Intro to Anesthesia Ch 1 & 2; Thomas F17 – Flashcards
Unlock all answers in this set
Unlock answersquestion
Anesthesia is used daily in most veterinary practices to provide ... (6)
answer
sedation, tranquilization, immobility, muscle relaxation, unconsciousness, and pain control
question
Define Anesthesia
answer
Loss of sensation; One extreme in a continuum level of CNS depression
question
Define General Anesthesia
answer
Reversible state of unconsciousness, immobility, muscle relaxation, and loss of sensation
question
Define Surgical Anesthesia
answer
1- A stage of general anesthesia 2- Analgesia and muscle relaxation 3- Eliminate pain and patient movement during the procedure
question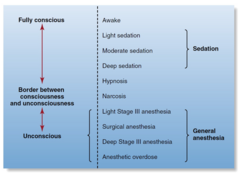
Explain the Continuum of CNS Depression (chart)
answer
(chart)
question
Sedation vs. Tranquilization
answer
Sedation = CNS depression Drowsiness Drug-induced Various levels Slightly aware or unaware of surroundings Aroused by noxious stimulation Uses: minor procedures Tranquilization = Calmness Patient is reluctant to move Aware of surroundings but doesn't care
question
Hypnosis vs. Narcosis
answer
Hypnosis = Drug-induced Sleeplike state Impairs patient's ability to respond to stimuli Patient can be aroused with sufficient stimulation Narcosis = Drug-induced sleep Patient is not easily aroused Associated with narcotic drugs
question
Define Local Anesthesia
answer
1- Targets a small, specific area of the body 2- Loss of sensation to a specific area 3- Drug is infiltrated into the desired area
question
Define Topical Anesthesia
answer
1- Applied to body surfaces or a wound 2- Produces a superficial loss of sensation
question
Define Regional Anesthesia
answer
1- Loss of sensation to a limited area of the body For example, Nerve blocks & Epidural anesthesia
question
Define Balanced Anesthesia
answer
1- Using multiple drugs in smaller quantities Maximizes benefits & Minimizes adverse effects Gives anesthetist greater control
question
The Credentialed Veterinary Technician's Role as an Anesthetist (4)
answer
1- Anesthetic machine (a) Preparation (b) Operation (c) Maintenance 2- Administer anesthetic agents 3- Endotracheal intubation 4- Patient monitoring
question
Anesthesia Challenges and Risks (5)
answer
1_ Dose calculation and rate adjustment 2- Vital signs and anesthetic depth 3- Assess multiple pieces of information 4- Patient management 5- Anesthetic accidents
question
Anesthetics have a Wide or Narrow therapeutic index?
answer
NARROW
question
Miscalculation during anesthesia can result in...
answer
serious consequences Most anesthetic agents have a very narrow therapeutic index, so the consequences of a calculation or administration error may be serious. Therefore care and attention to detail are critical when dosages are calculated and rates of administration are adjusted
question
What does "Assess Multiple Pieces of Information" during anesthetic monitoring mean?
answer
The anesthetist must accurately interpret a wide spectrum of visual, tactile, and auditory information from the patient, anesthetic equipment, and monitoring devices. To do this successfully, he or she must be able to rapidly assess multiple pieces of information and distinguish those that require action from those that do not.
question
What are "Anesthetic Accidents"?
answer
Death, stroke (in humans) The outcome can be devastating or lethal Owners may pursue legal action Prevent accidents by using high standards Keep meticulous records
question
Role of the Veterinary Anesthetist (6)
answer
Minimum patient database Proper patient fasting Preinduction patient care All supplies are available All equipment is in working order Preanesthetic medication
question
Minimum Patient Database (MPD)... 3 things
answer
Patient history Physical examination and assessment Preanesthetic diagnostic workup
question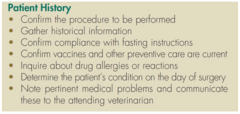
Patient Preparation "To Do" List (7 things)-- Chart
answer
(chart)
question
When obtaining patient history, remember to obtain these 5 things for each aspect...
