USMLE Step 1 – uWorld High Yield Notes – Flashcards
Unlock all answers in this set
Unlock answersquestion
What are the two major microtubular motor proteins? Which does anterograde axonal transport, which does retrograde axonal transport?
answer
Kinesin, Dynein Kinesin: Anterograde Dynein: Retrograde`
question
What do you think, immunologically speaking, when you see someone with recurrent Neisseria infections?
answer
Inability to form the membrane attack (MAC) complex this is a common complement deficiency
question
What is the defect in Chronic Granulomatous disease? What is the pathophysiology?
answer
NADPH Oxidase deficiency leads to the inability to kill intracellular organisms
question
Characteristic triad of ataxia telangiectasia?
answer
cerebellar ataxia, telangiectasias, increased risk of sinopulmonary infections
question
What is the major immune deficiency of ataxia telangiectasia?
answer
IgA deficiency, which predisposes to infections of the upper and lower airways (and other mucous membranes)
question
There's a useful mnemonic for Ataxia Telangiectasia and the gene that's mutated. What is it?
answer
ATM Ataxia Telangiectasia Mutated ATM gene is responsible for DNA break repair
question
What is one reason that lead intoxication causes hypochromic anemia?
answer
Mitochondrial iron transport is important for Heme synthesis! It's inhibited by lead. So you don't make heme in your mitochondria and you get hypochromic anemia.
question
What is the biochemical problem in Lesch-Nyhan syndrome? (And, only if you got that right, what are the really cool symptoms of it?)
answer
Defective purine catabolism, so buildup of purines. It's an X-linked recessive disorder with mutated HGPRT gene (hypoxanthine-guanine phosphoribosyltransferase, if you want to impress people). Now, if you got HGPRT and purine catabolism right, you can say: self-mutilating behavior on top of mental retardation, choreoathetoid (think Chorea) movements and spasticity.
question
What is the defect in Niemann-Pick disease? What causes that? What is the common macular finding?
answer
Sphingolipid degradation is defective Caused by an autosomal recessive defect in sphingomyelinase Cherry Spot on the macula? Niemann Pick's or Tay Sach's.
question
If a baby gets exposed to an unclean knife (...) and subsequently develops rigid paralysis, what is the diagnosis, where do we think this might happen, and how do we prevent it?
answer
Neonatal Tetanus Developing Countries Maternal immunization with tetanus toxoid is the best way to prevent it an adeuately immunized mom will transfer IgG's across the placenta to the neonate
question
Which microtubule associated protein aids in anterograde transport of intracellular vesicles and organelles? Which end of the microtubule do they go towards?
answer
Kinesin. Towards the (+) rapidly growing end.
question
What is an early BRAIN finding of Ataxia-Telangiectasia and how does it manifest itself?
answer
Cerebellar atrophy manifests as ataxia in the first years of life.
question
High yield path association for Alzheimer's disease?
answer
Neurofibrillary tangles in the neocortex
question
High yield path association for Parkinson's disease?
answer
Loss of neurons in the substantia nigra
question
High yield path association for Huntington disease?
answer
Atrophy of caudate nucleus
question
What are the major manifestations of Ataxia-telangiectasia?
answer
cerebellar ataxia, oculocutaneous tenlangiectasias, repeated sinopulmonary infections, and an increased incidence of malignancy
question
If you heard: amenorrhea, bitemporal hemianopsia, and enlargement of the pituitary gland on brain imaging, what would you be thinking?
answer
Prolactinoma, the most common pituitary adenoma.
question
What embryological layer is the anterior pituitary derived from?
answer
Surface ectoderm
question
What is the most common congenital abnormality associated with the use of Sodium Valproate during pregnancy?
answer
neural tube defects, e.g., meningocele because valproate inhibits intestinal folic acid absorption resulting in teratogenicity
question
What is the characteristic histology of a craniopharyngioma?
answer
On light microscopy, cysts are lined by stratified squamous epithelium, possibly with Keratin perals. Cysts are usually filled iwth a yellow, viscous fluid that's rich in cholesterol crystals.
question
Where do craniopharyngyomas arise from?
answer
Craniopharyngiomas are calcified cystic tumors that arise from remnants of Rathke's pouch (embryonic precuros of the anterior pituitary)
question
Failure of what process leads due neural tube defects? What can be seen in the amniotic fluid due to leakage of fetal cebebrospinal fluid?
answer
Failure of fusion of the neuropores. Alpha-fetoprotein and Acetylcholinesterase may appear in the amniotic fluid
question
Can a competent patient refuse healthcare? Can a competent patient refuse knowledge of their potential health situation?
answer
yes and yes
question
What is the consensus and professional standard regarding the receiving of gifts from patients?
answer
Don't do it. It's unethical to accept individual gifts from patients, especially of signficant value. AMA doesn't have clear cut answer, but they recommend careful consideration be used. some general guidelines: -cash gifts should never be accepted (this includes gift certificates) -a gift should never influence treatment -no specific dollar value is given; but as a rule of thumb, it shouldn't be above patient's or physician's means -psychiatrist must be super careful even with small gifts -maintain consistency among all patients -if physician would be embarrassed or uncomfortable if his colleagues found out about the gift, don't accept it
question
Is displacement a mature or immature defense mechanism? What is displacement?
answer
Immature. A patient redirects emotions from the person or object that's causing the emotions (e.g., wife), but who it woudl be completely unacceptable to direct those emotions toward, to a more acceptable, but still inappropriate, person or object (e.g., a wall or a vase).
question
Is sublimation a mature or immature defense mechanism? How does it work?
answer
Mature. Unacceptable drives are redirected toward completely acceptable targets. (Workout hard if you're angry)
question
Is projection a mature or immature defense mechanism? What is it?
answer
Immature. Unacceptable or personally disagreeable impulses are attributed to others; e.g., a student who wants to cheat on a test accuses his classmates of cheating. Or the gayness thing
question
Is reaction formation immature or mature defense mechanism? what is it?
answer
immature, where unacceptable feeligns are IGNORED and the opposite sentiment is adopted (forced). man who's mad at his wife instead compliments her dress
question
Is splitting a mature or immature defense mechanism? what is it?
answer
immature. frequently employed by patients with borderline personality disorder, everything is either "good or bad."
question
What do you do if you suspect child abuse? Ask the parents or call child protective services?
answer
Call Child Protective Services immediately!
question
Psychologically speaking, what phenomenon is "white coat syndrome" associated with?
answer
Classical Conditioning. In classical conditioning, a reflexive response normally elicited by an unconditioned stimulus becomes evocable by a second, formally neutral (conditioned) stimulus.
question
What three things can patients with bulimia develop (hint: one isn't weight loss because bulimia doesn't work.)?
answer
(1) bilateral partodi gland enlargement (2) erosion of tooth enamel* (3) irregular menses
question
What is the pulmonary capillary wedge pressure and what does it indirectly measure?
answer
Pressure in the pulmonary artey distal to the point of its occlusion by an inflated intravascular balloon. Since there's no significant blood flow towards the left atrium (LA) beyong this point of occlusion, the pressure at the tip of the "wedged" pulmonary artery catheter is an indirect measurement of LA Pressure.
question
What would we expect, in a normal patient, the relationship to be between LA and LV pressure during diastole?
answer
We would expect them to be nearly equale (both <12) since the open mitral valve offers minimal resistance to flow between the 2 chambers
question
What is the characteristic finding via cardiac catheterization in a patient with mitral valve stenosis? I.e., if we see what value elevated while the other remains normal, when do we think "Mitral Valve Stenosis."
answer
Cardiac Catheterization will reveal a LA end diastolic pressure (via pulmonary capillary wedge pressure) that is significantly greater than the LV end diastolic pressure (LVEDP). This abnormal pressure gradient implies increased resistance to flow between the LA and LV, i.e., mitral valve stenosis.
question
Summarize the key points of pulmonary capillary wedge pressures (PCWP) and how it helps us diagnose mitral valve stenosis.
