Epidural and Spinal Anesthesia – Flashcards
Unlock all answers in this set
Unlock answersquestion
Pharmacokinetics of neuraxial anesthesia: Epidural and subarachnoid
answer
A.) Spinal: -Mainly by BARICITY and patient POSITIONING -Drug dose relatively unimportant for block height -Volume/concentration does not affect block height if dose kept constant -Age, BMI, height not predictive of block -ONSET: Lidocaine/mepivicaine >> tetracaine/bupivicaine -DURATION: drug & dose, block height, adrenergic agonists (tetracaine responds best) B.) Epidural -VOLUME important independent of drug dose -PATIENT CHARACTERISTICS also important -Age-greater spread in older -Height/weight extremes -ONSET: DEPENDS ON DOSE -DURATION: Increases with dose, adrenergic agonists -Etidocaine: separation in intensity and duration of sensory/motor block
question
Factors influencing onset, duration, termination of action
answer
-Differential blockade: size of fiber types, myelinated vs. not, length of nerve fiber, concentration changes based on distance, etc.
question
Factors that influence level of a spinal block
answer
-Baricity of LA -Position of patient (during and immediately after) -Drug dosage -Site of injection Less important: -Age (decreases CSF volume) CSF - volume inversely correlates with dermatomal spread of anesthesia Curvature of spine Drug volume Intraabdominal pressure - ex. pregnancy increases pressure, engorges epidural veins, decreases CSF volume, so greater spread of dermatomes Needle direction Patient height Pregnancy General: larger drug dose and more cephalic injection = more cephalad spread
question
Systemic toxicity -Signs/symptoms -Risk -Prevention -Treatment
answer
-CNS - perioral numbness, tinnitus, lightheadedness, convulsions -CVS - malignant ventricular arrhythmias (bupivicaine most) -More likely if "full epidural dose" injected intrathecally or intravascularly -Test and incremental dosing decreases risk (through needle or catheter) -Intralipid 20%, 1.5ml/kg
question
Test dose
answer
-Detect both subarachnoid and intravascular injection -Combines LA and epinephrine -3ml 1.5% lido with 1:200,000 epinephrine -This much lidocaine if it were injected intrathecally would produce spinal anesthesia rapidly and detectably -HR increase with epinephrine if intravascularly: 20% or more -SBP > 20 mmHg increase -With or without hypertension too -False positives: uterine contraction - pain causes coincidental increased HR -False negatives: bradycardia and exaggerated HTN B-blocked patients -Aspirating prior to injection is not enough to test -If aspirating negative, then can inject 5ml increments - mild effects of intravascular injection can be tested, but not complete seizure or cardiovascular collapse
question
Easy anatomy landmarks
answer
C7 - first prominent spinous process down neck T4 - tip of scapula in elevated position T7 - tip of scapula in neutral position L4/5 or L4 body: line between iliac crests
question
Topographical anatomy for regional: neck spine (vertebra prominens, Chassaignac's tubercle, vertebral levels, caudal space) Nerves and bones
answer
-7 cervical, 12 thoracic, 5 lumbar vertebrae, sacrum fusion of 5 vertebrae -Paired spinal nerves exit CNS at each level -C1: atlas - lacks body, atypical articulating surfaces -C2: axis - atypical articulating surfaces -Thoracic vertebrae - articulate with rib -Lumbar vertebrae - large anterior cylindrical vertebral body -Articulate at facet joints (4 for each vertebrae) --> pedicles at top/bottom forintervertebral foramina --> spinal nerves go through this -C spine - first palpable process = C2 -Chassaignac's tubercle = carotid tubercle = anterior tubercle of transverse process of C6. Separates carotid artery from vertebral artery. Compress this, compresses carotid artery. Used as landmark for supraclavicular approach for brachial plexus and for cervical plexus -Vertebra prominens = C7 -T7 usually at same level as inferior scapulae (with arms at side) -Tuffier's line = line drawn between both iliac crests, either at body of L4 or L4-L5 interspace -S2 foramina = line connecting PSIS -Sacral hiatus = depression just above or between gluteal clefts, above coccyx
