Health Alterations LP 5 Diabetes maintenance and management ATI – Flashcards
Unlock all answers in this set
Unlock answersquestion
diabetes mellitus is a...
answer
complex disorder of metabolism stemming from deficiencies in insulin secretion. It is a group of metabolic diseases involving hyperglycemia d/t impaired insulin secretion, action or both.
question
alpha- glucosidase inhibitor
answer
type of oral antidiabetic agent that delays the absorption of carbs in the intestines
question
beta cells
answer
type of cell in the pancreas that secretes insulin
question
casual plasma glucose
answer
glucose concentration in the blood of a specimen taken at any time of day regardless of the time since the persons last meal; also called "random blood glucose"
question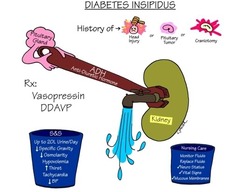
diabetes insipidus
answer
disorder of the posterior lobe of the pituitary gland that causes excessive thirst and excretion of large volumes of dilute urine.
question
duration
answer
referring to medications, the length of time a drug exerts a therapeutic effect.
question
fasting
answer
ingesting only water or nothing at all for a predetermined length of time
question
fingerstick

answer
use of a small lancet to puncture the skin on the side of a fingertip to obtain a single drop of capillary blood for diagnostic testing
question
glucometer
answer
a device used to determine the approximate concentration of glucose in the blood
question
glucose
answer
simple sugar that is the end product of carbohydrate metabolism
question
insulin
answer
hormone secreted by the beta cells of the islet of langerhans, that is essential for the metabolism of carbohydrates, proteins and fats.
question
islets of langerhans
answer
tiny, irregular structures distributed throughout the pancreas and comprising its endocrine portion.
question
Ketoacidosis
answer
accumulation of ketones (acids formed from the breakdown of free fatty acids in the absence of insulin) in the blood, associated with uncontrolled diabetes and resulting in metabolic acidosis
question
metabolic syndrome
answer
group of abnormalities (including high levels of glucose and triglycerides) associated with an increased risk of type II diabetes and coronary heart disease
question
Microalbuminuria
answer
early sign of renal disease involving the presence of albumin in the urine in amounts greater than the expected but too low to be detected by dipstick testing
question
nephropathy
answer
long term complication of diabetes that involves damage to the cells of the kidneys and eventually leads to end stage renal disease
question
neuropathy
answer
any of numerous disturbances or pathologic changes in the peripheral nervous system, most often affecting sensation, and often a long term complication of diabetes.
question
non-sulfonylurea secretagogue
answer
type of oral antidiabetic agent that stimulates insulin release; also called glinide.
question
onset
answer
the point when a drug begins to exert its therapeutic effect
question
pancreas
answer
large gland that secretes digestive enzymes and the hormones insulin and glucagon
question
peak
answer
the point when a drug is at its highest concentration in the body
question
polydipsia
answer
excessive thirst and fluid intake
question
polyphagia
answer
excessive hunger
question
polyuria
answer
excretion of abnormally large amounts of urine
question
postprandial

answer
after a meal
question
subcutaneous
answer
under the skin
question
sulfonylurea
answer
type of oral antidiabetic agent that stimulates insulin release
question
thiazolidinedione
answer
type of oral antidiabetic agent that reduces insulin resistance
question
type I diabetes mellitus
answer
disorder involving the complete destruction of the insulin producing beta cells in the pancreas and resulting in a lifelong need for daily insulin replacement therapy
question
type II diabetes mellitus
answer
disorder involving insulin resistance and impaired insulin secretion and resulting in the need for therapy that includes diet, exercise, oral medications and possibly inject-able medications.
question
What does insulin affect?
answer
utilization of glucose and the metabolism of proteins and fats.
question
most common forms of diabetes
answer
type I diabetes Type 2 diabetes gestational diabetes Diagnostic criteria for diabetes are the same for all types of diabetes mellitus
question
Hyperglycemia can be caused by diabetes mellitus as well as .....
