ia1: 3mm but 5mm deep (frank invasion) Stage II: spread adjacent to cervix - IIa: involves upper 2/3 of vagina - IIb: invasion of parametria Stage III: spread further from the cervix - IIIA: involves lower one third of vagina - IIIB: extends to pelvic side wall or hydronephrosis Stage IV: spread furthest from cervix - IVA: involves bladder or rectum or beyond true pelvis - IVB: Distant metastasis
question
What is the most common stage of cervical cancer?
answer
Stage 1 limited to the cervix
question
What is the staging for minimally invasive cervical cancer? Management? Management in pregnancy?
answer
Ia1 </= 3mm deep total simple hysterectomy during pregnancy: cone biopsy during pregnancy follow conservatively, deliver vaginally reevaluated and treated 2 months postpartum
question
What is the staging for microinvasive cervical cancer? Management? Management in pregnancy?
answer
Ia2 <3mm but </=5mm deep modified radical hysterectomy during pregnancy: cone biopsy during pregnancy follow conservatively, deliver vaginally reevaluated and treated 2 months postpartum
question
What is the staging for frank invasion cervical cancer? Management? Management in pregnancy?
answer
IB >5mm deep radical hysterectomy or radiation (IIa) during pregnancy: based on gestational age - before 24 weeks: receive definitive treatment as shown above - after 24 weeks: conservative management to 32-33 weeks, after C-section definitive treatment can be done
question
What ist he staging for cervical cancer that has spread adjacent to the cervix? Management? Management in pregnancy?
answer
II IIa: upper 2/3 of vagina involved Management: radical hysterectomy or radiation IIb: invasion of parametria Management IIb or above: radiation therapy and chemotherapy for all ages during pregnancy: based on gestational age - before 24 weeks: receive definitive treatment as shown above - after 24 weeks: conservative management to 32-33 weeks, after C-section definitive treatment can be done
question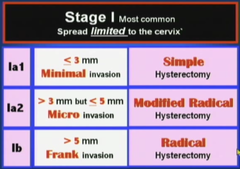
Cervical cancer: staging management
answer
Stage Ia1: - 3mm but 5mm frank invasion - IIa: involves upper 2/3 of vagina - radical hysterectomy with/without radiation Stage IIb, III, IV: - radiation therapy and chemotherapy for all ages
question
Cervical cancer: follow-up
answer
All patients with invasive cervical cancer should be followed up with... - Pap smear every 3 months for 2 years after treatment - then every 6 months for subsequent 3 years Patients who have local recurrence can be treated with radiation therapy Patients with distant metastases should be considered for chemotherapy treatment - Cisplatinum
question
What is the most active chemotherapeutic agent for cervical cancer?
answer
Cisplatinum
question
What is the effect of pregnancy in cervical neoplasia
answer
pregnancy does NOT predispose abnormal cytology and does not accelerate precancerous lesions progression
question
Diagnostic tests and findings for pregnant patients in cervical cancer
answer
Pregnant with abnormal Pap smear should be evaluated in the SAME FASHION - owing to increased cervical vascularity ECC is not performed during pregnancy (endocervical canal curettage)
question
What is the plan of management in pregnant patients with cervical cancer in CIN stages?
answer
Pap smear and colposcopy every 3 months during pregnancy 6~8 weeks postpartum the patient should be reevaluated with repeat colposcopy an dPap smear Any persistent lesions can be definitively treated postpartum
question
What is the plan of management for microinvasion cervical cancer in pregnant patients?
answer
evaluated with cone biopsy to ensure no rank invasion patients can be followed conservatively delivery can be vaginal reevaluation and treatment 2 months postpartum
question
What is the plan of management for frank invasion carcinoma in pregnant patients?
answer
Based on gestational age before 24 weeks - definitive treatment based on staging after 24 weeks - conservative management to about 32-33 weeks - C-section - definitive treatment after delivery
question
Gardasil: recommendation, coverage, regimen
answer
Recommendation: - females 8~26; target group 11~12yrs - Efficacy is highest before patient's immune system is exposed to HPV - No point in testing for HPV before vaccination, no easy method of identifying all HPV types - Pap smear continued to guidelines due to >70 types of HPV strains and vaccine covers only 4 most common - sexually active women can receive vaccine, same with women who has previous abnormal cervical cytology or genital warts, just less effective - patients with previous CIN, benefits limited - not recommended for pregnant, lactating, or immunosuppressed women, but no tests has been done to prove clinical relevant harm Coverage: - HPV 6, 11, 16, 18 - covers 70% of cervical cancer and 90% of genital warts of HPV strains Regimen: - initial, 2 months, 6 months - $300
question
What is the target group for Gardasil? Why?
answer
11~12 age group Efficacy best before host immune system is exposed to HPV strains
question
What strains of HPV does Gardasil cover?
answer
HPV 6, 11, 16, 18
question
When is the Gardasil vaccine contraindicated?
answer
Pregnant women Lactating women Immunosuppressed women Not clinically proven to be true
question
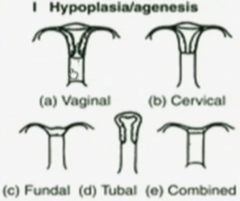
How many types of uterine anomalies are there? How are they divided?
answer
7 types by the American Fertility Society (1988) Divided by - failure to form - failure to fuse - failure to dissolve the septum
question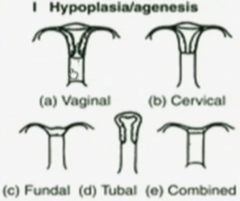
Hypoplasia/Agenesis of Uterus: description, cause, association
answer
description: - may lack a vagina, cervix, fallopian tubes, body of uterus - developmental problem with a section of both mullerian ducts association - urinary tract anomalies - urinary tract embryologically lie close to mullerian ducts
question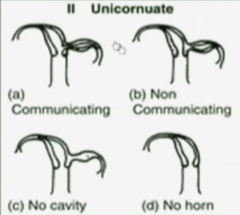
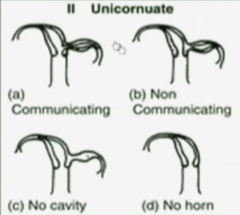
Unicornuate uterus: defect, description, complications, symptoms
answer
defect and description: - when ONE of the mullerian ducts fails to form - *sing-horn (banana-shaped) uterus develops from the remainder healthy mullerian duct - single uterus may stand alone complications: - 65% of women with unicornuate uterus, the defected mullerian duct may form an incomplete rudimentary horn - may or may not have cavity in the rudimentary horn but the opening that communicates with the healthy uterus is either small or nonexistent symptoms: if rudimentary horn forms - monthly pain during adolescence because no outlet for menses from rudimentary horn - risk of pregnancy in rudimentary horn, 90% ruptures due to anatomical limitations
question
Didelphys uterus: defect, description, risks

answer
defect and description: - results from complete failure of the 2 mullerian ducts to fuse together (stage 1 development) - each duct develops into a separate uterus - each uterus can have their own cervix or share a cervix - 67% of cases is associated with 2 vaginas separated by a thin wall risks: - preterm delivery is common
question
Bicornuate uterus: defects, description, types, risks

answer
defect and description: - most common congenital uterine anomaly (45%) - results from failure of fusion between the mullerian ducts at the fundus - 'complete' failure to fuse results in 2 separate single-horn uterine bodies sharing 1 cervix* - 'partial' failure to fuse results in fusion at the bottom but not the fundus causing single uterine cavity with 2 distinct horns on top and a shared cervix* Risks: - preterm delivery - malpresentations with pregnancy
question
What is the most common congenital uterine anomaly?
answer
Bicornuate uterus 45%
question
Septate uterus: defect, description, types, risks

answer
defect and description: - failure in degeneration of the median septum - complete failure: 2 single-horned uteri that share one cervix - partial failure: shared cavity at lower portion of uterus with 1 cervix - *external shape of uterus is normal-appearing* risks: - preterm delivery
question
Septate uterus vs. Bicornuate uterus
answer
septate uterus looks normal-appearing single unit exteriorly bicornuate uterus has distinct 2 separate horns at fundus both can result in separate cavity but sharing 1 cervix or partial shared cavity with 1 cervix
question
Arcuate uterus: defect, description, risks

answer
defect and description: - essentially NORMAL in shape - NORMAL in function as well - small midline indentation in the uterine fundus, results from failure to dissolve the median septum completely risks: - essentially none
question
DES uterus: defect, description, cause, risks

answer
defect and description: - *T-shaped cavity - mothers exposed to DES (diethylstilbestrol) which was used 30yrs ago to prevent miscarriages are predisposed to uterine abnormalities and clear cell carcinoma of the vagina, idiopathic risks: - cervical insufficiency
question
What teratogen is associated with predisposition of clear cell carcinoma of the vagina?
answer
DES (diethylstilbestrol) DES uterus + clear cell carcinoma of vagina idiopathic
question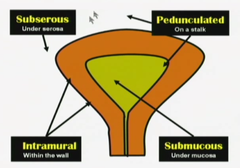
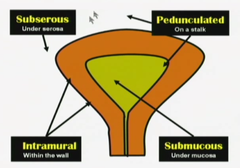
Leiomyoma Uteri: description, at risk group, different locations
answer
Description: benign smooth muscle growth of myometrium causing non-tender asymmetric distortions of the uterus; most common benign uterine tumor At risk group: 5x more common in black women than white women Location: Intramural: - most common location is within uterine wall - asymptomatic and cannot be felt on examination unless enlargement of uterus is altering external contour Submucosal: - located beneath the endometrium and can distort the uterine cavity - since endometrium may not respond appropriately to normal hormonal fluctuation the result is unpredictable, often intermenstrual, bleeding* - *most common symptom is vaginal bleeding and can result in anemia Subserosal: - located beneath uterine serosa; they can distort the external contour of the uterus - pedunculated subserosal leiomyomas can become parasitic fibroids - they break away from uterus and receive their blood supply form another abdominal organ
question
Leiomyoma uteri: natural history
answer
Natural history: - slow growth*: most leiomyomas are small, grow slowly and cause no symptoms - rapid growth: estrogen receptors are increased in leiomyomas resulting in rapid enlargement during times of high estrogen levels, such as pregnancy - degeneration: during rapid growth, myomas may outgrow their blood supply, resulting in ischemic degeneration of a fibroid (hyaline, calcific, red degeneration/carneous degeneration) - Shrinkage: when estrogen levels fall, leiomyomas will typically decrease in size; physiologically (menopause) or through treatment (GnRH agonist suppression of FSH)
question
How does most leiomyomas present clinically?
answer
Slow growth small, grow slowly, and asymptomatic
question
What is the most common form of leiomyoma of uterus?
answer
Intramural leiomyoma found within the uterine wall
question
What is the most common presentation of a submucosal leiomyoma of the uterus?
answer
vaginal bleeding metrorrhagia = irregular bleeding between menses menorrhagia = heavy menses
question
Which type of uterine leiomyoma can become parasitic fibroids?
