Review Labs & Pharmacology – Flashcards
Unlock all answers in this set
Unlock answersquestion
Purpose of laboratory and diagnostic tests
answer
- Screening - Diagnosis - Monitoring
question
Nurses role in laboratory and diagnostic tests
answer
In addition to ordering laboratory tests, nursing input is extremely critical to ascertain valid and reliable laboratory test results. The nurse must communicate with the client, physician, and laboratory personnel to obtain information that might affect test results. Responsibilities include explaining the laboratory test, ensuring that both the client and staff follow the procedure, assessing clinical findings with laboratory test results, noting pertinent information on the laboratory requisition slip (e.g., drugs the client is taking that might affect test results), and collecting the specimen.
question
Lab results
answer
• Dependent on facility/lab book • Normal range (reference range) • Baseline (before treatments) • Trends
question
Anticoagulant
answer
Preventing or delaying blood clots by reducing the formation of fibrin.
question
Anticoagulation
answer
• Blood clots can develop in many patients - Short and long-term immobilized patients - Cardiac conditions • Those at risk of developing clots are given anticoagulation to prevent clots - Aspirin - Heparin - Low molecular weight heparin - Warfarin (Coumadin) • Blood tests are used to measure the effectiveness of some of these anticoagulants
question
Aspirin
answer
Classification: Antiplatelet drug (also: antipyretic, nonopiod analgesic) Actions: suppresses platelet aggregation & vasoconstriction by irreversibly inhibiting cyclooxygenase (enzyme required by platelets to make thromboxane A2 (TXA2 promotes platelet activation & promotes vasoconstriction)); it also inhibits synthesis of prostacyclin by the blood vessel wall (prostacyclin suppresses platelet aggregation & promotes vasodilation = the opposite effects of TXA2); in order to maintain balance/to not offset beneficial effects of aspirin, need to keep dosage low (325mg/day or less)- this helps to maintain TXA2 inhibition & minimizes effect of inhibition of prostacyclin production Uses: prevention of thrombosis in arteries (also: for inflammatory disorders, mild to moderate pain, fever, prophylaxis of TIA & MI) Side Effects: increases risk of GI bleeding, hemorragic stroke Major Nursing Implications: *Monitor for hypersensitivity reactions (increased risk in patients with: asthma, allergies, nasal polyps, or if allergic to tartrazine) *assess for rash periodically (discontinue treatment if severe rash or if rash PLUS: fever, fatigue, general malaise, muscle/joint aches, blisters, oral lesions, conjunctivitis, hapatitis and/or eosinophilia) *consider lab tests to monitor hepatic function
question
Heparin
answer
- IV/SQ - Inexpensive Classification: antithrombotics Action: activates antithrombin which inactivates thrombin and factor Xa, ultimately suppressing the synthesis of fibrin. Fibrin forms the framework of thrombi in veins, so Herparin is especially useful for prophylaxis of venous thrombosis. Rapid acting ( w/in minutes). Highly polar and can not cross membranes, must be administered by injection, IV or Subq. Uses: Used during pregnancy b/c does not cross placenta. Emergencies (due to rapid onset) such as, pulmonary embolism, deep vein thrombosis (DVT), evolving stroke. Open heart surgery and renal dialysis, to prevent coagulation in devises (heart-lung machine, dialyzers). Low-dose used to prevent postoperative venous thrombosis. Disseminated intravascular coagulation. Side Effects: Hemorrhage. Spinal/Epidural Hematoma, leading to permanent paralysis. Anemia. Drug-indused hepatitis.. Hypersensitvity reactions (allergy). Major NSG Implications: * monitor for bleeding (if occurs, notify HC provider) * administration by IM injection causes hematoma and must not be done. * monitor platelet count every 2-3 days.
