Neurology Blueprints I – Flashcards
Unlock all answers in this set
Unlock answersquestion
What is the clinical utility of CT and MRI?
answer
*CT* is best used to identify fresh blood *MRI* in general is better than CT for deeper brain structures such as the posterior fossa and craniocervical junction. *DWI MRI* is best used to catch early tissue ischemia, i.e. suspected stroke.
question
What are the three steps in approaching a coma patient?
answer
1. check for meningitis 2. attempt to reverse by administering thiamine, dextrose and naloxone 3. check brainstem reflexes and focal signs
question
What are the "focal signs?"
answer
hemiparesis aphasia reflex asymmetry facial droop unilateral babinski
question
What are the brainstem reflexes? (5)
answer
*Pupillary*: Shine light into each pupil and look for direct and consensual response. CN 2 in, CN 3 out *Oculocephalic*: Turn head horizontally and vertically and look for conjugate movement in the opposite direction. CN 8 in, CNs 3, 4, 5 out *Caloric*: inject ice water into ear and look for eye deviation towards ear injected. Do if oculocephalic is contraindicated (spine injury) *Corneal*: rub cornea with cotton and look for direct and consensual blink. CN V1 in, CN 7 out *Gag*: gag reflex, 9 in, 10/11 out
question
What are the general causes of depressed consciousness?
answer
Damage to the brainstem, which would cause absent brainstem reflexes Damage to *both* cerebral hemispheres simultaneously Damage to one of the hemispehres with pressure on the other side
question
Structural Causes of depressed consciousness
answer
Focal signs are present. If focal signs are absent, this suggests a diffuse cause, such as metabolic, infectious or toxic *Ischemic stroke* of brainstem or unilateral cerebral hemisphere. *Intracranial hemorrhage*: intraparenchymal, subdural, epidural *Brain Tumor*: with edema or hemorrhage *Brain Abscess*
question
What is the difference between Wernicke's encephalopathy and korsakoff syndrome?
answer
Wernicke's is an acute confusional state brought on by thiamine deficiency in alcoholics Korsakiff is a long-term memory disorder that can arise after Wernicke's has been resolved
question
Vision
answer
p. 26-36
question
What is the approach to weakness?
answer
1. confirm the complaint is indeed weakness and not pain, fatigue, etc 2. identify which muscle(s) are weak 3. Determine the pattern of weakness (muscle, NMJ, nerve, root, plexus, cord, brain) 4. associated symptoms 5. differential 6. labs, imaging
question
Muscles, with their movements, nerves and roots
answer
Table 5-1, p. 40
question
Differential Diagnosis for Peripheral Nerve Disorders
answer
*mononeuropathy*: entrapment (carpel tunnel), systemic vasculitis, metabolic and rheum disease *Polyneuropathy*: demyelinating (charcot marie tooth, GBS), axonal
question
What is the difference between a nerve root and a nerve plexus?
answer
A nerve exits the spinal cord as a *root* and then multiple roots form a *plexus*, in which individual fibers seperate and form peripheral nerves. Peripheral nerves thus often originate in more than one nerve root
question
What is the difference between a neuropathy and a radiculopathy?
answer
neuropathy implies peripheral nerve while radiculopathy implies nerve root
question
Associated signs for neuropathy vs radicupathy
answer
Mononeuropathy: pain Polyneuropathy: sensory loss, loss/diminished reflexes Radiculopathy: radiating tingling, pain, sometimes absent reflexes
question
Muscle Reflexes and their nerve roota
answer
1, 2 buckle my shoe - ankle jerk (S1) 3, 4 kick the door - hip and patellar (L3, L4) 5, 6 pick up sticks - biceps/brachioradialis (C5, C6) 7, 8 lay them straight - triceps, fingers (C7, C8)
question
Radiculopathy differential
answer
single = herniated disc, shingles reactivation poly = inflammatory, infectious
question
How can you tell if an injury is in a peripheral nerve or a plexus?