answer
Pedunculated subserosal uterine leiomyoma Break away from uterus and receive blood supply from another organ in the abdomen
question
Where is the intramural leiomyoma of the uterus found? How does it present?
answer
Most common location of leiomyoma uteri Found within the wall of the uterus Mostly asymptomatic and cannot be felt on examination unless it enlarges to where the normal uterine external contour is altered
question
Where is the submucosal leiomyoma of the uterus found? How does it present?
answer
It is found beneath the endometrium and can distort the uterine cavity It can be pedunculated and extend into the vagina through the cervix Due to overlying endometrium may not respond appropriately to the normal hormonal fluctuations, it results in unpredictable and often intermenstrual bleeding - menorrhagia - metrorrhagia - menometrorrhagia = combined of irregular bleeding between menses and heavy menses Most common presentation is vaginal bleeding
question
Where is the subserosal leiomyoma of the uterus found? How does it present?
answer
It is found beneath the uterine serosa They can distort the external contour of the uterus causing firm, nontender asymmetry Pedunculated subserosal leiomyomas can break away from uterus and form parasitic fibroids receiving blood supply from another organ
question
What are the top causes of uterine enlargement?
answer
1. pregnancy 2. leiomyoma 3. adenomyosis 4. leiomyosarcoma (extremely rare)
question
What is the cause of leiomyoma uteri degeneration? What are the types? Presentations?
answer
Sometimes the leiomyoma outgrows its blood supply and can result in ischemic infarction causing degeneration hyaline, calcified, red degeneration Red degeneration is also called carneous degeneration - cause extreme, acute pain - morphine and narcotics required - this is most common during pregnancy
question
What is the most common type of degeneration of uterine leiomyoma during pregnancy?
answer
Red degeneration
question
When does uterine leiomyoma present with rapid growth?
answer
estrogen receptors are increased in leiomyomas resulting in rapid enlargement during times of high estrogen levels example: pregnancy
question
Leiomyoma uteri: management
answer
Observation: - most leiomyomas can be managed conservatively and followed expectantly with regular pelvic examinations Presurgical shrinkage: - 3~6 months GnRH analog therapy; leuprolide/Lupron - adjuvant to surgical removal - reduction in size up to 60%~70% - decrease in blood loss in myomectomy - makes vaginal hysterectomy possible Myomectomy: - removal of myoma - maintains fertility - laparoscopic or laparotomy - future deliveries through cesarean section Embolization: - catheter placed into vessels supplying myoma - microspheres are injected, causing ischemia and necrosis of myoma - ~10% mortality rate (wrong vessel; uterine necrosis) Hysterectomy: - definitive therapy
question
How can you shrink a uterine leiomyoma before surgery? Purpose?
answer
3~6 months of GnRH (gonadotropin releasing hormone) analog therapy; Lupron (leuprolide) Results in 60%~70% shrinkage in size Not used for definitive cure, due to stoppage of leuprolide can cause regrowth of leiomyoma Mostly used as an adjuvant to surgical removal of myoma; decreases blood loss in myomectomy the decrease in size can also result in vaginal hysterectomy instead of abdominal hysterectomy
question
Uterine leiomyoma: diagnosis methods
answer
Diagnosis: Pelvic examination: enlarged, asymmetric, non-tender uterus in teh absence of pregnancy most common - 20wks gestation size = uterus reaching umbilicus (belly button) - 12wks gestation size = uterus reaching pubis symphysis Sonography: ultrasound, saline infusion sonography is helpful for identifying submucosal myomas Hysteroscopy Histology is only confirmed through surgical confirmation of excised tissue
question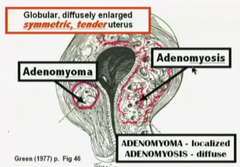
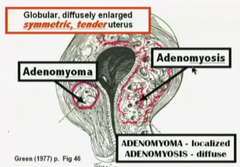
Adenomyosis: definition, presentation, diagnosis, Sx, examination, imaging, management
answer
Definition: ectopic endometrial glands and stroma are located within the myometrium of the uterine wall Presentation: - most common presentation is diffuse involvement of the myometrium - adenomyoma is termed for focal involvement, surrounded by a pseudocapsule Diagnosis: - enlarged, symmetric, tender uterus in teh absence of pregnancy - definitive diagnosis is by histologic confirmation of the surgically excised tissue Sx: - mostly asymptomatic - most common symptoms are secondary dysmenorrhea and menorrhagia Examination: - uterus is globular and up to 2~3x normal size - tenderness is most common immediately before and during menses Imaging: - ultrasound - MRI - *cystic areas found within the myometrial wall Management: - surgery is the definitive treatment - LNG-IUS (levonorgestrel intrauterine system may decrease heavy menstrual bleeding)
question
Primary dysmenorrhea findings
answer
onset 2~3yrs after menarche menarche = 11~16.5 yrs
question
What is the most common presentation of adenomyosis? Otherwise?
answer
Most common is diffuse involvement resulting in symmetric, soft, tender enlargement of the uterus When it becomes focalized and surrounded by a pseudocapsule, it is called adenomyoma
question
What is the most common symptoms of adenomyosis?
answer
mostly asymptomatic most common symptomatic presentation is - menorrhagia - 2° dysmenorrhea
question
When does tenderness most likely occur in patients with adenomyosis?
answer
most common immediately before and during menses
question
What is the most likely diagnosis upon seeing cystic areas found within the myometrial wall and the uterus is symmetrically enlarged?
answer
Adenomyosis
question
What is the management for adenomyosis?
answer
LNG-IUS - levonorgestrel intrauterine system - T-shaped intrauterine device that secretes progesterone into the uterine cavity - decreases heavy menstrual bleeding Surgery - hysterectomy is the definitive treatment
question
Define menopause
answer
3 continuous months of cessation of menses and elevated gonadotropins ~52 years old
question
What is the most common cause of postmenopausal bleeding?
answer
vaginal or endometrial atrophy
question
BMI range
answer
formula = kg/m² 40: obesity class 3 (very severely obese)
question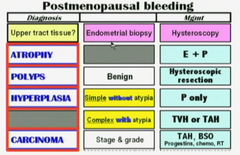
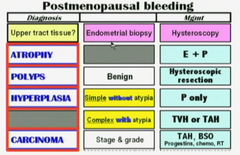
Synopsis: Postmenopausal bleeding steps of diagnosis and management
answer
Speculum exam: rule out vaginal lesions and cervical lesions Once ruled out... obtaining upper tract tissue: - endometrial biopsy - hysteroscopy and ultrasonography - send biopsy to pathology If finding is... atrophy: - management is estrogen with progestin polyps: - benign - hysteroscopic resection hyperplasia: - simple *without atypia: progestin treatment - complex *with atypia: total vaginal or abdominal hysterectomy carcinoma: - stage & grade - total abdominal hysterectomy + bilateral salpingo-oophorectomy (TAH-BSO) + lymph node dissection - according to staging and necessary radiation + chemotherapy
question
Most common cause of endometrial carcinomas?
answer
upposed estrogen without the stabilizing effect of progesterone
question
What are the major risk factors of postmenopausal bleeding?
answer
Obesity***: increased peripheral conversion of androgen to estrogen due to increased adipose tissue hypertension, diabetes mellitus (both points towards obesity) nulliparity: no kids means no exposure to the long period of progesterone during pregnancy; equal to possible unopposed estrogen chronic anovulation conditions (PCOS, etc.): no ovulation means no progesterone
question
What are some the diagnostic tests to confirm cause of postmenopausal bleeding?
answer
Endometrial sampling: - sampling process may miss diagnosis due to localized growth in the endometrium - example: dilatation and curettage of endometrial misses a small section where neoplastic growth is occurring Hysteroscopy: - with hysteroscope, cervical or endometrial polyps can be identified as cause of postmenopausal bleeding Ultrasound: - ultrasonography can be used to measure the thickness of the lining of the endometrium (postmenopausal patients should be <5mm)
question
What is the endometrial lining stripe measurement supposed to be for postmenopausal women?
answer
<5mm Ultrasound
question
Endometrial cancer: staging
answer
Most common cause of gynecological cancer Staging is surgical Stage I: spread limited to the uterus (most common stage at diagnosis) - IA: limited to the endometrium or invasion *less than 1/2 of myometrium* - IB: invasion *more than 1/2 of myometrium* Stage II: extension to teh cervix but not outside the uterus Stage III: Spread adjacent to teh uterus - IIIA: invades serosa or adnexa or positive cytology - IIIB: invasion of vagina - IIIC: invasion of pelvic or para-aortic nodes Stage IV: Spread further from the uterus - IVA: involves bladder or rectum - IVB: distant metastasis
question
What is the management of atrophy of endometrium induced postmenopausal bleeding?
answer
hormone replacement therapy estrogen + progestin
question
Endometrial cancer: management
answer
Stages I~IV: TAH-BSO + lymph node resection - TAH: total abdominal hysterectomy - BSO: bilateral salpingo-oophorectomy After surgery: radiation and chemotherapy - Stage I: none - Stage II: radiation - Stage III + IV: radiation + chemotherapy
question
What is the management for endometrial hyperplasia? What is the most common cause?
answer
Unopposed estrogen can cause hyperplasia of endometrium Simple hyperplasia with no atypia: progestin Complex hyperplasia, no atypia: progestin Complex hyperplasia with atypia: hysterectomy or progestin for non-surgical candidates Endometrial carcinoma: staging + TAH/BSO
question
Which types of hyperplasia can be managed with progestin?
answer
simple hyperplasia with no atypia complex hyperplasia with no atypia
question
How does complex hyperplasia histologically present? Complex hyperplasia with atypia?
answer
decreased stroma with increased glandular tissue atypia will show misshapen nucleus, etc.
question
What are some prevention methods of postmenopausal bleeding? Reproductive age women bleeding? Dietary?
answer
postmenopausal patient: - estrogen replacement therapy with progestin reproductive age women: - most likely due to chronic anovulation (PCOS, etc.) - progestin treatment Dietary - soy: 30~40% reduction of endometrial cancer risk
question
Tamoxifen association with vaginal bleeding
answer
Tamoxifen is used for breast cancer prevention by its estrogen antagonistic effects on the breast However, it has estrogen agonist effects on the uterus It can induce hyperplasia and endometrial polyps
question
Embryologic origin of uterus
answer
Fusion of the 2 Mullerian ducts
question
When is transvaginal transducer ultrasound used? Transabdominal transducer?
answer
Transvaginal transducer: ("pie shaped image") - lower pelvic masses - not influenced by thickness of maternal abdominal wall Transabdominal transducer: - entire pelvis as well as abdomen imaging Ultrasound works best when adjacent tissues have differing echodensities, particularly fluid/tissue interfaces
question
Average age range of menarche? Thelarche?
answer
menarche: 10-16.5y thelarche: breast development; 8~11y
question
What is the average age for Tanner II stage of breast development? Presentation?