question
Warfarin (Coumadin & Jantoven brand names)
answer
*high alert medication - PO, IV, Inexpensive Classification: Therapeutic anticoagulant Action: anticoagulants decrease formation of firbin. supressed coagulation by decreasing production of 4 clotting factors VII, IX, X and prothrombin (all al vitamin K dependent clotting factors) Uses: prevent thrombosis in beins and the artria of the heart. in therapeutic uses warfarin reduces production of vitamin K dependent clotting factors by 30-50% Pharmacokinetics: readily absorbed after oral dosing and 99% binds to albumin, inactivated in the liver and excreted in urine and feces. Even though warfarin readily absorbs it does not have an effect on clotting factors already in circulation therefore warfarin remains ineffective until those clotting factors have decayed. Side Effects: Hemorrahage, excessive bleeding, GI ulcers Major Nsg Impications: *monitor PT and INR carefully *patients should continue with normal vitamin K intake in foods and should not avoid them, dosage of warfarin will be adjusted according to dietary intake of vitamin K.
question
Low molecular weight heparin
answer
Heparin preparations that are composed of molecules that are shorter than those found in unfractionated heparin. As effective as unfractionated heparin but easier to use. Can be given in fixed-dosage and do not require lab monitoring, allowing home use.
question
Other anticoagulant drugs
answer
• Low molecular weight heparins - Lovenox (enoxaparin) - Fragmin (dalteparin) - Innohep (tinzaparin) - SQ • New meds - Atrial fibrillation (AF) only - Pradaxa (dabigatran etexilate) - Xarelto (rivaroxaban) - AF and DVT - Elizuis (apixaban) - Expensive $$$$
question
Lovenox (enoxaparin)
answer
US hospitals spend more money on Lovenox than any other drug! Classification: Antithrombotics Action: Activation of antithrombin, resulting in preferential inactivation of factor Xa, and some inactivation of thrombin, SYNTHESIS of fibrin is reduced, leading to suppressed clotting. Uses: prevention of DVT after knee or hip replacement or abdominal surgery in pt considered high risk for thromboembolic complications (obese, over 40yrs, history of DVT or pulmonary embolism). Preventing ischemic complication in pt w/unstable angina, non-Q wave MI, or STEMI. Major NSG Implications: * assess for signs of bleeding * monitor for hypersensitivity * assess for increased thrombosis * monitor of signs of neurolgic impairment in pt undergoing spinal puncture, or epidural anesthesia.
question
Fragmin (dalteparin)
answer
Classification: Antithrombotics Action: Activation of antithrombin, resulting in preferential inactivation of factor Xa, and some inactivation of thrombin, SYNTHESIS of fibrin is reduced, leading to suppressed clotting. Uses: prevention of DVT after knee or hip replacement or abdominal surgery in pt considered high risk for thromboembolic complications (obese, over 40yrs, history of DVT or pulmonary embolism). Preventing ischemic complication in pt w/unstable angina, non-Q wave MI, and management of symptomatic venous thromboembolism (VTE). Major NSG Implications: * assess for signs of bleeding * monitor for hypersensitivity * assess for increased thrombosis * monitor of signs of neurolgic impairment in pt undergoing spinal puncture, or epidural anesthesia.
question
Thrombin inhibitors
answer
These anticoagulants work by direct inhibition of thrombin. Hence they differ from heparin-like anticoagulants, which inhibit thrombin indirectly (by enhancing the activity of antithrombin.)