answer
The Pulmonary capillary wedge pressure (PCWP) measures LAEDP. Under normal conditions, the LAEDP is nearly equal to the LVEDP. Mitral stenosis eleveates the LAEDP and PCWP relative to the LVEDP.
question
Generally speaking, regarding blood flow through our vessels, the law of conservation of mass states that the total flow of mass into a contained system must be equal to the total outflow of mass from that system in a steady state. What equation helps us prove the following condition: to maintain a constant fluid flow througha tube with varying diametes, how are cross-sectional area and flow velocities related?
answer
Volume in must equal volume out, right? Vol(in) = A1 * V1 ; Vol(out) = A2*V2 So any rearrangement of that equation holds true in a physiological system. A2 = A1*V1 / V2 for example, works. This applies for blood flow in the cardiovascular system.
question
What do you think when you hear a patient who has a heart murmur presenting with the following physical exam findings: Bounding femoral pulses, carotid pulsations accompanied by head-bobbing.
answer
Aortic Regurgitation
question
How does the pathophysiology of aortic regurgitation explain the characteristic findings of these patients? And what are those findings again (2 major ones)?
answer
(1) Bounding femoral pulses; (2) Carotid Pulsations with head-bobbing (de Musset sign) There is a large LVSV, a large regurgitant SV, and a large pulse pressure. Bounding femoeral and carotid pulses marked by abrupt distention and quick collapse ("water hammer" pulses) are the result of large pulse pressure the head bobbing is due to the transfer of mementum from htel arge left ventricular stroke volume to the head and neck
question
What is the order of cardiac tissue conduction velocity from *fastest* to *slowest*?
answer
Purkinje System Atrial Muscle Ventricular Muscle AV node
question
What is the mnemonic to help you remember the order of cardiac tissue conduction velocity?
answer
P ark (purkinje's) AT (atria) VENT ura (ventricles) AV enue (AV node)
question
Where does Atrial Natriuretic Peptide (ANP) come from? In response to what?
answer
Atrial Cardiomyocytes in response to atrial stretch, it is a signifier of volume expansion
question
What is the ultimate action of ANP?
answer
Lowers blood pressure through peripheral vasodilation, natriuresis, and diuresis.
question
How does ANP affect the following organs: (1) kidney? (2) adrenal gland? (3) blood vessels?
answer
(1) Dilates the afferent arterioles, increasing GFR and urinary excretion of sodium and water (diuresis); also limits sodium reabsorption (in proximal tubule) and inhibits renin secretion (2) restricts aldosterone secretion --> increase in sodium and water excretion by the kidneys (3) relaxes vascular smooth mucles, producing vasodilation; also increases capillary permeability, leading to fluid extravasation to the interstitium and a decrease in circulating blood volume
question
What major hormone comes from the renal juxtaglomerular cells, and what is its net effect on the vasculature?
answer
Renin, which catalyzes angiotensinogen --> ang I angiotensin causes vasoconstriction, increased blood pressure, and aldosterone release
question
What is the pathophysiology of CHF in general terms?
answer
CHF occurs when the heart is unable to pump sufficient amounts of blood to meet body's metabolic demands
question
How is the reduced cardiac output in CHF initially detected? How does the body attempt to compensate?
answer
A drop in blood pressure Compensatory neurohormonal stimulation that is directed at maintaining blood pressure and tissue perfusion Chiefly mediated through: (1)increased sympathetic nervous system activity, (2)stimulation of the renin-angiotensin-aldosterone pathway, (3) release of ADH
question
What are the adverse consequences of the body's adaptations to CHF? There are 3 major ones to keep in mind.
answer
(1) increased afterload from excessive vasoconstriction (2) excess fluid retention (3) deleterious cardiac remodeling, which perpetuates a downward spiral of progressive cardiac deterioration
question
What is the most common cause of heart failure in developed countries?
answer
repeated bouts of myocardial ischemia
question
When do we most commonly (or typically for Step 1) hear an S3 ventricular gallop?
answer
in patients with left ventricular systolic failure or restrictive cardiomyopathy
question
When does S3 heart sound happen?
answer
immediately following S2 during phase of rapid passive ventricular filling
question
How do we best auscultate an S3 gallop?
answer
with the bell of the stethoscope at the ventricular apex
question
What 2 physical examination maneuvers can help bring out an S3 more audibly?
answer
(1) lying the patient in a left lateral decubitus position (2) ask the patient to exhale completely while in that position by decreasing the volume of the lungs and bringing heart closer to the chest wall
question
Summarize the key facts of the S3 sound or S3 gallop.
answer
An S3 sound is a low frequency sound that can be physiologic in younger individuals, but typically pathologic in older adults. In older adults, it results from left ventricular systolic failure or restrictive cardiomyopathy. The S3 sound can be accentuated by having the patient lie in the left lateral decubitus position and fully exhale.
question
What are the characteristic ECG findings of a patient in A-fib?
answer
(1) absent P waves replaced with chaotic f (fibrillatory) waves (2) irregularly irregular R-R intervals (3) narrow QRS complexes
question
What causes ventricular contraction rate in a patient in atrial fibrillation?
answer
Atrial fibrillation occurs due to irregular, chaotic electrical activity within the atria Some of the atrial impulses are transmitted to the ventricles, but most are not. this is due to the AV nodal refractory period.
question
What three pathologies do we associate a holosytolic murmur with?
answer
(1) tricuspid regurgitation (2) mitral regurgitation (3) ventricular septal defect
question
Does more or less blood return to the right heart during inspiration? Why?
answer
More blood returns because during inspiration intrathoracic pressure drops, allowing more blood to return to the right heart
question
How do we differentiate a holosystolic murmur? I.e., how do we know if it's tricuspid valve regurgitation vs. mitral regurgitation vs. ventricular septal defect?
answer
A tricuspid regurgitation murmur would be expected to increase in intensity during inspiraiton, while the other two would not
question
Summarize the cardiac findings in a patient with a tricuspid valve regurgitation.
answer
A holosystolic murmur that increase in intensity on inspiration most likely represents tricuspid regurgitaiton.
question
How do arterial baroreceptors monitor systemic blood pressure?
answer
Baroreceptors sense arterial wall stretch, which is an indicator of systemic pressure in arterial circulation. When stimulated by: (1) stretch: nerves innvervating those baroreceptors increase firing --> blood pressure decrease through peripheral vasodilation and decreased cardiac output (2) hypotension: decreased baroreceptor signaling --> releases inhibition of vasoconstrictor center and increases blood pressure
question
Which two nerves monitor the baroreceptors in the neck?
answer
Glossopharyngeal nerve (IX) & Vagus nerve (X)
question
Which two anatomical landmarks are important loctaions of barroreceptors that are especially important in blood pressure control?
answer
(1) the carotid sinus [located just above the bifurcation of the common carotid artery] (2) the aortic arch
question
Which nerve innervates the baroreceptors of the aortic arch?
answer
the vagus nerve; fibers from the baroreceptors run within the vagus nerve (X)
question
Which nerve is more associated with the carotid sinus? How is it associated, and what is the name of the actual nerve / who is that nerve a branch of?
answer
(1) glossopharyngeal nerve (2) AFferent fibers from the carotid sinus stretch receptors form a small carotid sinus nerve called HERING'S NERVE, which is a branch of the glossopharyngeal nerve
question
Where do all of our important baroreceptor nerves terminate? I.e., fibers from the aortic arch baroreceptors and the carotid sinus baroreceptors send their fibers to what brain structure?
answer
the solitary nucleus of the medulla
question
Describe the net impact on Mean Arterial Pressure (MAP) of exercise on exercising muscle.
answer
There is only a modest blood pressure increase! this is because of peripheral vasodilation to skeletal muscle within the muscle significantly decreases the total systemic vascular resistance.
question
In what condition do where hear a "snap" followed by a rumbling diastolic murmur, best heard over the cardiac apex?
answer
Mitral Stenosis Opening snap results from abrupt halting of motion of the stenotic mitral valve leaflets during MITRAL VALVE OPENING (visualize where that is on a pressure-volume curve) [the point between isoblumetric relaxation and diastolic filling] the diastolic murmur is the result of turbulent blood flow through the stenotic mitral valve during LEFT ATRIAL CONTRACTION
question
What is the most common cause of mitral valve stenosis?
