Endocrine Path Lab – PICTURES – Flashcards
Unlock all answers in this set
Unlock answersquestion
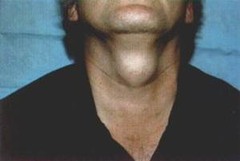
Multinodular goiter
answer
Multinodular goiters can get to be quite large (up to 100x normal wt.). In addition to being a cosmetic problem, large multinodular goiters can cause problems due to mass effects, with compression of the larynx & trachea causing airway obstruction and compression of the esophagus causing dysphagia (difficulty swallowing). Goiters are the result of impaired thyroid hormone synthesis, which results in increased release of TSH from the pituitary gland. In addition to stimulating increased secretion of T3 & T4 from the thyroid gland, TSH also acts as a growth factor and causes the thyroid follicular cells to undergo hyperplasia and hypertrophy. Most patients with a goiter are euthyroid (i.e. their T3 & T4 levels are normal), but at the cost of an increased TSH level.
question
Gross pic of multinodular goiter

answer
Note the presence of multiple nodules of varying size interspersed throughout the thyroid gland. Darker areas (white arrow) are due to the presence of hemorrhage, and lighter areas (yellow arrow) are due to the presence of fibrosis. The nodules that develop in a multinodular goiter are probably due in part to the fact that some follicular cells are inherently more responsive to TSH than others. In addition, over time somatic mutations develop in some of the follicular cells that gives them a growth advantage. Indeed, both monoclonal & polyclonal nodules coexist within a multinodular goiter.
question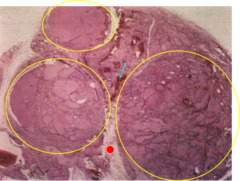
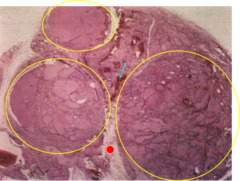
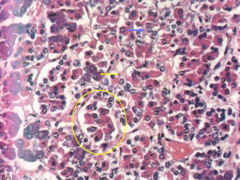
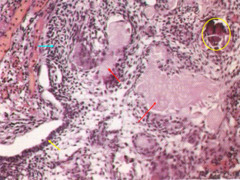
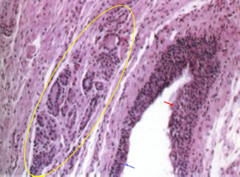
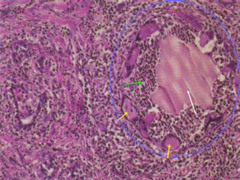
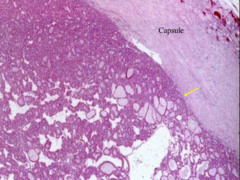
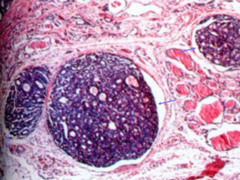
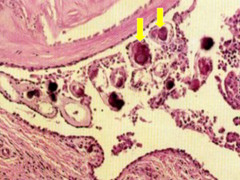
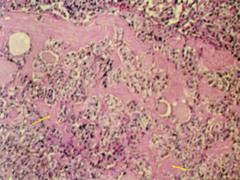
Histo of multinodular goiter
answer
This section shows three nodules of varying size. There are scattered areas of hemorrhage (a light blue arrow is pointing to one of these). There are also a few areas exhibiting fibrosis (a red circle is present in one of these areas). The regressive changes present in multinodular goiters (i.e. areas of hemorrhage, fibrosis, calcification & cystic change) are felt to be related to the uneven asymmetric growth that occurs in multinodular goiters, which produces stresses in the gland resulting in rupture of blood vessels & dilated follicles.