answer
genetic disorders, disease of the pancreas, endocrinopathies, drugs, infections, and immune disorders.
question
When is diabetes diagnosed?
answer
patient has classic disease manifestations: Polydipsia (excessive thirst), polyuria (excessive urine output), sometimes with polyphagia (excessive hunger) and unexplained wt loss and a casual plasma glucose of 200 mg/dl or higher, or when a patient has a fasting plasma glucose level of 126 mg/dl or higher, or when a patient has a 2 hour postprandial plasma glucose of 200 mg/dl or higher during an oral glucose tolerance test.
question
form of diabetes that requires lifelong daily insulin replacement therapy either through subcutaneous injections or intravenous pump administration
answer
type 1 diabetes
question
Type I diabetes (formerly known as insulin dependent, or juvenile onset diabetes)
answer
involving the complete destruction of beta cells of the pancreas located in a regioincalle dthe islets of langerhans. beta cells produce insulin; therefore when all the beta cells are destroyed the body cant produce insulin to meet ongoing physiologic needs. Patients will typically develop polydipsia, polyphagia, polyuria and otherwise unexplained weight loss.
question
Type II diabetes (formerly known as non-insulin dependent or adult onset diabetes)
answer
complex metabolic condition with components of cellular insulin resistance and impaired insulin secretion. there is some beta cell function in the pancreas, so the patient does still produce some insulin. Can be managed through a combo of diet and exercise, oral and injectable meds, insulin.
question
patients start to exhibit early symptoms of type II diabetes
answer
considered to be pre-diabetic or having impaired glucose tolerance.
question
Development of type II diabetes is strongly associated with __________ and ________
answer
obesity, inactivity
question
what medication to be given to gestational diabetic mom
answer
metformin (glucophage) otherwise oral anti-diabetic meds are not typically prescribed for women who have gestational diabetes
question
acute complications of diabetes
answer
hyperglycemia hypoglycemia diabetic ketoacidosis (DKA) Hyperglycemi hypersomolar state (HHS) Infections
question
Chronic complications of diabetes
answer
Macrovascular complications (coronary artery disease, cerebrovascular accident and peripheral vascular disease) Microvascular complications (retinopathy, neuropathy and nephropathy)
question
Pregnancy related complications
answer
higher risk of perinatal infant mortality and congenital anomalies
question
exercise reduces blood ________ levels by promoting the uptake of glucose by active muscle cells and also making better use of insulin.
answer
glucose
question
Why would a patient with a blood glucose above 250 be advised not to exercise?
answer
because levels should be closer to the expected range when engaging in exercise. Exercising while hyperglycemic can further increase blood glucose levels d/t the release of glucagon, growth hormone and catecholamines, all which prompt the liver to release more glucose.
question
what to advise a patient who is exercising with diabetes
answer
have snacks and glucose replacement prior to and during exercise to prevent hypoglycemia. Monitor glucose prior to during and after the exercise if patients participate in an extended exercise.
question
Stress related to blood sugars
answer
stress has been shown to increase blood glucose levels. The release of hormones during stress in addition to changes in daily routine can raise glucose levels. watch promptly if under stress.
question
Insulin
answer
hormone secreted by beta cells of pancreas in response to glucose. This secretion is also prompted by amino acids, fatty acids and ketone bodies. Helps the body to utilize and store energy. Insufficient or absent insulin in the body decreases the metabolism of complex molecules which results in the classic clinical manifestations of uncontrolled diabetes
question
Rapid-acting and short acting insulin
answer
used in managing postprandial increases in blood glucose. This type of insulin should be used with an intermediate or long acting agent to ensure optimal blood glucose control. Rapid: Mostly given right before meals. short: administered before meals to control postprandial hyperglycemia, injected subq to ensure basal glycemic control and infused iv in emergency situations.
question
Intermediate acting insulin
answer
intended for once or twice a day dosing to control blood glucose levels. Delayed reaction makes it less effective for mealtime increases in blood glucose levels.
question
long acting insulin
answer
intended to provide basal glucose control. Typically once daily at the same time each day. Because the drug exerts a steady effect with no peak, it carries a risk of hypoglycemia.