question
Pradaxa (dabigatran etexilate)
answer
Classification:Therapeutic: Anticoagulants Pharmacologic: thrombin inhibitors Action: Acts as a direct inhibitor of thrombin Uses: Atrial Fibrillation-Approved for use in patients with non-valvular atrial Fibrillation. Pharmacokinetics: Absorption: 3-7% absorbed following oral administration. Distribution: Unknown Metabolism and Excretion: Of the amount absorbed, mostly excreted by kidneys (80%); 86% of ingested dose is eliminated in feces due to poor bioavailability. Food delays absorption, but does not reduce the extent of absorption. Half Life:13-17 hours Side Effects: GI: abdominal pain, diarrhea, dyspepsia, gastritis, nausea. Hemat: Bleeding, thrombocytopenia. Misc.: Angioedema, hypersensitivity reactions including anaphylaxis. Major Nsg Implications: * Assess for symptoms of stroke or peripheral vascular disease periodically during therapy. * Assess for symptoms of bleeding and blood loss; may be fatal. * Lab Test Considerations: Use a PTT or ECT, not INR, to assess anticoagulant activity, if needed. * Monitor renal function prior to and periodically during therapy. Patients with renal impairment may require dose reduction or discontinuation. * For surgery, discontinue dabigatran 1-5 days before invasive or surgical procedures; consider longer times for major surgery. Administered by mouth (PO)
question
Xarelto (rivaroxaban)
answer
Classification: therapeutic: anti coagulant pharmacologic: antithrombotics, factor Xa inhibitors Indications: prevention of DVT that may lead to pulmonary embolism following hip or knee replacement surgery Action: selective factor X inhibitor that blocks the active site of factor Xa, inactivating the cascade of coagulation Pharmacokinetics: Well absorbed (80%) following oral administration; absorption occurs in the stomach and decreases as it enters the sm intestine. (Note: healthy Japanese have blood levels that are 50% higher than other groups). Distribution is unknown. 51% is metabolized by the liver, 36% excreted unchanged in the urine. Metabolites do not have anticoagulant activity. Half-life: 5-9 hrs Route: PO Onset: unknown Peak: 2-4 hrs Duration: 24 hrs Contraindications: hypersensitivity, active major bleeding, severe renal impairment, moderate to severe hepatic impairment or any liver pathology resulting in altered coagulation, lactation--avoid breast feeding Adverse reactions: syncope, blister, pruritis, BLEEDING, wound secretion, extremity pain, muscle spasm Nrs implications: *Assess for signs of BLEEDING and HEMORRHAGE (bleeding gums, nosebleed, unusual bruising, tarry stools, hematuria, fall in Hct or BP, bleeding from surgical site). Notify health professional *Monitor pt w epidural catheters freq for S/Sx of neurologic impairment. Do not remove catheter earlier than 18 hrs after last dose of Xarelto, and next dose after removal shoudl be >6 hrs
question
Anticoagulant antidotes: Heparin
answer
- Stop heparin - Protamine sulfate
question
Anticoagulant antidotes: Low molecular weight heparins
answer
- Stop med - Protamine sulfate
question
Anticoagulant antidotes: Pradaxa, Xarelto, Eliquis
answer
- None
question
Anticoagulant antidotes: Warfarin
answer
- Skip med - Vitamin K - phytonadione (AquaMEPHYTON)
question
Anticoagulant testing: Heparin
answer
- PTT/APTT (Thromboplastin time/Activated partial thromboplastin time )
question
Anticoagulant testing: Low molecular weight heparins
answer
- No testing
question
Anticoagulant testing: Pradaxa, Xarelto, Eliquis
answer
- No testing
question
Anticoagulant testing: Warfarin
answer
- PT/INR (Protime/International Normalized Ratio)
question
Prothrombin time (PT)
answer
• Used to monitor oral anticoagulation therapy (warfarin) in patients at risk for a clot. - Too little warfarin can lead to a clot - Too much warfarin can lead to bleeding - internally and externally A ocagulation test that is especially sensitive to alterations in vitamin K-dependent factors. The average pretreatment value for PT is 12 seconds. Treatment with warfarin prolongs PT. • Protime differs from facility to facility
question
International normalized ratio (INR)
answer
• Used to monitor oral anticoagulation therapy (warfarin) in patients at risk for a clot. - Too little warfarin can lead to a clot - Too much warfarin can lead to bleeding - internally and externally To ensure that test results from different laboratories are comparable,results are now reported in terms of the INR - Standardized system for communicating and interpreting the PT results - Used to determine if warfarin blood level is at a therapeutic level - not too high (bleeding), not too low (clot)
question
Protime/INR (PT/INR)
answer
• Patients with an INR in the desired range will be - At less risk of developing a clot - At higher risk of bleeding - Desired range is somewhere between 2.0-4.0, depending on the patient's condition • INR 5 - bleeding likely
question
Baseline INR
answer
• Lab results before patient is started on anticoagulation • Should be ≈ 1.0 (0.8-1.2 at NWH) • INR higher than 1.0 may mean liver problems
question
Normal Range for INR
answer
• INR value without anticoagulation • INR higher than ≈ 1.0-1.2 is called elevated.