question
Anatomy: caudal space -Contraindications
answer
-Sacrum still has intervertebral foramina, anterior and posterior -Sacral hiatus: laminae of S5 and part of S4 normally don't fuse, leaving caudal opening to spinal canal -Space limited by sacral cornu -Covered by sacrococcygeal ligament -Large volume of LA given to compensate for consistent leakage to perineural space Contraindications -Major malformations of the sacrum -Myelomeningocele -Meningitis
question
Caudal epidural
answer
-Peds commonly combined with GA for procedures below diaphragm (urogenital, rectal, inguinal, lower extremity) -Peds usually done after induction GA -Adults - anorectal surgery -Go through sacrococcygeal ligament, covering sacral hiatus -Sacral hiatus made by unfused S4 and S5 laminae -Hiatus is groove/notch above coccyx between 2 body prominences (sacral cornua) -Triangle made between PSIS and sacral hiatus -Lateral or prone position, 1-2 hips flexed -Needle/catheter advanced at 45 degrees until pierces sacrococcygeal ligament, then angle of needle flattened and advanced -Test dose or incrimental injections after aspiration -Tachycardia or increasing size of T waves on EKG = intravascular injection
question
Transforaminal approach
answer
-Typically for epidural steroid injections -inject medication around specific nerve root exiting spinal canal
question
Caudal drug doses
answer
-0.5-1.0 ml/kg bupivicaine or ropivicaine 0.125-0.25%, with or without epinephrine -Opioids optional: 50-70 mcg/kg morphine (not for outpatients - delayed risk respiratory depression) -Clonidine -Block lasts for hours post-operatively, can usually urinate within 8 hours so can be used for outpatient 0.5 ml/kg - high sacral 1.0 ml/kg - high lumbar 1.5 ml/kg - mid thoracic
question
Meninges/spaces (epidural, subdural & subarachnoid spaces)
answer
Meninges: External to internal Dura mater: -denser, thicker, most external -Ends at S2 adults, S3 children -Lateral extension along nerve roots -Acellular, random fibers Arachnoid mater: -closely adherent to dura mater -tight junction cells -Resistant to drug infusion Pia mater: -closely adhered to spina cord. -Terminates as filum terminale (penetrates dura and attaches to coccyx periosteum) -Fenestrated, spinal cord exposed to CSF directly Spaces: External to internal Epidural space: -between dura and ligamentum flavum Spinal subdural space: -POTENTIAL space, between dura and arachnoid membranes -Explains failed spinals, "high spinal" after epidural without CSF aspirate Subarachnoid space: -CSF, spinal nerve roots -between pia and arachnoid mater (subarachnoid space)
question
Variations in vertebral configurations
answer
-Spinous processes C and L spine nearly horizontal (only slight cephalic angle) -Thoracic spine slant in caudal direction, overlap significantly (needle angled very cephalic) -Most dependent region T4-T8 in supine position, so hyperbaric solutions will usually stay at or below T4 in this position
question
Spinal nerves (level of exit, covering, sensory distribution)
answer
-C: nerves arise above respective vertebrae (8 total C spinal nerves) -T1: nerves start to exit below respective levels -Dural sheath covers spinal nerves even after they exit spinal canal (blocks near intervertebral foramen have risk of subdural or subarachnoid injection)
question
Indications
answer
-Lower abdominal -Inguinal -Urogenital -Rectal -Lower extremity surgery -Lumbar spine surgery - spinal
question
Contraindications
answer