answer
Prior rehumatic carditis
question
What is the classic physical exam finding in mitral valve stenosis best heard over the apex of the heart?
answer
MItral valve stenosis has a characteristic opening snap followed by a diastolic rumbling murmur.
question
What are the two important formulae for cardiac output? What principle underlies the second?
answer
(1) CO = Stroke Volume * Heart Rate (2) Oxygen Consumption / Arteriovenous O2 difference *the second formula is explained by Fick's principle; it states that the cardiac output is equal to the oxygen consupmtion by the tissues divided by Arteriovenous Oxygen difference
question
What kinds of methods, invasive or noninvase, are used to assess the necessary parameters (O2 consumption, arteriovenous O2 difference) to determine cardiac output by Fick's principle?
answer
Invasive methods
question
When is the myocardium best perfused with blood? (this is a unique property of myocardium)
answer
DIASTOLE The coronary circulation is unique in that only 10% of total perfusion through the myocardial capillaries of the left ventricle occurs during systole (contraction of the muscular left ventricle compresses the coronary arteries!) The great majority of blood flow through the vascular beds supplied by the coronary arteries to the LV occurs during diastole, when the blood vessels are not compressed by myocardial contraction
question
What area of the heart is most prone to ischemia and myocardial infarction and why?
answer
The Left Ventricular subendocardial myocardium, because the systolic reduction in coronary blood flow in this region is the greatest
question
What are the two most important factors that metabolically autoregulate coronary blood flow?
answer
Adenosine and Nitric Oxide (NO)
question
Which of the two major metabolites that regulates coronary blood flow works more on small coronary arterioles?
answer
Adenosine
question
Which of the two major metabolites that regulates coronary blood flow works more on large arteries and pre-arteriolar vessels of the heart?
answer
Nitric Oxide
question
How does nitric oxide act within vascular smooth muscle to affect vasodilation?
answer
Nitric Oxide acts within smooth muscle with a soluble guanylate cyclase enzyme to INCREASE PRODUCTION OF CYCLIC GMP and CAUSE SMOOTH MUSCLE RELAXATION
question
Does neuronal input typically have a strong impact on coronary circulation?
answer
no. nervous input generally has very little effect on coronary blood flow (so NE, Ach, etc. doesn't have a lot to do with coronary flow... what does? adenosine for small arterioles, NO for larger vessels)
question
What type of drug, generally speaking, is Verapamil? I.e., what is it's mechanism of action?
answer
Verapamil is a calcium channel blocker
question
Why does verapamil only exhibit a minimal effect on skeletal muscle?
answer
Skeletal muscle does NOT require calcium to enter from the extracellular space to cause calcium release from within the cell. [review of skeletal muscle contraction: Calcium released from the sarcoplasmic reticulum binds to Troponic C allowing actin and myosin to bind. ATP bound to myosin is then hydrolyzed and contraction occurs]
question
What properties of cardiac muscle make it a better target for calcium channel blockers such as verapamil?
answer
In cardiac muscles, the L-type channel-RYR mechanical coupling mechanism DOES NOT EXST. In cardiac muscle, depolarization causes L-type calcium channels on the plasma membrane to open and allow influx of EXTRACELLULAR CALCIUM. This calcium then binds to and activates sarcoplasmic RyR-2 channels by a mechanism known as calcium-induced-calcium-release, which then allows calcium to move out of hte sarcoplasmic reticulum. [contraction then proceeds in a similar manner to that seen in skeletal muscle: Calcium binds to Troponin-C allowing actin and Myosin to bind, ATP bound to myosin is then hydrolyzed and contraction occurs]
question
Medically speaking, how do we define palpitations? [I.e., not just a black woman saying "You give me heart palpitations."]
answer
subjective sensation and awareness of one's own heart beating
question
What is the most common cause of palpitations?
answer
anxiety. this was in there to remind you to THINK and not just "take the test"
question
Whenever you hear "irregularly irregular," you should think of the most common chronic arrhythmia, which is what?
answer
Atrial Fibrillation
question
What are some important precipitating factors for isolated episodes of a-fib?
answer
(1) binge alcohol consumption ("holiday heart syndrome") (2) increased cardiac sympathetic tone (3) pericarditis
question
What are the ECG hallmarks of A-Fib?
answer
(1) absent p-waves (2) irregularly spaced ventricular contractions (3) variable r-r intervals (showing (2))
question
What is the most common paroxysmal tachycardia, and what is its common pathophysiology?
answer
Paroxysmal supraventricular tachycardia (PSVT) PSVT typically results from a re-entrant impulse traveling through slowly and rapidly conducting segments of the AV node
question
What are some simple maneuvers to treat PSVT?
answer
carotid sinus massage and valsalva maneuver both of these increase cardiac parasympathetic tone the parasympathetic nervous system primarly functions to slow the heart rate by slowing conduction through the AV node
question
How does the parasympathetic nervous system primarily function to slow the heart rate?
answer
Slowing conduction through the AV node
question
How does carotid sinus massage help a person in PSVT recover?
answer
The nerves innervating the carotid sinuses are constantly firing; when pressure at the carotid bodies increases, the number of impulses sent to the CNS also increases Carotid sinus massage increases carotid sinus baroreceptor firing (involving cranial nerve IX, not X like the aortic arch), thus increasing parasympathetic influence on the heart and vessles this ultimately prolongs the AV node refractory period which stops AV re-entrant tachycardias
question
What is the clinical picture of congestive heart failure? What is the super general pathophysiology?
answer
Dyspnea, edema, and fatigue poor cardiac output
question
What are early responses by our body makes to combat CHF? How do these cause further problems?
answer
Inadequate visceral perfusion causes activation of the sympathetic nervous system and the renin-angiotensin-aldosterone system Both the Sympathetic NS and the RAS system are meant to increase cardiac output, but their effect on the diseased heart is to cause an inappropriately high AFTERLOAD and CIRCULATING VOLUME this leads to progressive heart disease
question
Where does our body synthesize ACE? What does ACE stand for?
answer
Lung endothelium Angiotensin-converting-enzyme (Ang I --> Ang II)
question
How, physiologically speaking, is cardiac relaxation achieved, which is best detected by a rapid decrease in cytoplasmic calcium levels?
answer
Relaxation occurs subsequent to calcium efflux from the cytoplasm, which is accomplished through the use of : Calcium-ATPase and Na+/Ca2+ exchange mechanisms the Ca2+ ATP-ase pump uses active transport to sequester calcium in the sarcoplasmic reticulum and re-establish ion gradient the sarcolemmal Na+/Ca2+ transmembrane protein does not require ATP and acceps three Na+ ions in exchange for one intracellular Ca2+ ions
question
So, summarize the two important ways cardiac myocyte relaxation is accomplished.
answer
Calcium efflux, governed by the use of Ca2+-ATPase and Na+/Ca2+ exchange mechanisms
question
What does the Frank-Starling effect state?
answer
As cardiac muscle is increasingly stretched (by venous return), the cardiac output increases (up to a limit). [This is essentially the same length-tension relationship that is seen in skeletal muscle]
question
What would we expect in terms of cardiac output in a patient with chronic anemia?
answer
Cardiac output increases in an effort to meet the metabolic demands of the tissues
question
What would we expect in anaphylaxis in terms of venous return and cardiac output?
answer
Anaphylaxis causes widespread venous and arteriolar dilation along with increased capillary permeability and third-spacing of fluids this results in a serious drop in venous return cardiac contractility is also increased as the body attempts to maintain blood pressure
question
How does acetylcholine and adenosine influence cardiac pacemaker cells, particularly at Phase 4 (pacemaker potential)?
answer
Ach and adenosine reduce the rate of spontaneous depolarization in cardiac pacemaker cells
question
What is unique to cardiac muscle actions potentials, and what channel mediates it?
