STABLE Course – Flashcards
Unlock all answers in this set
Unlock answersquestion
STABLE stands for:
answer
Sugar and Safe care Temperature Airway Blood pressure Labs Emotion
question
Fetal/infant hypoxemia and hypotension can result in...
answer
Reduced intestinal blood flow, and ischemic injury --> withhold enteral feeds in sick infants!!
question
Causes of Bowel Obstruction
answer
Congenital: Stenosis/Atresia, Malrotation + volvulus, imperforate anus Functional: Hirschprung's, meconium plug (?CF), meconium ileus, hypothyroidism Acquired: NEC, peritoneal adhesions (congenital = bands) ** Note: consider obstruction if polyhydramnios is present **
question
Name of surgery for malrotation?
answer
Ladd's procedure - cutting obstructing bands, widening mesentery, to prevent volvulus
question
Bilious emesis
answer
= bowel obstruction - work up: bloods, PFA, UGI series
question
Where is best site for IV in infants?
answer
Hand, Foot, Scalp veins Umbilical vein --> IV fluids, meds; can be cannulated for up to 1 week after birth 24 gauge IV cath or 23/25 gauge butterfly, usually Insertion aided by transillumination under hand/foot
question
Maternal meds affecting neonatal glucose metabolism
answer
1. Beta-sympathomimetics (terbutaline) - maternal hyperglycaemia --> fetal hyperinsulinemia - crosses placenta, breaks down glycogen stores 2. Sulfonylureas - maternal hypergly, fetal hyperinsulin - crosses placenta, promotes insulin secretion 3. Beta blockers - blocks fetal adrenergic receptors, prevent stimulation of glycogenolysis (persists after birth) 4. Thiazide diuretics, TCA - maternal hypergly... 5. Maternal IV Dextrose during labour - increased fetal insulin secretion
question
High risk groups for inadequate glycogen stores
answer
1. Preterm infants 2. Late preterm (34 - 36+6) 3. SGA - chronically stressed fetus may use all placental insulin --> not creating enough glycogen stores
question
High risk groups for hyperinsulinemia
answer
1. Infant of diabetic mother - can takes days or longer for insulin levels to down regulate --> regular feeding, +/- IV dextrose 2. LGA 3. IEM, hypopituitarism, hypothyroidism
question
High risk groups for increased utilization of glucose
answer
1. Sick - including preterm, SGA 2. Also infection, shock, resp and cardiac disease, hypothermia, hypoxia
question
Late preterms are at risk of
answer
- hypoglycaemia - feeding problems - temperature instability - respiratory distress - apnea - hyperbilirubinemia - higher hospital readmission rates - 3-fold higher mortality rates than term
question
Monitoring hypoglycaemia post-delivery
answer
1. Check blood glucose within 1-2 hours after birth, then every 1-3 hours based on glucose/interventions/health status. Evaluate prior to feeding. 2. If glucose shows pattern of stability and remains in 50-110 range, slow and then stop monitoring. Can require monitoring 24-72+ hours
question
How to check blood glucose
answer
- Plasma glucose is gold standard - Bedside is faster, but if low can confirm with a plasma test - but don't delay tx
question
Signs/Symptoms of Hypoglycemia
answer
General: - weak, high pitched cry - poor feeding, poor suck coordination - hypothermia - diaphoresis Neuro: - tremors - irritability - hypotonia - lethargy - seizures Cardioresp: - tachypnea - apnea - cyanosis
question
Sugar level that defines hypoglycemia? Goal of tx?
answer
In a sick infant --> <25-30, need IV dextrose Aim: 50-110 mg/dL
question
Fluid/glucose management for the sick infant
answer
IV 10% Dextrose (D10W) if: a) ; 50 and symptomatic b) ;25-30 and asymptomatic 1. Confirm with plasma glucose, but proceed with tx 2. Bolus: 2 mL/kg D10 at rate of 1 mL/minute 3. Infusion: 80 mL/kg/day (divide by 24 for hourly rate; round up) 4. Recheck bedside glucose 15-30 minutes after completion of bolus or any increase in infusion rate 5. If still 25-30 mg/dL --> enteral feed ** if due to hyperinsulinemia, may need higher concentration of dextrose --> must be given through central venous line ** ** without electrolytes, unless infant is > 24 hours old **
question
If fluids are given via umbilical venous or artery cath, add...