Absolute: -Patient refusal -Bleeding diathesis -Severe hypovolemia -Elevated ICP (particularly with intracranial mass) -Infection at site of injection -Severe AS or MS Relative contraindications: -Stenotic valvular heart lesions (Lange mentions in 2 different contexts) -Uncooperative patient -Demyelinating lesions -Severe LV outflow obstruction (HOCM) -Severe spinal deformity -Can be safely performed in valvular heart disease with close monitoring Controversial: -Prior back surgery at site -Complicated surgery -Prolonged operation -Major blood loss -Maneuvers that compromise respiration
question
Techniques
answer
-Volume load 10-20 ml/kg IVF before initiation of block to prevent hypotension -Left uterine displacement in pregnancy (last trimester) A.) Midline approach -Spine palpated, plane of back perpendicular to flow -Sterile prep -Skin wheel, slightly cephalic angle -Through supraspinous/intraspinous ligaments -If bone contacted superficially, most likely inferior spinous process -Bone contacted deeper - most likely hitting upper spinous process, or lateral/lamina -Ligamentum flavum: if penetrates, sudden loss of resistance, enters epidural space B.) Paramedian Approach: -May be routinely used for thoracic -Skin wheel 2 cm lateral to inferior superior spinous process of desired level -Needle with little resistance as it passes through (does not go through interspinous ligaments, supraspinous) -Directed/advanced 10-25 degree angle toward midline -Bone shallow - medial part of lower lamina most likely -Bone deep - lateral part of lower lamina, redirect crannied, toward midline -Lamina is landmark C.) Taylor Approach: -variant of paramedian -L5-S1 interspace -needle 1 cm medial, 1 cm inferior to PSIS (posterior superior iliac spine) -Directed cephalad and toward midline Spinal approaches: -Midline, paramedian -Lateral decub, sitting, prone -2 pops = ligamentum flavum, then dura -Withdraw stylet, CSF flowing. Small gauge needles may need to aspirate -Persistent parasthesias/pain - withdraw and redirect needle
question
Specific for epidural techniques: determining passage past ligamentum flavum
answer
A.) Loss of resistance -Stylet removed, syringe with air or saline used when resistance felt at interspinous ligament -advanced mm by mm -Sudden loss of resistance when enter epidural space, and injection is easy B.) Hanging drop -Interspinous ligament entered, stylet removed -Needle hub filled with solution so drop hangs from outside opening -When needle enters epidural space, negative pressure created and drop is sucked up into it -If needle gets plugged, drop will not be sucked in and can get inadvertent dural puncture -Possibly more preferred for paramedic approach and cervical epidurals
question
Comparison of techniques
answer
-Paramedian if block is difficult (epidural or spinal) -Paramedian in patients who cannot be positioned easily (spinal disease like arthritis, kyphoscoliosis, prior spine surgery)
question
Sites of action
answer
-Principal site of action of spinal and epidural believed to be nerve roots -Spinal: most dependent region T4-T8 in supine position, so hyperbaric solutions will usually stay at or below T4 in this position
question
Premedication
answer
-Anxiolysis, but avoid heavy sedation -ex.) midazolam 1.5 mg, fentanyl 75 ug -GI premedication for aspiration pox if indicated in case of conversion to GA
question
Patient positioning
answer
1.) Sitting -Easier to palpate midline, esp obese -Elbows on thighs, table, or hugging pillow -Flex spine - arch back like mad cat -Keeping in this position, spinal "saddle block" in 3-5 minutes --> only lower lumbar/sacral nerves blocked 2.) Lateral decubitus -Lie on side with knees flexed and pulled high against abdomen or chest -"Fetal position" -Assistant can help hold 3.) Jackknife (Buie's) -Anorectal procedures -Isobaric or hypobaric solution -Block done in same position as operative procedure -Disadvantage: CSF will not freely flow through needle, need to confirm by aspiration -Prone when fluoro guidance needed
question
Equipment: spinals
answer