answer
A plexus injury will manifest as weakness in multiple muscles that have different roots. A peripheral nerve injury will be weakness only in the muscle that nerve supplies
question
Brachia Plexus
answer
MARMU - p. 42
question
Upper Motor Neuron
answer
- Constitutes the neuron from the motor cortex in the cerebral hemisphere through the pyramidal decussation into the spinal cord - Presents as weakness, spasticity, hyperreflexia, positive babinski
question
Lower Motor Neuron
answer
- Constitutes the anterior horn cell and its axon all the way through the root to the NMJ (basically everything outsides the spinal cord) - Presents as wasting and fasciculations
question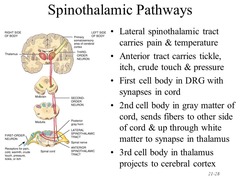
Spinothalamic Tract
answer
Lateral: Pain and temperature Anterior: Crude Touch Thinly myelinated or unmyelinated fibers Synapses in the dorsal horn and cross at the level of entry into the cord. Travel *contralaterally* up the cord Then travels up to the ventral posterolateral (*VPL*) nucleus in the thalamus, then to the somatosensory cortex of the postcentral gyrus
question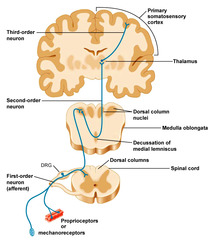
Dorsal Column
answer
Conscious Proprioception, vibration, well localized touch Heavily myelinated fibers Enter spinal cord and travel *ipsilaterally* up the cord in the nucleus gracilis and cuneatus to the lower medulla, where they cross as the medial lemniscus
question
Spinocerebellar Tract
answer
non conscious proprioception
question
Basic Lesion Localization
answer
*Peripheral Nerve*: sensory loss according to that nerve's territory *Nerve Root*: dermatomal sensory loss *Plexus*: sensory loss in multiple enrve territories *Spinal Cord*: sensory loss below level of lesion *Brainstem*: sensory loss in ipsilateral face and contralateral body *Thalamus/Cortex*: contralateral face, arm, leg
question
Dermatomes
answer
Back of head/neck = C2 Nipple = T4 Umbilucus = T10/T11 Genitals = S2/S3 Upper Leg = L2 Lateral foot = S1 Medial Foot = L5
question
Dissociated Sensory Loss
answer
Loss of a single tract with preservation of other tracts. Ex: Syringomyelia: loss of pain/temp, preservation of proprioception anterior spinal artery stroke: loss of pain/temp, preservation of proprioception Subacute combined degeneration: loss of proprioception, preservation of pain/temp
question
What 4 things could "dizziness" mean?
answer
vertigo: rotational sense of movement lightheadedness: faint-feeling, presyncopal dysequilibrium: imbalance/unsteadyness of legs ill-defined dizziness
question
Peripheral vs central vertigo
answer
Peripheral will have associated tinnitus/hearing loss, nausea, vomiting Central will have associated diplopia, dysarthria, dysphagia, vertical nystagmus
question
causes of vertigo
answer
*vestibular neuronitis*: acute unilateral peripheral vestibulopathy (no inflammation). acute onset, self-resolving *Labyrinthine Concussion*: head injury *Infarct*: (labyrinth, brainstem, cerebellum): PICA and AICA supply the vestibular apparatus and the internal auditory artery is supplied by AICA. sudden onset deafness/vertigo. Will have other neuro deficits *Meniere Disease*: episodic vertigo w/ nausea/vomiting along with fluctuating but progressive hearing loss, tinnitus, sensation of fullness/pressure in ear. Caused by increase in endolymph volume *Perilymph fistula*: the endolymph "pops" during increased pressure (straign) *Benign positional paroxysmal vertigo*: brief attacks of vertigo brought on by positional changes. Caused by free moving calcium carbonate crystals in the semicircular canals
question
Dix Halpike Maneuvar
answer
p. 54 combined vertical/torsional nystagmus treat w/ epley maneuvar (p. 57) t
question
Causes of Syncope
answer
*Neurogenic Syncope*: the pathophysiologic activation of mechanoreceptors leading to cardioinhibition of vasodepression (carried by vagus), leading to hypotension and bradycardia *Autonomic Failure*: failure to release norepi upon standing, leading to inability to vasoconstrict to counteract gravity's pull on blood. Causes could include parkinson's, MSA
question
Friedreich Ataxia
answer
Autosomal recessive progressive ataxia. Affects arms more than legs. Often has severe dysarthria, areflexia, spasticity, impaired vibration and positional sensation. Childhood onset.
question
Inherited Episodic Ataxia
answer
Two types, both marked by brief episodes of ataxia, vertigo, nausea, vomiting EA-1: mutation in voltage gated *potassium* channels. Brief attacks w/ muscle myokymia (quivering) in between attacks EA-2: mutations in pore forming alpha1 subunit in the P/Q type voltage gated *calcium* channels. Attacks are longer (several minutes) with interictal nystagmus
question
Autosomal Domiant Spinocerebellar Degeneration
answer
Insidious (slow) onset of gait and dysarthria n early adulthood. Mild to moderate cognitive decline is a late sign. Some subtypes are due to a *CAG* trinucleotide repeat expansion.