question
Therapeutic Range
answer
• For the patient taking warfarin, - The therapeutic range for INR is a level where o The patient's risk of developing a clot is lowered. o The risk of bleeding is higher, but not to the point of active bleeding. • For warfarin to be therapeutic (not cause clots and also not cause bleeding), the INR is usually between 2-4, depending on why the patient is taking warfarin. • An INR less than 2 means that while the patient is taking warfarin, they may not be taking enough to significantly lower the risk of clot formation. • An INR above 4-5 means the patient is taking too much warfarin.
question
PT/INR Lab Results
answer
• These are the preferred values for patients taking oral anticoagulation (warfarin) • Patient who has or is at risk of developing Deep vein thrombosis (DVT) or Pulmonary Embolism (PE) - INR 2.0 - 4.0 • Examples - Patient who is immobile Ex: hip fracture o INR 2.0 - 3.0 - Patient with Atrial fibrillation (AF) o INR 2.0 - 3.0 - Patient with a Mechanical Heart Valve o INR 2.5 - 3.5
question
Interventions for heparin
answer
• Nursing interventions - Monitor for any bleeding - Monitor for/teach about signs of a blood clot - Patient teaching • Electric razor instead of a blade • Food and drug interactions • Follow prescribed testing schedule • Collaborative interventions - Notify PCP of abnormal test results - Administer warfarin/Vitamin K
question
Blood
answer
• 6%-8% of total body weight • Functions - Transport - Waste removal - Body regulation
question
Plasma
answer
Fluid portion of blood. About 55% of blood volume.
question
CBC-Complete Blood Count
answer
• Composed of - White blood cell count - Red blood cell count - Hemoglobin - Hematocrit - Red blood cell indices - Blood smear - Platelet count • Done for diagnostic testing
question
Red blood cell (RBC)
answer
A cellular component of blood involved in the transport of oxygen and carbon dioxide (synonym: erythrocyte)
question
RBC count (Erythrocyte)
answer
• Adult / elderly - 4.0-6.0 x 106 microL (Average) • Higher in male than in female • Lab/lab book specific • Lifespan - 120 days • Decreased Level - Blood loss - Anemia - Over hydration • Elevated Level - Dehydration - High altitude - COPD/Cardiovascular disease
question
Hemoglobin
answer
• Main component of RBCs - Carries O2/CO2 • Adult Male: 13.5 - 17 g/dL • Adult Female: 12 - 15 g/dL • Critical: 20 g/dL
question
Hematocrit
answer
• Volume of packed RBCs - Adult male: 40 - 54% - Adult female: 36 - 46% • Elderly: Slightly decreased normals • Critical: 60% • May be indicator of hydration status of patient
question
RBC Indices
answer
• Related to Anemia • Calculated values • Provide information about RBCs - Size - Weight - Hemoglobin concentration • Used to help categorize anemia • Listed as - MCV - MCH - MCHC - RDW
question
Interventions - Low Hct, Hgb, RBCs
answer
• Nursing interventions - Health teaching o Diet - Foods rich in iron - Safety issues o Postural BP o Position changes o Monitor for fatigue, weakness o Monitor for bleeding • Collaborative interventions - Monitor labs - Transfusion - Give medications o Iron o B12 / Folate
question
Platelets
answer
• Smallest element in blood • No nucleus • Needed for blood clotting, vascular integrity, vasoconstriction • Lifespan - 7-9 days • Normal - 150,000-400,000/ mm3 • Critical; 1,000,000/mm3 • Aspirin (ASA)
question
Interventions for low platelet count
answer
• Nursing interventions - Monitor o Bleeding, bruising - Safety o Avoid bumping • Collaborative interventions - Consult with MD about aspirin usage - Monitor labs - Administer platelets
question
White Blood Cells (Leukocytes)
answer
• Major function of WBCs - fight infection, react against foreign bodies • WBC count - total number of leukocytes in 1 mm3 blood • Decreased WBCs - Leucopenia • Increased WBCs - Leukocytosis