-All equipment and drugs needed for intubation, resuscitation, general anesthesia immediately available -May need supplemental O2 NC or FM Spinal needles: -Removeable stylet that occludes lumen -Shap cutting tipped -Blunt-tipped (pencil-point) - decreased incidence of post-dural puncture headache ex.) -22-29 G (smaller to decrease risk PDPH) -Whitacre - pencil-point, side injection port -Sprotte - pencil-point, side injection, long opening - more CSF flow, but can lead to failed block if opening is half in subarachnoid, half not past dura -Quincke or Greene: beveled edge with cutting edge Spinal catheters: -Larger epidural catheters used if accidentally get a spinal puncture during epidural test
question
Equipment: epidural
answer
Needles: -16-19 gauge usually -3-3.5 inches long -Blunt bevel, 15-30 degrees curve at tip -Tuohy needle most common - blunt curved tip in theory pushes dura away after passing through ligamentum flavum -Tuohy and Hustead: curved tip - catheter placement -Crawford - straight needles without curved tip - greater incidence dural puncture, but let you pass through epidural catheter - lumbar drain placement Catheters: -19-20 gauge usually -curved tip needle, bevel directed either up or down -Catheter advanced 2-6 cm into epidural space -shorter the distance, more likely to get dislodged -further catheter advanced, more likely to get unilateral block -May tunnel catheter under skin if remains in for 1 week or prolonged period of time -Single port at distal end, or multiple side ports close to the tip -Some styleted -Some wire-reinforced to resist kinking -Spiral or spring-tip: fewer, less intense parasthesias, ?less incidence intravascular insertion Warning: anti-septics are neurotoxic, avoid contamination of needles/LA
question
Epidural drugs
answer
-Short to intermediate duration: chlorprocaine, lidorcaine, mepivicaine -Longer acting: bupivicaine, levobupivicaine, ropivicaine -Preservative-free only -Initial dose given, then repeated doses possible with 1/3-1/2 of initial dose usually -Chlorprocaine may interfere with analgesia of opioids added epidurally -Previous chlorprocaine preserved with bisulfite and EDTA - risk of caudal equine syndrome -bisulfite alone risk of neurotoxicity, EDTA alone severe back pain -Current chlorprocaine no preservatives -Increase pH of solution increases % of LA in uncharged form, able to penetrate lipid layers (sodium bicarb 1mEq/10mL (just don't add to bupivicaine b/c precipitates above pH 6.8) Bupiviciane: -0.5% is surgical anesthesthesia (0.75% too high, cardiac arrest) -Low-dose 0.0625% with opioid common for labor and postop pain
question
Monitoring
answer
-Minimum: BP, pulse ox - OB -Surgical blocks: same as that in general anesthesia -Epidurals for chronic pain (little or no local injected): do not require continuous monitoring
question
Epidural: cervical, thoracic, lumbar, caudal, transforaminal
answer
-Epidural: loss of resistance as needle goes through ligamentum flavum -Slower onset (10-20 min) and not as dense as spinal blockade -Larger quantity of LA needed -C/S performed under spinal or epidural, both allow mother to remain awake -Sacral epidural block = caudal injection -Can be single-shot or catheter for intermittent boluses/continuous infusion -Motor block can be none or complete, so may have a more pronounced differential block -Dilute concentrations LA with opioid - may give analgesia without motor block -Segmental block: well-defined band of anesthesia at certain nerve roots - above and below are unblocked. Good for thoracic for upper andominal coverage(spares cervical and lumbar) Lumbar - Any procedure below diaphragm -Thoracic - more technically difficult because of angulation of spinous processes, higher risk of spinal cord injury with accidental dural puncture. -Thoracic - single short or catheter for chronic pain -Cervical - performed with patient sitting, neck flexed, midline approach. Used for pain management usually.