question
Miller Fisher Syndrome
answer
A variant of BGS characterized by the triad of ataxia, areflexia, ophthalmoplegia. The ataxia is due to proprioceptive loss, not cerebellar dysfunction. 90% of patients have IgG-anti-GQ1b antibodies in serum Self-limiting. Full recovery
question
What should you suspect in a patient with ataxia and ophthalmoplegia?
answer
Wernicke's Miller fisher MS cerebellar stroke posterior fossa mass
question
What should you suspect in a patient with ataxia and extrapyramidal signs?
answer
wilson's creutzfeldt jacob olivopontocerebellar atrophy
question
What should you suspect in a patient with ataxia and downbeat nystagmus?
answer
foramen magnum lesion posterior fossa mass
question
Other Gaits
answer
p.61
question
14 yo girl + 3 year history of slowly progressive gait ataxia and slurred speech + nystagmus + absent ankle reflexes + hammering toes + high arched feet + diminished virbatorysense in toes + no family history Diagnosis?
answer
*Friedreich Ataxia* (FRDA), a autosomal recessive mutation in FXN gene on chromosome 9 (GAA repeat of at least 66 units) with damage to cerebellum and peripheral nerves. Onset is between 10 and 15. Diabetes occurs in 30% of FRDA patients Hypertrophic cardiomyopathy occurs in 66% Hearing loss in 13% Patients are fertile
question
What part of the brain controls the bladder? (p. 66)
answer
*Voluntary*: dorsomedial *frontal lobe* ? *medial* pontine micturition center (PMC) ? detrusor muscle contraction ? voiding Lateral PMC ? urethral sphincter contraction ? urine retention *Spinobulbospinal*: bladder ? PMC ? parasympathetic sacral nuclei *Spinal Segmental*: detrusor ? Onuf's nucleus in S2-S4 spinal cord ? striated sphincter muscles (pudendal)
question
What happens when the PMC is damaged?
answer
incontinence? p. 65
question
Urge Incontinence
answer
Involuntary loss of urine along with strong desire to void (i.e. urgency). Detrusor instability (DI). If the cause of the DI is neurologic, it is termed "detrusor hyperreflexia* or spastic bladder. Essentially, the detrusor is contracting too much, reducing bladder capacity and causing involuntary voiding. *Causes*: strokes, frontal lobe dysfunction, suprasacral lesions, MS -> i.e. UMN
question
Detrusor Sphincter Dyssynergia
answer
inappropriate contraction of the external sphincter upon detrusor contraction. This is bad because detrusor contraction forces urine out and sphincter contraction keeps urine in. This usually happens in the context of urge incontinence and can lead to VU reflux and renal damage
question
Stress Incontinence
answer
involuntary loss of urine during periods of increased strain (laughing, sneezing, coughing) due to weakened pelvic floor muscles.
question
Overflow Incontinence
answer
involuntary loss of urine associated with overdistension of the bladder, reflecting a LMN problem. constant dribbling Results in atonic bladder, i.e. ?capacity ?compliance *Causes*: drugs, diabetic neuropathy, lower spinal cord injury, radical pelvic surgery, bladder/urethral obstruction
question
Supraspinal Disease Causing Urinary Incontinence
answer
*Stroke*: hyperreflexic, small bladder with ?urgency and ?frequency. Associated with poor functional outcome *parkinsons*: hyperreflexia, pseudodyssnergia
question
Treatment of Urinary Incontinence
answer
p. 69
question
What nerves are responsible for male sex?
answer
Pudendal: motor and sensory Para S2-S4: erection Sympa - T11-T12:ejaculation
question
What labs are important to get when working up erectile dysfunction?
answer
Prolactin, testosterone, gonadotropins
question
What physical exam findings suggest a physical cause of headache (making the headache secondary to this cause)?
answer
Papilledema = ICP temporal artery tenderness nuchal rigidity - meningitis
question
Migraine
answer
2nd most common headache, after tension Unilateral, throbbing, pulsatile, associated with nausea/vomiting, photophobia, phonophobia Last 3-72 hours May or may not have aura, usually visual (flashing lines, scotoma) Pain is thought to be carried by the trigeminal nucleus caudalis and parasympathetic efferents
question
Tension Headaches
answer
Most common headache Recurrent attacks of bilateral, pressing, squeezing, around the head (vice-like). Not accompanied by nausea or aura, not made worse by physical activity.