answer
Tanner II: Breast development - 8-13 yrs - Breast buds begin
question
ASCUS?
answer
Atypical Squamous Cells of Uncertain Significance misreadings on Pap smears due to mechanical errors (drying, etc.)
question
Major structures of the uterus (3)
answer
Corpus (body) - Cornu (uterus join with fallopian tubes) Isthmus Cervix
question
Describe satisfactory colposcopy vs. unsatisfactory colposcopy
answer
Satisfactory colposcopy 1. T-zone does NOT extend into the endocervical canal 2. No lesions visualized within T-zone Unsatisfactory is the opposite..
question
Tanner stages: Pubic Hair
answer
Male + Female Tanner I: None (prepubertal state) Tanner II: small amount of long, downy hair with slight pigmentation on the labia majora Tanner III: hair becomes more coarse and curly and begins to extend laterally Tanner IV: adult-like hair quality, extending across pubis but sparing medial thighs Tanner V: hair extends to medial surface of the thighs
question
What are the risks of cone biopsy? (3)
answer
1. incompetent cervix (cutting too much) 2. cervical stenosis (can cause amenorrhea) 3. preterm birth
question
Traditional Pap vs. Liquid-based Pap
answer
Traditional Pap: - spatula for ectocervix* - cyto-brush for endocervical canal* (rotating in 1 direction 360°) - both specimens are smeared onto a glass slide, fixed with formalin, then stained *Potential problems* - ASCUS (atypical squamous cells of uncertain significance) cannot be diagnosed - insufficient smearing, air-drying artifacts if process is delayed, mechanical problems makes traditional technique obsolete Liquid-based Pap: - cervical broom* to collect specimens (rotated 5 times in same direction) - broom is placed into "formalin" solution and rotated 10 times to release collected material - this method is more preferred vs. traditional Pap due to absence of mechanical errors - ASCUS can also be used for HPV-DNA typing
question
What is special about Tanner IV stage of breast development?
answer
Papilla and areola forms a 2' mound not contour with surrounding breast
question
LEEP (loop electrosurgical excision procedure) description, procedure, followup, risks
answer
A thin low-voltaged loop cuts out abnormal cervical tissue identified with colposcopy advantage: visual confirmation lesions have been removed; no anesthesia needed followup Pap smear every 3-6 months for 2 years to ensure dysplastic changes to not return long-term risks of LEEP include - cervical stenosis - cervical insufficiency
question
What type of blood supply do oviducts receive? From where?
answer
Dual blood supply* Receives blood from the uterine artery and ovarian artery
question
What is the average age range for Tanner V stage of breast development?
answer
Tanner V: Breast development - 12.5~18.5 yrs - development is complete
question
What does the ovarian stroma produce?
answer
androgen Important for libido after menopause
question
Dilation and Curettage (D&C) procedure
answer
under anesthesia examines histology of endometrial lesions similar to endometrial biopsy; dilation of cervix is required to introduce curette can collect large amounts of endometrial tissue (>endometrial biopsy)
question
What are the 4 segments of the oviducts?
answer
Proximal → Distal "INTERcourse IS AMP and FUN" 1. Interstitium 2. Isthmus 3. Ampulla 4. Infundibulum
question
American Cancer Society recommendations
answer
1. initial study at age 34 if there are risk factors (breast cancer in first degree relative, BRCA genes, etc.) 2. routine screening at age 40 if there are no risk factors
question
Explain the formation of the T-zone
answer
at puberty the vaginal pH falls (due to estrogen dominance) the "native" columnar epithelium goes through metaplasia and becomes the transformation zone; normal-appearing "metaplastic" stratified squamous epithelium Old→New squamocolumnar junction (outer-to-inner)
question
Procedure associated with assessment of Asherman's syndrome
answer
HSG hysterosalpingogram
question
Cryotherapy description, procedure, followup, risks
answer
Destroys dysplastic cervical tissue identified by colposcopy and cervical biopsy; no anesthesia needed Cryo probe at -50℃ with liquid nitrogen Freeze and destroy tissue; 3 minutes intervals of freezing Watery discharge will occur over next few weeks as destroyed tissue sloughs off Followup Pap smears every 3-6 months for 2 years; disadvantage of not knowing if lesions are destroyed until followups Risks: cervical stenosis
question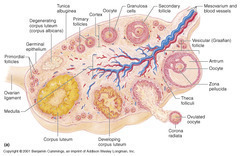
Phases of development: Folliculogenesis
answer
Primordial: - dormant, small - 1 layer of flat granulosa cells Primary: - Mitotic cells - cuboidal granulosa cells Secondary: - Theca cells - Multiple layers of granulosa cells Tertiary: - Fully formed antrum Graafian (vesicular) follicle: - preovulatory follicle; fully mature
question
Tanner stages: Breast development
answer
Tanner I: no glandular tissue; areola follows skin contours of the chest (prepubertal) Tanner II: breast bud forms with small area of surrounding glandular tissue; areola beings to widen - 8-13yrs Tanner III: breast begins to become more elevated and extends beyond borders of areola; remains in contour with surrounding breast Tanner IV: increased breast size and elevation; areola and papilla form a secondary mound projecting from the contour of the surrounding breast Tanner V: adult size; areola returns to contour of the surrounding breast, with projecting central papilla (nipple) - 12.5-18.5yrs
question
Colposcopy description
answer
"binoculars into the vagina" 1. *visually* identify where abnormal Pap smear cells originated 2. biopsy that area to send for histologic diagnosis
question
Average length of a vagina
answer
8-9cm
question
What is the lymphatic drainage of the ovaries?
answer
Pelvic nodes Para-aortic nodes
question
What are the organ systems we need to consider involving pelvic pain/pelvic mass?
answer
GI (colons) Uterus Bladder
question
What is the most common anatomical position of the uterus?
answer
Anteverted (50%) mid-position (25%) retroverted (25%)
question
Endometrial biopsy
answer
examines histology of endometrial lesions hollow suction cannula is placed into uterine cavity and suction is applied; rotation of cannula before fixing with formalin
question
Which portion of the cervix is most concerned for scrapings during a Pap smear?
answer
Transformation zone (T-zone) - 95% of cervical dysplasia and cancer develops here - screening for squamous cell carcinoma (most common cancer of the cervix 80%) - area between old (outer, "O") squamocolumnar junction and new (inner) squamocolumnar junction
question
Risks of mammography
answer
high radiation (0.7 mSv) same as background radiation in 3 months 1 rad = 10 mSv
question
What is the specimens required for a Pap smear? What diseases are they mostly screening for?
answer
2 areas 1. T-zone of the ectocervix (squamous cell carcinoma; most common cancer of cervix 80%) 2. columnar epithelium of endocervical canal (adenocarcinoma; 2nd most common cancer of cervix 15%)
question
Hysterosalpingogram (HSG) description and procedure
answer
procedure performed without anesthesia, radio-opaque fluid injected at endocervical canal allowing assessment of uterine malformations and Asherman's syndrome dye is supposed to spill into pelvic cavity; non-spillage can be a sign of fallopian tube occlusion or blockage
question
Vulvar biopsy
answer
done with punch biopsy or scalpel performed under local anesthesia, histology of vulvar lesions
question
Hysterectomy types
answer
removal of uterus "hyster" root comes from the misled belief women are crazy because of their uterus 1. subtotal: removes only teh corpus, leaving cervix in place 2. total: removes both corpus and cervix of uterus (aka simple hysterectomy) 3. radical hysterectomy: performed for early stage CIN, involves removal of the uterus, cervix, and surrounding tissues, including cardinal ligaments, uterosacral ligaments, and the upper vagina (can involve removing lymph nodes depending on stages of CIN)
question
What is the term for the surgery of removing ovaries?
answer
removal of ovaries Salpingo-oophorectomy
question
Cone biopsy: wide-shallow cone vs. narrow-deep cone
answer
Cone biopsy; both procedures need anesthesia Wide-shallow cone: - performed if Pap smear shows changes more severe than the colposcopically directed biopsy Narrow-deep cone: - performed if a lesion extends from the exocervix into teh endocervical canal
question
The pelvic floor is made up of which diaphragms? What structures do they hold?
answer
Pelvic diaphragm: - levator ani (puborectalis, pubococcygeus, ileococcygeus) - coccygeus muscles Perineal membrane (urogenital diaphragm): - triangular sheet of dense fibromuscular tissue "anterior triangle" that spans the anterior half of the pelvic outlet - vagina and urethra pass through the perineal membrane
question
Most common cause of uterine prolapse?
answer
childbirth
question
Uterine prolapse classification
answer
Grade I: cervix descends half way to introitus Grade II: cervix descends to introitus Grade III: cervix extends outside the introitus Grade IV or procidentia: entire uterus, as well as the anterior and posterior vaginal walls, extends outside the introitus
question
What is procidentia?
answer
Grade IV Uterine prolapse entire uterus + anterior and posterior vaginal walls extends outside the introitus
question
Vaginal prolapse classification
answer
Cystocele (most common): anterior vaginal wall prolapse; contains the bladder Rectocele (2nd most common): posterior vaginal wall prolapse; contains the rectum Enterocele (3rd): rectouterine pouch/pouch of Douglas prolapse
question
What is the triad for rectocele diagnosis?
answer
1. postmenopausal woman 2. Posterior vaginal wall protrusion 3. Digitally assisted removal of stool "digital splitting"
question
Management of pelvic relaxation: non-surgical
answer
Non-surgical: - Kegel exercises (learning to control pubococcygeus muscle; "magazine for better sex"; kegel weights) - Estrogen replacement in postmenopausal women - Pessaries (mechanical method)
question
Management of pelvic relaxation: surgical
answer
Surgical: when conservative methods fail - vaginal hysterectomy (with vagina vault suspension) + anterior/posterior vaginal repair - anterior and posterior colporrhaphy: uses endopelvic fascia that supports bladder and rectum
question
Diagnosis of prolapse in pelvic relaxation is done how?
answer
Tell the patient to perform Valsalva in lithotomy position
question
Average age of menopause?