question
combo/mixed insulin
answer
premixed combo of insulin are typically composed of intermediate acting and short acting insulin.
question
exenatide (byetta)
answer
incretin mimetic med available for treating type II diabetes when patients already taking metformin, a sulfonylurea or both and have not achieved adequate bs control. injectable med with some risk of hypoglycemia and delayed gastric emptying with weight loss.
question
how does exenatide (byettA) work?
answer
promotes better glucose control by slowing gastric emptying, stimulates glucose-dependent release of insulin, inhibits postprandial release of glucagon, and suppresses appetite. Adverse effects: hypoglycemia, nausea and pancreatits
question
pramlintide (symlin)
answer
amylin mimetic medication used to supplement the effects of insulin in patients who have type I or type II diabetes. Delays gastric emptying and suppressing glucagon secretion. Helps increase feelings of satiety, thus helping to reduce caloric intake. Recommended for supplementing mealtime insulin in patients with type I or type II diabetes who cannot achieve glycemic control.
question
overall goals of diabetes management
answer
achieving metabolic control and optimal blood lipid levels, attaining and maintaining body wt within an acceptable range, avoiding acute complications and improving overall health through optimal nutrition
question
goal of nutrition planning of patient with diabetes
answer
planning includes controlling caloric intake while balancing and meeting nutritional needs to regulate not just glucose levels but also lipid levels and blood pressure
question
MNT
answer
medical nutritional therapy, a nutritional plan geard not only to prevent and manage diabetes but also an overall component of a healthy lifestyle. Helps patients to learn to incorporate good dietary choices into everyday life to promote healthful wt loss as needed and to maintain glucose control. *life long*
question
diabetic diet %ages
answer
45-65% of cal from CARBS 15-20% of cal from PROTEIN remainder from fat
question
how to manage hypoglycemic patients
answer
when suspected or determined based on b.s level. give patient (if alert and oriented and able to swallow) 15-20 g of rapid acting concentrated carbohydrate. such as 4-6 oz fruit juice, 8 ounces of skim milk, 1 tbsp of honey or 3-5 commercially prepared glucose tablets. retest in 15" (if still low below 70-75 retreat and re check in 15") make sure snack contains protein and carbohydrate ex: milk or cheese and crackers if patient's meal is longer than an hour away.
question
patients with blood sugars above 250 should or should not exercise?
answer
Should NOT. patient's should refrain from exercise until their levels are closer to the expected range. This is because exercising when hyperglycemic can further increase blood glucose levels d/t the release of glucagon, growth hormone and catecholamines. All of which prompt the liver to release more glucose. Patients should be informed that if they have diabetes use proper footwear, avoid exercise in extreme heat or cold and inspect their feet after exercise.
question
when should patients take snacks in regards to exercise?
answer
patients should have snacks and glucose replacement prior to and during exercise to prevent hypoglycemia.
question
When are oral hypoglycemics prescribed for patients who have type 2 diabetes?
answer
when they cannot achieve good glycemic control with diet and exercise alone. these meds should not be prescribed unless the patient has diet and exercise planning in place.
question
Treatment of type 2 diabetes is a five step process involving escalation of tx as the severity of insulin resistance increases.
answer
1. implement diet and exercise therapy 2. initiate therapy with one oral hypoglycemic. Medication choice depends on body composition and severity of hyperglycemia 3. treat with 2 oral hypoglycemics, preferably from different classes, to maximize their benefits. 4. treat with 3 oral hypoglycemics or with 1 oral hypoglycemic plus insulin 5. treat with insulin alone
question
types of oral hypoglycemics
answer
sulfonylureas meglitinides (glinides) biguanides thiazolidinedioines (glitzones) alpha glucosidase inhibitors gliptins combo therapies
question
sulfonylureas
answer
(glyburide *micronase*, glipizide *glucotrol* and glimepiride *amaryl*) work by increasing insulin secretion by beta cells of pancreas.