answer
Information given freely Duration Severity or volume Frequency Appearance or character
question
When obtaining the history, determine each of the following: (5)
answer
The signalment Current and past illnesses Medications currently being administered Allergies or drug reactions The status of preventive care
question
Patient History - SIGNALMENT (5)
answer
Species Breed Age Sex Reproductive status
question
Anticholinergics avoided in ...
answer
ruminants
question
Ventilation and physical support for...?
answer
large animals
question
Excess airway secretions occur in ...?
answer
cats and ruminants
question
Exotic animals are handled ...?
answer
differently; they're weird
question
___ and ____ are more sensitive to opioids
answer
Horses and cats
question
____ and ____ are sensitive to acepromazine
answer
Boxers and giant breeds
question
____ are resistant to acepromazine
answer
Terriers
question
_______ are difficult to intubate
answer
Brachiocephalic dogs
question
______ are sensitive to barbiturates
answer
Sighthounds
question
_____ are sensitive to sedatives
answer
Draft horses
question
Don't use thiobarbiturates on _______ (and give examples)
answer
sight hounds Which are = Greyhounds Irish Wolf hounds Saluki Afghan Borzoi Whippet Basenji Pharaoh hound
question
During the Anesthesia Pre anesthetic evaluation, Signalment can alert to possible problems, give 3 examples
answer
1- Age 2- Sex (Status) 3- Breed Young patients may have Hypothermia or Hypoglycemia. Old patient may have Decrease liver and kidney function. Decreased muscle mass May also affect dose. Sex and reproductive status; are they In heat ? Pregnant?
question
Acepromazine is contraindicated in ...?
answer
stallions
question
Xylazine is contraindicated in pregnant ___ and ____.
answer
cows and ewes
question
Re: Patient History—Medications; May influence effect of anesthetic agents, give 5 different ways
answer
1- Sympathomimetics 2- Tricyclic antidepressants 3- Antibiotics 4- Monoamine oxidase inhibitors 5- Antihistamines Detailed explinations = 1- Epinephrine and cyclohexamines, xylazine, barbiturates, and halothane can cause cardiac arrhythmias. 2- Amitriptyline and clomipramine can cause cardiac arrhythmias. 3- Chloramphenicol can cause decreased biotransformation of barbiturate anesthetics and lead to prolonged recovery. 4- Amitraz and selegeline can increase the effects of morphine and other opioids. They can also lead to additive effects with anticholinergics or CNS depressants. 5- Antihistamines can cause CNS and respiratory depression with opioids.
question
What does an average Cat ketamine recovery look like?
answer
prolonged
question
What will Dogs have after acepromazine sedation?
answer
behavioral change
question
Patient History—Record Preventive Care includes... (2+ species specific)
answer
1- Vaccination—date and type 2- Fecal analysis and parasite control Heartworm status—dogs FLV and FIV testing—cats Tetanus toxoid—horses
question
Physical Examination (PE) vs. Physical Assessment (PA)
answer
PE = Performed by a veterinarian To determine diagnosis and treatment planning PA = Performed by a veterinary technician To provide maximum patient care, respond to patient needs, detect changes in patient condition
question
What organ systems are most affected by anesthetic agents?
answer
Cardiovascular, nervous, and pulmonary systems are most affected by anesthetic agents
question
Describe the body condition scales of 1-9 and 1-5 for dogs and cats
answer
1-9 scale 4-5 in dogs or 5 in cats is the ideal weight 1 is extreme cachexia; 9 is extreme obesity 1-5 scale 3 is the ideal weight for both 1 is extreme cachexia; 5 is extreme obesity
question
A B/A/R patient is....
answer
bright, alert, and responsive—he is noticeably engaged and interested in his environment.
question
A Q/A/R patient is...
answer
quiet, alert, and responsive—he is not really engaged or interested in what is going on around him.
question
What does an elevated or decreased body temp indicate?
answer
Elevated = inflammation Decreased = numerous systemic disorders ----------------------------------------------- A high body temperature most commonly indicates an inflammatory condition, which must be identified and may require pretreatment with antibiotics, antiinflammatories, or other medication. A significantly low body temperature may be associated with one of a number of serious systemic disorders.