answer
51-52
question
Physiology: continence vs. micturition
answer
balance between urethral closure & detrusor muscle (bladder muscle) activity urethral sphincter pressure normally > bladder pressure = urine continence urethral pressure decreases < bladder pressure = micturition/voiding Normally proximal urethra + bladder both within the pelvis (prolapse can alter this state leading to incontinence); intraabdominal pressure increases (valsalva) are transmitted equally to both, leaving the pressure difference unchanged; continence detrusor muscle spontaneous contractions are normally easily suppressed
question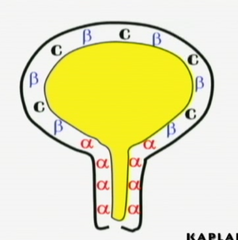
Pharmacology: bladder receptors innervation
answer
α-adrenergic receptors: Sympathetic nervous system - "Sympathetic SHOOTS" hence urethral sphincters contract to inhibit incontinence during ejaculation - primarily found in urethra - *prevent* micturition; *contraction* of urethral - Drugs agonists: ephedrine, imipramine, estrogens - Drugs antagonists: phenoxybenzamine β-adrenergic receptors: Sym. nervous system - *prevents micturition*; relaxation of bladder detrusor muscles hence prevents urination - primarily in the detrusor muscle - Drugs agonists: flavoxate, progestins Cholinergic receptors: Parasympathetic innervation - *enhances micturition* - primarily also in detrusor muscle; *contraction* - Drugs agonists: bethanecol, neostigmine - Drugs antagonists: oxybutynin, propantheline
question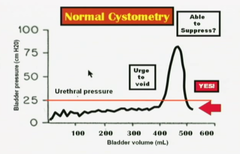
Cystometry Volume Measurements
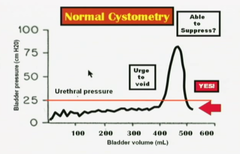
answer
Post-void residual volume = <50mL Sensation of fullness = 200-225mL Urge to void = 400-500mL Normally a patient should be able to suppress the urge to void. (shown on graph) Involuntary contractions can be seen by watching saline level in the syringe rise/fall; normally there should not be any involuntary contractions
question
Sensory Irritative Incontinence: etiology, history, examination, investigative studies, management
answer
Etiology: - involuntary rises in bladder pressure - results in detrusor contractions - possible causes: infection, stone, tumor, foreign body History: - loss of urine occurs with *urgency, frequency and dysuria* - can take place *day or night* Examination: - suprapubic tenderness may be elicited - pelvic examination normal (no prolapse of any sort) - neurological exam normal (anal contraction reflex normal, S2-3-4; by stimulating labia majora we get a anal contraction) Investigative study: *urinalysis* - bacteria and WBC (infection) - RBC (stone, foreign body, tumor) - positive urine culture (infection) - normal cystometric studies (normal RV with involuntary detrusor contractions present) Management: - antibiotics (infections) - cystoscopy to diagnose and remove stones, foreign bodies, tumors
question
Inhibit voiding Tx: bladder relaxants/antispasmodics
answer
oxybutynin (Ditropan) flavoxate (Urispas)
question
Inhibit voiding Tx: bladder relaxant/anticholinergics
answer
Pro-Banthine
question
Inhibit voiding Tx: bladder relaxant/tricyclics
answer
Imipramine (Tofranil)
question
Inhibit voiding Tx: vesical neck contraction/alpha adrenergics
answer
ephedrine Imipramine Estrogen stimulates alpha receptors Progesterone stimulates beta receptors
question
Which receptors do estrogen stimulate? progesterone?
answer
Estrogen stimulates alpha receptors Progesterone stimulates beta receptors
question
Promote voiding Tx: bladder contraction/cholinergics
answer
Bethanechol (Urecholine) Neostigmine (Prostigmin)
question
Promote voiding Tx: vesicle neck relaxants/alpha antagonists
answer
methyldopa phenothiazines
question
Genuine Stress Incontinence: Etiology, history, examination, investigative studies, management
answer
Etiology: - most common form of true urinary incontinence - rises in bladder pressure because of intraabdominal pressure increase - not transmitted to proximal urethra due to pelvic relaxation and not being a part of pelvic structures anymore - *loss of bladder support* History: - loss of urine occurs in small spurts simultaneously with coughing or sneezing - *Does NOT* take place when patient is sleeping Examination: - cystocele may be seen - Neurologic examination is normal - Q-tip test is positive (q-tip placed within the urethra and patient increases intraabdominal pressure, the q-tip will rotate >30 degrees) Investigative studies: - urinalysis + culture are normal - cystometric studies are normal - *no* involuntary detrusor contractions seen Management: Mostly similar to pelvic relaxation management - Kegel exercises - estrogen replacement (stimulates alpha receptors) - surgical therapy aims to elevate the urethral sphincter (Burch procedure, MML, tension-free vaginal tape procedure)
question
What is the most common form of true urinary incontinence?
answer
Genuine stress incontinence
question
What is the only incontinence that does not result in voiding during the night?
answer
Genuine stress incontinence
question
What is the triad of stress incontinence?
answer
Involuntary loss of urine (large) with coughing and sneezing (increase abdominal pressure) No urine lost at night
question
Motor Urge (Hypertonic) Incontinence: etiology, history, examination, investigative studies, management
answer
Etiology: 'Itty-Bitty Bladder Syndrome' - involuntary rises in bladder pressure from idiopathic detrusor contractions that cannot be voluntarily suppressed History: - loss of urine occurs in large amounts; often without warning - day + night - most common symptom is urgency Examination: - pelvic examination shows normal anatomy - neurologic examination is normal Investigative studies: - urinalysis + culture normal - cystometric studies show normal residual volume - *involuntary detrusor contractions are present even with small volumes of urine in the bladder* Management: - anticholinergic medications - NSAIDS to inhibit detrusor contractions - tricyclic anti-depressants - calcium-channel blockers
question
What is the triad for hypertonic bladder?
answer
Involuntary loss of urine cannot suppress urge to void urine loss day + night
question
Hypertonic incontinence vs. Hypotonic incontinence
answer
Hypertonic: - large volume urine loss - idiopathic detrusor muscle contraction - day + night Hypotonic: - small volume urine loss (until urethral sphincter = bladder pressure) - bladder never empties; detrusor muscle relaxation - day + night
question
Overflow/Neurogenic (Hypotonic) Incontinence: etiology, history, examination, investigative studies, management
answer
etiology: - Rises in bladder pressure occur gradually from over-distended, hypotonic bladder - voiding occurs only when bladder pressure > urethral sphincter pressure - *bladder never empties*; voiding occurs only until bladder pressure = urethral sphincter pressure - may be due to denervated bladder (diabetic neuropathy, MS, or systemic medication) history: - loss of urine occurs intermittently in small amounts* - day + night - pelvic fullness is a common symptom examination: - pelvic examination may show normal anatomy - *decreased pudendal nerve sensation* investigative studies: - urinalysis and culture usually normal; may show infection - cystometric studies show markedly increased residual volume - involuntary detrusor muscle contractions do NOT occur management: - intermittent self-catheterization may be necessary - discontinue the offending systemic medications - bladder contraction stimulation (alpha receptor blocker; cholinergic drugs)
question
What is the triad for hypotonic bladder?
answer
involuntary loss of urine detrusor muscle not contracted urine loss day + night
question
Types of urinary incontinence with irregular detrusor muscle contractions
answer
Hypertonic incontinence
question
Types of urinary incontinence with no involuntary detrusor muscle contractions
answer
Stress incontinence Hypotonic incontinence
question
Fistula incontinence: etiology, history, examination, investigative studies, management
answer
etiology: - normal urethral-bladder mechanism is intact - bypassed by urine leaking out through a fistula from urinary tract history: - *radical pelvic surgery* or *pelvic radiation therapy* - loss of urine occurs continually in small amounts - day + night examination: - normal anatomy and normal neurologic findings investigative studies: - urinalysis and culture are normal - IVP (intravenous pyelogram) will demonstrate dye leakage from urinary tract fistula management: - surgical repair of the fistula
question
Triad for bypass incontinence
answer
involuntary loss of urine history: radical pelvic surgery or radiation urine loss day + night continuously* (small amounts)
question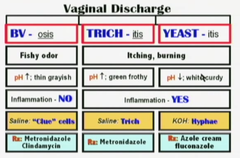
Vaginal discharge: BV, parasitic, yeast
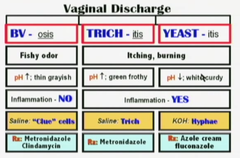
answer
BV; bacterial vaginosis (most common) - fishy odor - pH↑; thin grayish exudate - no inflammation; endogenous transmission - diagnostic: clue cells - Rx: metronidazole; clindamycin Trichomonas vaginalis - itching, burning "strawberry cervix" - inflammation prominent; pH↑ - green/yellowish frothy discharge - Methylene blue wet mount; mobile flagellates - Rx: Metronidazole Candida albicans - itching, burning - inflammation not as prominent as Trichomonas vaginalis; white "cottage cheese" discharge - pH stays same or ↓ - KOH: pseudohyphae/hyphae - Rx: fluconazole; azole cream Note: metronidazole is safe to use in all trimesters of pregnancy; class B
question
Most common cause of vagina discharge? 2nd? 3rd?
answer
Bacterial vaginosis (50%) Candidiasis (30%) Trichomonas (15%)...STD's
question
What is the predominant bacteria in the vagina?
answer
Lactobacillus Normal flora (70%) in BV it decreases to 15%
question
What is the normal pH of the vagina?
answer
pH < 4.5 estrogen dominance
question
Diagnostic Test: Vaginal Discharge
answer
Visual inspection: the vulva and vagina should be examined for evidence of inflammatory response; check vaginal discharge on speculum Vaginal pH: normal <4.5 Microscopic examination 2 drops of vaginal discharge are placed on glass slide (saline on one side, KOH on the other) looking for clue cells, hyphae, flagellates, WBC's
question
What is a positive "whiff" test in BV?
answer
when KOH is placed on the discharge, releasing a fishy odor KOH is for Candida albicans diagnostics; but it dissolves tissue
question
How does BV most commonly present as?
answer
asymptomatic 50%
question
Rx: Bacterial vaginosis
answer
Metronidazole - safe to use in all 3 trimesters of pregnancy - 250mg - t.i.d. for 7 days - no alcohol for 24-48 hrs Clindamycin - 300mg - b.i.d. for 7 days
question
Trimethylamineuria
answer
Fish odor syndrome AR a rare clinical entity where the patient has an offensive persistent odor that no amount of bathing can correct differential diagnosis with BV
question
What is associated with bubbly vaginal discharge?
answer
Trichomonas vaginalis
question
Trichomoniasis: Men vs. Woman symptoms
answer
Men: 90% asymptomatic Woman: 50% asymptomatic Both needs treatment despite presentations
question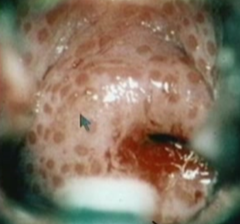
What is associated with strawberry cervix?