question
meglitinides (glinides)
answer
(Repaglinide *prandin*, nateglinide *starlix*) increase insulin secretion by beta cells of pancreas. These medications target postprandial glycemia and are less likely to cause hypoglycemia than sulfonylureas are.
question
biguanides
answer
(Metformin *glucophage*) work by reducing hepatic glucose production while increasing insulin action on muscle glucose uptake. These medications can cause gi side effects, vitamin B12 and folic acid deficiencies and lactic acidosis. They are withheld before radiographic contrast media.
question
thiazolidinediones (glitazones)
answer
(pioglitazone *actos*) Increase the cellular response to insulin by decreasing insulin resistance. This results in increased glucose uptake and decreased glucose production. only available in restricted access and well tolerated but may reduce the effectiveness of oral contraceptives and should be used cautiously in patients with heart failure.
question
alpha glucosidase inhibitors
answer
(acarbose *precose* and miglitol *glyset*)delay carbohydrate digestion. Advantages are that it targets postprandial glucose and their effects are not systemic. Do not depend on the presence of insulin at all but it does cause GI side effects .
question
Gliptins
answer
(Sitagliptin *januvia*) Work by augmenting naturally occurring incretin hormones, which promote the release of insulin and decrease the secretion of glucagon. The result is reduced fasting and postprandial glucose levels.
question
Combination therapies
answer
there are some oral antidiabetic medications that are combination products developed to make it easier for patients to adhere to their medication regimens when more than one medication is needed examples include metformin and glyburide (glucovance), metformin and glipizide (metaglip) and metformin and rosiglitazone (avandamet).
question
foundation for diabetes management
answer
nutrition, meal planning and weight control are foundations of diabetes management, with a goal of maintaining blood glucose and lipid levels as close to normal as possible.
question
Risk factors for diabetes mellitus ?
answer
family hx, race/ethnicity, advancing age over 45, hx of impaired fasting glucose or impaired glucose tolerance, hypertension (140/90) HDL below 35 mg/dl, triglyceride levels 250 mg/dl and above, hz of gestational diabetes and delivery of infants over 9 lbs
question
what does glycosylated hemoglobin (HbA1c) mean for patients with diabetes?
answer
it is a blood test that provides a long term measure of glucose control. This test measures the glucose attached to a hemoglobin molecule for the life of a RBC (120 days) to provide an average blood glucose reading for a period of 2-3 months. Unlike the fasting blood sugar, HbA1c results are not altered by eating habits the day before the test.
question
mild hypoglycemia
answer
sweating, tremors, tachycardia, palpitations, anxiety and hunger
question
severe hypoglycemia
answer
disorientation, seizures, difficulty arousing from sleep, and loss of consciousness. whenever suspecting hypoglycemia immediately check patient's blood glucose level.
question
how do you treat simple hypoglycemia in an alert and oriented patient who has diabetes?
answer
assuming they are able to swallow, give him 15-20 grams of rapid acting concentrated carbohydrate (4-6 ounces of fruit juice, 8 oz skim milk, 1 tbsp of honey, 3-4 commercial prepared glucose tablets) retest in 15 minutes. If blood glucose is still below 70-75 mg/dl retreat and check again in 15 minutes. Once clinical manifestations subside and glucose stabilizes, make sure patient consumes snack that contains protein and carbohydrate (milk, cheese and crackers) if patients next meal is longer than an hour away
question
blood pressure and cholesterol goals for patients who have diabetes?
answer
ADA a BP below 130/80 cholesterol LDL should be below 100 mg/dl triglycerides below 150 mg/dl HDL above 40 mg/dl
question
Macrovascular accidents
answer
cerebrovascular accident, myocardial infarction, atherosclerosis and peripheral arterial disease
question
self administration of insulin using a pre filled pen administration system.
answer
store unopened insulin cartridges in a refrigerator to reserve their therapeutic activity. Check expiration date Once pierced, a cartridge can stay at room temp and the pen may be used until empty for up to 30 days. New needle each time
question
why do you rotate sites for insulin injections?