answer
Plateua, characterized by the opening of L-type dihydropyridine-sensitive Ca++ channels and the closure of some K+ channels thus, the membrane becoems highly permeable to Ca++ ions and minimally permeable to K+ ions
question
What are the 4 phases of a cardiac myocyte action potential?
answer
Phase 0: rapid depolarization Phase 1: intial rapid repolarization Phase 2: plateua Phase 3: late rapid repolarization Phase 4: resting potential the action potential is associated with increased membrane permeability to Na+ and Ca++ and decreased permeability to K+
question
What is the major limiting factor for coronary blood flow?
answer
the duration of diastole most of the blood supply to the heart occurs during diastole and the duration or length of diastole is a critical factor in determining coronary blood flow
question
What heart defect classically has a continueous murmur?
answer
Patent Ductus Arteriosus
question
What heart defect is classically heard with a Patent Ductus Arteriosus? Where do we best auscultate it?
answer
PDA is associated with a continuous murmur best heard at the left infraclavicular region with maximal intensity at S2
question
What patients are at greatest risks of PDA?
answer
Kids born prematurely Kids with cyanotic Heart Disease
question
What is the classic cardiac finding in Mitral Valve Prolapse?
answer
Mitral Valve Prolapse classically results in a midsystolic click and mid-to-late systolic murmur
question
From a cardiac pathophysiology standpoint, summarize patent ductus arteriosus.
answer
PDA is characterized by a continuous murmur heard best in the left infraclavicular region with maximal intensity at S2. A small PDA is often asymptomatic and detected incidentally during routine cardiac auscultation. It occurs most commonly in patients born prematurely and those with cyanotic congenital heart disease.
question
How do natriuretic peptides (BNP and ANP) work?
answer
they cause vasodilation, diuresis/natriuresis (as their name suggests...), and a decrease in blood pressure they counteract: endothelin sympathetic effects angiotensin II
question
How can atrial fibrillation precipitate sudden heart failure?
answer
the sudden loss of the contribution of normal atrial contraction to ventricular filling (loss of the atrial systolic kick) decreases LV preload (end diastolic volume)
question
What is the classic cardiac finding of mitral stenosis again?
answer
Opening snap followed by rumbling murmur.
question
So what is the best auscultatory indicator of the severity of mitral stenosis (MS)?
answer
The length of the interval between S2 and the opening snap. The shorter the interval, the more severe the stenosis
question
What condition do we associate an extra low-frequency heart sound at the end of diastole just before S1 (known as S4) with?
answer
Left Ventricular hypertrophy... sounds like ba-dum BUM, ba-dum BUM, ba-dum BUM, etc. [may also occur in restrictive cardiomyopathy]
question
What is the phenomenon of hibernating myocardium, and how does it explain why coronary artery bypass grafting is an effective treatment of a failing left ventricle?
answer
Repetitive ischemia of cardiac myocytes or persistent hypoperfusion of myocytes can result in a chronic, but reversible, loss of contractile function that's HIBERNATION
question
What is the characteristic cardiac finding on auscultation of ventricular septal defect?
answer
low-pitched holosytolic murmur heard best at the left sternal border with accentuation during the hand-grip exercise the hand-grip maneuver accentuates it because of increased afterload, which results in an increase in the movement of blood from the left ventricle to the right ventricle across the VSD
question
What are korotkoff sounds?

answer
blood pressure sounds
question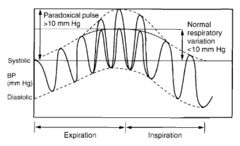
What is pulsus paradoxus, and what disease do we associated it with?
answer
Pulsus Paradoxus is defined by a decrease in systolic blood pressure of greater than 10 mmHg with inspiration, and is detected by inflating a blood pressure cuff above systolic pressure and then SLOWLY releasing it [just buzzword cap'd there] as the kuff is deflated, korotkoff sounds first become audbile during expiration and subsequently become audible during all phses of respiration Inspiration causes increase in systemic venous return... so normally, this results in expansion of right ventricle into the pericardial space with little impact on the left side of the heart in conditions that impair expansion into the pericardial space [PERICARDIAL DISEASE], the increased right ventricular volume pushes the interventricular septum to the left therefore, the left heart diastolic volume and stroke volume are reduced, resulting in decreased systemic blood pressure during inspiration and hence pulsus paradoxus
question
Okay, short version. What is pulsus pardoxus? A disease of what heart layer causes it?
answer
Decreased systolic blood pressure during inspiration. Pericardial Disease.
question
What are acute asthma exacerbations treated with?
answer
Beta-adrenergic Agonists
question
How do beta-agonsists work? Why is this effective in acute asthma exacerbations?
answer
Beta-agonists produce relaxation of bronchial smooth muscle by stimulating beta-2 receptors, which si a Gs protein-coupted receptor that activates adenylyl cyclase and increases intracellular cAMP concentrations
question
Simply put, how do beta-agonists treat asthma attacks?
answer
by causing bronchial smooth muscle relaxation by increasing intracellular cAMP
question
What ist he classic auscultatory findings in mitral regurigtation?
answer
Blowing, holosystolic murmur heard best over the apex with radiation to the axilla
question
What is a very common cause of mitral regurgitation in developing countries? And what is the classic auscultatory finding for mitral regurgitation?
answer
Rheumatic Heart Disease A blowing, holosystolic murmur heard best of the cardiac apex that radiates to the axilla
question
What is the characteristic blood pressure of a patient with aortic regurgitation?
answer
Abnormally large (wide) pulse pressure is caused by aortic regurgitation, and is responsible for many of the symptoms of Aortic Regurgitation
question
What is the syndromic name given to a condition in which an accessory AV conduction pathway is used [i.e., the AV node is bypassed and something else sets heart rhythm]?
answer
Wolff-Parkinson-White syndrome
question![What is the characteristic triad of abnormalities corresponding to ventricular pre-excitation [due to Wolff-Parkinson-White syndrome]? What is the characteristic triad of abnormalities corresponding to ventricular pre-excitation [due to Wolff-Parkinson-White syndrome]?](https://studyhippo.com/wp-content/uploads/2018/03/what-is-the-characteristic-triad-of-abnormalities-corresponding-to-ventricular-pre-excitation-due-to-wolff-parkinson-white-syndrome.jpg)
What is the characteristic triad of abnormalities corresponding to ventricular pre-excitation [due to Wolff-Parkinson-White syndrome]?
![What is the characteristic triad of abnormalities corresponding to ventricular pre-excitation [due to Wolff-Parkinson-White syndrome]? What is the characteristic triad of abnormalities corresponding to ventricular pre-excitation [due to Wolff-Parkinson-White syndrome]?](https://studyhippo.com/wp-content/uploads/2018/03/what-is-the-characteristic-triad-of-abnormalities-corresponding-to-ventricular-pre-excitation-due-to-wolff-parkinson-white-syndrome.jpg)
answer
(1) shortened PR-interval (2) delta wave at the start of the QRS complex (3) widened QRS interval
question
What is the classic cardiac auscultation finding in aortic stenosis?
answer
A Harsh, crescendo-decrescendo systolic ejection murmur heard at the right sternal border
question
Where do we hear the class cardiac auscultation finding in aortic stenosis? [and what does it sound like]
answer
The right sternal border harsh, crescendo-decrescendo systolic ejection murmur
question
What are the 3 main causes of valvular aortic stenosis?
answer
(1) Congenitally abnormal valve with calcification --e.g., a bicuspid aortic valve (2) a calcified normal valve (3) rheumatic heart disease N.B. rheumatic heart disease is most common cause worldwide, calcific aortic valve disease is more common in U.S.
question
A patient has deep venous thrombus and develops a stroke. What type of embolus is this? Why?
answer
A Paradoxical embolus, because it originated in the venous system but crossed over into the arterial circulation (bypassing the lungs)
question
What does a paradoxical embolism usually indicate, generally speaking?
answer
That there is some abnormal connection between the right and left heart, allowing the DVT to cross over from the venous system to arterial system bypassing the lungs.
question
What classic heart defect would allow a DVT to become a paradoxical embolus leading to a stroke in a patient?