question
Normal vital signs for a dog
answer
Body temp 100-102.5 HR 60-180 Heart Rhythm NSR or SA RR 10-30 (panting is normal)
question
Normal vital signs in a cat
answer
Body Temp 100-102.5 HR 120-240 Heart Rhythm NSR only RR 15-30
question
Normal vital signs for a horse
answer
Body Temp 99-100.5 HR 30-45 Heart Rhythm NSR, SA or 1st or 2nd degree AV block RR 8-20
question
Normal vital signs for a cow
answer
Body Temp 100-102.5 HR 60-80 Heart Rhythm NSR or SA RR 8-20
question
Acronym for Eyes, ears, nose, oral cavity (throat)
answer
EENT
question
What does PLR stand for?
answer
Pupillary Light Reflex
question
Normal sinus rhythm (NSR) can be expected in healthy....
answer
Dogs, cats, rodents, ferrets, rabbits, horses, ruminants No rhythm irregularities
question
Sinus arrhythmia (SA) can be expected in HEALTHY....
answer
Dogs, horses, ruminants Heart rate is affected by respiration but they're still healthy Sinus arrhythmia is a rhythm in which the heart rate cyclically increases during inspiration and decreases during expiration. This rhythm may be pronounced in young, healthy dogs and can sound to the inexperienced anesthetist as if there are skipped or premature beats. Abnormal rhythms can be differentiated from sinus arrhythmia by observing the respirations while listening to the heart.
question
How to find and listen to a heart murmur
answer
Listen over each valve; Cranial-most aspect of left axilla—PDA They are Caused by blood flow turbulence and May result in increased patient anesthetic risk Murmurs can be associated with leaking valves, stenotic valves, stenotic vessels, and abnormal communication between heart chambers.
question
Pulse palpation points in Dogs and cats....
answer
femoral artery
question
Pulse palpation points in large animals...
answer
animals—facial artery, ventral tail artery, or auricular artery
question
How do you find the femoral artery in a dog or cat?
answer
In the conscious dog and cat the pulse is most easily palpated at the femoral artery, on the medial side of the rear leg. The patient should be standing quietly, and the femoral artery should be located by cupping the hand around the medial aspect of the thigh with the pad of the first or second finger in the groin just over the femur
question
Pale mucous membranes or prolonged capillary refill time are indicative of ...
answer
decreased perfusion from shock, vasoconstriction, hypotension, or a variety of other issues including anemia.
question
Cyanotic mucous membranes indicate what?
answer
reduced oxygen saturation, which is a medical emergency.
question
Dyspnea and cyanosis are both what?
answer
medical emergencies and should be brought to the veterinarian's attention immediately.
question
Avoid _________ dyspneic or cyanotic patients... because why?
answer
STRESSING; as they are very intolerant of handling and can die during examination.
question
RE: Respiratory System Examination Lung Auscultation, what are Discontinuous sounds?
answer
crackles, rales, or rhonchi
question
RE: Respiratory System Examination Lung Auscultation, what are Continuous sounds?
answer
wheezes
question
RE: Respiratory System Examination Lung Auscultation, what may Discontinuous or Continuous be an indication of?
answer
either pulmonary conditions (including pneumonia, bronchial disease, or asthma) or heart failure
question
A distended abdomen may indicate ....?
answer
fluid accumulation, pregnancy, organ enlargement, or tumor
question
RE: Abdominal Palpation and Auscultation, normal is....?
answer
soft and not painful
question
RE: Preanesthetic Diagnostic Workup.... No one standardized diagnostic workup fits every patient to be anesthetized, give 3 examples of types of workups that could occur
answer
Geriatric patient workup Elective surgery patient workup Sick patient workup Workup based on financial considerations
question
What blood test is in-house and an excellent indicator of the likelihood of perioperative bleeding?
answer
The buccal mucosal bleeding time is a simple in-house screening test that is an excellent indicator of the likelihood of perioperative bleeding
question
What things are RED FLAGS and should be pointed out to the attending DVM immediately?