answer
0.1 - 1 unit heparin per mL of fluid e.g. 250 mL bag of D10, heparin concentration 1000 units/mL --> draw up 0.25 mL of heparin solution (=250 units), add to 250 mL bag
question
Umbilical Vein Catheter (UVC)
answer
Indications: - rapid IV access needed - based on health status, if no time for trying peripheral access - more than 1 line is needed - need to give fluids with ; 12.5% dextrose - exchange transfusion C/I: - omphalitis, peritonitis, omphalocele, NEC Position: - at IVC/RA junction; confirm on AP CXR - in emergency, if no time to confirm location --> then just insert it 2-4 cm until there is blood return - malposition --> arrhythmias, thrombus, myocardial perf, cardiac tamponade/effusion, endocarditis, pulmonary hemorrhage/infarction - if malpositioned into liver --> hepatic necrosis, portal htn, intestinal ischemia, hepatic vessel perf... Meds: - can give all meds including vasopressors (if properly positioned)
question
Umbilical Artery Catheter (UAC)
answer
Indications: - continuous arterial BP monitoring - frequent ABG necessary C/I: - omphalitis, peritonitis, omphalocele, NEC, vascular compromise in the lower limbs or buttocks Position: - High: between T6 and T9 on AP CXR - to avoid ischemic injury to organs and tissues supplied by celiac (T11) and SMA (T11-12) arteries - Low: in lower abdominal aorta between L3 and L4, and above bifurcation of iliac arteries (L4/5) - to avoid injury to renal (L1) and IMA (L2) Meds: - for fluids mainly ** NOT recommended for meds or blood products; do NOT give vasopressors or calcium ** monitor temp and colour of toes, legs, groin, abdomen --> signs of arterial spasm, clot/emboli
question
Intraosseous Access
answer
- 18 gauge IO needle, or 18/20 gauge short spinal needle - medial aspect of tibial bone, below tibial tuberosity - can give meds, fluids, blood products
question
If the UAC/UVC is malpositioned and needs to be advanced...
answer
DO NOT DO IT if you already took down sterile field! Can pull out but cannot advance in unless sterile!!
question
Calculating Umbilical Catheter Depth
answer
1. High UAC (cm) = {3 x BW (kg)} + 9 + length of umbilical stump (cm) --> between T6 and T9 (above diaphragm, below aortic valve) 2. Low UAC (cm) = BW (kg) + 7 + length of umbilical stump (cm) --> between L3 and L4 (above bifurcation) 3. UVC (cm) = {0.5 X high line UAC length (cm)} + 1 + length of stump (cm) --> at jcn of IVC and RA (above diaphragm)
question
Normal core temperature
answer
36.5 to 37.5 (97.7 - 99.5)
question
Hypothermia levels
answer
Mild: 36 - 36.4 (96.8 - 97.6) Moderate: 32 - 35.9 (89.6 - 96.6) Severe: 37C, check temperature every 15-30 minutes
question
Physiologic response to cold stress
answer
Action of norepinephrine (release mediated by hypothalamus) - peripheral vasoconstriction --> risk of anaerobic metabolism and lactic acidosis causing tissue damage - pulmonary vasoconstriction --> increased pulmonary vascular resistance, leads to R-to-L shunting thru ductus arteriosus or PFO --> hypoxemia because lungs bypassed --> worsens shunting (not really in preterm infants) - metabolism of brown fat --> "non-shivering thermogenesis"; however requires O2 and glucose so hypoglycaemic, low glycogen stores, and hypoxic infants will not be able to metabolize brown fat - increased muscle flexion and activity --> generates heat, reduces surface area for heat loss; hypotonia is worse for infants
question
Why are premies at higher risk of hypothermia?
answer
- larger surface area to body mass ratio - weak muscle tone/poor flexion - thinner skin - increased evaporative water loss - poor ability to vasoconstrict - decreased amounts of insulating fat - reduced amounts or no brown fat
question
Physiological effects of low temperature
answer
- outside of normal range, O2 consumption, glucose consumption, metabolic rate increase --> hypoxemia, hypoxia, hypoglycemia - progressive hypothermia (34-35 or lower) --> reduced consciousness, hypoventilation, bradycardia, hypotension - impaired coagulation (intraventricular or pulmonary hemorrhage), patent ductus arteriosus, increased risk of infection, AKI ** hypothermia can also impair surfactant production, worsening RDS in premies **
question
Thermal neutral temperature/zone
answer
The temperature that permits the infant to expend the least amount of energy to maintain a normal body temperature.