answer
insulin is a hormone, it can cause excess growth of fat beneath the skin, called lipodystrophy. This reduces the absorption of insulin thus reducing its effect. Space insulin injection sites within the same general locale (such as abdomen or thigh 1 ich apart and do not use the same site more than once per month.
question
Does stress really alter blood glucose levels in patients who have diabetes?
answer
Yes. Illness, surgery and infections can cause a release in hormones that increase blood glucose levels. During periods of emotional stress, patients are more likely to change their routines for meals, exercise and medication. Alterations in routine can lead to both hyperglycemia and hypolgycemia.
question
a nurse instructing a patient about using an insulin pump should explain that the risk of diabetic ketoacidosis *DKA* increases with the use of a pump because: a. the pump must be removed for bathing b. insulin is injected continuously c. the pump uses intermediate acting insulin d. the tubing could become occluded
answer
d. the tubing could become occluded
question
_______ acting insulin, such as insulin glargine (lantus) is intended to provide basal glucose control. The dosage is typically once daily at the same time each day, usually with the evening meal.
answer
long acting insulin
question
What can patient do to reduce injection pain?
answer
inject room temperature insulin to reduce pain instead of injecting cold insulin.
question
120 mg/dl is an abnormal result for which type? a. casual random blood glucose measurement b. fasting blood glucose measurement c. glycosylated hemoglobin measurement d. 2- hour measurement for an oral glucose tolerance test.
answer
b. fasting blood glucose level of 120 is abnormal normal range for fasting blood glucose is generally between 70-105
question
a nurse is teaching a patient with type 1 diabetes mellitus who is beginning a complex regimen of glycemic control about the properties and actions of the various types of insulin. The nurse should explain that the type of insulin that has an onset of 60-120 minutes, peaks in 6 to 14 hours, and has a duration of 16-24 hours is a. regular insulin (humulin R, Novolin R) b. insulin glargine (lantus) c. neutral protamine hagedorn (NPH) insulin d. insulin detemir (levemir)
answer
c. neutral proatmine hagedorn (NPH) insulin has an onset of 60-120 minutes, peaks in about 6-14 hours and has a duration of 16-24 hours
question
A nurse is teaching a diabetic support group about the cause of type I diabetes.The teaching is determined to be effective when the group is able to attribute which of the following factors as a cause of type 1 diabetes? a. rare ketosis b. presence of autoantibodies against islet cells c. altered glucose metabolism d. obesity
answer
b. presence of autoantibodies against islet cells
question
A nurse is preparing to d/c a patient with CAD and HTN. Who is at risk for type II diabetes. Which of the following info is important to include in D/C teaching? a. how to self inject insulin b. how to control blood glucose through lifestyle modifications diet/exercise c. how to recognize signs of diabetic ketoacidosis (DKA) d. how to monitor ketones daily.
answer
b. how to control through lifestyle mods.
question
Nurse is administering lispro (humalog). Based on the onset of action, how soon should the nurse administer the injection prior to breakfast? a. 1-2 hours b. 30-40 minutes c. 10-15 minutes d. 3 hours
answer
c. 10-15 minutes
question
Which of the following should be included in the teaching plan for a patient receiving glargine (Lantus), "peakless" basal insulin? a. do not mix with other insulins b. administer the total daily dosage in 2 doses c. draw up the drug 1st, then add regular insulin d. it is rapidly absorbed, has a fast onset of action
answer
a. do not mix with other insulins.
question
A patient with type 1 diabetes is being taught self injection of insulin. Which facts should nurse teach about site rotation? a. use all available injection sites within one area b. choose a different site at random for each injection c. rotate sites from area to area every other day
answer
a. use all available injection sites within one area. To prevent localized changes in fatty tissues, promote insulin consistency of absorption.
