SAB, Epidural Anesthesia – Flashcards
Unlock all answers in this set
Unlock answersquestion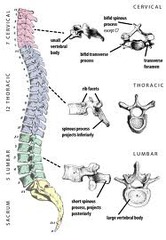
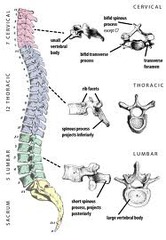
Vertebral Column
answer
-Cervical (7) and thoracic (12) vertebra spinous process angels caudad, tight angles, more difficult to insert needle - Lumbar (5) vertebra, shorter and broader, less overlap, easier access for needle placement, catheter passage, and the instillation of anesthetic into the epidural or subarachnoid space -Sacral horns important landmark for performance of a caudal anesthetic procedure - 33 total vertebrae, 24 movable
question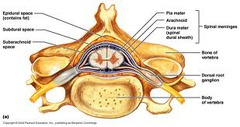
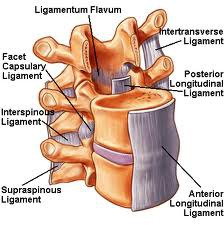
Which three spinal ligaments are of special interest to the anesthetist?
answer
-Supraspinous ligament - intraspinous ligament (thin) - ligamenta flava ("buttery") Landmarks that help identify and access the epidural and subarachnoid spaces. Pass through all three for epidural placement. Anterior: body Posterior: vertebra foramen
question
Facets & pain relief
answer
Compression of facets cause nerve pain, medication injected here is diagnostic if pain is relieved. Block with LA to relieve pain.
question
Transforaminal approach
answer
For temporary relief of bulging disk pain
question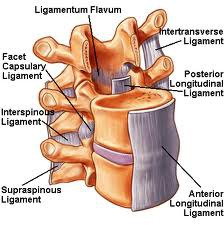
Supraspinous Ligament
answer
-Strong cordlike ligament connect apices of the spinous processes and is major ligament in the cervical and upper thoracic regions
question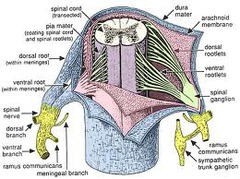
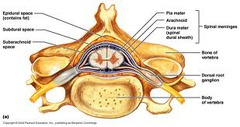
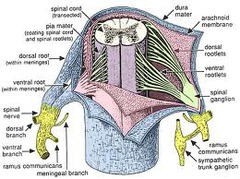
Spinal cord ligaments & meniges
answer
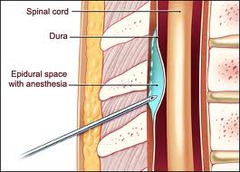
Dura: outermost, tough Arachnoid: thin, spider-like Pia: thin and in direct contact with outer surface of spinal cord Subarachnoid space: continuous with central canal of the spinal cord and ventricles, medium for the interaction with local anesthetics and opioids during regional anesthesia Epidural space: potential space outside of the dural sac inside the vertebral canal, tri-podal dune like space
question
Ligamenta Flava

answer
-Strongest of the posterior ligaments -Paired flat ligaments - 3-5mm at L2-L3 interspace -High content of elastic tissue, yellow
question
How much distance is there between the skin and the lumbar epidural space?
answer
- 2.5-8cm with the average being 5cm *Art says 6-7cm average -Epidural space is largest in the midline of the mid lumbar region, at 5-6mm -Stay midline to avoid veins and access largest space (especially with pregnancy, swollen veins)
question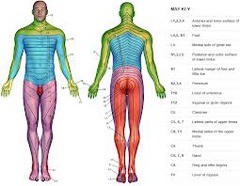
Neuroanatomic Mapping & Evaluation of Neuraxial Anesthesia
answer
- Use dermatomes to determine functional level of blockade - "Straight leg" or "step on the gas" - Cutaneous sensation, pin, nerve stimulator
question
What are the epidural levels for common procedures?
answer
-L1-L2: perianal -L2 or L3: labor or lower abdominal anesthesia - T8-T10: upper abdominal surgery, total hip - T4-T8: c-section - T4-T5: thoracic surgery - C7-T1: chronic pain treatments or arm, shoulder or upper chest surgery
question
T4 block symptoms?
answer
Can't breathe, bradycardia, hypotension, hands tingling or swollen
question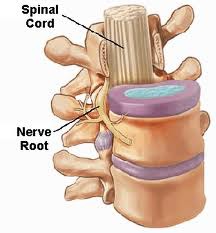
Physiology and Mechanism of Action
answer
- Primary site of action for local anesthetics is on the nerve roots within the spinal cord - Drug distributes through subarachnoid space and spreads - Neuronal transmission is altered and provides anesthesia - Affects sodium channels and inhibits information from being transferred along the spinal cord
question
What is a "differential block"?
answer
-When a local anesthetic interrupts nerve transmissions of autonomic nerves but not sensory nerves or motor nerves. - Can get sympathetic blockade as high as 6 dermatomal levels above injection site. -Hypotension & bradycardia
question
Central Neuraxial Blockade (CNB) Indications
answer
-Inpatient and ambulatory surgeries, lower extremities, perineum and abdomen - used in combination with other techniques to minimize side effects of any one technique Considerations: 1- Will patient be comfortable? 2- Able to remain in required position? 3- Does regional technique outweigh risks of alternate anesthetic technique?
question
CNB Advantages
answer
-Less N/V and urinary retention - Reduced total opioid requirement & can administer long acting analgesics or clonidine -Greater mental alertness - Quick to eat, void and ambulate - Improved outcomes, especially in high risk patients - Blunt body's stress response
question
CNB Contraindications/Disadvantages
answer
- History of HA or backache increases risk of these complications post-op -Backache, postdural puncture headache (PDPH) hearing loss, transient neurologic symptoms, infection and abscess or hematoma formation - If elevated ICP, increased herniation risk - Avoid with musculoskeletal disorders - May worsen diabetic neuropathy - Shock or severe uncorrected hypovolemia - Fixed-volume cardiac state - Arthritis or elderly who can't be immobile easily
question
Do SAB or epidurals often cause respiratory changes?
answer
Rarely affects pulmonary function because diaphragm isn't paralyzed but intraabdominal or intercostal muscle paralysis is present.
question
CNB and Coagulation
answer
-Existence of significant pre-existing or therapeutic coagulopathy increases risk of hematoma formation - Avoid: platelets <100,000, aPTT and bleeding times twice normal values
question
CNB and Medications
answer
-ASA and NSAIDS are safe -Herbal therapy is safe (DC 7 days if possible) - Heparin: have normal aPTT, indwelling catheters should be removed 2-4 hours after last heparin dose -Warfarin: INR <1.5, do not pull cath until INR <1.5 - Should not perform CNB if fibrinolytic or thrombolytic therapy in past 10 days.
question
What is a "total spinal"?
answer
-Spinal reaches too high and causes unresponsiveness accompanied by cardiac and respiratory compromise.
question
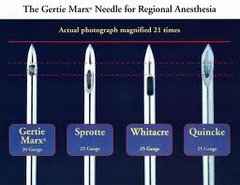
Most blocks are performed with what type of needle?