answer
Atrial Septal Defect
question
So a patient presents with a stroke after a DVT was confirmed in his legs. You astutely recognize that since this is a stroke it must be from a paradoxical embolus, and begin to think "this gal must have an ASD, a common abnormal connection between the right heart and left heart that would let the embolus become paradoxical." Then, you confirm this on physical exam by hearing what?
answer
Wide splitting of S2 that does not vary with respiration.
question
What is the cardiac auscultatory finding in atrial septal defect?
answer
Wide splitting of S2 that does not vary with respiration.
question
What is the pathophysiology / pathology of tetralogy of Fallot (ToF)?
answer
PROVe it (1) Pulmonary artery stenosis (2) RVH (3) Overriding aorta (overrides the VSD) (4) VSD
question
How does squatting improve the symptoms in a patient with Tetralogy of Fallot?
answer
Compresses the femoral arterites, increases total peripheral resistance thereby decreasing the R --> L shunt and direction more blood from the RV to the lungs compression-->resistance-->pressure
question
Again, how does squatting improve symptoms in Tetralogy of Fallot patients?
answer
Squatting increases Systemic Vascular Resistance (Total Peripheral Resistance) and decreases R to L shunting, thereby increasing pulmonary blood flow. Squatting thus counteracts arterial desaturation during hypoxemic spells
question
How does the heart myocardium normally support its own blood flow in coronary artery disease?
answer
Coronary vessel occlusion can be bypassed by the natural existence and compensatory recruitment of collateral vessels that help support blood flow I.e., collateral circulation helps to alleviate ischemia and preserve myocardial function
question
What types of drugs could potentially worsen myocardial ischemia?
answer
Coronary Arteriolar Dilators (e.g., Adenosine and Dipyridamole)
question
How could coronary arteriolar dilators worsen myocardial ischemia? What is this phenomenon called?
answer
Collateral microvessels form adjacent pathways for blood flow to areas distal to an occluded vessel. Adenosine and dipyridamole are selective vasodilators of coronary vessels that can cause the phenomenon of CORONARY STEAL in which blood flow in ischemic areas is reduced due to arteriolar vasodilation in nonischemic areas I.e., coronary steal can lead to hypoperfusion and worsening of existing ischemia
question
In a patient with an isolated diastolic heart failure (due to smoking, perhaps), what would we expect to see regarding these three parameters: (1) LVEDP (2) LVEDV (3) LVEF
answer
(1) Increased (2) Normal (3) Normal [Diastolic heart fialure is characterized by a decrease in ventricular diastolic compliance but normal ventricular contractile performance. As a result, LVEDP must be increased in order to achieve a normal LVEDV and stroke volume.]
question
So what do we think if we hear "heart failure with normal ejection fraction?"
answer
Some kind of a diastolic heart failure.
question
[This is a friendly but stern reminder to learn what a JVP looks like on a graph... FirstAID.] What is the first peak on a JVP tracing? When is it notably absent?
answer
The "a wave," which is generated by atrial contraction. This is notably absent in patients with atrial fibrillation.
question
What is the classic murmur of aortic stenosis?
answer
Systolic ejection-type, crescendo-decrescendo murmur that starts after the first heart sound and typically ends before the A2 component of the second heart sound.
question
What is the intensity of the Aortic Stenosis murmur proprotional to?
answer
The magnitude of the left ventricle-to-aorta pressure gradient during systole [measured via catheter]
question
What aspect of Tetralogy of Fallot determines the degree of right-to-left intracardiac shunting and thus hypoxemic symptom severity?
answer
The Degree of R.V. outflow tract obstruction, i.e., the degree of pulmonic stenosis PROVe *Pulmonary Stenosis* RVH Overriding Aorta VSD
question
What is the best, most reliable way to quantify the severity of aortic regurgitation?
answer
2D and Doppler Echocardiography
question
What is the classic auscultatory finding of mitral regurgitation? What is the best physical exam finding indicator of the severity of mitral regurgitation?
answer
A holosystolic murmur that radiates to the axilla. The presence of an audible S3; i.e., the best indicator of a high regurgitant volume indicating severe Mitral Regurgitation with left ventricular volume overload is the presence of a left ventricular S3 gallop
question
What does not correlate well with the severity of Mitral Regurgitation?
answer
Intensity of a holosytolic murmur that radiates to the axilla; it does not correlate well with regurgitatnt volume
question
What is the classic murmur of aortic regurgitation?
answer
Early diastolic, high-pitched and blowing decresendo murmur heard best at the left sternal border
question
What physical exam maneuvers help bring about an aortic regurgitation murmur?
answer
Have the patient lean forward (brings the valve close to the chest wall) and at end expiration (listening during expiration often accentuates left-sided heart murmur)
question
Summarize an Aortic Regurgitation Murmur.
answer
The murmur of AR is a diastolic decrescendo murmur, heard loudest in early diastole when the pressure gradient between the aorta and the left ventricle is maximal. The murmur of AR is typically best heard at the left sternal border with the patient leaning forward and at end expiration.
question
What is the clinical term for RVH (with or without congestive right heart failure) caused by pulmonary hypertension?
answer
Cor Pulmonale
question
In what heart condition do we hear the Ken-Tuck-y murmur?
answer
It's a classic S3, which may be normal in young patients and in well-trained athletes. In older adults, though, it's typically a sign of left ventricular failure So will have patients of exertional dyspnea and difficulty sleeping
question
What do the auscultatory findings of a patient with Left Ventricular Failure reflect?
answer
The S3 sound of left heart failure is the result of increased left ventricular end-systolic pressure; i.e., it's not pumping enough blood out of the LV
question
Given abrupt onset of total myocardial ischemia, how long does it take to lose cardiomyocyte contractility?
answer
60 seconds.
question
How long can we tolerate ischemia before it leads to irreversible heart damage?
answer
30 minutes [due to myocardial stunning] after 30 minutes of total ischemia, the injury becomes irreversible
question
What is a major hemodynamic finding indicative of mitral regurgitation?
answer
Abnormally prominent (regurgitant) left atrial V-wave during catheterization Left Atrial Pressure increases more than you would think towards the end / after systole
question
In a patient with relatively acute aortic regurgitation, what is the major hemodynamic adaptation that maintains cardiac output?
answer
An increase in the left ventricular end diastolic volume (LVEDV) in association with ECCENTRIC left ventricular hypertrophy
question
In the heart, when do we see eccentric hypertrophy, and when do we see concentric hypertrophy?
answer
Eccentric: with volume overload (e.g., in chamber dilation de to increased end diastolic volume Concentric: pressure overload (e.g., in aortic stenosis or systemic hypertension)
question
Generally speaking, what is cardiac tamponade?
answer
Cardiac tamponade is pressure on the heart muscle which occurs when the pericardial space fills up with fluid faster than the pericardial space can stretch
question
What can cause cardiac tamponade?
answer
hypothyroidism, physical trauma, pericarditis, iatrogenic trauma, myocardial rupture
question
What is the classic triad (Beck's Triad) of cardiac tamponade?
answer
(1) hypotension (2) distended neck veins (3) distant or muffled heart sounds
question
Pathologic ventricular hypertrophy is accompanied not only by morphologic changes, but by chanes in gene transcription patterns as well. When there is prolonged hemodynamic overload, there may be abnormal up-regulation or re-expression of fetal proteins fromboth atrial and ventricular myoctyes. What type of mRNA might ventricular myocytes express that is typically only expressed in atrial myocytes?
answer
mRNA for natriuretic peptides. The main learning point is in the question stem here.
question
How, in a physical sense, do we describe peripheral resistance in the total body circuit? What about circulation in an individual organ? What impact does that have on resistance and calculating resistance?
answer
Total body circulation is best described as a parallel circuit, whereas circulation in an individual organ is often best described by a series arrangement Total body / parallel: 1 / TPR = 1/R1 + 1/R2 + 1/R3.... In an organ: TPR = R1+R2+R3.....
question
what is the treatment of choice for diabetic ketoacidosis?
answer
Intravenous hydration with normal saline and insulin
question
How does I.V. hydration with normal saline and insulin help a person in diabetic ketoacidosis?