answer
Trichomonas vaginalis
question
Rx: Vaginal Trichomoniasis
answer
Metronidazole - 24~48hrs no liquor - recommended: 2g orally in a single dose - alternative: 500mg b.i.d for 7 days - pregnancy: 2g orally in a single dose
question
Rx: Vaginal Candidiasis
answer
Oral fluconazole - 150mg single dose azole cream
question
Physiologic discharge: Sx, risk factors, speculum exam, management
answer
Sx: - most common complaint is increased watery vaginal discharge - no burning or itching Speculum: - columnar epithelium of endocervical canal extends over a wide area of the ectocervix, producing abundant mucus discharge - thin and watery - pH is normal (<4.5) Risk factors: - chronic anovulatory conditions - PCOS, etc. (polycystic ovarian syndrome) Management: - steroid contraception with progestins - convert watery thin discharge into thick sticky progestin-dominant mucus
question
Most common symptom of benign/malignant vulvar lesions
answer
Vulvar itching
question
Premalignant vulvar dermatosis
answer
benign lesions with malignant predisposition - most common symptom is vulvar itching, most lesions are asymptomatic Diseases: - Squamous hyperplasia - Lichen sclerosis - Squamous dysplasia - CIS
question
Squamous hyperplasia : appearance, palpation, histology, management
answer
premalignant vulvar dermatosis Appearance: - lesions appear whitish focal or diffuse areas Palpation: - firm and cartilaginous on palpation Histologically: - thickened keratin - epithelial proliferation Management: - fluorinated corticosteroid cream
question
Lichen sclerosis: appearance, palpation, histology, management
answer
premalignant vulvar dermatosis Appearance: - lesions are bluish-white papula that can coalesce into white plaques Palpation: - thin and parchment-like Histology: - epithelial thinning Management: - Clobetasol cream
question
Vulvar squamous dysplasia: appearance, histology, management
answer
premalignant vulvar dermatosis Appearance: - lesions are white, red, or pigmented, often multifocal in location - almost identical to cervical dysplasia Histology: - cellular atypia restricted to the epithelium without breaking through the basement membrane Management: - surgical excision
question
CIS: appearance, histology, management
answer
premalignant vulvar dermatosis Appearance: - indistinguishable from vulvar dysplasia - white, red, or pigmented, often multifocal lesions Histology: - cellular atypia is full thickness but does not penetrate the basement membrane Management: - laser vaporization and vulvar wide local excision
question
Malignant vulvar lesions
answer
uncommon gynecologic malignancy (4th most common gynecologic malignancy) mean age 65 risk factors: old age, cigarette smoking, HIV, premalignant vulvar dermatosis Diseases: - squamous cell - melanoma - Paget disease
question
Squamous cell (malignant vulvar lesion)
answer
most common type of invasive vulvar cancer (90%) association with HPV Pathogenesis is chronic inflammation (for older woman) and HPV infection (for younger women) Most common stage at diagnosis is Stage 1
question
Melanoma (malignant vulvar lesion)
answer
second most common histologic type of vulvar cancer (5%) most important prognostic factor is the depth of invasion Any dark or black lesion in vulva should be biopsied and considered for melanoma
question
Paget disease (malignant vulvar lesion)
answer
Characteristics: - red lesion - most common in postmenopausal white women Any patient with red vulvar lesion must be considered for the possibility of Paget disease Most common form of Paget disease is intraepithelial process 18~20% of cases invasion of basement membrane is identified association with other cancers (mainly GI, urinary, and breast)
question
Malignant vulvar lesions: diagnosis
answer
Biopsy
question
Malignant vulvar lesions: pattern of spread
answer
starts with local growth and extension that embolizes to inguinal lymph nodes and finally, hemtogenous spread to distant sites
question
Malignant vulvar lesions: staging
answer
Staging is surgical Stage 0: CIS (basement membrane is intact) Stage I: - tumor confined to vulva with size </= 2cm - nodes not palpable Stage IA: invasion 1mm deep Stage II: - tumor confined to the vulva with size >2cm - nodes not palpable Stage III: - Tumor any size with spread to lower urethra, vagina, or anus - unilateral nodes Stage IV: widespread metastasis Stage IVA: involves upper urethra, bladder or rectum, pelvic bone, bilateral nodes Stage IVB: distant metastasis
question
Malignant vulvar lesions: management
answer
1) Wide local excision 2) Modified radical vulvectomy 3) Radical vulvectomy 4) Pelvic exenteration 5) Radiation therapy
question
Management for stage IA malignant vulvar lesions
answer
Wide local excision only
question
Malignant vulvar lesions management: wide local excision
answer
Stage IA only risk of metastasis is negligible No lymphadenectomy is needed
question
Malignant vulvar lesions management: Modified radical vulvectomy
answer
involves radical local excision - Ipsilateral inguinal dissection is used only if stage is IB and unifocal lesion > 1cm from midline AND no palpable nodes (less sexual morbidity) - Bilateral inguinal dissection is used if at least stage IB or a centrally located lesion OR palpable inguinal nodes or positive ipsilateral nodes (lower-extremity edema)
question
Malignant vulvar lesions management: radical vulvectomy
answer
involves removal of labia minora + majora, clitoris, perineum, perineal body, mons pubis seldom performed due to high morbidity sexual dysfunction may result
question
Malignant vulvar lesions management: pelvic exenteration
answer
radical vulvectomy + removal of cervix, vagina, ovaries + lower colon, rectum + bladder create appropriate stomas if necessary seldom indicated or performed due to high morbidity
question
Malignant vulvar lesions management: radiation therapy
answer
only used for patients who cannot undergo surgery
question
Benign vulvar lesions: diseases
answer
1) Mulluscom contagiosum 2) Condylomata acuminata 3) Bartholin cyst
question
Mulluscom contagiosum: at risk group, Sx, transmission, management
answer
Benign vulvar lesion Children, sexually active adults, immunodeficient patients Sx: - spontaneously regressing, umbilicated tumors of skin Transmission: - direct skin contact Management: - observation - curettage - cryotherapy
question
Condylomata acuminata: causative agent, Sx, management
answer
Benign vulvar lesions HPV 6, 11 (no malignant predisposition) Sx: - cauliflower-like vulvar lesions Management: - treat clinical lesions only
question
Bartholin cyst: pathogenesis, management
answer
Benign vulvar lesions obstruction of the Bartholins gland duct may occur due to infection (GC) After immune defenses overcome, duct remains obstructed resulting in cystic dilation of the gland aspiration of the cyst yields sterile fluid Management: - conservative unless pressure symptoms due to size
question
gynecologic cancer rankings 1~4 and age relevance
answer
1. endometrium (61) 2. ovaries (69) 3. cervix (45) 4. vulva (65)
question
What is the type of gynecological cancer occurs earliest in life? Oldest?
answer
Cervical cancer (45) Ovaries (69)
question
Cervical polyps: description, cause, at risk group, findings, management
answer
Description: fingerlike growths that start on the surface of the cervix or originate within endocervical canal/columnar epithelium (more common), can extend out of the cervical os. Cause: - Idiopathic - Associated with chronic inflammation - Associated with increased levels of estrogen (ex: pregnancy) - Associated with thrombosed cervical blood vessels At risk group: - relatively common - older multiparous women more common Findings: - vaginal bleeding, often after intercourse - bleeding occurs between normal menstrual periods - speculum examination: smooth, red/purple, fingerlike projections from cervical canal - biopsy typically reveals mildly atypical cells and signs of infection Management: - polyps can be removed by gentle twisting or by surgical string removal method (electrocautery/laser) - due to infected polyps being common, antibiotic may be given after the removal even if there are no or few signs of infection - although most polyps are benign, pathology exam of biopsy should still be done - regrowth of polyps is uncommon
question
What are cervical polyps associated with?
answer
Associations: - chronic inflammation - increased estrogen levels (pregnancy, etc.) - thrombosed cervical blood vessels - idiopathic
question
What do people with cervical polyps most commonly present with?
answer
vaginal bleeding, mostly after intercourse bleeding between normal menstrual cycles
question
What is the management of cervical polyps?
answer
polyps can be removed by gentle twisting or by surgical string removal method - electrocautery - laser antibiotics given after procedure due to common association of polyps with infection biopsy sent to pathology regardless of nature of polyps
question
Which group of people are at risk for developing cervical polyps?
answer
older women multiparous women
question
Nabothian cysts: description, cause, findings, management
answer
Description: mucus-filled cyst on the surface of the uterine cervix. These endocervical glands can become *covered* by squamous epithelium through metaplasia. Cause: - during the metaplasia and formation of the T-zone, columnar epithelium morphs into squamous epithelium; if the columnar cells beneath did not completely go through metaplasia, they can secrete mucus which can push the squamous epithelium outwards. Findings: - benign condition; rarely large enough to cause clinically relevant problems - pelvic examination reveals small, smooth, rounded lump (or collection of bumps) - rarely, colposcopic exam can be used to distinguish nabothian cysts from other types of cervical lesions Management: - no treatment necessary - Nabothian cysts do not clear spontaneously - Easily cured through electrocautery or cryotherapy
question
The cervical canal is lined by what type of cells? Function?
answer
Glandular cells / columnar epithelium secrete mucus
question
What does the Nabothian cyst present as? How do you treat it?
answer
small, smooth, rounded lump or collection of bumps caused by mucus-fileld cysts on the surface of the cervix (ectocervix) due to incomplete metaplasia of columnar epithelium beneath the T-zone during transformation benign condition No treatment necessary - electrocautery or cryotherapy can easily cure cyst
question
Cervicitis: symptoms, examination, investigative findings, management
answer
Symptoms: - no symptoms most common - vaginal discharge Examination: - most common finding is mucopurulent cervical discharge - friable cervix: endocervical bleeding easily induced by cotton swab palpation of cervical os - No pelvic tenderness noted - Patient is afebrile Investigative findings: DNA probe - Routine cervical cultures are positive for chlamydia or gonorrhea - STDs - WBC and ESR normal (no inflammation) Management: - Oral azithromycin in single dose - Oral doxycycline BID for 7 days
question
What is the most common finding in cervicitis?
answer
mucopurulent discharge from cervix friable cervix no pelvic tenderness or febrile condition
question
How do you manage cervicitis?
answer
Oral azithromycin single dose or Oral doxycycline BID for 7 days
question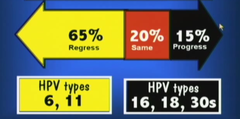
Cervical neoplasia: presentation, etiology, risk factors
answer
Presentation: - usually asymptomatic - progression from premalignant to invasive cancer has been reported to be approximately 8~10 yrs (good prognosis for early detection and slow progression) - Most regress (young women) Etiology: - most common* etiology of cervical cancer is HPV - Over 75 subtypes - most common HPV types: 16, 18, 31, 33, 35, 45 - most common for condyloma accuminata: 6, 11 risk factors: - early age intercourse - multiple sexual partners* (strong positive correlation) - cigarette smoking - immunosuppression
question
What is the most common presentation of cervical cancer? What is the most common progression? Associated age groups and types?
answer
most common presentation is asymptomatic progression is most commonly regression, especially in young women - age 14~19 has 33% HPV risk - age 20~29 has 28% HPV risk 65% regress, associated with HPV 6, 11 - young women most commonly regress, 61% within 1 yr, and 91% within 3 years 20% same + 15% progress - associated with HPV 16, 18, 30s
question
What are the risk factors for developing cervical cancer?
answer
early age of intercourse cigarette smoking multiple sex partners immunosuppression
question
What are the most common HPV types for cervical cancer? Order of malignancy? Condyloma accuminata?