answer
- 25-27g - 3.5 inch
question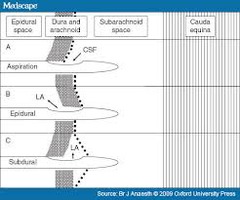
What are some advantages of a "non-cutting" needle? (AKA pencil-point needle)
answer
- Encourages midine insertion - Fewer skin contaminates into subdermal tissue - Clearly perceptible "pop" when the dura is pierced - Improved CSF rates - Reduction in PDPH <1% risk - Failure rate <5%
question
Surgical or OB spinal
answer
- C shaped "like a Halloween cat" - Intercristal or Tuffier's line is line between iliac crests at L4 process - Betadine left on for 1 minute for efficacy - 1% lidocaine around insertion, 3-5 ml - For needle<25g use introducer, 18-20g blunt 3.8cm - Dura anywhere from 2.5-9cm in, average 4-5cm
question
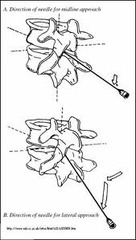
Straight Midline Approach
answer
-Insert needle directly midline between the spinous processes and toward the umbilicus -Slight caudad angle, perpendicular - "Pop" when through dura
question
What is a Bromage grip?

answer
Uses patient body to stabilize needle
question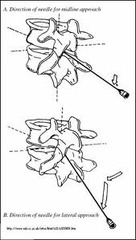
Paramedian Approach
answer
-Needle inserted 1 cm to the caudad aspect of interspace, 1 cm lower and over - Then direct towards spinal canal and angle slightly cephalad -Angle medially 10-15°
question
The paramedian approach passes through which ligaments?
answer
Ligamenta flavum only
question
Someone with scoliosis needs which approach?
answer
Nearly paramedian, angle needle towards processes inside, vertebrae rotate inward
question
Taylor Approach
answer
- L5 interspace - 1cm medial and 1 cm caudad to posterior superior iliac spine - Needle angled medially and cephalic at a 55° angle towards 5th lumbar interspace
question
What is the specific gravity of CSF?
answer
- 1.004-1.009 -500ml produced each day - 30-80ml present in spinal cord
question
What is baricity?
answer
- Resting position of two fluids with differing specific gravities when the fluids are mixed in a single container - CSF & anesthetic agent - Helps determine the spread of the anesthetic mixture into the subarachnoid space
question
When baricity is =1 the solution is?
answer
- Isobaric, not possible to make exact isobaric solution since variance in CSF exists but near isobaric solutions act in approximately the same location they are injected in
question
When baricity is <0.999 the solution is?
answer
- Hypobaric - Less dense than CSF, will rise or float to the highest anatomic position possible - Usually mixed with sterile water
question
When baricity is >1.0015
answer
-Hyperbaric - More dense than CSF, will sink to lowest anatomic position possible - Usually mixed with 5-8% dextrose
question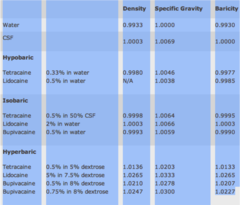
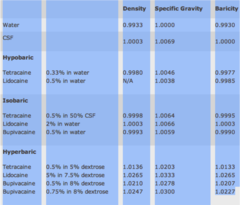
What are the various baricities of drugs?
answer
...
question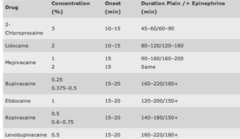
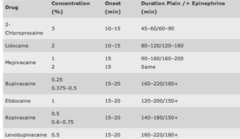
Drugs and epidural dosing...
answer
...
question
Agents
answer
Spinal: isobaric or hypobaric 5% lidocaine with or without epi, hyperbaric 0.75% bupivicaine, isobaric or hyperbaric 1% tetracaine Epidural: 2% lidocaine with or without epi, 0.5-0.75% bupivicaine, 2-3% 2-chloroprocaine, 1% ropivicaine
question
Which drugs have the longest duration, why?
answer
- Tetracaine, bupivicaine and ropivicaine are more protein bound, longer acting - Lidocaine and mepivicaine less protein bound, shorter acting
question
SAB/Epidural Additives
answer
Duramorph: 2.5-5 Fentanyl: 25-100mcg Sufentanil: 2.5-5 mcg Demerol: 25-100mg Dilaudid: Epinephrine: Clonidine: 75mcg epidural 15-30mcg spinal Phenylephrine: 5-10mcg spinal
question
What is tachyphylaxis?
answer
Acute sudden reduction in response to drug, need more drug for same response. Upregulation, replace epidural or move slightly.
question
How long would the duration of a spinal be increased if you increased hyperbaric bupivicaine from 10mg to 15mg?
answer
50% and increases maximum sensory level achieved
question
What is one consideration for OB patient and spinal anesthesia?
answer
-Epidural veins are engorged and they will have slightly higher level of spinal anesthesia
question
What is cauda equina syndrome?
answer
-Persistent paralysis of the nerves with lower extremity weakness and bowel and bladder dysfunction - Caused by deposition of neurotoxic concentrations of hyperbaric anesthetics particularly 5% lidocaine
question
What is transient neurologic symptoms, TNS?
answer
- Pain originating in the gluteal region that radiates to both lower extremities - Few hours- 24 hours after recovery - Last as long as 10 days, resolve spontaneously
question
What are some physiological effects of spinals and how are they managed?
answer
-Somnolence: decreased number of sensory impulses - Bradycardia & hypotension: if block is high enough paralyze nerve fibers that innervate heart, "cardiac accelerators", T1-T4 Treat hypotension: when >20% drop from baseline BP with crystalloids 15ml/kg 15 minutes before procedure Treat bradycardia: α-agonist, 50-100mcg IV phenyleprhine, or atropine 0.4-0.8 mg - GI: Will ↑ peristalsis, GI blood flow, causes N/V Treat: atropine provides indirect antiemetic effect - Urinary retention Treat: catheter
question
Post Dural Puncture Headache (PDPH)
answer
- 0.2-24% - Decreased circulating CSF, leak through dural puncture site - Stretches meninges and tentorium. - Young, female, pregnant at risk - Pain radiates from behind eyes and across head to neck and shoulders - Resolves spontaneously 10 days - Treated with theophylline, caffeine (300mgPO or 500mg IV) and supine position -Postural headache is diagnostic for PDPH
question
Blood Patch for PDPH
answer
- Definitive treatment, <90% cure - Autologous blood 20ml from vein into epidural space - Patient will feel at 12-15ml -Supine at least ½-1 hour post patch *Art says 24 hours... - Do not use with infection/ fever
question
PDPH risks
answer
Lumbar puncture>spinal>epidural
question
Epidural dosing for T8 block
answer
10x volume of spinal 1.5cc/level times
question
Nausea with CNB
answer
- Initial nausea caused by hypotension - Give fluids 15 minutes before spinal - ↑ GI motility - Propofol and midazolam have anti-emetic effects - Epi ↑ PONV - Addition of fentanyl (25mcg) or sufentanil (2.5-5mcg) to spinal ↓ PONV
question
What causes nausea and vomiting post epidural?