question
Mechanisms of heat loss
answer
1. Conduction: between 2 solid touching objects - prewarm objects before they come in contact with infant - insulation between body and cooler surface - clothing, hats - chemical thermal mattress 2. Convection: air currents - increased delivery room temp if premie - cover with food grade plastic (if ;1.5 kg) - closed, warmed incubator for transport - heated humidified O2 3. Evaporation: moisture on skin - quickly dry infant after delivery, after bathing with prewarmed blankets and immediately remove damp linens - hat - cover VLBW with plastic - increase room temp - minimize air turbulence - heated humidified O2 4.Radiation: between solid surfaces not in contact - move infant away from cold windows/walls - thermal shades over windows
question
Reducing risk of hyperthermia, burns
answer
- do not overheat surfaces hotter than the infant's skin temperatures (except for specific warming mattresses which are at 40C) - never place hot water bottles next to infant - use temperature controlled blanket warmer, not microwave - do not apply heat directly to extremities that are poorly perfused
question
Radiant Heat Gain
answer
- when surrounding surfaces are warmer than infant's skin temp --> e.g. using radiant warmer Reducing unwanted radiant heat gain: - when using radiant warming bed, ensure its on "sevo-control" not manual control - place temperature sensor probe over RUQ; ensure it is well secured otherwise can incorrectly heat infant - prevent direct sunlight on infant
question
Hypoxic-Ischemic Encephalopathy
answer
- [birth] asphyxia (impaired gas exchange; a known perinatal sentinel event) leads to hypoxemia, hypercarbia - anaerobic glycolysis, lactic acidosis, metabolic acidosis - drop in pH, base deficit increases --> end organ damage - in developed world, incidence 3-5/1000 live births - impact: CP, cognitive and motor deficits, epilepsy, deafness, learning problems - during resuscitation, prevent hyperthermia (>37.5), reduce fever if it occurs, monitor for hypoglycemia
question
Neonatal encephalopathy
answer
- due to HIE, brain hemorrhage, cerebral infarction - in USA, incidence 2-3/1000
question
Therapeutic/Neuroprotective Hypothermia
answer
- reduces mortality rate and decreases chance of major disability in infants with ischemic insult to brain (late decels, cord prolapse, uterine rupture, maternal hemorrhage, placental abruption, maternal trauma) - candidates: `must be started within 6 hours of birth `greater than or equal to 36 weeks gestation `greater than or equal to 1800 g `with abnormal neurological exam `must fill 3 domains of: seizures, consciousness level, posture, tone, primitive reflexes, autonomic symptoms (pupils, HR, respirations) - passive cooling prior to transport might be needed --> turning off radiant warmer, monitoring temp so it does not drop too low (below 33.5C) - rewarming: aim for 0.5C per hour, to avoid sudden vasodilation and hypotension
question
Rewarming a hypothermic infant
answer
- closely monitor vitals (HR and rhythm, pulses, BP, perfusion, resp effort and rate, O2 sats), level of consciousness, acid-base status, glucose level - in term infants, rectal temp is better measure; avoid in premies, use axillary temp; once normothermic, just use axillary - do not rewarm too rapidly - incubator or radiant warmer can be used; set incubator temp to 1-1.5 C above infant's core temp, and infant temp reaches the set temp, increase the set temp again by 1-1.5C - use humidified mist, cover with plastic sheet - signs of deterioration when rewarming: `tachycardia `hypotension `cardiac arrhythmia ` desating, cyanosis, worsening resp distress `worsening acidosis - be prepared for full CPR measures while rewarming
question
Severity of Respiratory Distress
answer
1. Mild - rapid resp rate with or without need for supplemental O2, and with or without signs of distress (e.g. nasal flaring) 2. Moderate - cyanotic on room air - signs of resp distress (e.g. grunting, retractions) 3. Severe - infant is struggling to breathe, increasing difficulty maintaining acceptable O2 say despite supplemental O2 - ABG shows respiratory failure - exhaustion, worsening hypoxia, altered mental status (p/w hypotonia, poor/no response to stimulation)
question
Normal Respiratory Rate
answer
30 - 60 breaths per minute Minute ventilation = Tidal Volume x Resp Rate
question
Causes of Bradypnea
answer
- exhaustion - decrease central resp drive due to HIE, hemorrhage, cerebral edema - metabolic disorders - meds: e.g. maternal opioids - neuromuscular disease - severe shock (may be initially high to compensate for metabolic acidosis)
question
Gasping
answer
** A sign of impending cardio-respiratory arrest!! ** - immediate PPV via a bag and mask - if HR low, may need LMA or ET tube - then continue PPV
question
Signs of Increased Work of Breathing
answer
1. Nasal Flaring: sign of air hunger 2. Grunting: to increase FRC when there is collapse of alveoli, to improve oxygenation and ventilation --> NOTE: some late preterm and term infants grunt 30 min after birth and stop by 2 hours; eval for other signs of resp distress 3. Retractions: with inspiration, attempts to increase tidal volume - intercostal alone, usually mild resp distress - when severe, assess for airway obstruction, pneumothorax, displaced or plugged ET tube, worsening atelectasis - can be: suprasternal, subcostal, substernal, intercostal
question
Normal O2 Sats
answer
By 24 hours of life, for healthy late preterm and term infants, SpO2 on RA ranges between 95.6 and 98.8%
question
Pre- and Post-Ductal Sats
answer
Pre-ductal: RIGHT hand; ABG from right radial art Post-ductal: any FOOT; ABG from UA or post tibialis art - if there is a > 10% difference in saturation between the two, caution! a) R-L shunt at ductus arteriosus: pre-ductal higher than post-; due to persistent pulm HTN, L sided heart obstructive lesions (tricuspid or pulmonary atresia) b) R-L shunt at foramen ovale, +/- shunt at DA: pre- and post- are nearly equal, but both are lower than normal c) Transposition of great arteries + wide open DA: pre- lower than post-
question
Universal Pulse Ox Screening
answer
- Can detect: hypoplastic L heart, coarctation of aorta, pulmonary atresia, ToF, TAPVR, transposition, tricuspid atresia, truncus arteriosus - Wait until after 24 hours of age to perform screening (after foramen ovale/ductus close) - report any difference of >3% between pre- and post-, any sat < 90%
question
Cyanosis
answer
- it takes 3-5 g/dL of reduced Hb for cyanosis to be evident --> implications for infants with low and high Hb levels (e.g. anemic infant will be more severely hypoxemic and desaturated than an infant with normal or elevated Hb level)
question
What to do with a cyanotic infant
answer
- Evaluate O2 sats - Supplemental oxygen, using O2/air blender when possible - Start with 21% oxygen, slowly increase amount of inspired oxygen until sat remains at 90% - If you need to give 100% O2 and the sats are still not rising to 90%, consider cyanotic CHD or PPHN
question
Retinopathy of Prematurity
answer
- the more preterm, the higher risk - avoid excessive O2 administration - aim for sats 91-95%
question
Rapidly increasing oxygen requirement with or without respiratory distress worsening...