answer
CIN: HPV-16, 18, 31, 33, 35, 45 (16>18>45>31>33) Condyloma accuminata: HPV-6, 11
question
What is the most effective medically cancer screening test ever developed?
answer
PAP smear 70~80% decrease of death rate
question
Which HPV is most associated with squamous cell carcinoma of cervix?
answer
HPV-16
question
Which HPV is most associated with adenocarcinoma of the cervix?
answer
HPV-18
question
Rank the most common malignant HPV types that causes cancer in the cervix + association
answer
HPV-16 (squamo)....59% HPV-18 (adeno)....12% HPV-45>31>33....squamo
question
Why do we NOT start PAP smear before age of 21?
answer
Most cases of HPV infection regresses (65%) More so, most cases of HPV infection in young woman regresses completely in 3 years (91%) HPV infection is correlated with sexual intercourse at young age if HPV is going to regress mostly in 3 years there isn't a point of starting PAP smears until after 21yrs old
question
When doing a Pap smear on pregnant women what should you use?
answer
spatula for T-zone *cotton swab for endocervical canal
question
Pap smear should be started at the following ages:
answer
Age < 21: - NO Pap test or screening for HPV, regardless of sexual activity Age 21: start Pap test with cytology alone *without HPV testing; the recommendation is the same whether HPV vaccinated or not
question
What is the frequency of recommended Pap smear for Age groups 21-29? 30-65?
answer
Age 21-29: - repeat Pap every 3 years with cytology alone; do not perform HPV testing in this age group (due to slow progression of the disease) Age 30-65: - Pap every 3 years with cytology but no HPV testing OR - repeat Pap every 5 years if both cytology + HPV (recommended choice)
question
When should Pap smears be discontinued?
answer
After age 65 - if negative cytology and/or HPV tests for past 10 years AND no history of CIN-2, 3, or cervical carcinoma Any age if total hysterectomy and no history of CIN
question
What is the system used to classify Pap smears in the U.S.?
answer
Bethesda system
question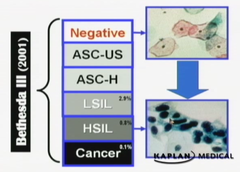
Classification os Bethesda system
answer
Negative: No intraepithelial lesions - may report trichomoniasis, candida, BV, HSV, atrophy, etc. Abnormal squamous cells (99% of abnormal Pap smears) ASCUS: (5%~20%) - atypical squamous cells of undetermined significance - suggestive of LSIL but not adequate - decrease ASCUS findings by making a thinner prep ASCH: - atypical squamous cells can't rule out HSIL - suggestive of but not adequate to label HSIL LSIL: - low-grade squamous intraepithelial lesion - biopsy is expected to show histologic findings of HPV, mild dysplasia, or CIN 1 HSIL: - high-grade squamous intraepithelial lesion - biopsy is expected to show histologic findings of moderate-severe dysplasia, CIN 2, 3, CIS Squamous cell carcinoma: - biopsy expected to show histologic findings of invasive cancer Abnormal endocervical cells (1% of abnormal Pap smears) AGC-NOS: - atypical glandular cells, not otherwise specified AGC-neoplastic: - atypical glandular cells, can't rule out neoplasia - changes suggestive of but not adequate to call AIS or cancer AIS: - adenocarcinoma in situ Adenocarcinoma
question
Describe ASCH on Bethesda system
answer
atypical squamous cells can't rule out HSIL - changes suggestive of but not adequate to label HSIL
question
Describe ASCUS on Bethesda system
answer
atypical squamous cells of undetermined significance - changes suggestive of but not adequate to label LSIL
question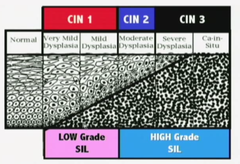
Describe LSIL on Bethesda system
answer
low-grade squamous intraepithelial lesion - biopsy is expected to show histologic findings of HPV, mild dysplasia, CIN1
question
Describe HSIL on Bethesda system
answer
high-grade squamous intraepithelial lesion - biopsy is expected to show histologic findings moderate-severe dysplasia, CIN2, CIN3, CIS
question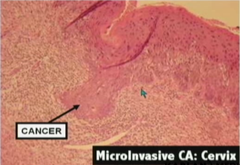
Squamous cell carcinoma on Bethesda system
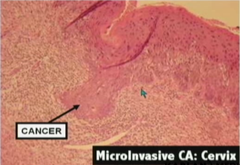
answer
Invasive carcinoma will enter staging instead of CIN numbers Stage 1 is after CIS - <2cm lesion (1a = 1mm deep lesion)
question
Describe AGC-NOS on Bethesda system
answer
atypical glandular cells not otherwise specified
question
Describe AGC-neoplastic on Bethesda system
answer
atypical glandular cells can't rule out neoplasia
question
Describe AIS on Bethesda system
answer
adenocarcinoma in situ
question
High-grade squamous intraepithelial lesions are associated with which histologic findings?
answer
moderate-severe dysplasia CIN-2 CIN-3 CIS
question
Low-grade squamous intraepithelial lesions are associated with which histologic findings?
answer
mild dysplasia HPV CIN 1
question
How often does ASCUS show up on Pap smears? How do you decrease ASCUS diagnosis? What is the management of ASCUS?

answer
<5% but up to 20% Decrease ASCUS findings by: - make a thinner prep or HPV/DNA typing: - if 6, 11 it will most likely regress (low-risk) but repeat Pap within 1 year - if 16, 18, 30s it is high-risk and need colposcopy and biopsy
question
If you find ASCUS on Pap smear, what are the tests you could run? (3)
answer
Accelerate repeat Pap: - 4~6 month intervals until 2 consecutive negative Paps - if a repeat Pap is again ASCUS or worse, this is an indication for colposcopy HPV-DNA testing: - if liquid-based cytology was used on initial Pap smear, it can be used for DNA testing (100% diagnostic) - indications for colposcopy: high-risk HPV types Colposcopy: - uses acetic acid to make vascular patterns more visible - 10~12 times magnification - satisfactory/non-satisfactory - unsatisfactory = t-zone invading into endocervical canal
question
What if you find cells other than ASCUS on a Pap smear, what tests should you run?
answer
Colposcopy and biopsy
question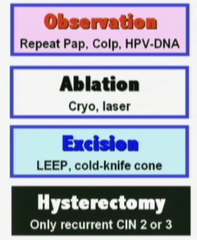
If you find cells others than ASCUS (ASC-H, LSIL, etc.) on a Pap smear, what is your plan of management?
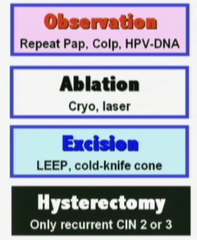
answer
Colposcopy Endocervical curettage (ECC) - not in pregnancy - ***colposcopy shows T-zone extending into endocervical canal, etc. Ectocervical biopsy - lesions identified on ectocervix by colposcopy*** - mosaicism, punctation, white lesions, abnormal vessels - biopsy and send for histology Compare Pap smear and biopsy - ensure level of severity is comparable with colposcopy - *Pap smear should not be worse than biopsy; means you missed the more malignant area on biopsy Diagnostic Cone biopsy indications: - Pap smear is worse than biopsy - ECC: abnormal cells - Lesions entering endocervical canal*** - Biopsy: microinvasive carcinoma Manage by histology: - observation: CIN1, repeat Pap in 6~12 months, colposcopy and repeat Pap in 12 months, or HPV/DNA testing in 12 months - ablation: CIN1, 2, 3 (cryotherapy, laser vaporization, electrofulguration) - resection: CIN1, 2, 3 (LEEP, cold-knife conization) - hysterectomy: biopsy-confirmed, recurrent CIN2 or 3 only
question
What are the risk of cone biopsy?
answer
incompetent cervix cervical stenosis
question
When Pap smear shows worse dysplasia than ASCUS, you use colposcopy examination and you see metaplastic epithelium entering the endocervical canal, what will you do next?
answer
ECC endocervical canal curettage
question
When Pap smear shows worse dysplasia than ASCUS, you use colposcopy examination and you see ectocervical lesions, what will you do next?
answer
Ectocervical biopsy
question
When Pap smear shows worse dysplasia than ASCUS, you use colposcopy examination and you see lesions entering the endocervical canal, what will you do next?
answer
Narrow cone biopsy
question
What are follow-up options for CIN1?
answer
Observation (repeat Pap, colposcopy and Pap, HPV-DNA) Ablative therapy (cryotherapy, laser, electrofulguration) Excisional procedure (LEEP, cold-knife)
question
What are follow-up options for CIN2?
answer
Ablative therapy (cryotherapy, laser, electrofulguration) Excisional procedure (LEEP, cold-knife cone) Hysterectomy (recurrent CIN2 only)
question
What are follow-up options for CIN3?
answer
Ablative therapy (cryotherapy, laser, electrofulguration) Excisional procedure (LEEP, cold-knife cone) Hysterectomy (recurrent CIN3 only)
question
When is hysterectomy indicated in CIN?
answer
recurrent CIN2, 3
question
CIN follow-up management: Observation
answer
Indicated for CIN1 Repeat Pap in 6~12 months Colposcopy and repeat Pap in 12 months HPV-DNA testing in 12 months
question
CIN follow-up management: Ablative therapy
answer
Indicated for CIN1, 2, 3 Cryotherapy Laser vaporization Electrofulguration Follow-up: repeat Pap smears, colposcopy and Pap smear, or HPV-DNA testing every 4~6 months for 2 years
question
CIN follow-up management: Excision/Resection
answer
Indicated for CIN1, 2, 3 LEEP cold-knife conization Follow-up: repeat Pap smears, colposcopy and Pap smear, or HPV-DNA testing every 4~6 months for 2 years
question
CIN follow-up management: hysterectomy
answer
CIN2, 3 only indicated in recurrent infections
question
What follow-up procedures are required for ablative therapy and excisional procedure patients for CIN?
answer
Follow-up: repeat Pap smears, colposcopy and Pap smear, or HPV-DNA testing every 4~6 months for 2 years
question
If cytologic findings of Pap smear reveals HSIL, what is the next step for patients ages 25-64?
answer
colposcopy + biopsy immediate LEEP**
question
Invasive Cervical Cancer definition
answer
cervical neoplasia that has penetrated through the basement membrane >CIS
question
Cervical cancer: definition, presentation, epidemiology, diagnostic findings
answer
Definition: cervical neoplasia penetrated through the basement membrane Presentation: - normal menstrual cycles - postcoital vaginal bleeding - irregular vaginal bleeding - lower extremity pain and edema in advanced stages Epidemiology: - 3rd most common gynecological carcinoma - ~45 years of age (youngest occurrence) - 250,000 deaths/yr world wide; 10,000/yr in U.S. Diagnostic Tests/Findings: - Cervical biopsy* - Metastatic workup: pelvic examination, chest x-ray, intravenous pyelogram, cystoscopy, sigmoidoscopy - Imaging studies: invasive cervical cancer is the ONLY gynecological cancer staged clinically (CT and MRI cannot be used for clinical staging)
question
What is the only gynecological carcinoma that uses clinical staging?