question
Epidural: Factors influencing level of block
answer
-1-2 mL per segment generally -T4 level from L4 injection: 12-24mL -Dose decreases with age -Patient height (i.e. shorter patients may only need 1 mL per level) -Partially affected by gravity -Additives (opioids) affect quality of block more than duration -Epi prolongs duration of lidocaine, mepiviciane, chlorprocaine the most. Delays vascular/systemic absorption Failed blocks: -unilateral block: withdraw catheter 1-2 cm, reinject with patient turned to unblocked side down -Sacral sparing: large size of L5, S1, S2 nerve roots, delayed penetration of nerve roots -Segmental sparing - may be from septations in epidural space -Peritoneal stretch - may be from vagal visceral pain - amenable to IV opioids
question
Contents of epidural space:
answer
-Nerve roots -fatty connective tissue -Lymphatics -Venous plexuses (Baton's) -Septae/connective tissue bands, possibly explaining rare one-sided block
question
Spinal
answer
-Spinal: needle advanced through epidural space and penetrates dura-subarachnoid membranes --> signaled by CSF free-flow -Lumbar spinal: below L1 adults, below L3 in child -Same technique as epidural, except when penetrate ligamentum flavum and feel loss of resistance, advance through dura-subarachnoid membranes, free-flowing CSF -Usually all-or nothing, single shot injection
question
Local anesthetic agents: Spinal
answer
-Vasoconstrictors and opioids/clonidine added - enhance quality or prolong duration -Preservative free solutions Most common: Hyperbaric bupivicaine and tetracaine -Onset slow - 5-10 minutes -Prolonged duration - 90-120 minutes -Tetracaine most consistent motor blockade compared to bupi, and tetracaine more prolonged by epinephrine Lidocaine/procaine -Rapid onset 3-5 minutes -Short duration - 60-90 minutes -Only modestly prolonged by vasoconstrictors -Avoid repeat lidocaine doses after "failed" block - higher risk TNS and caudal equine syndrome
question
Combined spinal-epidural
answer
-Subarachnoid block and epidural catheter placed simultaneously -Rapid onset, dense block -Catheter cannot be tested for subarachnoid placement
question
Complicatons: precipitating factors, prevention, therapy
answer
-Range: back soreness to debilitating neurologic complications to death Epidural hematoma: 1/150,000
question
Implications of anticoagulants and platelet inhibitors, ASRA guidelines
answer
-Warfarin: normal INR and PT documented prior to block -NSAIDs/Aspirin 81 mg, SC Heparin ppx: OK -Ticlopidine: 2 weeks -Plavix: 1 week -Eptifibatide (Integrilin): 8 hr -LMWH: -Preop: wait 10-12 hours for ppx doses, 25 hours for therapeutic doses -Postop: 6-8 hours for daily dosing, 24 hours for BID -Indwelling catheter cannot be removed until 10-12 hours after last dose and next dose only after 2 hours
question
Differential blockade
answer
Sympathetic (temperature): 2 segments or more cephalic than sensory Sensory (pain, light touch): several segments cephalic more than motor blockade
question
Spinal anatomy: bones picture
answer
...
question
Epidural: midline approach picture
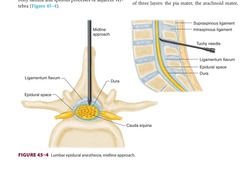
answer
...