question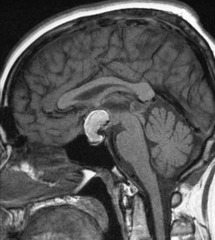
Pituitary adenoma
answer
MRI of a pituitary adenoma after administration of contrast media. The yellow arrow is pointing to a large pituitary adenoma. MRI, especially after administration of contrast media, is the best imaging technique to confirm a diagnosis of pituitary adenoma. Note the sharp border between the adenoma and surrounding brain. Pituitary adenomas being benign tumors most commonly exhibit expansile but not infiltrative growth. However, in as many as 30% of cases, pituitary adenomas are not grossly encapsulated and infiltrate neighboring tissues, such as the cavernous and sphenoid sinuses, dura, and on occasion, the brain itself. Such lesions are termed invasive adenomas. Not unexpectedly, macroadenomas tend to be invasive more frequently than smaller tumors. Some features associated with aggressive behavior by pituitary adenomas, include: increased mitotic activity, > 3% of the tumor cells staining positive for the proliferation marker Ki-67, overexpression of cyclin D1, p53 mutations, and epigenetic silencing of RB1. It is recommended that adenomas with these features be classified as atypical adenomas, since these tumors have a higher propensity for aggressive behavior, including invasion and recurrence. HRAS mutations are observed in the rarely occurring pituitary carcinomas.
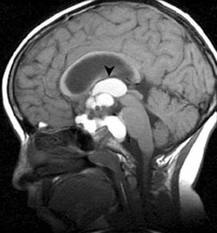
question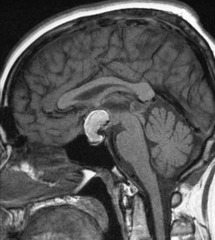
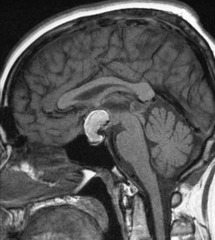
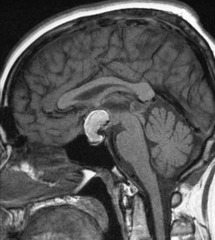
PItuitary adenoma
answer
Sagittal section of brain exhibiting a large pituitary adenoma (yellow arrow). Pituitary adenomas such as this, which are larger than 1cm in diameter, are referred to as macroadenomas. Macroadenomas are often nonfunctioning and most commonly cause symptoms due to local mass effects, including: visual field defects due to compression of the optic chiasm and headache, nausea & vomiting, and papilledema due to increased intracranial pressure. Light blue arrow is pointing to the pituitary stalk. Macroadenomas can also compress the pituitary stalk, thereby impeding the delivery of dopamine to the anterior pituitary resulting in hyperprolactinemia. This is referred to as the "stalk effect" (remember that dopamine inhibits the release of prolactin from the anterior pituitary).
question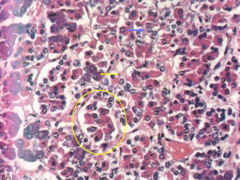
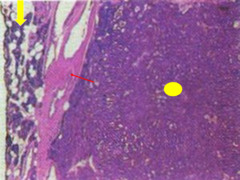
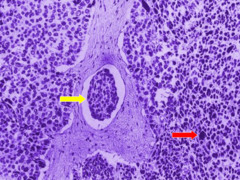
anterior pituitary- normal histo
answer
The endocrine cells are divided into discrete lobules by thin fibroconnective tissue trabeculae (yellow oval is encircling one of these). There are three types of cells in the anterior pituitary when viewed with a routine H&E stain... basophils (yellow arrow), acidophils (white arrow) and chromophobes (blue arrow).
question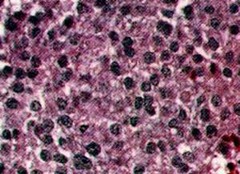
Prolactinoma or lactotroph adenoma
answer
Histologic section of a prolactin secreting adenoma referred to as a "prolactinoma"or "lactotroph adenoma." Note that in this typical example of a pituitary adenoma, there is a solid sheet of cells, and the tumor cells are not divided into discrete lobules. All of the tumor cells look essentially the same, which is referred to as "monotonous uniformity" or "cellular monomorphism." All of the tumor cells in this field are chromophobes. Immunostains are required to determine which hormone(s) the tumor is producing.