answer
Hypotension Ischemia in the vomit centers of the medulla, Ischemia of gut releasing emetogenic substances like serotonin *Treat pressors (ephedrine/neo), propofol, zofran
question
Urinary Retention & CNB
answer
-CNB blocks sympathetic fibers and increases urethral sphincter tone - Cath as last resort
question
Neurologic Risk & CNB
answer
- Patients concerned with risk of paraplegia - Very rare, nerve injury <1:10,000 - Reversibility of complication is time dependent
question
Unexpected Cardiac Arrest & CNB
answer
- Often occurs in young, previously healthy patient - 0.04:10,000-6.25:10,000 - Downward trend in HR followed by abrupt onset of severe bradycardia or systole - Associated with intra-op significant blood loss and orthopedic cement placement - May happen as late at 3 hours post placement Treat: IV fluids, atropine, cardiac resuscitation dose of epi
question
Auditory, Ocular and Facial Complications
answer
- Transient hypoacusis or hearing loss - Retinal hemorrhage - Caused by changes on CSF pressure - Usually self-limiting
question
What is the difference between a spinal and an epidural?
answer
-A spinal is an "all or none" CNB, puncture through dura - An epidural is titratable and allows better control of analgesia, do not puncture through dura, push away from the dura
question
What is the standard epidural needle size?
answer
- 16-18g - 3 inches long - blunted bevel, gentle 15-30° curve at tip - blunted bevel and curve allow needle to push away form dura instead of penetrate it
question
Tuohy needle

answer
-30° curve - Easiest for beginning practitioners - Directional placement - Less likely to puncture subarachnoid space - may inhibit penetration of skin and ligament flava as compared to other needle tips
question
Hustead Needle

answer
-Intermediate needle - 15° curve - Passes easily through skin and ligamenta flava
question
Crawford Needle

answer
- Straight tip - Used with difficult epidural space (calcified lesions) - Higher ratio of accidental dural puncture - Not used by beginners
question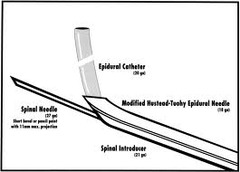
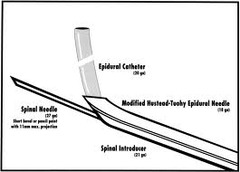
Combination epidural/ SAB Placement
answer
...
question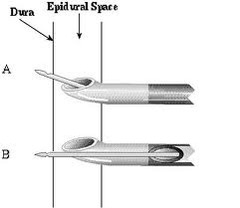
Combination needle
answer
...
question
What size catheters are used with epidural needles?
answer
-Typically 2 sizes smaller -EG 20g catheter with 18g Tuohy
question
Which distance seems to offer the greatest epidural success without causing migration?
answer
- Thread catheter 3-5 cm -5 intravenous cannulation *Art threads deep then pulls back. Big line mark indicates catheter is past needle, each mark on catheter is 1 cm. Needle at hub is 9cm (usually 6-7cm in before hit space)
question
What is the loss of resistance technique?
answer
- Most commonly used technique - Needle through dermis into interspinous ligament flava, stylet of epidural removed - Loss of resistance syringe with 2-3ml of normal saline and freely moveable plunger - As needle goes through ligamenta flava resistance increases - Loss of resistance when in epidural space
question
What causes the "funny bone" sensation in the legs after epidural?
answer
- Parathesia felt down one or both legs indicate the catheter brushed by a nerve root as it was passing into epidural space
question
What is the purpose of a "test dose"?
answer
- Determine catheter placement. - 3 ml of rapid acting, low toxicity anesthetic, lidocaine 1.5% with 1:200,000 epi (45mg lido:15mcg epi) - Subarachnoid space: spinal anesthesia within 3 mins - Blood vessel: 20% rise in HR and SBP within 30sec, metallic taste, mouth tingling etc. - 100mcg fentanyl can alternatively be used
question
Can you withdraw the catheter through the needle?
answer
- No, this can shear the catheter and embed foreign material into the patients back
question
What are the suggested volumes per segment?
answer
-Cervical and thoracic: 0.7-1ml/segment EG: initial dose <10ml 10-14 dermatomal spread - Lumbar: 1.25-1.5 ml/segment EG: initial dose 15-20ml 12-16 dermatomal spread
question
What factors affect epidural spread and what type of injection techniques can be used?
answer
- Spread of epidural anesthetics may be 3-4 dermatomes greater in elderly patients because of less compliant, less leaky epidural space -Also happens in pregnant patients - Limit to 0.5-1ml/segment initially
question
Spinal is located?
answer
Subarachnoid space
question
Spinal dosing for T8 block
answer
5 feet= .075-.1 cc
question
How should all solutions be injected?
answer
- 3-5ml every 3 minutes titrated to anesthesia level
question
Intermittent injection & continuous infusion
answer
- Intermittent used when high concentration of local anesthetic is administered (2% lidocaine, 0.5 bupivicaine) - Continuous used with lower concentrations of local anesthetic ( 0.0625%- 0.125% bupivicaine, or 0.1-0.2% ropivicaine -Opioid infusion of 2ml/hr for morphine up to 20ml/hr for dilute local (0.125% bupivicaine or 0.1% ropivicaine)
question
Epidural opioids
answer
- May undergo uptake into the epidural fat, systemic absorption or diffusion across the dura into the CSF -Must cross from epidural space to reach opioid receptors in the substantia gelatinosa - Dose is increased 10x from intrathecal dose - Significant absorption into systemic circulation
question
How long until maximal spread occurs?
answer
10-25 minutes When level regresses 1-2 dermatomes detected by scratch or ice test, 30-50% of initial dose is given.
question
What technique is attributed to causing one dermatome to remain unaffected?
answer
- Using an air bubble with the loss of resistance technique. -Recommended to use NS, no air
question
Complications of Epidural Anesthesia
answer
- Use of plain local creates high level of blockade, this will decrease MAP, CO, SV, HR & PVR Treat: ephedrine 5-10mg, phenylephrine 50-100mcg or low dose dopamine HR: atropine or robinul -Backache 30-45%, especially in OB patient, ketoralac 2mg/kg decreases - Dural perforation "wet tap" will cause PDPH
question
Epidural is located?
answer
Above dura
question
What is the most critical element to epidural placement?