answer
... may be a sign of impending respiratory or cardiac failure
question
Conditions that can lead to hypoxia
answer
- lung disease - intracardiac mixing of blood - cardiac failure (poor pumping) - increased metabolic demand (e.g. sepsis) - anemia, or abnormal Hb
question
Arterial Blood Gas in young infants
answer
pH 7.35 - 7.45 PCO2 35-45 mmHg PO2 60-80 mmHg HCO3 19-26 mEq/L Base Excess -4 to + 4 capillary not useful for assessing oxygenation
question
Metabolic Acidosis
answer
Causes: - anaerobic metabolism, secondary to: `shock, poor tissue perfusion `hypothermia `hypoglycemia `severe CHD - sepsis - IEM Treatment: - hypoxia: improve oxygenation and ventilation - do not use hyperventilation (only a temp fix) - tx hypotension and shock with fluids, pressers, correction of anemia - tx heart failure/cause - tx IEM
question
Respiratory Acidosis
answer
Causes: - loss of tidal volume: `lung disease (pneumonia, surfactant deficiency) `pneumothorax `airway obstruction - loss of respiratory drive `poor respiratory effort (most premies or very sick infants) `neurological injury (e.g. HIE, stroke) `apnea Treatment: - renal compensation is slow - CPAP, PPV by bag mask, Intubation - Tx cause
question
CPAP
answer
Candidates: - has adequate respiratory effort - infant doesn't meet criteria for PPV/ET: `increased WOB/O2 req `mild CO2 retention and mild acidosis `PCO2 ; 55-60 and infant req 60-70% is needed, raises concern ET may be required - increased frequency or severity of apnea - atelectasis on CXR - tracheobronchomalacia NOT Candidates: - rapidly progressing respiratory failure - severe apnea with cyanosis, and/or bradycardia - gasping - infants w/: poor resp drive, CDH, TOF, choanal atresia, cleft palate, CV instability, poor heart fcn ** Use with caution in infant with Pneumothorax **
question
PPV with Bag and Mask/T-piece resuscitator
answer
Indications: - apnea - inadequate breathing effort - bradycardia - hypoxemia not responsive to supplemental O2 - GASPING: if infant's HR is low and not rising despite effective ventilation, insert LMA/ET. PPV should be continued until HR maintained over 100
question
Troubleshooting Respiratory Distress in the Intubated Infant
answer
DOPE - Displaced - Obstructed - Pneumothorax - Equipment failure
question
Respiratory failure warning signs
answer
Consider PPV via LMA or ET when: - gasping (**PPV ASAP**) - periods of severe apnea and bradycardia - persistent bradycardia despite effective PPV - labored resp effort: mod-severe retractions, grunting, nasal flaring - hypercarbic with mod-severe resp acidosis - unable to ventilate/oxygenate adequately with PPV - rapidly increasing O2 concentration to maintain O2 sats > 90% - unable to maintain acceptable sats for the infant's suspected disease process - CDH
question
Endotracheal Intubation
answer
Equipment: - Laryngoscope - Blades: `No. 1 - term infant `No. 0 - preterm infant `No. 00 - very low birth weight infant - McGill forceps (for nasotracheal intubation) - Uncuffed ET tube - CO2 detector - Suction ...
question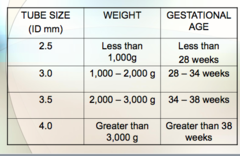
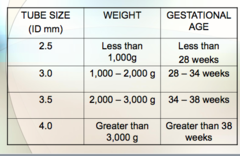
ET Tube Size and Insertion Depth
answer
Tube insertion depth at lip (cm) using Lip-to-Tip Rule (add 6 to infant's weight in kg - use kg of upper limit) < 750 g: 6 3 kg: 10
question
Correct ET tube location
answer
- in the mid trachea - halfway between the clavicles and carina - confirm on CXR, with neutral head position
question
What do you do after intubation?
answer
Insert OG or NG, to decompress the stomach. Then confirm ET position on CXR.