question
Prolactinoma with immunostain
answer
Immunostain for prolactin, which is strongly positive, confirming the diagnosis of a prolactinoma. Prolactinomas are the most common pituitary adenomas, accounting for 30% of pituitary adenomas. Prolactinomas occur more commonly in women than men and the peak incidence is between 20-30 years of age. In young women, the most common symptoms of hyperprolactinemia are amenorrhea and galactorrhea. In men, the most common symptoms of hyperprolactinemia are decreased libido and impotence. Galactorrhea and gynecomastia can rarely also be seen in men
question
Lymphocytic Hypophysitis
answer
Histologic section of the anterior pituitary involved by Lymphocytic Hypophysitis. The anterior pituitary is extensively infiltrated by lymphocytes and there is effacement of much of the parenchyma of the gland. Lymphocytic Hypophysitis is an autoimmune disorder of the anterior pituitary**. It occurs most commonly in young women late in pregnancy or during the postpartum period**. Lymphocytic Hypophysitis often results in hypopituitarism**. Patients with this disorder may have autoimmune disorders in other endocrine glands, such as Hashimoto thyroiditis and autoimmune adrenalitis. Anti-pituitary antibodies are seen in 20% of these patients.
question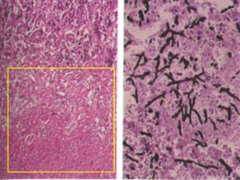
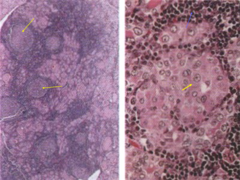
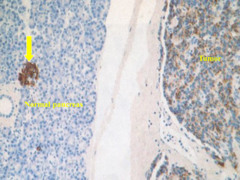
Aspergillus infxn of pituitary gland
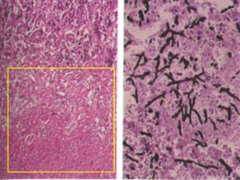
answer
Aspergillus infection of the pituitary gland. Fungal and Mycobacterial infections can involve the pituitary gland resulting in hypopituitarism. Most of these infections are encountered in immunosuppressed individuals. The histologic section on the left is from the anterior pituitary. The area bounded by the yellow rectangle is extensively necrotic. Remnants of viable pituitary are seen above the yellow rectangle. The section on the right is from the necrotic area inside the yellow rectangle stained with a Gomorri Methenamine Silver (GMS) stain. The GMS stain reveals the presence of numerous fungal hyphae. Some of the hyphae exhibit acute angle branching (yellow arrow) typical of Aspergillus species.
question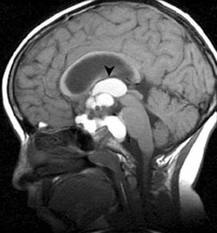
Craniopharyngioma
answer
Craniopharyngioma arising from the suprasellar region. Most craniopharyngiomas arise from the suprasellar region (i.e. the hypothalamic region), however, some of them can arise within the sella turcica (i.e. the intrasellar region). Most craniopharyngiomas are cystic and the tumor in this case exhibits multiple cystic spaces (yellow arrows are pointing to several of these). The blue arrow is pointing to the third ventricle, which is being compressed by the tumor. These tumors can cause symptoms due to local mass effects, such as visual field deficits. They can also cause symptoms due to deficiencies of pituitary hormones, including diabetes insipidus (dec ADH secretion). A bimodal age distribution is observed, with one peak in childhood (5 to 15 years) and a second peak in adults 65 years or older.
question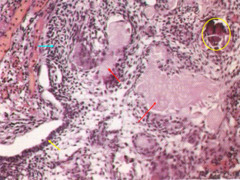
Histo of craniopharyngioma
answer
Craniopharyngiomas are benign tumors derived from vestigial remnants of Rathke pouch. Rathke pouch is an extension from the developing oral cavity. In this typical example of a craniopharyngioma, one can appreciate columnar epithelium (yellow arrow), squamous-like epithelium (light blue arrow) and glandular structures containing eosinophilic proteinaceous material (red arrows). An area of calcification is present inside the yellow oval. Calcification is commonly present in craniopharyngiomas and often allows these tumors to be seen on routine skull x-rays.