answer
decrease in: serum glucose, osmolality, and potassium Increase in: serum bicarbonate sodium
question
How do we relate blood flow and vessel radius?
answer
Blood flow is directly related to the vessel radius raised to the fourth power. Resistance to blood flow is inversely proportional to the vessel radius raised to the fourth power.
question
What are 3 specific features that distinguish heart circulation from the blood flow provided to skeletal muscle and viscera? (this is a pretty vague question so if you don't get it, just be sure to read the 3 points on the back)
answer
(1) Heart muscle is perfused during diastole and consumes approximately 5% of cardiac output (2) The myocardial oxygen requirement is very high [heart has a capillary density far exceeding that of skeletal muscle, and oxygen extraction from arterial blood is very effective within the heart: resting myocardium extracts 75% to 80% of oxygen from the blood, while myocardium at work extracts up to 90% of oxygen from the blood] (3) Coronary flow is regulated by local metabolic factors, including hypoxia and adenosine accumulation
question
What organ is associated with max oxygen extraction from the blood?
answer
the heart
question
What is more related to the likelihood of a plaque causing acute coronary syndrome: Plaque Size or Plaque Stability?
answer
Plaque Stability
question
How to atherosclerotic plaques achieve max stability?
answer
Plaque Stability depends significantly on mechanical strength o the fibrous cap.
question
How can macrophages reduce plaque stability?
answer
Inflammatory macrophages in the intima may reduce plaque stability by secreting METALLOPROTEINASES, which degrade collagen.
question
Describe the pathogenesis of atherosclerosis.
answer
Pathogenesis of atherosclerosis is thought to begin with endothelial cell injury in the response-to-injury model, chronic endothelial cell injury may result from hypertension, hyperlipidemia, smoking, diabetes, homocysteine, toxins (alcohol), viruses, and/or immune reactions Such injury results in endothelial cell dysfunction and/or exposure of subendothelial collagen Endothelial cell dysfunction results in increased permeability as well as monocyte and lymphocyte adhesion and migration into the intima Endothelial cell denudation (fancy name for exposure of collagen) promotes platelet adhesion Growth factors produced by monocytes and platelets stimulate medial smooth muscle cell migration into and proliferion in the intima Increased endothelial cell permeability allows LDL cholesterol into the intima, where it is phagocytosed by the accumulating macrophages and SMCs to produce FOAM CELLS
question
Wow, simply put, describe atherosclerosis.
answer
atherosclerosis is initiated by repetitive endothelial cell injury, which leads to a chronic inflammatory state in the underlying intima of large elastic arteries as well as large and medium-sized muscular arteries.
question
What compensatory mechanism can develop in the body to avoid edema in the context of cor pulmonale (right sided heart failure due to long standing pulmonary HTN)?
answer
When the central venous pressure (CVP) is increased as in right heart failure, the interstitial fluid pressure rises due to an increase in net plasma filtration. As interstitial fluid pressure increases, compensatory increase in LYMPHATIC DRAINAGE allows for avoidance of edema.
question
What cell provides major proliferative stimuli for the cellular components of atherosclerotic plaques? How / what are these components?
answer
Platelets release PDGR, which promotes migration of SMC from the media into the intima and their subsequent proliferation in the intima.
question
A more concise look than above at the pathogenesis of atherosclerotic plaques (atheromas) please?
answer
Atherosclerotic plaques (atheromas) develop like this: endothelial cell injury exposes subendothelial collagen. This promotes platelet adhesion, aggregation, and release of factos that promte migration of smooth muscle cells (SMCs) from the media into the intima, as well as SMC proliferation. 2 important factors are PDGF and TGF-beta, both released by platelets.
question
What causes isolated systolic hypertension in elderly patients?
answer
decrase in the compliance of the aorta and its proximal major branches
question
What cell types directly cause intimal changes and damage in the formation of atherosclerotic plaques?
answer
Smooth Muscle cells The vascular reaction to endothelial and intimal injury is intimal hyperplasia and fibrosis, predominantly mediated by reactive smooth muscle cells that migrate from the media to the intima
question
What types of defects in hematology, platelet or clotting factor, are more assocaited with hemarthroses? Which type is associated with small petechial lesions on the skin?
answer
Hemarthroses: clotting factor defect / coagulopathy Small Petechial Lesions of the skin: platelet defects
question
What are teh 2 major effects of Carbon Monoxide (CO) on oxygen delivery to tissues?
answer
(1) it binds to hemoglobin with an affinity 250x that of Oxygen, reducing the number of heme binding sites available to oxygen (CO-bound hemoglobin is called CARBOXYHEMOGLOBIN). By decreasing the fraction of hemoglobin available for oxygen binding, CO decreases the oxygen content of blood. (2) CO poisoning causes a leftward shift of the hemoglobin dissociation curve, reflecting a decreased tendency for oxygen to unload in the tissues
question
Does Carbon Monoxide affect the PaO2 and does it precepitate methemoglobinemia?
answer
No and no. PaO2 remains normal (~95) Methemoglobin is formed when the Fe2+ (ferrous) in heme is oxidzed to Fe3+ (ferric iron). Methemoglobinemia results from drug exposures (dapsone, nitrates) as well as enzyme deficiencies and hemoglobinopathies.
question
When treating an acute ST-elevation MI or ischemic stroke with fibrinolytics such as TPA, what may develop? Is it serious or benign?
answer
Fibrinolytics may cause reperfusion arrhythmia on arterial re-opening, but these arrhythmias are usually benign. [Accerlerated idioventricular (AIVR) rhythm is a common reperfusion arrhythmia]
question
What are 3 three plasmin-activating, clot-busting drugs?
answer
Streptokinase tPA Urokinase
question
What are 3 fibrin-specific throbolytic/fibrinolytic drugs?
answer
tPA, reteplase, tenecteplase these act only on fibrin attached to recently formed clot without systemic activation
question
What is a nonfibrin-specific fibrinolytic drug?
answer
Streptokinase
question
How is blood that will be used for transfusion typically stored? What electrolyte imbalance may develop in a patient who receives a massive blood transfusion? What symptoms will that electrolyte imbalance cause?
answer
Prior to storage, whole blood is generally mied with solutions containing citrate anticoagulant. Packed cells derived from these whole blood collections also contain citrate Infused citrate can chelate serum calcium in the receiving person, causing hypocalcium The patient may experience paresthesias due to hypocalcemia.
question
How does our body monitor total body iron?
answer
Total body iron content is regulated through HEPCIDIN's effects on the absorption of dietary iron Hepcidin is an acute phase reactant synthesized mainly in the liver by hepatocytes
question
Why is chloride much lower in arterial blood than in venous blood?
answer
Short answer: actions of carbonic anhydrase and chloride shift Longer answer: Hb is responsible for carrying 15% of our CO2 as carbamate and the rest of our CO2 is carried as bicarbonate ion within the RBCs. [CO2 enters RBCs and is converted by carbonic anhydrase to form carbonic acid and then HCO3- and H+] Many of the bicarbonate ions diffuse out of the RBC into the plasma; to maintain electrical neutrality chloride ions diffuse into RBCs to take their place This is called CHLORIDE SHIFT
question
What is the general pattern of airway resistance in the lungs?
answer
Medium and smalled sized bronchi greater than 2 mm in diameter (the first 10 generations of bronchi) account for the greatest summated frictional resistance to airflow in normal airways. The smallest bronchi and bronchioles have a larger total cross-sectional area, so they don't contribute much to total airway frictional resistance.
question
What cells characterize the late phase of atopic asthma? (3 types)
answer
eosinophils basophils neutrophils
question
What is the general histology of an eosinophil?
answer
Bilobed nucleus packed with large granules of relatively uniform size and inclusions seen on EM
question
What protein do eosinophils release that help them kill parasites (helminths, e.g.)?
answer
Eosinophils release major basic protein, a potent antihelminthic toxin that's capable of causing damage to epithelial and endothelial cells (as it does it atopic asthma)
question
What drugs are typically NOT used to treat asthma?