question
Suggested initial ventilator support
answer
1. VLBW ( 2.5 kg) Rate (/min): 20-40 Inspiratory Time (s): 0.35-0.4 PIP (cmH2O): 20-28 PEEP (cmH2O): 4-7
question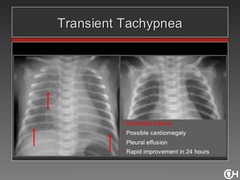
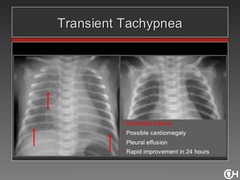
Transient Tachypnea of the Newborn
answer
- affects term or late preterm - one of most common causes of respiratory distress - resp distress onset within 1-2 hours after birth, due to failure to adequately absorb fetal lung fluid into circulation/lymphatics - RF: C-section, precipitous delivery, preterm delivery - usually mild/mod distress, O2 req < 40% - resolves in 2-3 days, sometimes within 24 hrs - CXR: fluid in fissures, perihilar markings/opacity, lung overinflation, +/or pleural effusion - DDx: pneumonia, sepsis, RDS, aspiration, pulmonary edema due to cardiac cause
question
RDS

answer
- seen in preterm infants, including late preterm - immature lung anatomy/physiology, surfactant insufficiency - increased risk in infants of diabetic mothers - onset of resp distress at birth or shortly after - CXR: uniform, diffuse granular appearance, air bronchograms, low lung volumes
question
Pneumonia

answer
- term or preterm - onset of resp distress at birth or with onset of infection - CXR: variable, may show diffuse or focal infiltrates, hazy/opaque lung fields, lobar consolidation
question
Aspiration

answer
- of amniotic fluid, blood, or gastric contents - affects term, preterm - onset of resp distress at birth or at time of aspiration - CXR: variable, may show patchy infiltrates, areas of atelectasis, hyperinflation
question
Meconium Aspiration Syndrome

answer
- term and post-term - common cause of hypoxemic respiratory failure - a/w increased risk of sepsis - issue starts in utero: poor placental blood flow/oxygenation causes fetus to pass meconium, aspirate, after birth obstruction of airways leads to both atelectasis and hyperinflation; increases risk of pneumothorax, impaired ventilation/oxygenation, surfactant inactivation, pulm htn - intrauterine infection might be a RF - CXR: coarse, nodular opacities, atelectasis, overinflation
question
Pulmonary Hemorrhage

answer
- term or preterm - onset of cardioresp distress is sudden, accompanied by blood in trachea - blood fills alveoli, inactivate surfactant - etiology: pulm edema, L-R ductal shunting through PDA, sepsis, LV failure, bleeding disorders
question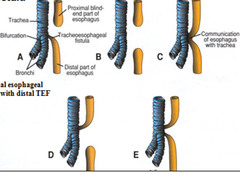
Tracheoesophageal Fistula/Esophageal Atresia
answer
- term or preterm - 85% of time are concurrent - onset of resp distress usually soon after birth - excessive salivation (if EA), choking, coughing, and cyanosis with feeding, abdominal distension - a/w hx of polyhydramnios (think TEF or obstruction) - a/w VACTERL: vertebral defects, anal atresia, cardiac defects, TEF with EA, renal dysplasia, limb anomalies - management: make NPO, IV access, assess oxygenation and ventilation, insert low continuous suction catheter into esophageal pouch, position prone/elevate head of bed
question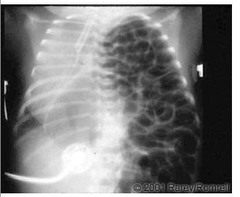
CDH
answer
- term or preterm - onset is at birth or shortly after - cyanotic, decreased breath sounds on side of hernia (usually left), scaphoid abdomen, barrel shaped chest - need to stop giving bag/mask, and need to intubate - otherwise you inflate the stomach which compresses mediastinal structures - hypoplastic lungs make oxygenation and ventilation difficult - commonly a/w PPHN; get pre-/post-ductal sats - watch for pneumothorax - insert NG or OG tube and frequently remove air from stomach to prevent air entering the bowel as this will further compromised lung expansion; leave tube open to air
question
Airway Obstruction
answer
1. Choanal Atresia - term or preterm, F>M - in >50% of cases there is other congenital abnormality, including incidence of CHD - can have one or both posterior nasal passages blocked by bony septum or soft tissue membrane - cyanotic at rest, but pinks up with crying - if bilateral, can be severely cyanotic at rest, even severe asphyxia --> need an oral airway - dx: inability to pass 6-French feeding tube through nares 2. Pierre Robin Syndrome - term or preterm - small jaw with normal sized tongue that obstructs airway; half can have cleft palate - to relieve obstruction, turn infant prone - if still obstructed, insert NP tube; if that doesn't work, then LMA (ET intubation may be difficult)
question
How to insert a NP tube
answer
- coat tip of 2.5 mm ET tube with water soluble gel - pass through one nostril until located at end of nasal passage - secure with tape - support breathing by attaching tube to device that provides CPAP at appx 6 cm H2O, or place infant into humidified O2 hood with supp O2
question
Persistent Pulmonary Htn of the Newborn
answer
- affects term predominantly - elevated pulm vasc resistance causes R-L shunting of blood across PDA or foramen ovale, leading to hypoxemia - resp distress and cyanosis usually apparent within hours of birth - may be a/w: MAS, pneumonia, RDS, CDH, pulmonary hypoplasia, CHD, HF (secondary to infection, asphyxia), sepsis, hypothermia, idiopathic - ask if mom took NSAIDs during pregnancy - these are PG synthetase inhibitors, may cause constriction of ductus arteriosus and structural changes in pulm vasculature causing PPHN
