Neurology (Stroke & TIA) – Flashcards
Unlock all answers in this set
Unlock answersquestion
When an artery to the brain becomes blocked or ruptures, resulting in death of an area of brain tissue (cerebral infarction) and causing sudden symptoms.
answer
When does a stroke occur?
question
1) Bleeding - Hemorrhage 2) Lack of blood flow - Thrombotic - Embolic
answer
What are the two mechanisms of action for a stroke?
question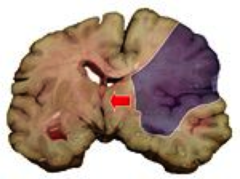
1.) Cells loose blood supply 2.) Aerobic metabolism stops 3.) Cells die 4.) Dead cells swell 5.) The amount of swelling depends on the volume of dead tissue 6.) Enlarging tissue increases the Intercranial pressure 7.) Blood flow decreases to the head - Remember what drives blood flow? 8.) Increased ICP (intercranial pressure) decreases blood flow which makes cerebral perfusion worse 9.) The area around an infarct becomes progressively hypoxic causing more swelling 10.) More swelling causes worse blood flow 11.) Eventually the brain becomes too big to stay in the cranium 12.) HERNIATION occurs (Next card, wait for it.....)
answer
Why does death occur as a result of a stroke?
question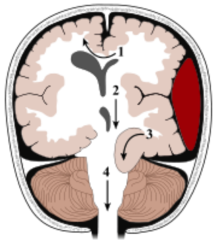
#1) Midline shift #2) Downward displacement of the cranium #3) Uncus and hippocampus herniate into the tentorial notch #4) Cerebellar tonsils herniate through the foramen magnum = DEATH
answer
What is herniation?
question
80% Ischemic Stokes : 20% Hemorrhagic
answer
Which occurs most, ischemic or hemorrhagic stroke?
question
STROKE!
answer
What is the most common disabling neurologic disorder?
question
Arterial Hypertension!!!! (Systolic and diastolic BP are independent risk factors)
answer
What is the most IMPORTANT risk factor for stroke?
question
1) A. Fib 2) Smoking 3) Lipids 4) Diabetes 5) Previous TIA 6) 1/3 will have a full stroke in 5 years Age
answer
What are some other risk factors for stroke?
question
1) Migraine 2) Seizures 3) Syncope 4) Transient global amnesia 5) Peripheral nerve disorders 6) Intracranial hemorrhage 7) Intracranial masses 8) Neuroses (panic, anxiety) 9) Metabolic disorders
answer
What are the diagnoses that may mimic stroke (AKA the differential diagnosis)
question
Thrombotic strokes
answer
This is described as when a thrombus formation in an artery causes decreased perfusion downstream and subsequent cell death
question
***Large vessel disease (inside & outside the head)*** 1) Circle of Willis 2) Carotids 3) Vertebral blood vessels
answer
What large vessels are affected in ischemic stroke??
question
1) Atherosclerosis 2) Vasoconstriction 3) Arterial Dissection
answer
What are the causes of large vessel disease?
question
Lacunar Infarcts
answer
What is another name for Small Vessel Disease ?
question
****Small (.5-1.5 mm) arteries from**** 2) Distal vertebral artery 3) Basilar artery 4) Middle cerebral artery stem
answer
What arteries are affected in small vessel disease?
question
1) Lipohyalinosis 2) Atheroma formation (when cholesterol and fatty sub. that is carried in the blood accumulates on the inside lining of the arteries and form a yellow deposits)
answer
What are the causes of small vessel disease?
question
1) Silent at first 2) AKA Lacunar infarcts 3) Step-wise progression 4) Slowly accumulates deficits - Pure motor hemiplegia - Dysarthria - Ataxic hemiparesis - Dementia (recall: multi-infarct dementia)
answer
What are the clinical features of small vessel disease?
question
Ischemic Strokes
answer
This is described as is death of an area of brain tissue (cerebral infarction) resulting from an inadequate supply of blood and oxygen to the brain due to blockage of an artery.
question
1) A particle from elsewhere that lands in the brain 2) Variable clinical picture
answer
What is an emboli?
question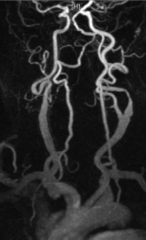
1) Cardiac - Atrial fibrillation - Valvular Disease (endocarditis) 2) Carotid - Atheroma 3) Aortic atheroma 4) Unknown
answer
What are the sources of an embolus that causes a stroke?