question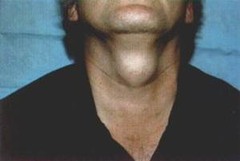
Thyroglossal duct cyst
answer
Thyroglossal duct cysts are derived from remnants of the thyroglossal duct, which connects the base of the tongue to the thyroid gland during embryologic development. Thyroglossal duct cysts are one of the most common causes of a neck mass. They usually occur in the midline of the neck, and typically move upward on swallowing, since they are nearly always connected to the hyoid bone. Uninfected thyroglossal duct cysts are asymptomatic, however, infected thyroglossal duct cysts are often accompanied by pain and tenderness to palpation
question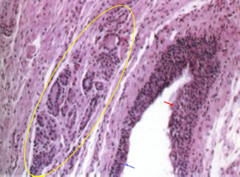
Thyroglossal duct cyst - histology
answer
The lumen of a thyroglossal duct cyst is lined by either respiratory (blue arrow) or squamous epithelium (red arrow). Thyroid tissue is present in the wall of a thyroglossal duct cyst in more than 60% of cases (tissue inside yellow oval). The thyroid tissue within the wall of a thyroglossal duct cyst can rarely give rise to a follicular adenoma or a carcinoma (usually a papillary carcinoma).
question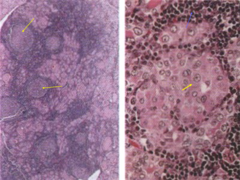
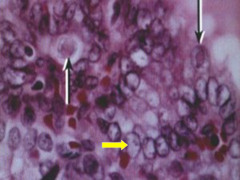
hashimotos thyroiditis- histo
answer
The low power image on the left reveals the presence of numerous lymphoid follicles with reactive germinal centers (yellow arrows point to several of these). The high power image on the right reveals numerous follicular epithelial cells exhibiting so-called "Hurthle cell metaplasia" (yellow arrow). Hurthle cells have abundant eosinophilic granular cytoplasm. Numerous mononuclear inflammatory cells are also noted (blue arrow). Hashimoto thyroiditis is an autoimmune disorder of the thyroid gland. These patients do not respond to anti-inflammatory drugs, and eventually develop hypothyroidism requiring thyroid hormone replacement therapy.
question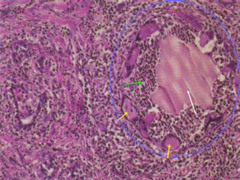
Subacute (granulomatous) thyroiditis
answer
-This entity is seen most often in women 30-50 years of age following a viral infection. ** -The patients often present with a variety of constitutional symptoms, such as fever, malaise and myalgias, as well as pain in the neck that often radiates upward**. They may have a transient period of hyperthyroidism related to disruption of follicles, followed by a transient period of hypothyroidism. The disease is self-limited and almost all of these patients regain normal thyroid function. This histologic section is typical of the active phase of the illness. There is a thyroid follicle (inside the blue oval) which has been disrupted by the inflammatory process. Residual colloid (white arrow) is present within the disrupted follicle and there are also numerous neutrophils (green arrow). Multiple multinucleated histiocytic giant cells (yellow arrows are pointing to some of these) are circumscribing the disrupted follicle.
question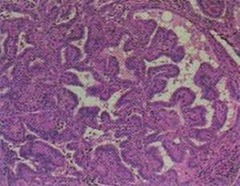
Graves
answer
Graves Disease is an autoimmune disorder of the thyroid gland in which the patients produce antibodies directed against the TSH receptor. In Graves Disease, the TSH receptor antibodies act as agonists and result in constitutive activation of the TSH receptors on the follicular epithelial cells. Constitutive activation of the TSH receptors results in hyperthyroidism, as well as hyperplasia and hypertrophy of the follicular epithelial cells. In this histologic section, there is formation of numerous papillae which project into the lumen of follicles. This change is caused by the increased number of cells lining the follicles, and is referred to as "papillary hyperplasia." Papillary hyperplasia occurs diffusely throughout the thyroid gland in Graves Disease. Also note the paucity of colloid within the follicles. In Graves Disease, the follicular epithelial cells are pinocytizing colloid and degrading thyroglobulin to release more T3 and T4, almost as fast as more colloid can be produced.