answer
The following findings should be reported to the attending veterinarian immediately: A PCV ;25% in a dog or ;20% in a cat, horse, or cow A PP ;4.0 in any species Any decrease in the platelet count Any coagulation test result outside the normal range
question
Preanesthetic Diagnostic Tests and Procedures... name some (6+)
answer
Complete blood count (CBC) Urinalysis Blood chemistry Blood coagulation screens Electrocardiogram (ECG) Radiography Other tests as deemed necessary
question
Blood test Ideally done day of or day prior for dogs categorized by age 7yrs
answer
Laboratory evaluation of patient Young dogs7yr: PCV, TPP, GLU, BUN, CREA,, ALT, ALK PHOS, +/- additional chemistries, and electrolytes (Na+, K+, Cl-)
question
Patient Status: American Society of Anesthesiologists standards; Class I
answer
Class I Normal patient with no organic disease
question
Patient Status: American Society of Anesthesiologists standards; Class II
answer
Class II Patient with mild systemic disease
question
Patient Status: American Society of Anesthesiologists standards; Class III
answer
Class III Patient with severe systemic disease limits activity but not incapacitating
question
Patient Status: American Society of Anesthesiologists standards; Class IV
answer
Class IV Patient with incapacitating systemic disease that is a constant threat to li
question
Patient Status: American Society of Anesthesiologists standards; Class V
answer
Class V Moribund patient is not expected to live 24 hours with or without surgery
question
How to Designate emergency operation?
answer
Designate emergency operation by "E" after appropriate classification
question
Classification is based on an evaluation of the Minimum Patient Database; explain
answer
Class P1 = minimal anesthetic risk Class P5 = extreme anesthetic risk Classes P1 and P2 use standard anesthetic protocol Classes P3 to P5 need special protocols and stabilization In general, class PS1 and class PS2 patients can be anesthetized with standard anesthetic protocols. Class PS3 to PS5 patients often require special protocols, and should be stabilized before surgery if possible.
question
_________ is a preanesthetic that is also an antiemetic—it will prevent vomiting
answer
Acetpromazine
question
_______ will induce vomiting so the stomach can be emptied.
answer
Xylazine
question
Reasons for placing an IV catheter (5)
answer
1- Fluid administration 2- Rapid IV access in an emergency 3- Constant rate infusion (CRI) of drugs or anesthetic agents 4- Administration of vesicants 5- Sequential administration of incompatible drugs
question
Sizes of IV catheters used in small animals and large animals
answer
Most commonly used 16-24 gauge, 3/4- to 2-inch catheter (small animals) 12-16 gauge, 5¼-inch catheter (large animals)
question
Two main types of IV catheters are in common use for fluid and drug administration in veterinary patients....
answer
through-the-needle catheters and over-the-needle catheters
question
Although commonly used in critical care patients, ___________catheters are not frequently used for anesthesia because they are more complex, expensive, and time-consuming to place, especially if the technician is not experienced with their use.
answer
through-the-needle catheters
question
When placing and maintaining an IV catheter for use during surgery, consider the following... (8)
answer
1- Choose a catheter of sufficient length to minimize the risk of dislodgement. 2- Choose a catheter of large diameter. 3- Choose a location that will not interfere with the procedure. 4- Use an administration set with an injection port. 5- After positioning the patient, check that fluids are flowing freely. 6- Avoid excessive catheter and patient movement during transfer. 7- Administer IV drugs slowly. 8- Use saline flush following IV injection of a drug.
question
Placing an IV Catheter in a Small Animal Patient (name the parts in the chart)

answer
a, Catheter (20 to 24 gauge, ¾ to 1 ½ inches long for cats; 16 to 22 gauge, 1 to 2 inches long for dogs); b, two approximately 6-inch-long strips of 1-inch porous adhesive tape, one approximately 6-inch-long and one approximately 3-inch-long strip of ½-inch tape; c, clipper with #40 blade; d, 1:1 chlorhexidine surgical scrub/water-soaked cotton balls and alcohol-soaked cotton balls; e, ½-inch plastic strip with antiseptic ointment; f, T-port, cap, or administration set (both the catheter and T-port should be flushed with saline before catheterization).
question
Placing an IV Catheter in a Small Animal Patient (1)

answer
Standard aseptic technique uses three chlorhexidine-soaked alcohol cotton balls followed by three alcohol-soaked cotton balls. Assistant is needed to hold off the vein. Apply tension in a ventral direction to tense the skin. Position the catheter with the needle fully inserted and with the bevel up.