question
Anoxic Brain injury
answer
What is another name for hypoperfusion?
question
1) Sepsis 2) Shock 3) Bleeding
answer
What does decreased oxygen supply in hypoperfusion (Anoxic Brain injury) cause?
question
Hemorrhagic stroke
answer
This is caused by include bleeding within the brain (intracerebral hemorrhage) and bleeding between the inner and outer layers of the tissue covering the brain (subarachnoid hemorrhage).
question
When blood vessels of the brain are weak, abnormal, or under unusual pressure, a hemorrhagic stroke can occur. In hemorrhagic strokes, bleeding may occur within the brain, as an intracerebral hemorrhage. Or bleeding may occur between the inner and middle layer of tissue covering the brain (in the subarachnoid space), as a subarachnoid hemorrhage
answer
OK so how does bleeding cause a hemorrhagic stroke?
question
1) Hypertension 2) Trauma 3) Illicit drug use (cocaine and/or methamph.)
answer
What are the causes of intercerbral hemorrhage?
question
1) Confined to the tissues that contain bleeding 2) Evolve over minutes-hours 3) Do NOT BEGIN ABRUPTLY 4) ARE NOT MAXIMAL AT ONSET 5) Symptoms are progressive
answer
What are the symptoms of an intercerabral hemorrhage?
question
1) Vomiting 2) Decreased level of consciousness
answer
What are the signs and symptoms of an intercerbral hemorrhage that has caused an elevated intracranial pressure (ICP)?
question
Arteriole-Venous Malformations (AVM)
answer
This is defined as: 1) Congenital Arterial-Venous connections w/o a capillary bed in-between 2) High flow of blood 3) Not completely normal blood vessels
question
A bulge (dilation) in the wall of an artery, usually the aorta.
answer
What is an Aneurysm?
question
Berry Anuerysm
answer
This is a small aneurysm at the base of the brain in the Circle of Willis
question
1) very common in elderly 2) rupture can be life threatening 3) 35% fatality on 1st hemorrhage 4) Sudden, severe headache followed by coma 5) **Associated with polycystic kidney disease**
answer
Describe a Berry Anuerysm
question
Rupture usually comes from increased intracranial pressure - Valsalva/coughing/sneezing **Note** Bleeding is white
answer
What usually causes a rupture of an aneurysm?
question
1) Blood is NOXIOUS to the Brain 2) Blood spreads throughout the CNS 3) Causes elevated ICP -->Coma-->Death
answer
What happens when there is Arterial bleeding into the CSF?
question
Cerebral hemorrhage
answer
This is hemorrhage within the brain substance
question
Subarachnoid hemorrhage
answer
This is bleeding into subarachnoid space, causing elevated intracranial pressure, vasospasm, and toxic effects.
question
Subdural or epidural hemorrhage
answer
This produces mass lesion that can compress the underlying brain.
question
1) Bleeding typically short - Arterial spasm common - Rebleeding very common o And fatal 2) Clot formation causes vasospasm 3) Distal hypoperfusion - Results in Ischemic damage
answer
Describe what happens during an aneurysm
question
Abrupt onset v. gradual 1) Severe--> Subarachnoid hemorrhage (SAH) 2) Headache--> (97% of cases of SAH) 3) "Worst headache of my life"--> SAH 4) Vomiting 5) Consciousness - Initially brief w/ Lucid interval to follow 6) Neck Stiffness 7) Aseptic Meningitis
answer
What are the symptoms of a stroke?
question
SUBARACHNOID HEMORRHAGE
answer
This is bleeding into the space (subarachnoid space) between the inner layer (pia mater) and middle layer (arachnoid mater) of the tissue covering the brain (meninges).
question
Rupture of a bulge (aneurysm) in an artery
answer
What is the most common cause of subarachnoid hemorrhage?
question
Because a Subarachnoid hemorrhage can occur as a result of trauma as well
answer
Why is a Subarachnoid hemorrhage is considered a stroke ONLY when it occurs spontaneously
question
1) Sentinal bleeds (Warning bleed) 2) TIA
answer
What are the "warning shots" of a stroke?
question
1) Sudden and severe headache 2) Typically 6-20 days before "THE BIG ONE"
answer
Describe the onset of a Sentinal bleeds (Warning bleed)
question
1) Brief episode of neurological dysfunction 2) Resulting from decreased perfusion 3) Impeding stroke!!! 4) Symptoms resolve in less than an hour
answer
What is a TIA (transient ischemic attack)?
question
1) Identifiy the cause of neurologic deficit - IF NOT stroke, then what? Can it be treated - Said another way, not all neurologic deficits are from stroke! 2) Plan an immediate plan of action - Candidate for lytics? Anticoagulation? 3) Long term management Can we prevent future strokes?