answer
Positioning, legs up, curled up
question
Combined Spinal and Epidural Anesthesia CSE
answer
- OB, post-op pain relief - Advantages of each technique while reducing or eliminating disadvantages - Quicker onset of a spinal combined with flexibility of an epidural
question
Two-level technique
answer
- Epidural placed then spinal anesthesia 1-2 interspaces lower - Able to test epidural catheter first then place spinal - Risk:↑ trauma, hematoma, infection
question
Single Level Technique: Needle-through-needle
answer
- Insertion of an epidural needle at appropriate interspace then using epidural needle as a guide - Pencil point spinal inserted through epidural needle into subarachnoid space, local injected - Spinal needle removed, epidural catheter threaded into place - Risk: nerve root trauma, difficulty obtaining CSF
question
Sequential Technique
answer
- Epidural needle placed at the selected interspace, low dose spinal placed using needle-through-needle technique - Patient supine with left lateral tilt - After 15 mins block extended by titrating epidural local anesthetic until desired level achieved
question
CSE technique and OB
answer
- Rapid onset of intrathecal - Minimal intrathecal opioids in early labor allow ambulation - Epidural needle followed by spinal with needle-through-needle, intrathecal opioids 5-15 sufenta or 25-50mcg fentanyl and/or 2.5 mg bupivicaine -Spinal withdrawn, epidural inserted -Can provide anesthesia for cesarean -Sufenta may cause hypotension - CSE allows faster onset, denser block, lower anxiety, lower pain, greater patient satisfaction
question
Complications of CSE
answer
- Failure to obtain SAB: 3.1-17%, needle misplacement, have longer, 7-15mm, beyond tip of epidural needle, orient bevel upward - Catheter migration: through the dural puncture caused by introduction of the spinal needle -Increased spinal level: more volume more spread, leak from epidural into subarachnoid space -Metallic particles: produced, not proven -Postdural puncture headache: lower incidence, better needle approach, CSF leakage abated, angle seals holes in dura - Infection:slightly increased risk -Neurological injury: 0.02-0.1%
question
What lab value should you check every day when an epidural is in place?
answer
INR want <1.5 Over 3 hold dose of blood thinner Also check platelets (less than 100,000 worrisome)
question
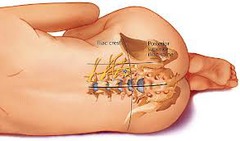
Caudal Anesthesia
answer
-Distal approach to epidural space - Perineal surgeries, OB, urologic, peds - Combined with light GA
question
Caudal Equipment & Techniques
answer
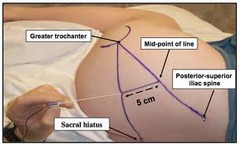
- Prone or lateral with knees to chest - Posterior iliac spines & sacral hiatus - 22g-25g short needle with 10ml local inserted midline between cornua at a steep angle into sacral hiatus - Popping sensation as ventral canal of sacrum entered - Needle lowered parallel advanced into epidural space
question
Caudal Anesthesia Agents
answer
- 0.5-1 ml of solution per kg (kids) - Bupivicaine or ropivicaine 0.125-0.5% - Epi max 2.5mg/kg of 1:200,000 - Clonidine 1mcg/kg for opioid - 12-15ml for sacral and up to 20-30 for lower extremity procedures
question
Management & Complications of Caudal Anesthesia
answer
- Similar to epidural - Sacral area has epidural venous plexus (IV injection) - Infection due to proximity to anus
question
What contributions did LaFargue and Pravaz & Rynd make to the advancement of regional anesthesia?
answer
- LaFargue: needle trochar, morphine under skin - Pravaz: hypodermic syringe - Ryng: hollow needle for delivering hypodermic medications
question
When is regional anesthesia used?
answer
- When local anesthesia requires supplementation with heavy sedation - Choice with difficult airway or full stomach - Permits patient to maintain upper airway and pharyngeal reflexes - NOT an alternative to securing the airway - C-section, TURP, cerclage, total hip, ankle fracture, trauma, aortic stenosis
question
What are some absolute contraindications to regional anesthesia?
answer
- Patient refusal - Coagulation deficiencies: Platelets 2x normal values - Hypovolemic shock (as regional may drop BP) - Abruptio placentae- hypotension will further reduce already low blood flow to fetus, uterine blood flow has few autoregulatory capabilities - Infection at the site - Can't get informed consent - Increased ICP
question
What are some relative contraindications and precautions to regional anesthesia?
answer
- Neonates: used cautiously when either surgery of pain management is required - Children: regional used for post-operative pain relief, easy landmarks, Bier block frequently used with arm fracture - HA or backache history - Underlying neurological disorder - Local anesthetic allergy (may use another chemical class EG ester or amide) - Mobitz 1 or 2 or pacemaker, regional may increase degree of heart block - Spinal issues, fusion, HELLP, DIC, vW disease - Fixed volume cardiac states -Hypovolemia/shock - Increased ICP, neuro issues - NSAIDS and ASA not absolute contraindications
question
What are NOT contraindications?
answer
NSAIDS and ASA Herbals alone
question
What are some complications of regional anesthesia?
answer
- Immediate complications: IV injection risk when tissues are around nerves or blood vessels and local is high volume, toxicity can occur LAST: cardiac dysrythmia, respiratory and CV collapse - Continuous peripheral nerve block complications: Catheter infection, neuro deficits, vascular puncture, bleeding, dyspnea, catheter dislodgment Benefits:Improves postoperative pain control, reduces opioid requirements, decreased PONV
question
Technical Difficulties and Regional Anesthesia
answer
- Broken needles, broken catheters, glass in epidural and subarachnoid spaces, wrong drug injected - Needle breaking: weakest at hub, avoid bending and extreme force - Broken or sheared catheters: as it is pulled back may be sheared off, NEVER pull back through the needle, most can be left in place unless in subarachnoid space. Risk of migrating cephalic reaching spinal cord or through foramen of nerve root. - Glass: break ampules away from tray, use filter needle
question
Regional Anesthesia Discharge Information
answer
- Regional is injection that numbs nerves that sense pain. - Site will be numb up to 24 hours, wears off slowly. - When sensation begins to return start pain meds. - Protect numb area from inadvertent injury. Return to hospital if: -Sensation not returning after 24 hours - Area was numb, sensation returned, numb again - Skin becomes blue or cold - Persistent pain in area that was numb several days after surgery
question
What is the mechanism of action of local anesthetics?
answer
- Primary function is to restrict movement of sodium into the cell. 1: Calcium ions are displaced from the receptor site 2: Reduction in cell permeability to sodium ions 3: Rate of depolarization of the membrane action potential is decreased 4: Cell cannot reach threshold 5: Action potential does not occur 6: Conduction blockade results
question
Synthetic local anesthetics have what kind of chemical structure?
answer
- Weakly basic tertiary amines that are not readily soluble in water
question
How are local anesthetics made soluble?
answer
- Dissolving local anesthetics into hydrochloric acid, producing water solubility -When in aqueous solution anesthetic dissociates into positively charged quaternary amine (cation) and an uncharged tertiary amine base (free base)
question
What effect does infection or a low tissue pH have on local anesthetics?
answer
- Local anesthetic has difficulty diffusing across the cellular membrane - Not enough positively charged cations to cause membrane stabilization
question
What are the two short acting LA?
answer
- Procaine and 2-chlorprocaine
question
What are the three moderate acting LA?
answer
- Lidoccaine, prilocaine, mepivicaine
question
What are the 4 long acting LA?
answer
-Tetracaine, bupivicaine, ropivicaine and chirocaine
question
What is the chemical composition of LA?
answer
- Aromatic group (benzene) lipid - Intermediate bond: either ester or amide - Tertiary amine
question
How are the LA esters and amides metabolized?