question
Placing an IV Catheter in a Small Animal Patient (Cont'd -2)

answer
Advance the catheter and needle assembly as a unit through the skin and the near wall of the vein. Blood will flashback into the needle hub when the vein is entered. Advance the unit a few more millimeters until the end of the catheter is firmly seated in the vein.
question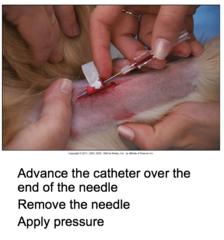
Placing an IV Catheter in a Small Animal Patient (Cont'd-3)
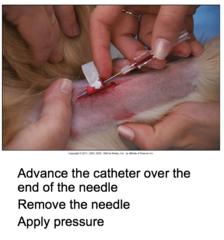
answer
Holding the needle stationary, advance the catheter over the end of the needle until it is inserted to the hub. Remove the needle. Have the assistant apply pressure at the insertion site to prevent bleeding.
question
Placing an IV Catheter in a Small Animal Patient (Cont'd-4)

answer
Flush the catheter with several milliliters of normal saline through the injection port.
question
Placing an IV Catheter in a Small Animal Patient (Cont'd-5)

answer
Twist the 3-inch-long strip of ½-inch tape into a "bow-tie" configuration.
question
Placing an IV Catheter in a Small Animal Patient (Cont'd-7)

answer
Chlorhexidine ointment is used on the plastic strip.
question
Placing an IV Catheter in a Small Animal Patient (Cont'd-8)

answer
Tear a ½-inch "V" in a 6-inch length of 1-inch tape about 1 inch from the end. Slip it under the catheter with the torn area directly under the catheter hub.
question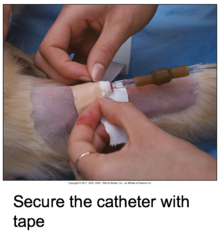
Placing an IV Catheter in a Small Animal Patient (Cont'd-9)
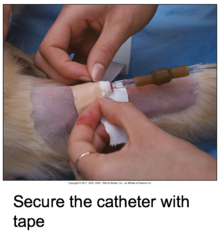
answer
Apply the remainder of this length of tape over the plastic strip to secure.
question
Placing an IV Catheter in a Small Animal Patient (Cont'd-10)

answer
Apply the remaining 6-inch-long strip of 1-inch tape around the administration set line or T-port to create a tension loop.
question
Giving an IV Injection Through an IV Administration Set Port -1

answer
IV fluids should be flowing at the standard infusion rate.
question
Giving an IV Injection Through an IV Administration Set Port (Cont'd-2)

answer
Pinching off the administration set line between the injection port and the fluid bag will prevent backflow of agent into the fluid bag during injection.
question
Giving an IV Injection Through an IV Administration Set Port (Cont'd-3)

answer
Give the medication at an appropriate rate as dictated by the VIC. For most medications, a slow IV bolus is appropriate.
question
Giving an IV Injection Through an IV Administration Set Port (Cont'd-4)

answer
Following injection, the administration set line must be released so that the entire dose of medication is flushed into the patient. As much as 0.5 to 2 mL of agent will remain in the fluid line and catheter until flushed out. When administering an induction agent, administer additional doses to effect by following these same steps. As soon as the patient is at an anesthetic depth adequate to permit intubation, remove the needle and syringe to prevent accidental overdose.
question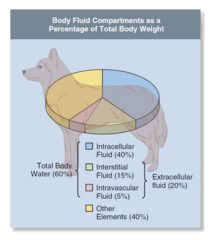
Composition of Body Fluids
answer
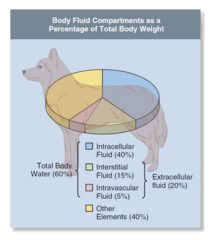
In adult animals, about 60% of the body weight is water. Of the 60% of the body weight that consists of water, about two thirds (or 40% of the body weight) is intracellular fluid (ICF). Although estimates of extracellular fluid (ECF) vary widely (about 15% to 30% of body weight for small animals), most clinicians use the figure 20% for the purpose of calculating fluid needs. About three fourths of the ECF (15% of the body weight) is interstitial fluid (fluid between the cells), and one fourth (5% of the total body weight) is intravascular fluid (plasma) .