question
Cluster Headaches
answer
A rare form of trigeminal autonomic cephalgia (TAC). Unilateral, usually orbital or temporal, trigeminal pain with concurrent ipsilateral autonomic symptoms such as lacrimation, conjuctival injection, facial swelling, eyelid edema, rhinorrea, horner syndrome. All of these, except horner's, occur at the time of headache. Patients like to move around when they get these headaches. Triptans and steroids for aboriton. verapamil, lithium may be helpful for prophylaxis
question
Paroxysmal Hemicrania
answer
Unilateral with autonomic symptoms much shorter than cluster, usually 10-30 minutes more frequent than cluster, up to 40X/day Very responsive to *indomethacin*, an NSAID
question
Subarachnoid headache
answer
"Worst headache of my life" Begins suddenly and peaks in intensity w/in a few seconds of onset = ''thunderclap headache'' Get head CT and LP. Blood or yellow on LP (xanthochromia)
question
Low Pressure Headaches
answer
?Pressure in subarachnoid place or CSF can cause headache. Pain is bilateral. Usually arises as a complication of LP. The "low pressure" is really low volume of CSF, which can be caused by LP or rupture of a CSF pouch/cyst. ?Pain while upright ?Pain while lying down Treatment is recumbency, aggressive fluid replacement, caffeine and, if needed, epidural blood patch
question
Idiopathic Intracranial Hypertension (pseudotumor cerebri)
answer
?Pain while lying down ?Pain while standing upright ?Pain in mornings Accompanied by pulsatile tinnitus and transient visual obstructions, CN 6 palsies, papilledema Can be precipitated by valsalva Typical in young overweight women who often have menstrual abnormalities. Be wary of visual loss (compression of optic nerve) Dx: mass lesion, venous sinus thrombosis Tx: ?ICP via LP, diuretics
question
Temporal Arteritis
answer
giant cell, (women) over 50 claudication inflammatory changes, granulomas
question
chronic daily headache
answer
most likely transformed (chronic) migraine, chronic tension, med overuse or withdrawal
question
Trigeminal Neuralgia
answer
electric shock pain in the trigeminal distribution, often brought on by combing hair, brushing teeth, shaving, eating, drinking, gentle breeze on face may be caused by compression at the cerebellopontine angle. MRI is needed to rule out other compressive lesions Tx: carbamazepine or surgery (percutaneous radiofrequency ablation, microvascular decompression)
question
Postherpetic Neuralgia
answer
pain after shingles. burning, itching, sensitive to touch. pain can remain after rash subsides. TCAs or gabapentin for the pain
question
What are the components of the exam that is used to test aphasias/
answer
Fluency Repetition Comprehension Naming Reading Writing
question
Broca Aphasia
answer
Difficulty producing speech (fluency). Pts have trouble getting the words out and speech has lots of hesitations and false starts. Pts are aware of and frustrated by the aphasia Cannot repeat or write. Can comprehend written instructions Difficulty w/ tricky commands ("under the paper place the pen") *Cause*: superior MCA stroke. Broca's area is in the left (dominant) posterior frontal lobe, bordering the superior temporal lobe *Associated signs*: right sided face/arml weakness
question
Wernicke Aphasia
answer
Impaired comprehension. Cannot understand others and their speech is incomprehensible while speech production is preserved (word salad). Cannot repeat Unaware of their deficit - get angry/paranoid at people *Cause*: damage (stroke) to dominant superior temporal gyrus. Often inferior MCA stroke. *Associated signs*: contralateral (right) homonymous superior quadrantanopia (pie in sky)
question
Conduciton Aphasia
answer
Inability to repeat with preserved fluency and comprehension *Cause*: lesion in arcuate fasciculus, the white matter that connects Broca to Wernicke. Or lesions in temporal/parietal lobes that spares werkicke
question
Transcortical Motor Aphasia
answer
Nonfluent aphasia (i.e. perisulvian broca's) but with preserved repetition. *Cause*: frontal lobe lesion with preservation of the connection between broca and wernicke
question
Transcortical Sensory Aphasia
answer
perisylvian wernicke's but with preserved repetition due to lesion near wernicke *Cause*: left PCA stroke
question
Global Aphasia
answer
wernicke + broca
question
Subcortical Aphasia
answer
lesions in basal ganglia, thalamus weird aphasia
question
Pure Alexia
answer
Patients can write but they cannot read, even what they have just written *Cause*: lesion in dominant occipital lobe and splenium of corpus callosum, interrupting connections between wernicke's and visual cortex.