question
Folicular adenoma-gross

answer
Follicular adenomas are benign tumors derived from the follicular epithelial cells. There are a variety of different subtypes based upon the extent of follicle formation, size of the follicles, etc.. For example, there are macrofollicular adenomas (large follicles), microfollicular adenomas (small follicles), trabecular adenomas (cords of tumor cells with few follicles), etc.. The various subtypes of follicular adenomas are not important, since the different subtypes of follicular adenomas have no bearing on biologic behavior. They are benign and that's all the surgeon and the patient care about. In this typical example of a follicular adenoma, the tumor is well circumscribed, encapsulated (yellow arrow) and lighter in color than the surrounding normal thyroid gland. Most follicular adenomas are cold nodules on scintillation scans and are therefore commonly biopsied. The majority of follicular adenomas are 2-3cm in diameter at the time they are biopsied
question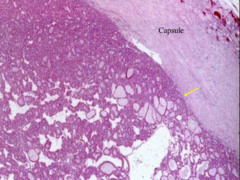
Follicular adenoma - histo
answer
The yellow arrow is pointing at the junction between the tumor and the capsule. Note how well this benign follicular neoplasm respects the capsule. Follicular adenomas never invade into the capsule.
question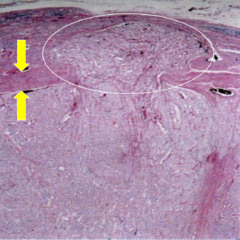
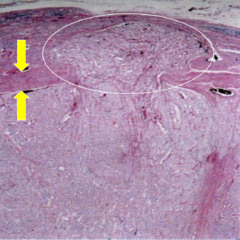
Follicular carcinoma-histo
answer
Follicular carcinomas are malignant neoplasms derived from the follicular epithelial cells that typically form small follicles. Follicular carcinoma is the second most common type of thyroid cancer and is most commonly encountered in women 40-60 years of age. Follicular carcinomas similar to follicular adenomas are usually encapsulated. The yellow arrows are pointing to the overlying capsule. The tumor can be seen to be invading through the capsule into surrounding thyroid tissue (area inside white oval). Since the tumor invades completely through the capsule into the surrounding thyroid tissue, it would be considered to be a "widely invasive" follicular carcinoma. If the tumor invades into the capsule, but does not extend beyond the capsule, it is considered to be a "minimally invasive" follicular carcinoma. Minimally invasive follicular carcinomas have a 10-year survival rate similar to that for papillary carcinomas, whereas the 10-year survival rate for widely invasive follicular carcinomas is only 50%.
question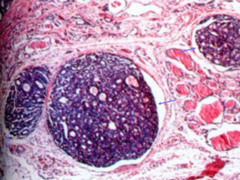
Follicular carcionma with vascular invasion
answer
Histologic section of a Follicular Carcinoma, contiguous to the main tumor mass, exhibiting vascular invasion. The blue arrows are pointing to nests of tumor, which are within vascular spaces. The nests of tumor exhibit small follicles typical of a follicular carcinoma. Follicular carcinomas have a propensity to invade blood vessels and these tumors therefore often give rise to disseminated metastases. The preferred sites for metastases include: bone, lungs and liver**. Because of their propensity for vascular invasion, follicular carcinomas overall have a worse prognosis than the more common papillary carcinomas
question
papillary carcinoma of thyroid

answer
Papillary carcinomas are malignant neoplasms, which are also derived from the follicular epithelial cells. It is the most common type of thyroid cancer and is most commonly encountered in women from 25 to 50 years of age. The vast majority of thyroid cancers related to previous exposure to ionizing radiation are of this type. The tumor in this example is largely unencapsulated with an irregular infiltrative margin. Most papillary carcinomas are unencapsulated. There is, however, an encapsulated variant comprising approximately 10% of these tumors. Note the "shaggy" or "ragged" appearance of the tumor on cut section, this appearance is due to the formation of numerous papillary fronds by the tumor
question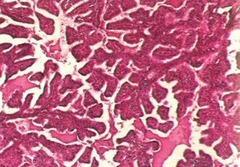
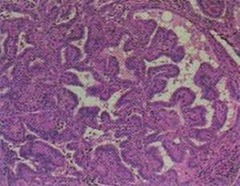
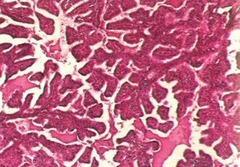
papillary carcinoma -histo (fronds)
answer
There are numerous papillary fronds having fairly broad fibroconnective tissue cores.