answer
- Esters: plasma and tissue cholinesterases - Amides: metabolized in liver
question
Which are longer acting amides or esters?
answer
- Amides are longer acting because they are more lipophilic and protein bound and require transport to the liver for metabolism.
question
Which drugs have tend to cause allergic reactions, amides or esters?
answer
-Esters: If a patient is allergic to one ester, cannot receive ANY ester, may receive amide, no cross allergy between esters and amides (Allergy to amides is very rare)
question
Most people allergic to local anesthetics are actually allergic to what?
answer
PABA (paraben) which is a preservative included in locals. Allergic to sunscreen or lotions will alert you to PABA allergy.
question
Which LA are esters?
answer
Cocaine, procaine, chlorprocaine, tetracaine, benzocaine *One "I" = ESTER
question
Which LA are amides?
answer
Lidocaine, prilocaine, ropivicaine, bupivicaine, articaine, mepivicaine * Two "I's"= AMIDE
question
Most anesthetics produce vasodilation since they relax smooth muscle, which two cause vasoconstriction?
answer
- Cocaine and ropivicaine cause vasoconstriction
question
Why is epinephrine added to LA?
answer
- Prolongs the duration of action by slowing the uptake of the local anesthetic. -Phenylephrine 100mcg may alternately be used
question
What is the concern with prilocaine metabolites?
answer
- Prilocaine is metabolized into o-toluidine which can cause methemoglobinemia, especially if dose is >400mg Treat: methylene blue 1-5 mg/kg
question
Electrical Stimulators in Anesthesia
answer
- Needle advances slowly and amplitude adjusted as the needle approaches the nerve - Negative lead attached to skin, positive to needle - Stimulator adjusted to deliver 2 mA after in subcutaneous tissues - When needle enters sheath amplitude reduced to 0.5mA - Stimulate at lowest possible for response, once response obtained anesthetic can be administered - Stimulus applied at 2.5mA for 15 seconds at intervals of 10-15 minutes
question
Ultrasond Guided Regional Anesthesia
answer
- direct visualization of the distribution of LA improves quality and avoid complications of blocks - best to being learning blocks on peripheral nerves using ultrasound under supervision before going on to more central blocks
question
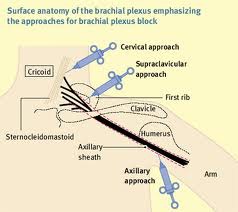
Upper Extremity Blocks
answer
- 4 approaches: axillary, interscalene, supraclavicular, infraclavicular - Most frequently used is axillary due to ease of performance and high success rate. Used for forearm and hand. - Interscalene: upper arm and shoulder
question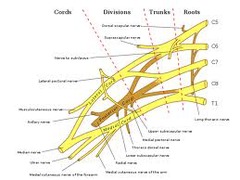
Brachial Plexus Block
answer
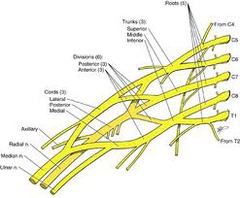
- Rami, trunks, divisions, cords, branches - Nerve trunks enveloped by sheath, posterior fascia of the anterior scalene and anterior fascia of middle scalene form interscalene space AKA sheath of brachial plexus - A single injection into this sheath often produces complete block for the upper extremity
question
Interscalene Space/ Sheath of Brachial Plexus

answer
...
question
Axillary Approach to Brachial Plexus

answer
- Best suited for procedures at or below the elbow - Supine, arm abducted 90°, forearm flexed 90° - Well defined pulse in axillary artery more important to successful blockade than the point of needle insertion
question
Loss of Resistance Technique
answer
- "Pop" as needle penetrates fascia and enters the sheath -22g 1½ inche "B" needle inserted medially at 20° angle, parallel to artery - May observe needle for pulsation as confirmation - Advance medially ½-1 inch parralel to axillary artery - Aspirate and observe for blood - 3-5ml test dose of LA - Inject rest of LA in 5 ml increments while aspirating and observing for blood intermittently - Firm pressure above needle to avoid retrograde flow - After 40ml of injection needle is withdrawn - Adduct arm to promote cephalad spread of LA
question
Transarterial Technique
answer
- Uses intentional penetration of brachial artery to confirm needle is within sheath - After artery is ID, wheal of anethstic raised directly above artery - 21g 1½inch needle (or 26g ½inch) inserted perpendicular to skin, and advanced slowly until blood is aspirated - Advanced slowly until blood is no longer aspirated - 3-5ml test dose of LA - Inject rest of LA in 5 ml increments while aspirating and observing for blood intermittently - Firm pressure above needle to avoid retrograde flow - After 40ml of injection needle is withdrawn
question
Interscalene Approach
answer
- Only technique that provides adequate anesthesia to shoulder and the rest of upper extremity - Catheter at level of the trunks - Patients head turned to opposite side - Palpate cricoid cartilage just below thyroid, C6 level (Chassaignac's tubercle) - Straight line drawn posteriorly over SCM - Palpate groove between anterior and middle scalene muscles - 22g, 1½ inch B level inserted into wheal angled caudad - Needle advanced until motor twitch - Lower mA to 0.5 from 1 -Aspirate, test dose - 3-5 ml injection up to 30-35ml
question
Subclavian Approach
answer
-Palpate for pulsations behind and 1-2 cm above clavicle - 22g B needle perpendicular, inward and caudad - Needle advanced until motor twitch - Lower mA to 0.5 from 1 -Aspirate, test dose - 3-5 ml injection up to 30-35ml Watch for Horner syndrome (miosis, partial ptosis, loss of hemifacial sweating) and pneumothorax
question
Intersternocleidomastoid Approach
answer
-Puncture site between heads of SCM muscle, 2 fingerbreadths above sternal notch - At 3-8 cm suprascapular, superior trunk, middle trunk and divisions and cords can be reached - Needle advanced laterally, posteriorly and caudally at 45° angle to table and 15° angle to clavicle -Motor responses at 2-8cm - Lower mA to 0.5 from 1 -Aspirate, test dose - 3-5 ml injection up to 30-35ml
question
Continuous Catheter Technique
answer
-Used for postoperative pain - Continuous administration of LA via brachial plexus catheter at the cervical level reduces opioid requirements and improved analgesia - 22g insulated block needle advanced at C6 level, 45° caudal, dorsal and medial angle - Pop felt upon sheath entrance -NS 5-10ml injected and aspirated for blood - Lower mA to 0.5 from 1 -Aspirate, test dose - 3-5 ml injection up to 30-35ml - Continuous infusion rate 0.125-0.25 at a rate of 4-6ml/hr
question
Selective Blocks at the Elbow
answer
- Primarily sensory blocks, still has motor function - Each nerve blocked at the elbow and wrist - When using tourniquet block intercostobrachial nerve and brachial cutaneous nerve in axilla
question
Ulnar Nerve Block at the Elbow
answer
- Limit volume of solution to reduce amount of pressure and possible ischemia 3-5ml - Elbow flexed 90°, medial condyle of humerus identified - Needle inserted 45° perpendicular to line between medial condyle and olecranon process
question
Median Block at the Elbow
answer
- Anesthesia of forearm and hand - Block median and ulnar nerve - Line drawn from medial to lateral condyles - Brachial artery identified - Short B needle inserted medially to brachial artery at a depth of 0.5-0.75 cm - LA injected 3-5ml, as needle is withdrawn inject 1-2ml to block cutaneous branches of nerve
question
Radial Nerve Block at the Elbow
answer
- Forearm and hand - ID brachioradialis muscle and biceps tendon - Line drawn between medial and lateral condyles - B needle inserted medial border of the brachioradialis muscle -After contact with condyle the needle is withdrawn 2mm - LA 3-5ml injected -Repeat 2-3 times after moving needle - As needle withdrawn inject 3-5ml LA
question
Is epinephrine added to LA for blocks beneath the elbow?