question
Apraxia
answer
Inability to carry out a task, ex hammer a nail, despite understanding the command and having the motor ability to enact it. It's as if they cannot imagine the execution, despite understanding it *Cause*: dominant frontal lobe = able to recognize the task done by others but cannot do it themselves parietal lesion = cannot recognize it either
question
Agnosia
answer
Inability to recognize objects. could be visual or tactile. due to sensory association lesions
question
Gerstmann's Syndrome
answer
Agraphia + acalculia + right-left confusion + finger agnosia Lesions in dominant inferior parietal lobe (the angular gyrus)
question
Sensory Neglect
answer
Cannot pay attention to left hemisphere, will only draw half a clock. Will also be unable to recognize when a stimulus is applied simultaneously, but will if applied separately. Lesions in nondominant (*right*) frontal or parietal lobe
question
Causes and Dementia and Tests to Run
answer
p. 89
question
Alzheimer's Disease (AD)
answer
usually above 65 yo, more common in women, associated with Down's syndrome and head trauma progressive, beginning with short-term memory impairment
question
AD Genes and Imaging
answer
*ApoE4* and *?2 macroglobulin* on chromosome 19 is a marker for both early and late onset - early onset genes: amyloid precursor protein (*APP*) on chromosome 21, presenilin 1 & 2 (*PS1/2*) on chromosomes 14 and 1 - ?tau ?A?-42 on CSF - hippocampus, amygdala, thalamus greatly reduced in size - bilateral temporoparietal hypometabolism on PET/SPECT scans *Autopsy*: brain atrophy, senile plaque (amyloid deposits) and neurofibrillary tangles (NFTs), which represent phosphorylated tau protein
question
AD Therapy
answer
*Donepezil* (Aricept): Achase inhibitor. SEs include GI and rarely liver *Rivastigmine* (exelon): Achase inhibitor. SEs include GI and rarely liver *Memantine* (namenda): NMDA receptor antagonist. SEs are dizziness, headache, confusion *Galantamine* (razadyne): Achase inhibitor. SEs include GI and weight loss
question
Vascular Dementia
answer
Acute onset/stepwise onset dementia along with focal neuro deficits. Brain imaging shows multiples strokes, lacunes, deep white matter changes. Most patients are hypertensive/diabetic. Must investigate cause of strokes (cardiac, coag).
question
Lewy Body Dementia
answer
The 2nd leading cause of dementia. Marked by cognitive impairment, impaired visuospatial perception and visual memory, fluctuations of alertness, prominent visual hallucinations, delusions, extrapyramidal symptoms, extreme sensitivity to neuroleptics (never give haldol). Death 10-15 years after diagnosis Lewy bodies are eosinophilic intracellular inclusions of ?synuclein. In Parkinson's they are in the substantia nigra In LBD, the *cortical neurons*. Treat with low dose atypical antipsychotics (risperidone, quetiapine)
question
Progressive Supranuclear Palsy (Steele-Richardson-Olszewski Syndrome)
answer
Failure of vertical gaze, dysarthia, dysphagia, extrapyramidal rigidity, gait ataxia, apathy and dementia. Atrophy of dorsal midbrain, globus pallidus, subthalamic nucleus Subcortical NFTs, neuron loss, gliosis Median survival = 6-10 years
question
Huntington Disease
answer
Autosomal dominant CAG repeat on chromosome 4. Requires at least 40 repeats for symptoms Onset 35-45 yo. Triad of chorea, behavior/personality changes (OCD, aggression) and dementia. Destruction of caudate/putamen (striatal GABA-nergic neurons) and loss of cortical neurons. The mutation causes flawed processing of proteins, resulting in deposits in nuclei and activation of cell death Treatment is dopamine antagonists
question
Frontotemporal Lobar Dementia
answer
First signs are congitive/behavioral, not memory.
question
Prion Disease
answer
Spongy degeneration, neuronal loss, gliosis, astrocytic proliferation CJD: rapidly progressive dementia, pyramidal signs, myoclonus, sharp waves on EEG. CSF is normal but may have 14-3-3 protein
question
HIV Associated Dementia
answer
HIV can cause encephalitis and also make patients prone tpo other CNS infections (toxo, TB, syphilis)