question
Plasma is ____ of body weight
answer
5%
question
Blood volume is ______ of body weight—dogs and large animals and _____ of body weight—cats
answer
8-9% of body weight—dogs and large animals 6-7% of body weight—cats
question
Calculating blood volume; Dogs and large animal and cats (2)
answer
Dogs and large animals = 90 mL/kg lean body weight Cats = 60 mL/kg lean body weight
question
Body fluids consist of water and ________.
answer
solutes
question
Body fluid solutes are either atoms or molecules dissolved in body water. The solutes most important in fluid therapy are small-molecular-weight electrically charged particles called _______, large-molecular-weight plasma proteins called _______, and small nonionic particles such as ______ and _________ ________.
answer
ions, colloids, glucose and small proteins.
question
Cations have a ______ charge Anions have a ______ charge
answer
positive , negative
question
Important Electrolytes: Anions (4)
answer
Chloride (Cl?) Bicarbonate (HCO3?) Phosphates (HPO42? and H2PO4?) Proteins
question
Important Electrolytes: Cations
answer
Sodium (Na+) Potassium (K+) Magnesium (Mg2+) Calcium (Ca2+)
question
What are Electrolytes?
answer
Electrolytes are substances that when dissolved separate into positively charged ions, called cations (so called because they migrate toward the cathode during electrolysis), and negatively charged ions, called anions (so called because they migrate toward the anode).
question
Define Homeostasis
answer
A constant state within the body created and maintained by normal physiologic processes Homeostasis is the state of health.
question
Solute concentration (osmolarity) in any fluid compartment must be __________..... WHY?
answer
300 mOms/L. Because Solutes must provide osmotic pressure to pull water into a compartment. In any given compartment, positively and negatively charged particle numbers must be equal.
question
What % of IV fluids will stay in the intravascular and interstitial space? WHY?
answer
One-third of IV fluids administered will stay in the intravascular space. Two-thirds will diffuse into the interstitial space. Colloids don't pass freely through the vascular endothelium. The presence of colloids in the intravascular space draws water into the space creating osmotic or oncotic pressure.
question
What 2 solutes must be monitored closely to make sure normal heart and muscle function continue?
answer
Some solute concentrations (Ca2+, K+) must be kept within a narrow range to maintain normal heart and muscle function.
question
Profound perioperative hemorrhage involves what?
answer
significant loss of albumin, blood cells, and other constituents of blood in addition to electrolytes and water. Patients with low albumin may require colloids or blood plasma (fluids containing large solutes), which provide oncotically active particles that remain in the vascular space for longer periods and help maintain blood volume and pressure.
question
To support patients experiencing severe perioperative hemorrhage, administration of WHAT may be necessary, and why?
answer
blood products may be necessary to provide RBCs or hemoglobin to support oxygen-carrying capacity, and in some cases clotting factors and platelets to support normal coagulation.
question
Perioperative hemorrhage involves what?
answer
fluid loss from the intravascular space, part of the ECF space.
question
Patients with perioperative hemorrhage may also benefit from what?
answer
Patients with perioperative hemorrhage may also benefit from hypertonic saline or colloid solutions, both of which draw water into the vascular space and raise blood pressure.
question
What are the 2 Classifications of IV fluids?
answer
These fluids are most commonly classified as either crystalloids or colloids based in the molecular weight of the primary solutes they contain All IV fluids are solutions consisting of one or more solutes dissolved in water. Most IV fluids contain one or more electrolytes. Dextrose, a naturally occurring form of glucose, is another ingredient present in some fluids. Some fluids also contain the buffers lactate, gluconate, or acetate, which are converted to HCO3- by the liver and help regulate pH. Others contain colloids (large-molecular-weight solutes). There are many intravenous solutions, each with different solute profiles.
question
Replacement fluids have high concentrations of ___ and ____ (as ECF does) and are designed to replace fluid losses.
answer
Na+ and Cl-
question
Maintenance fluids have lower concentrations of Na+ and Cl- but somewhat more ____ and are designed to maintain fluid balance over a longer period.