answer
-No, due to small vessel size of wrist, hand, and fingers circulation would be compromised.
question
Ulnar Block at the Wrist
answer
- Ulnar flexor ID with flexed wrist - Line drawn across forearm at level of styloid process to the ulna - Short B needle perpendicular to skin on radial side - 2-4 ml injected - Additional 2 ml as needle withdrawn -Dorsal branch blocked with 3-5 ml in half ring around ulnar aspect of wrist
question
Median Block at the Wrist
answer
- Long palmar muscle & radial flexor muscle ID - Line across wrist that parralels proximal crease - Short B needle perpendicular to skin, 0.5-1cm - LA 2-5 ml in carpal tunnel -2-3 ml as needle is withdrawn
question
Radial Block at the Wrist
answer
- Subcutaneous ring of LA beginning at radial flexor muscles of the wrist and extending to dorsal surface of the ulnar styloid - Avoid if also using ulnar block, circulation
question
Intravenous Regional Anesthesia: Bier Block
answer
- Simple, safe, rapid anesthesia - Lasts <1hr, used for hands and feet - Tourniquet discomfort, use dual tourniquet to extend procedure to 1½ hours - Risk of large amount of local going systemic - Have emergency equipment available, performed in operating area
question
Upper Extremity Bier Block
answer
- Small bore IV in distal vein - Vein in dorsum of hand preferred - Pt supine and padded extremity - Dual tourniquet preferred - After application on tourniquet arm is exsanguinated by wrapping Esmarch bandage tightly around arm - Alternative raise arm for 5 minutes - After exsangiounation cuff inflated 250mmHg - 50ml of 0.5% lidocaine injected in IV (preservative free no epinephrine) - Monitor for LAST - Add 15-30 mg ketoralac for postop analgesia
question
IV Regional Anesthesia: Lower Extremity Block
answer
- Surgery of short duration on foot - LA volume double that of upper extremity - Tourniquet up to 350-400mmHg 1.5 times wrapped around leg - Two separate 9cm wide cuffs ANKLE - LA injected with distal tourniquet inflated - Cuff below calf, LA 35-45ml of 0.5% lidocaine
question
Intercostal Nerve Block
answer
- High success, low pain, significant analgesia - LAST and pneumothorax risk - Supplement when epidural anesthesia can't be used - Analgesia during chest tube placement, easier for patients in pain to breathe - A 22g, B needle inserted perpendicular to rib and advanced then walked off -3ml increments of LA until desired strength - Tachyphylaxis switch to other class, amide to ester
question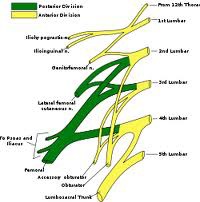
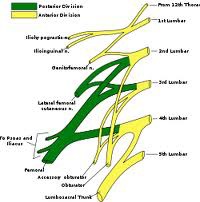
Lumbar Plexus
answer
...
question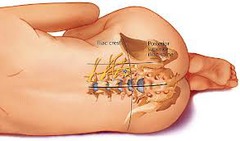
Psoas Compartment Block
answer
- Blockade of lumbar plexus as a unit by injecting LA into psoas compartment - Patient lateral or sitting - Spinous process L4, line caudally, 5cm line perpendicular and laterally to side - Skin wheal, needle perpendicularly advanced until contact with bone at about 5-10cm - Needle withdrawn directed cephalic advanced until slides over L5 - Loss of resistance technique psoas found at 8-12cm - After aspiration 30-40ml LA injected in 5 ml increments
question
Inguinal Perivascular Technique and Femoral Nerve Block
answer
- Three in one block of lower extremity - Supine, groin prepared and draped - Site of injection is 1cm lateral to femoral artery and 1cm inferior to inguinal ligament - 22g 4cm B needle advanced perpendicularly -2 Hz until quadriceps extend then decreased to <0.5 mA - LA 20-30 ml in 3-5ml increments with intermitted aspiration - Digital pressure for 5-10 minutes - Volume of 30 LA increases block of all 3 nerves - Bupivicaine, ropivicaine and levobupivicaine are commonly used
question
Continuous Femoral Nerve Block
answer
-Landmarks femoral artery and femoral crease -Patient supine, practitioner on side to be blocked - Needle insertion site at lateral border of the femoral artery (1cm lateral to the arterial pulse) - 17g 3½ inch needle with nerve stimulator at 1mA, 2Hz 100-300 µsec inserted and advanced at 45-60° angle - Upon quadriceps muscle twitch current reduced to 0.5 mA - If quadriceps twitch not elicited, needle withdrawn and directed more lateral to femoral artery - Initial bolus of 15-20ml is injected slowly after negative aspiration and catheter threaded slowly 5-10cm beyond needle - Continuous infusion of LA at 8-10ml/hr - 0.2% ropivicaine and 0.25% bupivicaine or levobupivicaine - Remove after 48 hours -Apply 2-3 mins pressure if artery or vein punctured
question
Fascia Iliaca Compartment Block
answer
- Anterior lumbar plexus approach with a puncture point distant from the neuromuscular sheath, no nerve stimulator - Widely used for postop analgesia after lower limb surgery - Supine, projection of inguinal ligament drawn on skin from pubic tubercle to anterior superiod iliac spine - Puncture site marked 1cm caudal to the point at which lateral meets middle third of inguinal ligament line - 10% povidone-iodine, short 24g 50mm needle inserted at less than 90° angle to skin -Loss of resistance as needle tip crosses the fascia lata - Advanced until second loss of resistance is felt as the facia iliac - 30ml of LA injected
question
Sciatic Nerve Block
answer
- In combination with lumbar plexus, femoral or saphenous nerve blocks - Largest nerve trunk in the body, supplies muscles of the back of thigh, skin of the leg and muscles of lower leg and foot - Sims position - Line from posterior superior iliac crest to greater trochanter of femur - Third line perpendicular and bisecting first line - Betadine prep and 2-3ml of lidocaine for wheal - 22g 10cm insulated B needle inserted perpendicularly to skin -Advanced until posterior tibial nerve distribution is elicited - 2Hz and 1 mA until plantar flexion response then <0.5 mA - LA injected 10ml in 5ml increment with intermittent aspiration - Repeated at peroneal nerve - Bupivicaine, ropivicaine, chirocaine and lidocaine
question
Popliteal Fossa Block
answer
- Landmarks: popliteal crease, medial border of femoris biceps, tendon of semitendonosus - Line drawn joining medial border of femurs biceps muscle laterally and semitendonosus - From middle of line second perpendicular line 15cm cephalad, insertion 1cm laterally - 10cm insulated needle through skin wheal at 45-60° angle, 1-2cm sciatic nerve -Aspirate and inject 35-40ml LA
question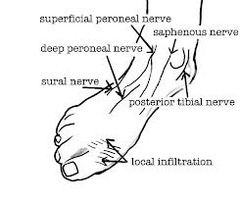
Ankle Anatomy
answer
...