answer
What are the three goals of managing a stroke?
question
1) Asymmetric facial paresis 2) Arm drift/weakness 3) Abnormal speech (dysarthria) **Note** Ischemia is dark (black)

answer
What are the three most predictive examination findings for acute stroke (Ischemic)?
question
Noncontrast CT
answer
What is the mot important diagnostic test for a stroke?
question
Looks dark - may be normal in first 24 hours
answer
How does Ischemic stroke look on non-contrast CT?
question
Looks bright/white - should show up earlier
answer
How does hemorrhagic stroke look on a non-contrast CT?
question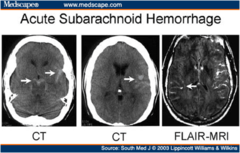
acute hemorrhage appears bright on CT scan, whether in the brain itself, or outside the brain parenchyma (subarachnoid, subdural hemorrhage).
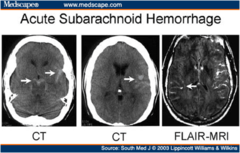
answer
How does a acute subarachnoid hemorrhage appear on Non-Contrast CT?
question
Sensitivity: 89%; specificity: 100%
answer
What is the sensitivity/ specificity of a non-contrast CT in diagnosing a Subarachnoid hemorrhage?
question
MRI
answer
What is much better than CT for detecting brainstem and cerebellar strokes?
question
True
answer
T or F. Acute infarction is seen sooner with MRI than CT
question
1) Elevated BP that cannot be controlled 2) Bleeding disorder 3) Stroke or head trauma in the prior 3 months 4) Prior history of intracranial hemorrhage 5) Major surgery in the past 14 days 6) GI or GU bleeding in the previous 21 days 7) MI in the prior 3 months 8) LP within the past 7 days 9) Evidence of hemorrhage on head CT 10) Symptoms suggestive of SAH, even if CT is normal 11) Pregnancy or lactation 12) Active bleeding or acute trauma/fracture
answer
What are the contraindications to using thrombolysis?
question
BLEEDING!! DO NOT PUSH LYTICS IN THE DARK
answer
What is the Big complication of pushing throbolytics?
question
Aspirin, after exclusion of hemorrhage on CT.
answer
If a stroke patient is not a candidate for thrombolytics, what shoule be prescribed?
question
220mgHg and/or DBP over 120mmHg
answer
Most guidelines recommend that BP NOT be treated acutely in the patient with ISCHEMIC stroke unless SBP over
question
220/120
answer
I say again, what is the threshold in ISCHEMIC stroke?
question
- Ischemic stroke causes decreased blood flow distal to obstruction, with blood flow in the distal blood vessels dependent upon systemic BP - Elevated BP may be a chronic condition or may be a response to decreased cerebral perfusion
answer
Why should I be permissive with the Blood pressure in ISCEHMIC stroke?
question
Labetolol (Beta Blocker) Works by relaxing blood vessels and slowing heart rate to improve blood flow and decrease blood pressure.
answer
If by chance the BP gets over 220/120, what should be prescribed?
question
Keep SBP between 140-160mmHg and monitor for signs of cerebral hypoperfusion induced by fall in BP
answer
OK. BP control in HEMORRHAGIC stroke is handled a little differently. What should I keep the BP at in a Intracerebral hemorrhage or a subarachnoid hemorrhage?
question
1) IV nitroprusside (Nitropress) - A vasodilator that works by relaxing the muscles in your blood vessels to help them dilate (widen). This lowers blood pressure and allows blood to flow more easily through your veins and arteries. 2) Nicardipineis (Cardene) - used to treat high blood pressure. It relaxes your blood vessels so your heart does not have to pump as hard. It also increases the supply of blood and oxygen to the heart to control chest pain (angina). 3) Labetalol
answer
What should be prescribed if a patient with a Intracerebral hemorrhage or a subarachnoid hemorrhage has a Systolic BP over 160?