answer
K+
question
General Facts about Crystalloid Intravenous Fluids (3)
answer
Water and small-molecular-weight solutes May contain dextrose and/or buffers Often used in anesthetized patients
question
Isotonic, polyionic replacement solutions (4)
answer
Lactated Ringer's solution (LR) Normosol-R (NR) Plasma-Lyte A and R (PA and PR) Isolyte S (IS)
question
____ & ________ and cannot be administered with blood products
answer
LR and PR contain calcium
question
Isotonic, polyionic maintenance solutions contain less ___ and _____
answer
Contain less sodium and chloride
question
Isotonic, polyionic maintenance solutions contain more _____
answer
potassium
question
Isotonic, polyionic maintenance solutions contain lower concentrations of _____
answer
buffer
question
Isotonic, polyionic maintenance solutions contain _____
answer
DEXTROSE
question
Isotonic, polyionic maintenance solutions INCLUDE _____ and _______
answer
Normosol-M in 5% dextrose (NM5) Plasma-Lyte 56 in 5% dextrose (PL5)
question
Normal saline (NS) includes.... (3)
answer
Physiologic saline 0.9% saline sodium chloride 0.9%
question
Normal saline (NS) is Sometimes used instead of ...?
answer
isotonic, polyionic replacement crystalloid solution
question
Normal saline (NS) is used to....(3)
answer
Used to bathe tissues during surgery Used to flush the IV catheter Used to flush body cavities
question
_____________ are the first choice for fluid therapy of healthy patients undergoing routine surgery as well as many sick patients, as long as the PCV is over ______ and the plasma protein is over _______
answer
Isotonic, polyionic replacement crystalloids, 20% , 3.5 gm/dL.
question
The hypertonicity results in ....?
answer
fluid being drawn into the intravascular space to maintain blood pressure
question
Concentrated saline solution (3%, 7%, and 23.4% [diluted to less than or equal to 7.5%]) is given with isotonic crystalloids in acute care settings to treat ....?
answer
patients with hypovolemic, traumatic, or endotoxic shock
question
Hypertonic saline rapidly but temporarily draws water ______ the intravascular space and supports blood pressure, but, like other crystalloids, _______________ into the interstitial space and so must be followed with _________ if the patient needs long-term blood volume expansion.
answer
into, rapidly diffuses, colloids
question
Dextrose solutions with or without electrolytes are used to support .....?
answer
blood glucose in neonatal, hypoglycemic, or debilitated patients and in patients with diabetes mellitus that are receiving insulin, or as a part of therapy for hyperkalemia.
question
Dextrose solutions are considered ________ solutions
answer
hypotonic
question
Dextrose solutions come in what %s?
answer
5% dextrose in water (D5W) or 2.5% dextrose
question
Colloids are used to support ...?
answer
expansion of blood volume and blood pressure.
question
Colloid solutions stay in the intravascular space longer because ?
answer
...of the large solutes that cannot pass through the endothelium. Colloids solutions (also referred to as colloids) contain large-molecular-weight solutes that do not freely diffuse across vascular endothelium and therefore stay in the intravascular space.
question
Give an example of a Synthetic colloid solutions
answer
Hetastarch
question
Fluid therapy is an exact or inexact science.
answer
INEXACT. Although there are generally accepted fluid choices and administration rates for animals that are in shock, ill, experiencing blood loss, or undergoing surgery, each patient must be managed in a unique manner appropriate to its condition. Even though these standard rates are used as a starting point, ultimately the veterinarian will use his or her professional judgment to determine the final rate for each patient.
question
Fluid Administration Rate During routine anesthesia and surgery
answer
10 mL/kg/hr during the first hour 5 mL/kg/hr during remainder of the procedure For both small and large animals, a rate of 10 mL/kg/hr during the first hour followed by 5 mL/kg/hr for the remainder of the procedure is commonly used as the IV administration rate for crystalloids during routine anesthesia and surgery. The authors of the 2013 AAHA/AAFP Fluid Therapy Guidelines for Dogs and Cats consider that this may be unnecessarily high for many patients, especially cats, which are more susceptible to overhydration. They therefore recommend an initial rate of 5 mL/kg/hr in dogs and 3 mL/kg/hr in cats, followed by a reduced rate if the patient is anesthetized for more than 1 hour.