answer
Cervical cancer
question
Common presentation of cervical carcinoma?
answer
normal menstrual cycle postcoital vaginal bleeding irregular vaginal bleeding
question
Cervical cancer: staging
answer
CLINICAL (only gynecological carcinoma staged clinically) Stage 0: CIS (basement membrane is intact) Stage I: Spread limited to the cervix. *most common* - Ia1: 3mm but 5mm deep (frank invasion) Stage II: spread adjacent to cervix - IIa: involves upper 2/3 of vagina - IIb: invasion of parametria Stage III: spread further from the cervix - IIIA: involves lower one third of vagina - IIIB: extends to pelvic side wall or hydronephrosis Stage IV: spread furthest from cervix - IVA: involves bladder or rectum or beyond true pelvis - IVB: Distant metastasis
question
What is the most common stage of cervical cancer?
answer
Stage 1 limited to the cervix
question
What is the staging for minimally invasive cervical cancer? Management? Management in pregnancy?
answer
Ia1 </= 3mm deep total simple hysterectomy during pregnancy: cone biopsy during pregnancy follow conservatively, deliver vaginally reevaluated and treated 2 months postpartum
question
What is the staging for microinvasive cervical cancer? Management? Management in pregnancy?
answer
Ia2 <3mm but </=5mm deep modified radical hysterectomy during pregnancy: cone biopsy during pregnancy follow conservatively, deliver vaginally reevaluated and treated 2 months postpartum
question
What is the staging for frank invasion cervical cancer? Management? Management in pregnancy?
answer
IB >5mm deep radical hysterectomy or radiation (IIa) during pregnancy: based on gestational age - before 24 weeks: receive definitive treatment as shown above - after 24 weeks: conservative management to 32-33 weeks, after C-section definitive treatment can be done
question
What ist he staging for cervical cancer that has spread adjacent to the cervix? Management? Management in pregnancy?
answer
II IIa: upper 2/3 of vagina involved Management: radical hysterectomy or radiation IIb: invasion of parametria Management IIb or above: radiation therapy and chemotherapy for all ages during pregnancy: based on gestational age - before 24 weeks: receive definitive treatment as shown above - after 24 weeks: conservative management to 32-33 weeks, after C-section definitive treatment can be done
question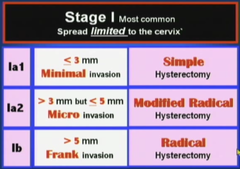
Cervical cancer: staging management
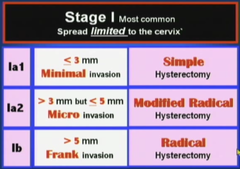
answer
Stage Ia1: - 3mm but 5mm frank invasion - IIa: involves upper 2/3 of vagina - radical hysterectomy with/without radiation Stage IIb, III, IV: - radiation therapy and chemotherapy for all ages
question
Cervical cancer: follow-up
answer
All patients with invasive cervical cancer should be followed up with... - Pap smear every 3 months for 2 years after treatment - then every 6 months for subsequent 3 years Patients who have local recurrence can be treated with radiation therapy Patients with distant metastases should be considered for chemotherapy treatment - Cisplatinum
question
What is the most active chemotherapeutic agent for cervical cancer?
answer
Cisplatinum
question
What is the effect of pregnancy in cervical neoplasia
answer
pregnancy does NOT predispose abnormal cytology and does not accelerate precancerous lesions progression
question
Diagnostic tests and findings for pregnant patients in cervical cancer
answer
Pregnant with abnormal Pap smear should be evaluated in the SAME FASHION - owing to increased cervical vascularity ECC is not performed during pregnancy (endocervical canal curettage)
question
What is the plan of management in pregnant patients with cervical cancer in CIN stages?
answer
Pap smear and colposcopy every 3 months during pregnancy 6~8 weeks postpartum the patient should be reevaluated with repeat colposcopy an dPap smear Any persistent lesions can be definitively treated postpartum
question
What is the plan of management for microinvasion cervical cancer in pregnant patients?
answer
evaluated with cone biopsy to ensure no rank invasion patients can be followed conservatively delivery can be vaginal reevaluation and treatment 2 months postpartum
question
What is the plan of management for frank invasion carcinoma in pregnant patients?
answer
Based on gestational age before 24 weeks - definitive treatment based on staging after 24 weeks - conservative management to about 32-33 weeks - C-section - definitive treatment after delivery
question
Gardasil: recommendation, coverage, regimen
answer
Recommendation: - females 8~26; target group 11~12yrs - Efficacy is highest before patient's immune system is exposed to HPV - No point in testing for HPV before vaccination, no easy method of identifying all HPV types - Pap smear continued to guidelines due to >70 types of HPV strains and vaccine covers only 4 most common - sexually active women can receive vaccine, same with women who has previous abnormal cervical cytology or genital warts, just less effective - patients with previous CIN, benefits limited - not recommended for pregnant, lactating, or immunosuppressed women, but no tests has been done to prove clinical relevant harm Coverage: - HPV 6, 11, 16, 18 - covers 70% of cervical cancer and 90% of genital warts of HPV strains Regimen: - initial, 2 months, 6 months - $300
question
What is the target group for Gardasil? Why?
answer
11~12 age group Efficacy best before host immune system is exposed to HPV strains
question
What strains of HPV does Gardasil cover?
answer
HPV 6, 11, 16, 18
question
When is the Gardasil vaccine contraindicated?
answer
Pregnant women Lactating women Immunosuppressed women Not clinically proven to be true
question
How many types of uterine anomalies are there? How are they divided?
answer
7 types by the American Fertility Society (1988) Divided by - failure to form - failure to fuse - failure to dissolve the septum
question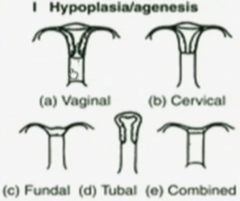
Hypoplasia/Agenesis of Uterus: description, cause, association
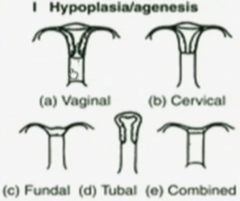
answer
description: - may lack a vagina, cervix, fallopian tubes, body of uterus - developmental problem with a section of both mullerian ducts association - urinary tract anomalies - urinary tract embryologically lie close to mullerian ducts
question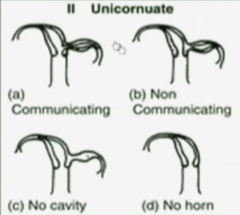
Unicornuate uterus: defect, description, complications, symptoms
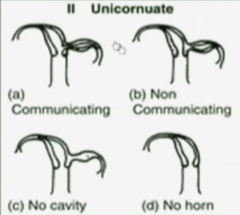
answer
defect and description: - when ONE of the mullerian ducts fails to form - *sing-horn (banana-shaped) uterus develops from the remainder healthy mullerian duct - single uterus may stand alone complications: - 65% of women with unicornuate uterus, the defected mullerian duct may form an incomplete rudimentary horn - may or may not have cavity in the rudimentary horn but the opening that communicates with the healthy uterus is either small or nonexistent symptoms: if rudimentary horn forms - monthly pain during adolescence because no outlet for menses from rudimentary horn - risk of pregnancy in rudimentary horn, 90% ruptures due to anatomical limitations
question
Didelphys uterus: defect, description, risks

answer
defect and description: - results from complete failure of the 2 mullerian ducts to fuse together (stage 1 development) - each duct develops into a separate uterus - each uterus can have their own cervix or share a cervix - 67% of cases is associated with 2 vaginas separated by a thin wall risks: - preterm delivery is common
question
Bicornuate uterus: defects, description, types, risks

answer
defect and description: - most common congenital uterine anomaly (45%) - results from failure of fusion between the mullerian ducts at the fundus - 'complete' failure to fuse results in 2 separate single-horn uterine bodies sharing 1 cervix* - 'partial' failure to fuse results in fusion at the bottom but not the fundus causing single uterine cavity with 2 distinct horns on top and a shared cervix* Risks: - preterm delivery - malpresentations with pregnancy
question
What is the most common congenital uterine anomaly?
answer
Bicornuate uterus 45%
question
Septate uterus: defect, description, types, risks

answer
defect and description: - failure in degeneration of the median septum - complete failure: 2 single-horned uteri that share one cervix - partial failure: shared cavity at lower portion of uterus with 1 cervix - *external shape of uterus is normal-appearing* risks: - preterm delivery
question
Septate uterus vs. Bicornuate uterus
answer
septate uterus looks normal-appearing single unit exteriorly bicornuate uterus has distinct 2 separate horns at fundus both can result in separate cavity but sharing 1 cervix or partial shared cavity with 1 cervix
question
Arcuate uterus: defect, description, risks

answer
defect and description: - essentially NORMAL in shape - NORMAL in function as well - small midline indentation in the uterine fundus, results from failure to dissolve the median septum completely risks: - essentially none
question
DES uterus: defect, description, cause, risks

answer
defect and description: - *T-shaped cavity - mothers exposed to DES (diethylstilbestrol) which was used 30yrs ago to prevent miscarriages are predisposed to uterine abnormalities and clear cell carcinoma of the vagina, idiopathic risks: - cervical insufficiency
question
What teratogen is associated with predisposition of clear cell carcinoma of the vagina?
answer
DES (diethylstilbestrol) DES uterus + clear cell carcinoma of vagina idiopathic
question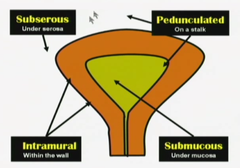
Leiomyoma Uteri: description, at risk group, different locations
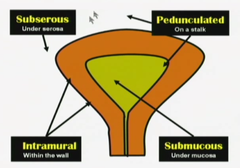
answer
Description: benign smooth muscle growth of myometrium causing non-tender asymmetric distortions of the uterus; most common benign uterine tumor At risk group: 5x more common in black women than white women Location: Intramural: - most common location is within uterine wall - asymptomatic and cannot be felt on examination unless enlargement of uterus is altering external contour Submucosal: - located beneath the endometrium and can distort the uterine cavity - since endometrium may not respond appropriately to normal hormonal fluctuation the result is unpredictable, often intermenstrual, bleeding* - *most common symptom is vaginal bleeding and can result in anemia Subserosal: - located beneath uterine serosa; they can distort the external contour of the uterus - pedunculated subserosal leiomyomas can become parasitic fibroids - they break away from uterus and receive their blood supply form another abdominal organ
question
Leiomyoma uteri: natural history
answer
Natural history: - slow growth*: most leiomyomas are small, grow slowly and cause no symptoms - rapid growth: estrogen receptors are increased in leiomyomas resulting in rapid enlargement during times of high estrogen levels, such as pregnancy - degeneration: during rapid growth, myomas may outgrow their blood supply, resulting in ischemic degeneration of a fibroid (hyaline, calcific, red degeneration/carneous degeneration) - Shrinkage: when estrogen levels fall, leiomyomas will typically decrease in size; physiologically (menopause) or through treatment (GnRH agonist suppression of FSH)
question
How does most leiomyomas present clinically?