question
Pneumothorax
answer
- preterm or term - can occur spontaneously in non-intubated infants, or as complication of PPV - symptoms: increased resp distress, acute onset of brady or tachycardia, irritability, hypotension, resp and/or metabolic acidosis - signs: positive transillumination, chest asymmetry, asymmetric breath sounds, shift in point of maximum impulse, mottled appearance, poor peripheral pulses, hypotension, flattened or decreased QRS on ECG - CXR gives definitive diagnosis, if there's time... don't delay tx if infant severely compromised and transillumination is positive
question
Transillumination of the chest
answer
- False positives: chest wall edema (hydrops), subcutaneous emphysema, pneumomediastinum, very preterm infants, light source not held perpendicular - False negatives: thick chest wall, darkly pigmented skin
question
Pneumopericardium
answer
- almost always because of mechanical ventilation - signs: sudden onset of severe cyanosis, muffled heart sounds, flattened or decreased QRS, initial tachycardia followed by bradycardia, poor or absent peripheral pulses, poor perfusion, narrow pulse pressure
question
Pain Control with Analgesics
answer
1. Non-pharmacologic comforting measures - non-nutritive sucking, swaddling, facilitated tucking, kangaroo care, music therapy 2. Oral sucrose - for minor procedures like heel stick or venepuncture 3. Opioids - block pain sensation at the level of CNS - indicated for painful procedures like intubation, chest tube insertion, surgery; infants mechanically ventilated and who become cyanotic with minimum stimulation may benefit - need to monitor for hypotension, tachy or bradycardia, resp status/apnea
question
Morphine
answer
0.05 mg/kg per dose every 4-8 hours (IV, IM, SC) - dilute, give slowly over at least 15 min - onset of action should be in 15-30 min - causes resp depression, may lead to apnea --> be prepared to assist ventilation - s/e reversible with Naloxone
question
Fentanyl
answer
1-2 mcg/kg per dose IV - dilute to a 2-3 mL volume, and give slowly over at least 15 min - onset of action within minutes - causes apnea, be prepped to assist ventilation
question
Sucrose
answer
24% solution Full term - 0.5-2 mL Preterm - 0.1-0.4 mL Place a few drops on anterior portion of tongue or into buccal pocket 2 min before painful stimulus. Duration of effect 3-5 minutes. - sucking may be synergistic with sucrose in pain relief - pacifier can be dipped in sucrose solution - no point in giving via a gastric tube, no relief this way - best to give only to infants who are able to protect their airway; ensure an intact sucking reflex prior to administration
question
Causes of Tachypnea
answer
1. With LOW PCO2 --> non-pulmonary - metabolic acidosis (shock, CHD/hypoxemia) - brain disorders (hemorrhage, meningitis, cerebral edema) 2. With HIGH PCO2 --> pulmonary - transient tachypnea of newborn - RDS - pneumonia, aspiration - pulmonary hemorrhage - TEF/EA - CDH - obstruction - pneumothorax
question
Effects of Shock
answer
- oxygen debt, anaeorbic glycolysis, lactic (metabolic) acidosis - cardiac output drops - when hypotension develops, shock now Uncompensated (it's a late sign of cardiac decompensation)
question
Tachycardia
answer
- if >220, consider SVT - may indicate poor CO and/or CHF - causes include pain, fever, hypoxia, meds
question
Shock + heart murmur?
answer
TR most commonly. Rule out structural disease.
question
Urine output with shock?
answer
< 1 mL/kg/hour or declining
question
CRT
answer
- be consistent with testing - hold for 5 seconds - compare upper and lower body, if >3 second discrepancy, alert staff
question
Pulse Pressure
answer
1. Normal - term: 25-30 - preterm: 15-25 2. Narrow - peripheral vasoconstriction - HF - compression on heart (pneumopericardium, effusion, tension pneumo) - severe aortic stenosis 3. Wide - large aortic diastolic run off lesion (PDA, AVM, truncus arteriosus, AR) - sepsis with vasodilated (warm) shock
question
Hypovolemic Shock
answer
1. Causes - acute blood loss intrapartum `placental abruption or previa `umbilical cord injury `organ laceration (spleen or liver) `fetal-to-maternal hemorrhage `TTTS - postnatal hemorrhage `brain, lung, adrenal, scalp - obstructive `tension pneumothorax `pneumopericardium - non-hemorrhagic `umbilical cord accident (prolapse, knot, vasa previa) `severe capillary leake secondary to infection `dehydration 2. S/S - tachycardia - weak pulses - prolonged CRT - mottling - cyanosis
question
Cardiogenic Shock
answer
1. Causes - intrapartum or postpartum asphyxia - hypoxia and/or metabolic acidosis - bacterial or viral infection - severe resp distress requiring ventilation - severe hypoglycemia - severe metabolic/electrolyte disturbance -arrhythmias - CHD
question
Septic/Distributive Shock
answer
- hypotension that responds POORLY to fluid resuscitation - loss of vascular integrity, fluid leaks out of vessels into tissues - infants often need BP meds to treat severe hypertension