question
Labetalol (Because a patient will get increased blood flow with nitroprusside vasodilation)
answer
What is the DOC in a patient with a subarachnoid hemorrhage and why?
question
***Liberal use of antipyretics*** - Decreased stress - Watch for worsening disease - Think edema--> Increased ICP o Neuro checks q2 hrs o Vitals q2 hrs
answer
Manage the Temperature! But how?
question
1) Keep head of bed elevated 2) Consider sedation (barbiturate coma) 3) Consider mannitol 4) Consider hyperventilation
answer
What are the ways to prevent elevated intracranial pressure in patients with intracerebral hemorrhage and subarachnoid hemorrhage?
question
1) Prophylaxis for DVT and PE 2) Physical therapy, speech therapy, occupational therapy, swallowing studies 3) Recall that, of the patients who survive the acute period, only a little over half regain independent function - 30% remain incapacitated and require long-term care.
answer
What should be done after a intracerebral hemorrhage and subarachnoid hemorrhage that cause a stroke?
question
Transient ischemic attack (TIA)
answer
This is a sudden or rapid onset of neurologic deficit caused by cerebral ischemia. It may last for a few minutes or up to 24 hours and clears without residual signs. "a brief episode of neurologic dysfunction caused by focal brain or retinal ischemia, with clinical symptoms typically lasting less than 1 hour, and without evidence of acute infarction."
question
1) Determine type and location of TIA 2) Non-contrast CT scan 3) Duplex ultrasound and transcranial doppler 4) MRI/MRA can demonstrate circulation, evaluate for stenosis 5) ECG and transesophageal echocardiography 6) Hospitalization may expedite workup 7) Consider hospitalization for patient with first TIA in the past 24-48 hours, as well as those with symptoms that are worsening or last for more than one hour, if there is a known carotid artery stenosis, afib, or hypercoagulable state
answer
What should I do with Patients who have had a suspected TIA and require urgent evaluation?
question
1) * Consider thrombolytic therapy 2) Antiplatelet therapy - Aspirin reduces risk of subsequent TIAs or stroke - 325mg po qD - Ticlopidine 250mg po BID may be more effective than aspirin in preventing stroke but it's a lot more expensive - Clopidogrel (Plavix) 75mg po qD is another antiplatelet option. 3) Carotid endarterectomy (may be indicated for patients with 70% or more carotid stenosis (of course, only works for patients with stenosis of common or internal carotid artery, not in treatment of vertebrobasilar TIAs) 4) Angioplasty or stenting? ****Either way, antiplatelet agents should be started ****
answer
What is the treatment of a patient with a TIA?
question
1) HTN --> Control it baby! If you don't its badness 2) Other cardiac risk factors - Risk of stroke is 50% higher in smokers than in nonsmokers 3) Aspirin 4) Consider anticoagulation for patients with A-fibrillation
answer
What is the PRIMARY prevention of stroke and TIA?
question
STATINS 1) Statin therapy provides protection for all-cause mortality and nonhemorrhagic strokes 2) Statin therapy for all-stroke prevention: RR 0.84 (95% CI 0.79-0.91) 3) Statin therapy for all-cause mortality RR 0.88 (95% CI 0.88-0.93)
answer
How can I control my patient's lipids?
question
1) Lipid-lowering therapy (aggressive) - LDL 100 or less 2) Smoking cessation 3) Other cardiac risk factors 4) Stroke survivors average 10 outpatient visits/year
answer
What is the secondary prevention of stroke and TIA?
question
Carotid Doppler

answer
What is used in the evaluation "screening" of suspected stenosis of the intracranial internal carotid artery, middle cerebral artery, or basilar artery.
question
Conventional angiography
answer
**What is the s "gold standard" for AVM or SAH but has a 1% risk of stroke during procedure.**?
question
Transthoracic and transesophageal echocardiography (TTE or TEE)
answer
What is used to detect cardiogenic and aortic sources for cerebral embolism?
question
True
answer
T or F. Transthoracic and transesophageal echocardiography can be postponed until after the acute treatment phase
question
Coumadin
answer
Which is better in Atrial Fibrillation, Coumadin or Aspirin?
question
Surgical clipping or placement of coil for aneurysm Ligate or embolize AVM. Evacuation
answer
What are the surgical options for patietns with TIA/stroke?