question
Which of the factors is the focus of nutrition intervention for patients with type 2 diabetes? a. weight loss b. carb intake
answer
a. weight loss
question
a patient admitted with DKA. The Dr writes all of the following orders. Which order should the nurse implement first? a. administer regular insulin 30 U IV push. b. start an infusion of regular insulin at 50 U/hr c. administer sodium bicarbonate 50 mEq IV push d. Infuse 0.9% normal saline sol 1 L/hr for 2 hours
answer
d. infuse 0.9% normal saline solution 1 L/hr for 2 hours
question
A patient newly diagnosed with type 1 diabetes has an unusual increase in blood glucose from bedtime to morning. The Dr suspects the patient is experiencing insulin waning. based on this diagnosis, the nurse will expect which of the following changes to the patients medication regimen? a. decrease evening bedtime dose of intermediate acting insulin and administering a bedtime snack b. changing the time of injection of evening intermediate acting insulin from dinnertime to bedtime c. administering a dose of intermediate acting insulin before the evening meal
answer
c. administering a dose of intermediate acting insulin before the evening meal. Insulin waning is a progressive rise in blood glucose from bedtime to morning. Tx includes increasing the evening (predinner or bedtime) dose of intermediate acting or long acting insulin or initiating a dose of insulin before the evening meal if that is not already part of the treatment regimen.
question
A patient receives a daily injection of glargine (lantus) insulin at 0700. When should nurse monitor pt for hypoglycemic reaction?
answer
No peak action time because this insulin has no peak action and does not cause a hypoglycemic reaction
question
When mixing insulin, the ____ insulin is drawn up into the syringe first.
answer
regular
question
A nurse is teaching a patient recovering from DKA about managment of sick days. The pt asks nurse why its important to monitor urine for ketones. Which is best nurse response? a. excess glucose in the blood is metabolized by the liver and turned into ketones, which are an acid. b. ketones accumulate in the blood and urine when fat breaks down. Ketones signal a deficiency of insulin that will cause the body to start to breakdown stored fat for energy
answer
b.
question
Glycosylated hemoglobin level
answer
blood test that reflects average blood glucose period of approximately 2-3 months. When blood glucose levels are elevated, glucose molecules attach to hgb in RBC's. The longer the amount of glucose in the blood remains above normal, the more glucose binds to hgb and the higher the glycated hemoglobin level becomes
question
What assessment is helpful in determining/confirming the diagnosis of DKA?
answer
assessing breath odor. DKA is commonly preceded by a day or more of polyuria, polydipsia, N/V and fatigue with eventual stupor and coma if not treated. The breath has characteristic fruity odor d/t presence of ketoacids.
question
Hemoglobin A1C "glycolosated hemoglobin"
answer
needs to be checked Q 6 months Could be Q 3 months for patients NOT meeting goal. Indicates how blood sugar is controlled over 120 days results >8%= poor diabetic control. GOAL= less than 7%
question
if A1C 8%
answer
blood sugar is consistent basis is average 205 each day. we want it down to 7% or less.
question
if A1C 7%
answer
blood sugar is averaging 170 on a daily basis.
question
fif A1C 6%
answer
blood sugar is averaging 135 each day
question
Screening for kidney disease involves
answer
Glomerular filtration rate: calculated based on serum creatinine, age, race and gender. Creatinine levels
question
Further assessments of kidneys include
answer
screening for albumin in the urine Screening for protein in the urine (using dipstick) Screening for microalbumin very important for kidney function *ANNUALLY*
question
Lipid levels
answer
LDL below 100 mg/dl HDL greater than 40 mg/dl Triglycerides less than 150 mg/dl total cholesterol lower than 200 or 180 **Lipid levels done YEARLY**
question
Blood pressure
answer
measured at each office visit for q 10-mm HG reduction in systolic pressure the risk can be REDUCED by 12% *BP needs to be lower in diabetic patients* 130/80 risk for cardiovascular disease or adverse cardiac reaction
question
Eye exam
answer
pupils need to be dilated in order to see vessels in the back of the eye. retinopathy takes about 5 years to develop after the onset of hyperglycemia. **Annual ophthalmologic examination**
question
Dental exam
answer
diabetics have TWICE the risk for peridontal disease Severe periodontitis includes loss of gums to teeth of 5 mm or greater, tooth loss **Annual dental exam is recommended**
question
Foot exam
answer
Neuropathy causes damage to the ANS which results inability to sweat... leading to dry and cracked skin. Moisturize with petroleum jelly or unscented cream.