answer
Slow growth small, grow slowly, and asymptomatic
question
What is the most common form of leiomyoma of uterus?
answer
Intramural leiomyoma found within the uterine wall
question
What is the most common presentation of a submucosal leiomyoma of the uterus?
answer
vaginal bleeding metrorrhagia = irregular bleeding between menses menorrhagia = heavy menses
question
Which type of uterine leiomyoma can become parasitic fibroids?
answer
Pedunculated subserosal uterine leiomyoma Break away from uterus and receive blood supply from another organ in the abdomen
question
Where is the intramural leiomyoma of the uterus found? How does it present?
answer
Most common location of leiomyoma uteri Found within the wall of the uterus Mostly asymptomatic and cannot be felt on examination unless it enlarges to where the normal uterine external contour is altered
question
Where is the submucosal leiomyoma of the uterus found? How does it present?
answer
It is found beneath the endometrium and can distort the uterine cavity It can be pedunculated and extend into the vagina through the cervix Due to overlying endometrium may not respond appropriately to the normal hormonal fluctuations, it results in unpredictable and often intermenstrual bleeding - menorrhagia - metrorrhagia - menometrorrhagia = combined of irregular bleeding between menses and heavy menses Most common presentation is vaginal bleeding
question
Where is the subserosal leiomyoma of the uterus found? How does it present?
answer
It is found beneath the uterine serosa They can distort the external contour of the uterus causing firm, nontender asymmetry Pedunculated subserosal leiomyomas can break away from uterus and form parasitic fibroids receiving blood supply from another organ
question
What are the top causes of uterine enlargement?
answer
1. pregnancy 2. leiomyoma 3. adenomyosis 4. leiomyosarcoma (extremely rare)
question
What is the cause of leiomyoma uteri degeneration? What are the types? Presentations?
answer
Sometimes the leiomyoma outgrows its blood supply and can result in ischemic infarction causing degeneration hyaline, calcified, red degeneration Red degeneration is also called carneous degeneration - cause extreme, acute pain - morphine and narcotics required - this is most common during pregnancy
question
What is the most common type of degeneration of uterine leiomyoma during pregnancy?
answer
Red degeneration
question
When does uterine leiomyoma present with rapid growth?
answer
estrogen receptors are increased in leiomyomas resulting in rapid enlargement during times of high estrogen levels example: pregnancy
question
Leiomyoma uteri: management
answer
Observation: - most leiomyomas can be managed conservatively and followed expectantly with regular pelvic examinations Presurgical shrinkage: - 3~6 months GnRH analog therapy; leuprolide/Lupron - adjuvant to surgical removal - reduction in size up to 60%~70% - decrease in blood loss in myomectomy - makes vaginal hysterectomy possible Myomectomy: - removal of myoma - maintains fertility - laparoscopic or laparotomy - future deliveries through cesarean section Embolization: - catheter placed into vessels supplying myoma - microspheres are injected, causing ischemia and necrosis of myoma - ~10% mortality rate (wrong vessel; uterine necrosis) Hysterectomy: - definitive therapy
question
How can you shrink a uterine leiomyoma before surgery? Purpose?
answer
3~6 months of GnRH (gonadotropin releasing hormone) analog therapy; Lupron (leuprolide) Results in 60%~70% shrinkage in size Not used for definitive cure, due to stoppage of leuprolide can cause regrowth of leiomyoma Mostly used as an adjuvant to surgical removal of myoma; decreases blood loss in myomectomy the decrease in size can also result in vaginal hysterectomy instead of abdominal hysterectomy
question
Uterine leiomyoma: diagnosis methods
answer
Diagnosis: Pelvic examination: enlarged, asymmetric, non-tender uterus in teh absence of pregnancy most common - 20wks gestation size = uterus reaching umbilicus (belly button) - 12wks gestation size = uterus reaching pubis symphysis Sonography: ultrasound, saline infusion sonography is helpful for identifying submucosal myomas Hysteroscopy Histology is only confirmed through surgical confirmation of excised tissue
question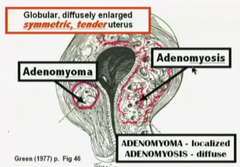
Adenomyosis: definition, presentation, diagnosis, Sx, examination, imaging, management
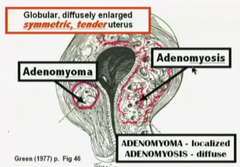
answer
Definition: ectopic endometrial glands and stroma are located within the myometrium of the uterine wall Presentation: - most common presentation is diffuse involvement of the myometrium - adenomyoma is termed for focal involvement, surrounded by a pseudocapsule Diagnosis: - enlarged, symmetric, tender uterus in teh absence of pregnancy - definitive diagnosis is by histologic confirmation of the surgically excised tissue Sx: - mostly asymptomatic - most common symptoms are secondary dysmenorrhea and menorrhagia Examination: - uterus is globular and up to 2~3x normal size - tenderness is most common immediately before and during menses Imaging: - ultrasound - MRI - *cystic areas found within the myometrial wall Management: - surgery is the definitive treatment - LNG-IUS (levonorgestrel intrauterine system may decrease heavy menstrual bleeding)
question
Primary dysmenorrhea findings
answer
onset 2~3yrs after menarche menarche = 11~16.5 yrs
question
What is the most common presentation of adenomyosis? Otherwise?
answer
Most common is diffuse involvement resulting in symmetric, soft, tender enlargement of the uterus When it becomes focalized and surrounded by a pseudocapsule, it is called adenomyoma
question
What is the most common symptoms of adenomyosis?
answer
mostly asymptomatic most common symptomatic presentation is - menorrhagia - 2° dysmenorrhea
question
When does tenderness most likely occur in patients with adenomyosis?
answer
most common immediately before and during menses
question
What is the most likely diagnosis upon seeing cystic areas found within the myometrial wall and the uterus is symmetrically enlarged?
answer
Adenomyosis
question
What is the management for adenomyosis?
answer
LNG-IUS - levonorgestrel intrauterine system - T-shaped intrauterine device that secretes progesterone into the uterine cavity - decreases heavy menstrual bleeding Surgery - hysterectomy is the definitive treatment
question
Define menopause
answer
3 continuous months of cessation of menses and elevated gonadotropins ~52 years old
question
What is the most common cause of postmenopausal bleeding?
answer
vaginal or endometrial atrophy
question
BMI range
answer
formula = kg/m² 40: obesity class 3 (very severely obese)
question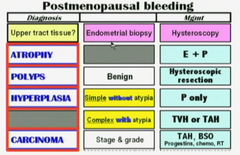
Synopsis: Postmenopausal bleeding steps of diagnosis and management
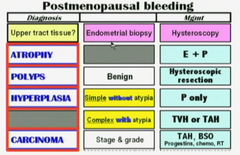
answer
Speculum exam: rule out vaginal lesions and cervical lesions Once ruled out... obtaining upper tract tissue: - endometrial biopsy - hysteroscopy and ultrasonography - send biopsy to pathology If finding is... atrophy: - management is estrogen with progestin polyps: - benign - hysteroscopic resection hyperplasia: - simple *without atypia: progestin treatment - complex *with atypia: total vaginal or abdominal hysterectomy carcinoma: - stage & grade - total abdominal hysterectomy + bilateral salpingo-oophorectomy (TAH-BSO) + lymph node dissection - according to staging and necessary radiation + chemotherapy
question
Most common cause of endometrial carcinomas?
answer
upposed estrogen without the stabilizing effect of progesterone
question
What are the major risk factors of postmenopausal bleeding?
answer
Obesity***: increased peripheral conversion of androgen to estrogen due to increased adipose tissue hypertension, diabetes mellitus (both points towards obesity) nulliparity: no kids means no exposure to the long period of progesterone during pregnancy; equal to possible unopposed estrogen chronic anovulation conditions (PCOS, etc.): no ovulation means no progesterone
question
What are some the diagnostic tests to confirm cause of postmenopausal bleeding?
answer
Endometrial sampling: - sampling process may miss diagnosis due to localized growth in the endometrium - example: dilatation and curettage of endometrial misses a small section where neoplastic growth is occurring Hysteroscopy: - with hysteroscope, cervical or endometrial polyps can be identified as cause of postmenopausal bleeding Ultrasound: - ultrasonography can be used to measure the thickness of the lining of the endometrium (postmenopausal patients should be <5mm)
question
What is the endometrial lining stripe measurement supposed to be for postmenopausal women?
answer
<5mm Ultrasound
question
Endometrial cancer: staging
answer
Most common cause of gynecological cancer Staging is surgical Stage I: spread limited to the uterus (most common stage at diagnosis) - IA: limited to the endometrium or invasion *less than 1/2 of myometrium* - IB: invasion *more than 1/2 of myometrium* Stage II: extension to teh cervix but not outside the uterus Stage III: Spread adjacent to teh uterus - IIIA: invades serosa or adnexa or positive cytology - IIIB: invasion of vagina - IIIC: invasion of pelvic or para-aortic nodes Stage IV: Spread further from the uterus - IVA: involves bladder or rectum - IVB: distant metastasis
question
What is the management of atrophy of endometrium induced postmenopausal bleeding?
answer
hormone replacement therapy estrogen + progestin
question
Endometrial cancer: management
answer
Stages I~IV: TAH-BSO + lymph node resection - TAH: total abdominal hysterectomy - BSO: bilateral salpingo-oophorectomy After surgery: radiation and chemotherapy - Stage I: none - Stage II: radiation - Stage III + IV: radiation + chemotherapy
question
What is the management for endometrial hyperplasia? What is the most common cause?
answer
Unopposed estrogen can cause hyperplasia of endometrium Simple hyperplasia with no atypia: progestin Complex hyperplasia, no atypia: progestin Complex hyperplasia with atypia: hysterectomy or progestin for non-surgical candidates Endometrial carcinoma: staging + TAH/BSO
question
Which types of hyperplasia can be managed with progestin?
answer
simple hyperplasia with no atypia complex hyperplasia with no atypia
question
How does complex hyperplasia histologically present? Complex hyperplasia with atypia?
answer
decreased stroma with increased glandular tissue atypia will show misshapen nucleus, etc.
question
What are some prevention methods of postmenopausal bleeding? Reproductive age women bleeding? Dietary?
answer
postmenopausal patient: - estrogen replacement therapy with progestin reproductive age women: - most likely due to chronic anovulation (PCOS, etc.) - progestin treatment Dietary - soy: 30~40% reduction of endometrial cancer risk
question
Tamoxifen association with vaginal bleeding
answer
Tamoxifen is used for breast cancer prevention by its estrogen antagonistic effects on the breast However, it has estrogen agonist effects on the uterus It can induce hyperplasia and endometrial polyps