answer
Antihistamines
question
What roles do leukotrienes (from mast cells, eosinophils, basophils, and other cells that infiltrate bonchilal mucosa in asthmatics) play in mediating asthma symptoms?
answer
They cause bronchial constriction and hyperreactivity and also promote mucosal edema and mucus hypersecretion
question
How do zafirlukast and montelukast offer long-term control of atopic asthma?
answer
They increase airway caliber and reduce mucosal inflammation by antagonizing the leukotriene receptors
question
What is the major protease of extracellular elastin degradation? What is the major serum inhibitor of this extracellular elastase?
answer
Neutrophil Elastase (comes from neutrophils and macrophages) The major serum inhibitor of elastase is Alpha-1 Antitrypsin
question
What are the 3 most common causes of metabolic alkalosis?
answer
(1) Loss of hydrogen ions from the body: e.g., vomiting and nasogastric suction may cause loss of hydrochloric acid; this causes serum chloride to decrease leadign to decrease in urinary cholirde (this would be SALINE-RESPONSIVE metabolic alkalosis) (2) Thiazide and Loop Diuretics: cause increase renal losses of Na, followed by excretion of Cl-; reabsorption of HCO3- increases to maintain electric neutrality in cells; this is CONTRACTION ALKALOSIS (3) Increased aldosterone secretion: seen in primary hyperaldosteronism (Conn Syndrome) and associated with metabolic alkalosis; aldosterone increases renal Na reabsorption and urinary lossess of K, Cl, and H with relative increase in HCO3- resulting from H losses; urinary Cl concentration is increased, but chloride doesn't correct it either (saline-resistant alkalosis)
question
What's the most important thing to do when doing a workup of metabolic alkalosis?
answer
Measure the urine chloride and ascertaining the patient's volume status.
question
How, immunologically speaking, are eosinophils recruited and activated?
answer
Eosinophils are recruited and activated by IL-5, which is secreted by Th2 helper T-cells
question
What is an important and easy equation to measure PaCO2?
answer
Basal Metabolic Rate / alveolar ventilation
question
What is considered to be the main indicator of alveolar ventilation?
answer
Arterial PaCO2 (inversely related to alveolar hyperventilation)
question
So what does hypocapnia imply?
answer
Ongoing alveolar hyperventilation
question
Again, what's a useful equation for PaCO2?
answer
PaCO2 = Basal Metabolic Rate / alveolar hyperventilation
question
What is the general pathophysiology of centroacinar emphysema?
answer
Associated with chronic, heavy smoking predominantly involves intraalveolar release of proteases, especially elastase, from infiltrating neutrophils and from alveolar macrophages
question
More specifically, what is the pathophysiology of centroacinar emphysema?
answer
Oxidative injury to the respiratory bronchioles and activation of resident macrophages --> neutrophil infiltrate Neutrophils release NEUTROPHIL ELASTASE, proteinase 3, cathepsin G, and matrix metalloproteinases, as well as generating OXYGEN-FREE RADICALS The oxygen free radicals inhibit the antiprotease activity of alpha-1-antitrypsin the resultant net protease-antiprotease imbalance and oxidant-antioxidant imbalance destroys acinar walls
question
What's the major factor in the development of centriacinar emphysema?
answer
excess neutrophil elastase activity
question
What is the clinical picture consistent with a COPD patient?
answer
COPD encompasses chronic bronchitis and emphysema; heavy smoking is the most common cause hallmark of any obstructive PFT profile is DECREASED FEV1/FVC ratio due to expiratory airflow obstruction Emphysema also tends to increase TLC and RV
question
A mom brings in a 6 y.o. child who has had recurrent sinusitis. You're worried about CF, so you order a "sweat test" (chloride sweat test), but this comes back normal. You next order a "nasal transepithelial potential difference" test. Why would a patient with CF have a significantly more negative nasoepithelial surface?
answer
Increased luminal SODIUM ABSORPTION. The CFTR normally SECRETES chloride ions into the lumen and has a tonic inhibitory effect on the opening of apical sodium channel (which abosrbds sodium into the cell) Impaired CFTR functioning directly reduces ductal epithelial chloride secretion and indirectly increases sodium absorption through lack of CFTR's inhibitory effect on the apical sodium channel. The result is dehydrated mucus and a widened, negative transepithelial potential difference
question
What are the classic LFT findings in a patient with emphysema (either a-1-antitrypisin deficiency or centroacinar)?
answer
FEV1/FVC: decreased (hallmark of obstructive lung disease) Total Lung Volume: Increased (air can't get out) Diffusing Capacity: decreased (due to destruction of alveoli and adjoining capillary beds)
question
Why would we want to harvest the great saphenous vein?
answer
For use in coronary bypass surgery
question
Where is the best place to harvest the great saphenous vein from, surgically?
answer
Just inferolateral to the pubic tubercle
question
Is the great saphenous vein located on the medial or lateral side of the foot?
answer
It originates on the medial side of the foot, courses anterior to the medial malleolus, and then travels up the medial aspect of the leg and thigh. IT drains into the femoral vein within the region of the femoral triangle, a few centimeters inferolateral to the pubic tubercle
question
If you saw elastase in a healthy individual's bronchoalveolar lavage, what cell did it come from?
answer
Macrophages. Macrophages and PMNs both make elastase, but this guy is healthy, so why would he have neutrophils in his lungs? We always have some dust cells in our lungs, so that's more likely.
question
Be sure to refer to FirstAid for the histological changes in the cells lining our airway. Here's a verbal description of the changes that we see from trachea to alveolus: (answer this first: What's the last feature to disappear as the epithelium changes along the respiratory tube?)
answer
Cilia. Bronchi have a pseudostratified columnar ciliated epithelium with goblet cells and submucosal mucoserous glands and cartilage Bronchioles, terminal bronchioles, and respiratory bronchioles lack: goblet cells, glands, and cartilage By the level of the terminal bronchioles, the airway epithelium is CILIATED simple cuboidal. Epithelial cilia persist up to the end of the respiratory bronchioles
question
What are lamellar bodies in Type II pneumocytes?
answer
membrane-bound intracellular inclusions composed of stacked layeres of cell membrane like material they contain phospholipids (dipalmitoyl phosphatidylcholine..... surfactant.)
question
What is the major physiological function of surfactant?
answer
to decrease the surface tension of fluid layer lining the alveolar surface
question
What is the result of insufficient surfactant (as seen in neonatal respiratory distress syndrome, or maybe a guy who doesn't have lamellar bodies in his type II pneumocytes)?
answer
patchy atelectasis (collapse) of alveoli due to increased surface tension
question
Here's a high yield overview of the histology of the lungs:
answer
Alveolar surface is 95% covered by flat Type I pneumocytes Interspersed cuboidal type II pneumocytes are the source of pulmonary surfactant (stored in lamellar bodies) Type II pneumocytes are also the main cell type responsible for replacing the alveolar epithelium after alveolar injury
question
What is unique about type II pneumocytes regarding alveolar injury?
answer
Type II pneumocytes are unique in their ability to proliferate in response to injury
question
What are clara cells?
answer
non-ciliated, secretory constituents of the terminal respiratory epithelium they secrete clara cell secretory protein (CCSP), which INHIBITS NEUTROPHIL RECRUITMENT and ACTIVATION as well as neutrophil-dependent mucin production
question
Describe the pathogenesis and pathophysiology of Paget's Disease of the Bone.
answer
Disease process starts with marked osteoclastic activation, followed by an increase in activity of bone forming cells osteoblasts. The net result is increased bone resorption and also formation of abnormal bone. A new collagen is laid down in a haphazard manner as compared to the normal, linear manner. The end product is a MOSAIC PATTERN of lamellar bone with irregular sections linked by CEMENT LINES which represent previous areas of bone resorption
question
What are the 4 collagen subtypes, where is each found, and what are associated diseases with each?