question
Blood supply spinal cord
answer
-Single anterior artery - starts at vertebral artery base of skull -Paired posterior spinal arteries - arise from PICA -Additional blood flow: intercostal arteries, lumbar arteries (abdomen) -Artery of Ademkiewicz - large radicular artery, unilateral supply, usually L side, major blood supply of anterior, lower 2/3 of spinal cord
question
Vagus nerve
answer
Not blocked by neuraxial anesthesia
question
Vasomotor tone levels
answer
T5-L1 mainly (arterial and venous smooth muscle)
question
Sympathetic cardioaccelerator fibers
answer
T1-T4 -Profound hypotension, bradycardia with these fibers and vasomotor tone
question
Procedures and block height needed -Perianal/perirectal -Low ext/Hip/TURP/Vaginal -Hernia/Pelvic/Appy -C-section/Abdomen
answer
-L1-2 -T10 -T6-8 -T4-6 Lower extremity procedures: can use isobaric/hypobaric because will not lie on that limb (limb will be non-dependent)
question
Spinal subarachoid space -Adults -Children
answer
Foramen magnum to: S2 - adults S3 - children
question
CSF specific gravity -Addition of additives to LAs and baricity
answer
1.003-1.008 CSF Hypobaric 1.0015 with dextrose Isobaric = regularly dispensed bottles of LA
question
Specific gravities of LA's Bupivicaine 0.5% plain Bupi 0.5% in dextrose Lidocaine 2% plain Lido 5% in dextrose Procaine 10% plain Pricaone 2.5% in water Tetracaine 0.5% in water Tetracaine 0.5% in D5W
answer
Bupi pain = 1.0227-1.0278 Bupi dextrose = 0.9990 - 1.0058 Lido plain = 1.0004-1.0066 Lido in dextrose = 1.0262-1.0333 Procaine plain = 1.0104 Procaine in water = 0.9983 Tetracaine in water = 0.9977 - 0.9997 Tetracaine in D5W = 1.0133 - 1.0203 *addition of glucose - makes hyperbaric *addition of sterile water or fentanyl - makes hypobaric
question
Complications: Excessive response to appropriately placed drug
answer
A.) High neural block -Causes: excessive dose, failure to reduce standard doses for some patients (elderly, obese, pregnant, short), unusual spread of local anesthetic -Signs/symptoms: dyspnea, weakness arms, nausea, hypotension -Treatment: reassurance, O2, treating bradycardia/hypotension -Cervical ascension: severe bradycardia, hypotension, respiratory insufficiency, apnea, unconsciousness = "high spinal" -Cranial nerves = "total spinal" - spread of LA to block entire spinal cord/brainstem -Anterior spinal artery syndrome - more from prolonged hypotension/spinal pressure -Treatment high/total spinal: ABCs, IVF, head-down, pressors/atropine B.) Cardiac Arrest -Causes: oversedation and unrecognized hypoventilation/hypoxia -1:1500 incidence --> high for spinals -Risk: high baseline vagal tone, hypoveolemia -Prevent: IVF administration, treating bradycardia/hypotension promptly C.) Urinary retention -S2-S4 block -Urinary catheterization for all but shortest-acting blocks
question
Complications: Needle or catheter insertion
answer
A.) Inadequate anesthesia/analgesia -Causes: movement of needle, incomplete entry of needle opening into subarachnoid space, subdural injection, loss of potency of local anesthetic solution (for spinals) -See epidural card for causes epidural B.) Intravascular injection -Signs/symptoms: seizures, unconsciousness, hypotension, arrhythmias, depress contractility -Usually seen with epidurals or caudal, but not spinals (because spinal doses are so low) -Causes: injected directly into vessel, or catheter enters blood vessel -Avoid: aspirating before each injection, test dose, close observation for signs/symtpoms early (tinnitus, tongue sensation) -Treatment: rescuscitation, lipid rescue -Potency for cardiac toxicity = potency for nerve blocks C.) Total spinal anesthesia -Causes: attempted epidural/caudal if accidental intrathecal injection -Rapid onset -Prevent: careful aspiration, test dose, incremental injections D.) Subdural injection -More serious complication of epidural > spinal because of amount used -Similar presentation to high spinal, but may be delayed 15-30 minutes and block may be "patchy" -Potential space that extends INTRACRANIALLY -Treatment: supportive, possible intubation, CV support E.) Backache -11-30% incidence -Epidural > Spinal -Bruising, local inflammation, muscle spasm -Many people also complain of backache after GA also -Treatment if needed: NSAIDs, acetaminophen, warm/cold