question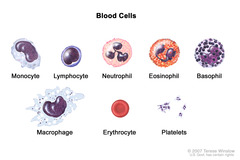
WBCs
answer
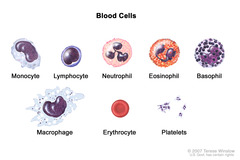
• Five types of WBCs - Divided into groups Granulocytes • Neutrophils - PMNs, polys, segs • Basophils (mast cells) • Eosinophils Nongranulocytes • Lymphocytes • Monocytes • Differential count ("diff") • Percentage of each type of white blood cell in 1 mm^3 blood
question
WBC count - Normal findings
answer
- Adult • 4500-10,000 /mm^3 - Child (Newborn) • 9000-30,000 /mm^3 - Child (2-10 years) • 6000-17,000 /mm^3 - Child > 10 • 4500-13,500 /mm^3 - Critical • 30,000/mm^3
question
Differential count
answer
Test that enumerates the distribution of WBC's in a stained blood smear by counting the different kinds of WBC's and reporting each as a percentage of the total examined
question
Differential count WBCs
answer
• Neutrophils - 50-70%, 2500-7000 /mm^3 • Lymphocytes - 25-35%, 1700-3500 /mm^3 • Monocytes - 4-6%, 200-600 /mm^3 • Eosinophils - 1-3%, 100-300 /mm^3 • Basophils - 0.4-1%, 40-100 /mm^3
question
"Left Shift"
answer
• Neutrophils have life span of 7-14 days • Remain in circulation 6 hours • Acute bacterial infection and trauma stimulate production • When body runs out of mature cells to fight an infection, immature cells begin to be released into the blood • It is called a "left shift" when the mature neutrophils have been used up and the body is using immature cells to fight infection. • These immature cells do not have the same capabilities as the mature neutrophils.
question
Interventions - High WBC
answer
- Nursing interventions o VS o Monitor for improvement/relapse - Collaborative interventions o Give antibiotics o Check labs
question
Interventions - Low WBC
answer
- Nursing interventions o Protect patient o Neutropenic precautions - Collaborative interventions o Give meds o Check labs o Assist with bone marrow biopsy
question
Urinalysis
answer
• Diagnosing - Urinary tract infection (UTI) - Renal disease • Detecting metabolic disease not related to kidneys - Diabetes mellitus • Routine - Routine UA has two components: • Macroscopic analysis • Microscopic analysis
question
Urinalysis-Selected Normal findings
answer
• Appearance: clear • Color: light straw to dark amber • Odor: aromatic • pH: 4.5 - 8 • Protein: 2-8 mg/dL • Specific gravity - Adult: 1.005 - 1.030 • Leukocyte esterase: negative • Nitrites: negative • Glucose: negative Under Low-power Field • WBCs: 0 - 4 per • RBCs: ≤ 2 • Bacteria: negative - (< 1,000 bacteria /mL)
question
Culture & Sensitivity Urinalysis
answer
• Culture - Growing any bacteria found in the urine or other sites in the body • Sensitivity - Measures bacteria's strength • UA, C& S • UA, C & S if indicated
question
Interventions for abnormal urinalysis
answer
• Nursing interventions - Obtain a history of medications patient currently taking - Assess fluid status of patient • Collaborative interventions - Give antibiotics - Obtain urine specimen o Clean catch specimen o Catheter specimen o Urine specimen should be taken to lab within 30 minutes or refrigerated
question
Total protein, albumin, prealbumin
answer
• Total protein • Albumin largest - Nutritional status - AKA - Thyroxine-binding prealbumin, thyretin, transthyretin
question
Total Protein normal range
answer
- 6.0-8.0 g/dL
question
Albumin normal range
answer
- 3.5-5 g/dL
question
Prealbumin normal range
answer
- 17-40 mg/dL
question
Interventions abnormal protein, albumin, prealbumin levels
answer
• Nursing interventions - Assessment - Health teaching • Collaborative interventions - Give meds - Monitor labs - Dietary consult
question
Types of point of care testing
answer
• Blood glucose monitoring • Occult blood (Feces) • Guaiac • Urinalysis • Pulse oximetry • PT/INR, PTT