answer
(1) Dermis, bone, tendons, ligaments, dentin, cornea, blood vessels, scar tissue; osteogenesis imperfecta (2) cartilage, vitreous humor, nucleus pulposus (3) skin, lungs, intestines, blood vessels, bone marrow, lymphatics, granulation tissue Ehlers-Danlos Syndrome (types 3 and 4) (4) basement membranes Alpart Syndrome
question
In the final stage of the healing process of myocardial infarction, what type of collagen is deposited?
answer
Type I
question
What intercellular connection connects osteocytes?
answer
Gap Junctions this is so they can send signals to modulate activity of surface osteoblasts, thereby helping to regulate bony remodeling
question
What is the t(9;22) Translocation also called? What is its associated disorder?
answer
Philadelphia Chromosome bcr-abl gene product Associated with CML "Philadelphia CreaML cheese"
question
What does the t(8;14) translocation cause? What disorder is it associated with?
answer
c-myc overexpression Burkitt's Lymphoma
question
What does the t(14;18) translocation cause? What disorder is it assocaited with?
answer
bcl-2 activation Follicular Lymphoma
question
What disorder does the t(15;17) cause? Why is this special?
answer
M3 type of AML, which is responsive to all-trans retinoic acid.
question
What disorder is the t(11;33) translocation associated with?
answer
Ewing's Sarcoma 11+22 = 33, Patrick EWING's number
question
What disorder is the t(11;14) translocation associated with?
answer
Mantle Cell Lymphoma
question
What cause of mental retardation is associated with t(8,21)? What disorder is further associated with this?
answer
Down's Syndrome ALL "We ALL fall DOWN together."
question
Epigenetics: Acetylating histones vs. Methylating cytosine and adenine?
answer
A cetylating A ctivates DNA M ethylation M utes DNA
question
What does genomic imprinting refer to?
answer
The phenomenon in which an offspring's genes are expressed in a parent-specific manner It occurs via an epigenetic process that alters phenotype of an organism independent of genetic code DNA methylation: mutes gene expression is important in imprinting
question
What is the characteristic histological finding of many forms of Acute Myelogenous Leukemia?
answer
Auer Rods
question
Which type of AML is associated with many Auer Rods? What chromosomal translocation? What's it's "specific" differentiation / name? What do we treat it with?
answer
M3 t(15;17) Acute promyelocytic leukemia all-trans retinoic acid
question
Which cyclooxygenase is an inducible enzyme that is normally undetectable in most tissues except during inflammation?
answer
COX-2
question
What dermatological layers are apocrine glands found at?
answer
Dermis and subcutaneous fat
question
What regions of the body have apocrine glands?
answer
The dermis and subcutaneous fat of the: breast areaolae, axillae, genital regions
question
If you're soaked with sweat, what types of glands are responsible for the distinctive smell of you?
answer
Apocrine glands Initially odorless, but can become malodorous secondary to bacterial decomposition on the skin surface
question
What are the classic signs of phenylketonuria (PKU)?
answer
Mental retardation, eczema, and a mousy, musty body odor.
question
If a child pressents with mental retardation, eczema, and a mousy, musty body odor, what disease are you thinking of?
answer
PKU
question
How is PKU inherited?
answer
Autosomal Recessive
question
People with Down Syndrome are at an increased risk to develop what type of cancer?
answer
ALL (we ALL fall DOWN together) Also increased risk of AML
question
What's the term for the tendency of a study population to affect an outcome due to the knowledge of being studied?
answer
the Hawthorne Effect i.e., if a doc knows someone is monitoring how often he takes a sexual history, more likely to take lots of sexual histories
question
What is Berkson's bias?
answer
Berkson's bias refers to selection bias created by selecting hospitalized patients as control group
question
What is the pygmailion effect?
answer
Describes researcher's beliefs in teh efficacy of treatment this can potentially affect outcome
question
This is an important one: LEAD TIME BIAS. What is it?
answer
Lead-time bias refers to apparent prolongation of survival after a SCREENING TEST without any real effect on prognosis
question
So it's a biostats question and there's a lot of jargon about a new screening test and patient's surviving longer? What do you think about?
answer
Lead-Time bias
question
In terms of vitamin D synthesis, where does sunlight exposure fall?
answer
It catalyzes the first reaction in the chain of active vitamin D synthesis: 7-dehydrocholesterol --> cholecalciferol (vitamin D3)
question
So, we should try to get lots of sunlight to catalyze the first step in vitamin D synthesis, right?
answer
No, excess sunlight exposure shunts previtamin D3 to a pathway that forms inactive products this is a mechanism to prevent against excessive Vitamin D
question
Once activated from 7-dehydrocholesterol to cholecalciferol by sunlight, how many hydroxylations must Vitamin D3 undergo to become active? Where do each of these occur?
answer
2 the first is in the liver by cytochrome P450 25-hydroxylase [this step is NOT tightly regulated] the second is in the kidney, performed by 1-alpha hydroxylase
question
What is a common clinical picture of Paget's disease of the bone?
answer
Older gentleman with pain and deformity in a bony area and hearing loss
question
What is the primary abnormality in Paget's disease of the bone?
answer
excessive OSTEOCLASTIC bone resorption; osteoclasts in Paget's disease are typically very large and can have up to 100 nuclei bone turnover is markedly increased in Paget's disease, culminating in chaotic bone formation
question
What cell lineage do osteoclasts come from?
answer
Mononuclear Phagocytic cell lineage (same as macrophages)
question
What are the 2 most important factors for osteoclastic differentiation and where do these 2 factors come from?
answer
M-CSF (macrophage colony-stimulating-factor) and RANK-L these both come from osteoblasts
question
So what is paget's disease of the bone caused by?
answer
excessive osteoclastic resorption [childhood infection of osteoclasts by a paramyxovirus may be responsible]
question
Who has denser bones, black ladies or white ladies?
answer
Statistically, black females have higher bone density than white females
question
There are 7 important risk factors for osteoporosis....
answer
smoking menopause corticosteroid therapy physical inactivity caucasian race low total body weight alcohol use
question
What is the RANK receptor/RANK-L interaction essential for?
answer
Formation and Differentiation of osteoclasts. [2 most important factors for differentiation of osteoclasts: RANK-L and M-CSF]
question
When you hear the term "humoral hypercalcemia of malignancy" what does it sound like?
answer
elevated serum calcium in the presence of cancer [so, patient has risk factors for types of cancer, and an elevated calcium, think this]
question
What is the cause of humoral hypercalcemia of malignancy?
answer
The hypercalcemia is caused by release of parathyroid hormone-related peptide (PTHrP) PTHrP acts like PTH, although the degree of hypercalcemia is generally higher with PTHrP than with primary hyperparathyroidism
question
What's the relationship between high/low calcium and high/low phosphorous?
answer
As a rule of thumb, if calcium levels are high, phosphorous levels are low, and vice versa
question
What are the serum calcium and PTH findings in primary osteoporosis (this is important, so know it)?
answer
Serum calcium and PTH are typically within the normal range.
question
Again, what are the serum calcium and PTH findings in primary osteoporosis?
answer
In primary osteoporosis (osteoporosis not caused by a medical disorder), serum calcium, phosphorous, and PTH levels are typically normal.
question
When considering disease epidemiology, what is the latent period?
answer
The time elapsed from initial exposure to clinically apparent disease
question
What 2 aspects of disease epidemiology can be related to latent period and how?
answer
(1) disease pathogenesis: exposure and how long it takes for symptoms (2) exposure to risk modifiers (e.g., anti-oxidants)
question
What is a 95% confidence interval?
answer
the range of values in which one can be 95% confident that the true mean o the underlying population falls
question
How do we calculate "Standard Error of the Mean"
answer
SEM = SD / (square root: n [sample size])
question
Statistically define incidence:
answer
the number of new cases of a disease per year divided by the total population at risk
question
Who is a tricky subset of a population who's NOT at risk to get a disease, statistically speaking?
answer
people who already have the disease! population of 40 and 5 people have disease, population at risk is 35
question
What is a "positive predictive value" because you obviously don't know...
answer
The PPV reflects the number of true positives divided by the number of subjects testing positive for a test
question
How is the positive predictive value related to disease prevalence?
answer
As the disease prevalence increases, the PPV also increases