question
Why is foot exam important?
answer
loss of sensation to the feet. Need to inspect feet DAILY. if the patient cannot see his or her feet need to have a friend or family inspect. floating thermometers for tub Comprehensive exam annually.
question
What questions to ask patient in regards to foot exams
answer
neuropathic symptoms? numbness, tingling, pain down the foot? Previous ulcers? PVD? Smoker? smoking adds to the problem of circulation connection. Advise to wear well-fit shoes.
question
Immunizations recommendations for diabetics
answer
pneumonia influenza
question
Types of testing for diabetics
answer
fasting blood glucose Glucose tolerance test
question
Types of testing: Fasting blood glucose levels
answer
less than 100 mg/dl ... will rise 1 mg/dL per decade of age. Diabetic = 126 mg/dL or greater at least 2 occasions
question
Types of testing: Glucose tolerance test
answer
less than 140 mg/dL Diabetics readings= Greater than 140 mg/dL, if greater than 200 mg/dL indicates provisional diagnosis of diabetes
question
what do you want for fasting blood glucose?
answer
less than 100 on fasting. Diabetics= 126 or greater on at least 2 occasions
question
oral medication for diabetes management
answer
1st generation sulfonylureas Meglitinide Biguanides Thiazolidinediones
question
1st generation Sulfonylureas
answer
used when remaining beta cell functioning. Stimulate insulin secretion and increase sensitivity problems because of weight gain seldom used.
question
2nd generation slfonylureas
answer
*Glipizide, glyburide, amaryl* increase insulin secretion Must always assess hypoglycemia. taken 30 minutes before meals
question
Meglitinide
answer
*Prandin, Starlix* triggers insulin secretion. very much used in conjunction with meal time coordination. Administer around meal time because increase insulin that is released for meal time related insulin secretions. Prandin: VERY rapid onset given before meals Starlix: 20 minutes before meals. (no meal= skipped)
question
Biguanides
answer
*metformin* opposite of other meds (does NOT increase insulin secretion) Decreases liver glucose production and improves insulin receptor sensitivity
question
important information regarding metformin
answer
diarrhea will happen when start taking. be very careful using with anyone with Renal impairment/BUN, creatinine issues. Make sure medication is held 48 hours before and after any contrast material or surgical procedure requiring anesthetic
question
thiazolidinediones (TZD's)
answer
*stimulates enzyme that regulates glucose and lipid metabolism* improve insulin sensitivity and reduce liver production of glucose Improve the insulin action on muscle, fat, and lipid metabolism.
question
pos and negs of thiazolidinediones
answer
positives: decrease lipid levels. negatives: Major side effects; increased adipose tissue (fat tissue) and fluid retention.
question
important teachings regarding TZD's for patients who are diabetic
answer
report N/V, abdominal pain, fatigue, anorexia or dark urine.
question
TZD: Avandi
answer
bad rep. questionable to be taken off the market. huge risk in heart related death, bone fractures and macular edema. NASTY side effects
question
TZD: Actos
answer
TZD that is seen more.
question
Blood glucose monitoring
answer
instruct on good hand washing ensure meter is accurate alternate site testing (pts with a hx of hypoglycemia unawareness shouldn't test at alternative sites)
question
Nutrition for diabetics
answer
nutritionalist develops a meal plan depending on usual food intake, wt management goals, lipid and blood glucose.
question
protein % of daily calories for diabetics
answer
15-20 %
question
carbohydrate % of daily calories
answer
45-65% minimum of 130 g/day
question
fat and cholesterol restriction for diabetics ____% of daily calories
answer
7%
question
________ improves carbohydrate metabolism and lowers cholesterol. Can reduce abdominal cramping, loose stools and flatulence
answer
Fiber
question
Careful with increasing _____ too quickly b/c can cause hypoglycemia
answer
Fiber