compresses -Make sure not epidural hematoma or abscess F.) Post-Dural Puncture Headache (PDPH) -Cause: any breach of the dura, even if no apparent wet tap on epidural. CSF leakage, traction on structures supporting brain (meninges, dura, tentorium, blood vessels) -Signs/symptoms: bilateral, frontal or retroorbital, or occipital and extends to neck -Throbbing or constant, photophobia/nausea -** Association with BODY POSITION -Worse with sitting or standing, better by lying flat -Onset 12-72 hours, may be immediate too -May last for weeks -Traction on cranial nerves: diplopia (CN VI), tinnitus -Risk: large needle, young women -Treatment: lying down, analgesics (acetaminophen, NSAIDs, opioids), IVF, caffeine (vasoconstrics cerebral vessels) -Advanced treatment: epidural blood patch - 15-20 mL autologous blood into epidermal space at or 1 below dural puncture (90% will respond, 90% after second injection) G.) Neurologic injury: -0.03-0.1% -Injury to nerve roots or spinal cord -Avoid: if blockade performed below L1 adults, 3 in children (end of conus) -Risk: multiple attempts -Can cause paraplegia, isolated sacral nerve dysfunction, paralysis isolated muslces, anesthesia to isolated areas, loss of bowel/bladder function -Can occur from hematoma, abscess too, surgical/OB positioning, etc H.) Spinal or epidural Hematoma -1:150,000 epidurals -1:220,000 spinals -Risk: abnormal coags, insertion and removal of epidural catheters -Mass effect of hematoma causes insult to nerves/spinal cord -Symptoms: sharp back pain and leg pain with motor weakness or sphincter dysfunction -Treatment: CT/MRI dx, neurosurgical consult, surgical decompression in 8-12 hours I.) Meningitis/arachnoiditis -Causes: contamination of equipment or injected solutions, organisms tracked in from skin, indwelling catheters colonized -Arachnoiditis - can be noninfectious - pain/neuro symptoms --> imaging shows clumping of nerve roots -Prevention: sterile technique, face masks everyone in room J.) Epidural abscess -1:6500 - 1:500,000 incidence varies for epidurals -5 days- weeks after catheter insertion -4 stages: 1.) Back or vertebral pain increased by percussing over spine 2.) Nerve root or radicular pain 3.) Motor/sensory deficits or sphincter dysfunction 4.) Paraplegia/paralysis -Treatment: staph abc coverage if suspected, CT/MRI, neurosurgery/ID consultation, surgical decompression or CT-guided drainage -Reduce risk: minimizing catheter manipulations, using bacterial filter, removing catheter or changing at defined intervals (i.e. 4 days) K.) Sheering of an epidural catheter -if withdrawn through the needle -If catheter must be withdrawn when needle is in place, remove BOTH TOGETHER -Treatment: leave sheared tip in place, observe patient -If occurs in superficial tissues - surgically remove
question
Complications with drug toxicity
answer
A.) Systemic - see other card/Local anesthetics B.) TNS -transient neurologic symptoms/transient radicular irritation -back pain radiating to legs without sensory or motor deficits -Time: after resolution of anesthesia, resolves within a few days -12% highest incidence with lidocaine -1-2% with others -Usually with spinal, but can happen with epidural -Risk: outpatients, males in lithotomy position -Cause: concentration-dependent neurotoxicity of local anesthetics C.) Lidocaine Neurotoxicity -Cauda equina syndrome - risk with continuous spinal catheters, and 5% lidocaine -Signs/symptoms: Bowel/bladder dysfunction, evidence of multiple nerve root injury, lower motor neuron, paresis of legs -Patchy sensory deficits, peripheral nerve pattern -Cause: pooling or maldistribution of hyperbaric solutions can damage nerve roots of caudal equine
question
Epidural space boundaries:
answer
Foramen magnum to sacrum Anterior - posterior longitudinal ligament posterior - ligamentum flavum & laminae Inner - dura Lateral - pediclaes & intervertebral foramen
question
Spinal cord anatomy -Ends
answer
L1 ends as conus medullar is L/S roots form cauda equina Spinal space ends at S2 -31 pairs spinal nerves -Sympathetics: T1-L2
question
Layers penetrated for epidural/spinal
answer
Skin SubQ tissue Supraspinous ligament Interspinous ligament Ligamentum Flavum (epidural stops here) Epidural Space Dura mater Arachnoid mater