question
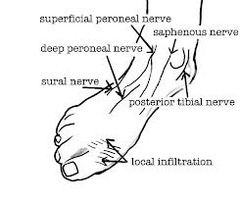
Ankle Block
answer
- Blocks tibial, sural, superficial peroneal and deep peroneal nerves and saphenous nerve - 5 ml of LA injected after direction and redirection of needle
question
Regional Anesthesia and Trauma
answer
- Sympathetic stimulation may mask hypotension - Give fluids - Decompensation can occur after deduction in circulating catecholamines - Prone to nausea -May lose consciousness after regional and require airway support
question
Spinal, epidural and caudal blocks are also known as?
answer
-Neuraxial anesthesia - Each of these blocks can be performed as a single injection or with a catheter to allow intermittent boluses or continuous infusions.
question
Performing a lumbar (subarachnoid) puncture below which level avoids needle trauma to the cord in an adult? Child?
answer
Adult: below L1 Child: below L3
question
What is the principle site of action for neuraxial blockade?
answer
Nerve root
question
What does differential blockade typically result in?
answer
Sympathetic blockade (judged by temperature sensitivity). May be 2 segments higher than the sensory block which is 2 segments higher than the motor blockade.
question
What can produce sympathetic and some parasympathetic blockade?
answer
Interruption of efferent autonomic transmission at the spinal nerve roots.
question
What effects do neuraxial blocks typically have on the CV system?
answer
-Variable decrease in BP - ↓ HR - ↓ cardiac contractility
question
How can you negate deleterious cardiac effects of neuraxial anesthesia?
answer
-10-20ml/kg of IV fluids will partially compensate for venous pooling minimizing the degree of hypotension
question
How should excessive or symptomatic bradycardia be treated? Hypotension?
answer
Bradycardia: atropine Hypotension: vasopressors
question
What are several major contraindications to neuraxial anesthesia?
answer
Patient refusal, bleeding diathesis, severe hypovolemia, elevated ICP, infection at site of injection, severe stenotic valvular heart disease or ventricular outflow obstruction.
question
What indicates you are in the epidural space? Subarachnoid?
answer
Epidural: sudden loss of resistance as needle penetrates ligamenta flavum Spinal: advanced further through the epidural space and penetrates the dura-subarachnoid membranes as signaled by free-flowing CSF
question
Why is epidural anesthesia used, what types of blocks can be performed?
answer
Epidural anesthesia is a neuraxial technique offering a range of applications wider than the typical "all or nothing" spinal. An epidural block can be performed at the lumbar, thoracic or cervical level.
question
What are epidural techniques widely used for?
answer
Operative anesthesia, obstetric analgesia, postoperative pain control, chronic pain management
question
What is the difference in an epidural vs. a spinal onset?
answer
-Epidural anesthesia is slower in onset (10-20mins) and may not be as dense as spinal anesthesia.
question
Which is quicker spinal or epidural? Volume?
answer
Spinal works quickly. Epidural needs test dose, not comfortable until they lay back down. Reason is spinal is direct shot into subarachnoid space, spreads rapidly. Usually 1-2cc, while epidural is 10-15cc.
question
What is the difference in quantity of local anesthetic required for an epidural vs a spinal?
answer
The quantity (volume and concentration) of local anesthetic is very large in an epidural vs a spinal. Significant toxicity can occur if this amount is injected intrathecally or intravascularly. Safe guards against this include the epidural test dose and incremental dosing.
question
What is one of the most commonly used regional techniques in pediatric patients?
answer
- Caudal epidural anesthesia
question
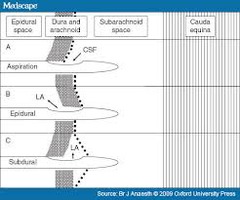
A needle passes through anatomical structures in what order?
answer
-Skin - Supraspinous ligament - Intraspinous ligament - Ligamenta flavum - Epidural space -Dura - Arachnoid membrane ( M&M page 292, figure A)
question
Why doesn't spinal injury due to needle puncture occur below L1 in adults and L3 in children ?
answer
Spinal cord ends at these levels and the nerves travel by caudal equina "horses tail". These nerves are easily pushed aside (rather than punctured) by an advancing needle. The nerves also float in a dura sac.
question
Why does caudal anesthesia carry a greater risk of subarachnoid injection in children than in adults?
answer
- Dural sac extends to S3 in children (S2 in adults) and they are smaller so it is easier to inject in subarachnoid space
question
What is the blood supply to the spinal cord?
answer
- Anterior artery: anterior 2/3 of cord - Posterior artery: posterior 1/3
question
Why does a differential blockade occur?
answer
-Spinal nerves are composed of a variety of fiber types, the smaller are easier to anesthetize. - Concentration of local anesthetic decreases with increasing distance from the level of injection.
question
Sympathetic outflow is? Parasympathetic outflow is?
answer
Sympathetic: thoracolumbar (T5-L1) Parasympathetic: craniosacral
question
What determines vasomotor tone?
answer
Sympathetic fibers arising from T5-L1 which innervate arterial and venous smooth muscle. Block leads to: - vasodilation of venous capacitance vessels - pooling of blood - decreased venous return to the heart - decreased SVR
question
What is the waiting period for anticoagulant medications and neuraxial anesthesia?
answer
- Ticlopidine/ticlid 14 days - Clopidrogel/plavix 7 days - Abciximab/rheopro 48 hours - Eptifibatide/integrillin 8 hours *ASA and NSAIDS with normal coagulation profile safe.
question
How long should herbals be held?
answer
No contraindications but 7 days is preferred, won't delay surgery if they're on herbals. Garlic: 7 days Ginko: 36 hour Ginseng: 24 hours
question
If a patient is receiving heparin for DVT prophylaxis can they undergo neuraxial block?
answer
-Yes, perform 1 hour or more post administration -Remove 1 hour prior of 4 hours after administration
question
Coumadin
answer
4-5 days hold before placement INR <1.2 don't do it One dose of coumadin before surgery is ok (hasn't started working yet)
question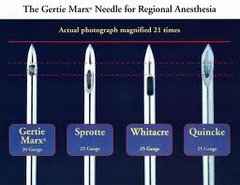
Various Types of Spinal Needle
answer
Cutting: Quincke is most likely to damage spinal cord (calcified lesions) Pencil point: Whitacre and Sprotte *22g pencil point <risk PDPH compared to 25g Quincke
question
In spinal anesthesia two "pops" are felt. What do these "pops" indicate?