question
Labs for Shock
answer
1. Blood Gas 2. Blood lactate 3. CBC + differential 4. Cultures 5. LFTs 6. Coag studies 7. Glucose - in response to stress/catecholamines, may be initially hyperglycemic; glucose utilization can be markedly increased which raises risk for hypoglycemia 8. Electrolytes - hypo- or hypernatremia, hypo- or hyperkalemia 9. Ionized Calcium - calcium needed for myocardial contractility, if it is low other inotropes will be significantly less effective 10. Renal Function tests 11. Cardiac enzymes - BNP, Troponin, CPK-MB to look for myocardial tissue injury 12 .Others: - ECHO, ECG - Evaluate urine output for oliguria or anuria
question
Anion Gap
answer
Na - (Cl + HCO3) Normal for neonates is 5-15 1. High: - lactic acidosis - ketoacidosis - renal failure - late metabolic acidosis - toxins 2. Normal - loss of bicarb, usually GI or renal losses - excessive Cl in fluids - aldosterone deficiency - hyperchloremia is a compensatory mechanism 3. Low - caused by hypoalbuminemia
question
Ionized Calcium
answer
- the best indicator of physiologic blood calcium activity - hypocalcemia: < 4.4 mg/dL (1.1 mmol/L) - if there is insufficient Ca available for myocardial contraction, other inotropes will be significantly less effective
question
Cardiac Enzymes
answer
BNP - raised in: - CHF - Pulmonary Htn - CHD - Septic shock Troponin - newborns have slightly higher levels than adults - increased levels when asphyxiated
question
Treating Shock, general principles
answer
1. Identify cause, start treating e.g. antibiotics for septic shock 2. ID can correct any related or underlying problems that may impair heart function (e.g. poor cardiac filling b/c of hypovolemia, tamponace, hypoglycemia, arrhythmias, hypoxemia) - volume infusions, +/- inotropic medications 3. Support ventilation and oxygenation
question
Treatment of Hypovolemic Shock
answer
1. No acute blood loss - NS 0.9% 10 mL/kg/dose IV/UVC/IO over 15-30 minutes - may need 2 or 3 more boluses if severe - monitor response (HR, perfusion, BP) following each bolus 2. Acute blood loss - give NS while awaiting pRBC or whole blood - Type O- or cross matched - 10 mL/kg/dose IV/UVC/IO over 30 min to 2 hours - get newborn screen before any blood transfusion, but don't delay tx ** if there is a hx of chronic blood loss, some infants in severe shock may not tolerate volume boluses - VLBW infants would benefit from: a) Leukoreduction of cellular products (pRBC or platelets) for CMV safety +/- b) Irradiation of cellular products to reduce risk of transfusion-associated graft-versus-host disease - all babies who receive a blood transfusion must receive filtered cellular products
question
Treatment of Cardiogenic Shock
answer
- correct underlying problems that may negatively affect heart function: `hypoxia `hypoglycemia `hypothermia `hypotension `acidosis `arrythmias `infection `electrolyte imbalance
question
Treatment of Septic Shock
answer
- may require more fluid boluses - may need continuous dopamine infusion to help hypotension - optimize ventilation and oxygenation
question
Other medications used for Shock
answer
1. Sodium bicarbonate 4.2% solution - tx severe acidosis (pH ; 7.15) - dose: 1-2 mEq/kg/dose (2-4 mL/kg/dose) IV over 30-60 minutes - too rapid administration can cause IVH in premies - infant must be adequately ventilated when administered or acidosis will worsen b/c of increase in CO2 as bicarb is metabolized 2. Dopamine Hydrochloride - for poor cardiac contractility; alpha receptors activated, vasoconstriction, increased systolic and diastolic BP; but after trial of fluid bolus - dose: 5-20 mcg/kg/min IV continuous pump ** do NOT give via arterial route or through an ET tube - mixed in D5W, so monitor blood glucose - monitor BP and HR every 1-2 minutes for 15 min then every 2-5 depending on response to medication - if fails to respond to 20mcg/kg/min, then increasing dose further is NOT recommended ** do NOT flush lines containing dopamine! - recommended to give via central line b/c extravasation can cause tissue necrosis - if in a peripheral IV and get extravasation - inject saline solution containing phentolamine mesylate
question
Caput Succedaneum
answer
- molding of head during labour, causing superficial edema - in subcutaneous tissues of scalp; can cross suture lines - shifts with position - soft and spongy, pits on pressure - resolves in 48-72 hours
question
Cephalohematoma
answer
- hemorrhage under the periosteum - does not cross suture lines - usually over parietal or occipital bones; may be bilateral - initially firm, more fluctuant after 48 hours - x-ray skull if fracture is suspected - resolves in 2 weeks - 3 months - blood loss rarely severe
question
Subgaleal hemorrhage
answer