question
Fluid Administration Rate Isotonic Crystalloids; Excessive hemorrhage or hypotension
answer
40 mL/kg/hr (dogs and large animals) 20 mL/kg/hr (cats) As mentioned in the previous section, isotonic, polyionic replacement crystalloids including LR, PLA, PL148, and NR are the first choice fluid for healthy patients undergoing routine surgery as well as many sick patients as long as the PCV is over 20% and the plasma protein is over 3.5 gm/dL. Consequently these fluids are used in the vast majority of anesthetized patients.
question
Fluid Administration Rate Isotonic Crystalloids; Shock
answer
90 mL/kg/hr as rapidly as possibly (dogs and large animals) 55 mL/kg/hr as rapidly as possible (cats) As mentioned in the previous section, isotonic, polyionic replacement crystalloids including LR, PLA, PL148, and NR are the first choice fluid for healthy patients undergoing routine surgery as well as many sick patients as long as the PCV is over 20% and the plasma protein is over 3.5 gm/dL. Consequently these fluids are used in the vast majority of anesthetized patients.
question
Fluid Administration Rate Isotonic Crystalloids; Shock and blood loss (large and small animals)
answer
7% hypertonic saline 3-4 mL/kg slowly over 5 minutes Followed by isotonic crystalloid solution As mentioned in the previous section, isotonic, polyionic replacement crystalloids including LR, PLA, PL148, and NR are the first choice fluid for healthy patients undergoing routine surgery as well as many sick patients as long as the PCV is over 20% and the plasma protein is over 3.5 gm/dL. Consequently these fluids are used in the vast majority of anesthetized patients.
question
Hetastarch can cause ____ and _____ if administered too rapidly
answer
nausea and vomiting
question
Fluid Administration Rate Colloids; Administer as a slow bolus
answer
Over 15-60 minutes (dogs and large animals) Over 30-60 minutes (cats) Synthetic colloids should be administered to dogs and large animals as a slow bolus of 5 mL/kg over 15 to 60 minutes and to cats as a slow bolus of 2.5 to 3 mL/kg over 30 to 60 minutes with reassessment before giving additional boluses, up to a maximum of 10 to 20 mL/kg/day for dogs and for large animals and 5 to 10 mL/kg/day for cats.
question
Adverse Effects of Fluid Administration
answer
1- Volume overload Pulmonary or cerebral edema Use slower infusion rate 2- Overhydration Ocular and nasal discharge Chemosis (edema and swelling of the conjunctiva), Subcutaneous edema Increased lung sounds Increased respiratory rate and dyspnea Coughing and restlessness if patient is awake Hemodilution (dilution of the RBCs and plasma proteins)
question
Who is at greater risk for fluid Volume overload?
answer
Animals weighing less than 5 kg and those with cardiac or renal disease are at greatest risk.
question
Use macrodrip sets (10 or 15 gtt/mL) for infusion rates equal to or greater than _______
answer
100 mL/hr.
question
Use microdrip sets (60 drops/mL) for infusion rates less than ________
answer
100 mL/hr.
question
Preanesthetic/Preoperative Medications (5)
answer
Antibiotics Preemptive analgesia Antiemetics Anticonvulsants Antiinflammatory drugs
question
Anesthetic agent is....?
answer
any drug used to induce a loss of sensation with or without unconsciousness
question
Adjunct is...?
answer
a drug that is not a true anesthetic, but that is used during anesthesia to produce other desired effects such as sedation, muscle relaxation, analgesia, reversal, neuromuscular blockade, or parasympathetic blockade
question
Route of administration for Anesthetic Agents and Adjuncts (4)
answer
Inhalant Injectable Oral Topical
question
Time of administration periods (3)
answer
Preanesthetic Induction Maintenance
question
Agonists does what?
answer
Bind to and stimulate target tissue Most anesthetic agents and adjuncts are Agonists
question
Antagonists do what?
answer
Bind to target tissue but don't stimulate Reversal agents are Antagonists Antagonists competitively bind to target tissues preventing the corresponding agonist from causing more stimulation. Must use the proper antagonist when "waking" a patient from anesthesia.
question
Partial Agonists and Agonist-Antagonists
answer
Opioids Partial agonists Agonist-antagonists Used to block pure agonists