answer
- First pop: through ligament flavum -Second pop: through dura-arachnoid membrane
question
How can you make a solution hypobaric or hyperbaric?
answer
Hypobaric: add sterile water Hyperbaric: add glucose
question
Does a parturient patient require more or less anesthetic? Why?
answer
-Less, reduce anesthetic by 1/3 -CSF is decreased due to engorgement of veins
question
What are two commonly used hyperbaric agents?
answer
Bupivicaine and tetracaine Onset: 5-10 mins Duration: 90-120 mins Addition of epinephrine or phenylephrine prolongs tetracaine action but does not work well with bupivicaine.
question
What is the most common type of epidural needle?
answer
-Standard is 17-18g -3 or 3.5 inches -Gentle 15-30° curve at the tip
question
What is a common test dose for epidurals?
answer
- 3 ml of 1.5% lidocaine (45mg) WITH - 3 ml 1:200,000 epinephrine (15µg)
question
Anesthetic Toxicity
answer
Least toxic: chloroprocaine Intermediate: lidocaine, mepivicaine, levobupivicaine, and ropivicaine Most toxic: bupivicaine
question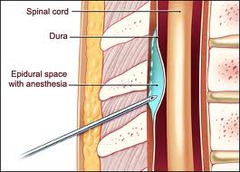
What are the symptoms of an epidural or spinal hematoma?
answer
-Sharp back pain and leg pain - Progression to numbness, motor weakness and sphincter dysfunction
question
What is the timeframe to decompress hematoma from spinal to restore function?
answer
8 hours, anything longer recovery is unlikely.
question
What is the greatest immediate risk of nerve block?
answer
Systemic toxicity caused by inadvertent IV injection. Delayed toxicity can follow the initial injection when rapid or excessive amounts of local anesthetic are absorbed systemically.
question
How is good anesthesia obtained?
answer
Only when local anesthetic is injected in close proximity to the nerve or nerves that are to be blocked.
question
A perineural injection may produce brief accentuation of the parasthesia, what indicates intraneural injection?
answer
Intraneural injection produces an intense searing pain and indicates the injection should immediately be terminated and the needle repositioned.
question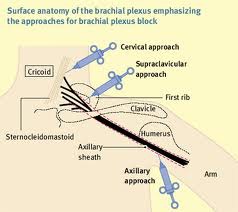
How can surgical anesthesia of the shoulder and upper extremity be obtained?
answer
Neural blockade of the brachial plexus (C5-T1) or its terminal branches at several sites.
question
Which approach is most optimal for procedures on the shoulder, arm and forearm?

answer
Interscalene approach, produces a block that is most intense at the C5-C7 dermatomes and least intense in the C8-T1 dermatomes.
question
Which approach is optimal for procedures from the elbow to the hand?

answer
Axillary approach to the brachial plexus, produces the most intense nerve block in the distribution of the C7-T1 (ulnar nerve)
question
Which type of block provides good homogenous anesthesia to the brachial plexus, can be used for procedures involving the hand, forearm, elbow and upper arm and are conducive to indwelling catheter placement for postoperative analgesia?
answer
Infraclavicular blocks
question
Which type of block produces intense surgical anesthesia for short surgical procedures (45-60minutes) in the forearm, hand and leg?

answer
Intravenous regional anesthesia AKA Bier block
question
Which type of block is useful in numerous procedures involving the thigh and knee, or as an adjunct to procedures distal to the knee that require anesthesia to the medial aspect of the lower leg (saphenous distribution)?
answer
Femoral nerve block
question
Which block does not require a nerve stimulator, is performed quickly, is not very stimulating and patients do not often require sedation?

answer
Fascia iliaca blocks
question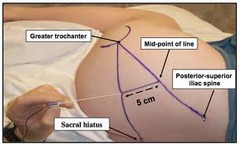
Blockade of which nerve provides anesthesia for many surgical procedures involving the hip, knee, or distal lower extremity?
answer
Sciatic which may be blocked at numerous sites along its course.
question
Which block is useful for foot and ankle surgery and can result in complete anesthesia of the limb distal to the knee if a separate saphenous nerve block (terminal nerve of the femoral nerve) is also included?
answer
Popliteal block
question
Which block is being increasingly used to provide postoperative analgesia following mastectomy, inguinal hernia repair, and several procedures involving the chest and body wall?

answer
Paravertebral block
question
From superior to inferior what is the order of anatomical structures?
answer
VAN: vein, artery, nerve
question
From lateral to medial what is the order of anatomical structures?
answer
NAVEL: nerve, artery, vein, empty space, lymphatics
question
What causes hydrostatic (ischemic) injury to nerve fibers?
answer
- Injection that is intraneural, within the nerve substance, generates high pressures and cause hydrostatic (ischemic) injury to nerve fibers.
question
When blocking the upper extremity which two nerves muct be blocked separately to prevent pain from tourniquet?
answer
-medial brachial cutaneous - intercostobrachial
question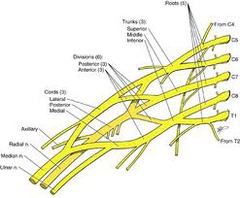
Brachial Plexus Anatomy
answer
...
question
What are some complications of inter scalene blocks?
answer
- Incidental blockade of phrenic nerve leading to respiratory failure. - Horner's syndrome: miosis, ptosis, anhidrosis, dyspnea, hoarseness - Even a small amount (1-3ml) of LA injected into the vertebral artery goes straight to the brain and causes seizures. - Advancing the needle too far can lead to puncture of the pleura and pneumothorax.
question
In the axilla where is the musculocutaneous nerve?
answer
The musculocutaneous nerve has already left the sheath and lies within the coracobrachialis muscle. This is why this nerve must be blocked separately.
question
What is the "pull-push-pin-pin" technique to assess quality of
answer
Pull: flex the arm (checks musculocutaneous nerve) Push: arm against resistance (radial nerve) Pin: prominence (median nerve) Pin: fifth digit (ulnar nerve)
question
When a procedure involves use of a pneumatic tourniquet which two nerves must be blocked proximal to the axilla?
answer
Intercostobrachial Medial Brachial
question
The lumbar plexus is innervated from which vertebrae?
answer
Ventral rami of L1-T4 (with some contribution from T12)
question
The lumbar plexus (primarily L2-L4) forms which three nerves that innervate the lower extremity?
answer
- Femoral cutaneous - Femoral -Obturator Lie within the substance of the psoas muscle and emerge within a common fascial sheath that extends proximal to thigh. The common peroneal and tibial nerves arise from the sciatic nerve in the lower leg.
question
How is the deep peroneal nerve blocked for an ankle block?
answer
The deep peroneal nerve is blocked by identifying the groove formed proximally by the extensor halluicus longs tendon and the extensor digitorum longs tendons.
question
Intercostal blocks are rarely used as sole anesthesia techniques, when are they used?
answer
To supplement general anesthesia, for postoperative analgesia following thoracic and upper abdominal surgery, and for relief of pain associated with rib fractures, herpes zoster, and cancer.
question
Which block results in the highest blood levels of local anesthetic in the body (per volume)?
answer
Intercostal blocks