- rupture of emissary veins, which bring blood from scalp to dural sinuses, bleeding into subaponeurotic space, above periosteum - can occur in vacuum deliveries due to traction applied, or as a consequence of pop-offs during vacuum assisted delivery - can cross suture lines; may extend from eyes to nape of neck; swelling can extend to ears, eyes - firm, fluctuant, boggy - may lead to severe anemia and hypovolemic shock - resolves in 2-3 weeks - can be tx: tx anemia, stop bleeding, restore BP --> pRBCs, FFP, platelets, cryoprecipitate, NS volume infusions, dopamine - RF for SGH after VAD: `nulliparous mothers `failed vacuum extraction `pop-offs `sequential use of vacuum and forceps `APGAR <8 at 5 minutes `paramedian or deflexing cup application
question
Risk Factors for Neonatal Infection
answer
- PPROM - Premature onset of labour - Rupture of membranes ; 18 hours - Chorioamnionitis (maternal signs!) - Recent maternal illness/infection - Maternal fever in peripartum period - Maternal GU infection - Perinatal asphyxia - CVS, amniocentesis - Fetal scalp electrode, vacuum - IV lines, invasive procedures
question
Neonatal sepsis
answer
- early onset (first 72 hours) vs late - GBS and E. coli commonest - viruses: HSV, HIV, Hep, CMV, Parvovirus, Rubella
question
HSV
answer
- infants who are exposed at birth may not have symptoms for 3-7 days - can p/w vesicles as well as: poor feeding, lethargy, fever, shock - Tx: aciclovir, while awaiting confirmatory culture/PCR
question
4 B's of labs for ?infection prior to transfer
answer
1. Blood count (CBC) 2. Blood culture - at least 1 mL/culture bottle (if not enough blood, take aerobic before anaerobic) 3. Blood glucose 4. Blood gas
question
Labs for after transfer
answer
1. CRP - normal: < 1.6 in first 2 days of life, < 1 mg/dL after - does not cross placenta - higher levels with: infection, resp illness, after surgery, after vacuum or forceps, immunizations, bruising, vaginal birth (rel to c-section) - does not rise immediately but within 4-8 hours - not always positive with sepsis 2. CSF - for meningitis - gram stain and culture, cell count, glucose and protein conc 3. Electrolytes, Ionized calcium, Mg - Mg if the mother was given MgSO4 during labour 4. Renal function tests 5. LFTs, including coag
question
In an ILL neonate with normal CBC and CRP?
answer
NEVER withhold antibiotic treatment because of these normal results. There is a 4-6 lag for CBC and 8-12 hour lag for CRP.
question
Left shift
answer
The presence of immature neutrophils in the blood
question
Immature to Total Ratio (I/T)
answer
I/T = {band + metamyelocytes %}/{band + metamyelocytes + segs} - proportion of immature (band + metamyelocytes) to mature (segmented) neutrophils - most sensitive for estimating risk that infection may be present ** when > 20-25%, suspect bacterial infection **
question
Absolute Neutrophil Count (ANC)
answer
ANC = {segmented neutrophil + band neutrophils + metamyelocytes} (count, %) * WCC (# cells) - normally, the WBC and neutrophil counts rise for the first day after birth; in term infants, neuts peak at 8 hours ** Therefore, a DECLINING neutrophil count (rather than the expected physiologic rise) should raise concern that the infant may be infected ** - low ANC means depleted neutrophil reserves, which means high risk of dying from sepsis - infants born to hypertensive mothers might have low ANC compared to others; also with trisomies - ANC increases with increasing gestational age - use ANC charts which considers hours from birth for different gestational ages
question
Thrombocytopenia
answer
1. Causes - infectious - maternal conditions (PIH) - maternal auto- or isoimmunization (SLE, ITP) - genetic (familial thrombocytopenia, trisomies) - NEC, hyperviscosity, DIC following perinatal asphyxia, metabolic 2. Levels - mild: 100-149 - mod: 50-100 - severe: < 50k ** levels increase with gestational age 3. Evaluate - for signs of bleeding - e.g. from mucosal sites, lines, petechiae, bruising
question
Ampicillin
answer
Dose: 50 mg/kg/dose < 29 weeks: 30-36 weeks: 37-44 weeks: - every 12 hours - IV slow push over 3-5 minutes, not faster than 100 mg/min S/E: - prolongs bleeding time because impacts platelet function; use with caution
question
Gentamicin
answer
- different dosing recommendations based on gestational age - generally dose 4-5 mg/kg every 24-36-48 hours - IV over 30 minutes - can also be given IM Levels: - peak therapeutic range 6-12 mcg/mL - trough therapeutic range 0.5-1 mcg/mL - if worries about renal function, trough can be obtained before second dose - when given for 5-7 days, do levels *Traditional dosing: 2.5 mg/kg/dose, q12-18-24 hours IV - trough 0.5-2 mcg/mL, peak 5-10 - check trough before 3rd dose, then peak after (if given for > 3 days)
question
When to do an LP?
answer
Indicated in any infant with a positive blood culture or in whom sepsis is highly suspected based on clinical signs, response to tx, and §lab results.
question
Evaluating Asymptomatic Infants with RF for Sepsis
answer
RF: chorioamnionitis, PROM > 18 hours, IAP indicated but not adequate --> blood culture at birth, WBC/diff +/- CRP at age 6-12 hours --> if: a) cultures +: continue Abx b) cultures -, infant well, labs abnormal: continue Abx if mother received Abx during L&D c) all neg/normal: discontinue Abx ** note in term with no chorioamnionitis but PROM > 18 hours, do not empirically tx with Abx, if labs abnormal check culture