question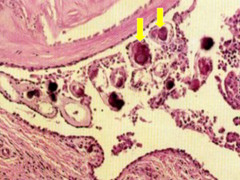
Psammoma bodies of papillary carcinoma
answer
No definite papillary fronds are evident in this section, however, there are a number of psammoma bodies (yellow arrows point to several of these). Psammoma bodies are laminated calcified concretions, which are a very characteristic feature of papillary carcinoma. Psammoma bodies are rarely if ever found in the other carcinomas arising in the thyroid gland, so when present they are virtually diagnostic of a papillary carcinoma.
question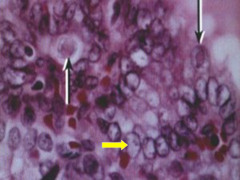
orphan annie's eye of papillary carcinoma
answer
Note the optically clear "ground glass" or "Orphan Annie eye" nuclei (yellow arrow points to a good example of this). These nuclear features are characteristic of a papillary carcinoma. In fact, these nuclear features are more important in making the diagnosis of papillary carcinoma than are the architectural features. There is a variant of papillary carcinoma referred to as "follicular variant of papillary carcinoma," in which the tumor principally forms follicles similar to a follicular carcinoma. This variant, however, has the nuclear features of a papillary carcinoma with the optically clear nuclei, and indeed the biologic behavior is that of a typical papillary carcinoma. The black arrows are pointing to eosinophilic intranuclear inclusions, which are another feature of these tumors, albeit not as important as the optically clear nuclei. Papillary carcinomas have a propensity to invade lymphatics and often involve the cervical lymph nodes. Papillary carcinomas do not, however, usually exhibit vascular invasion, so that only 10-15% of patients with these tumors ever develop distant metastases. The prognosis for papillary carcinoma is therefore excellent with the overall 10-year survival rate being > 95%.
question
Medullary carcionoma
answer
In this typical example, the tumor is unencapsulated and has an irregular infiltrative border. Medullary carcinomas arise from C cells, which are neuroendocrine cells that normally secrete calcitonin. Medullary carcinomas can secrete other peptides as well, including: CEA, VIP, somatostatin and serotonin. Medullary carcinomas are familial in 30% of the cases. In the familial cases, the tumor is often multifocal and frequently involves both lobes. It is common practice to screen relatives of patients with medullary carcinoma with serum calcitonin levels or genetic testing for RET protooncogene mutations.
question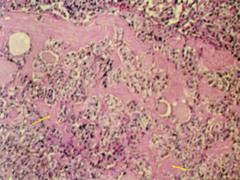
Medullary carcinoma- histo
answer
The tumor cells are polygonal to spindle-shaped, relatively small with hyperchromatic nuclei. The extracellular eosinophilic material represents deposition of amyloid (yellow arrows point to some examples of this). The amyloid deposition is a characteristic feature of this tumor and is due to the abundant production of calcitonin. Postoperatively, patients with medullary carcinoma are followed with serum calcitonin and CEA levels.
question
parathyroid adenoma

answer
Parathyroid adenomas are benign tumors which are often functional. The functional parathyroid adenomas autonomously secrete PTH resulting in hypercalcemia. Parathyroid adenomas can be in ectopic locations, such as higher up in the neck, within the substance of the thyroid gland or even within the mediastinum. This can make finding the adenoma at the time of surgery a challenge for the surgeon. The adenoma in this instance was readily apparent and easily accessible and this would have been an easy case for the surgeon, i.e. "Miller time!"
question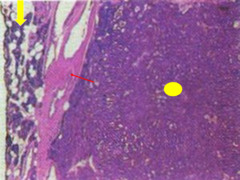
parathyroid adenoma-histo
answer
The adenoma (area marked by the yellow oval) is very cellular with no intervening adipose tissue. The red arrow is pointing to the capsule of the adenoma. Outside of the capsule, there is a rim of surrounding normal parathyroid tissue with readily apparent intervening adipose tissue (yellow arrow).
question
osteitis fibrosa cystica- a/w parathyroid adenoma

answer
X-ray of the hands from a patient with a parathyroid adenoma who developed osteitis fibrosa cystica. Osteitis fibrosa cystica is the name given to the skeletal changes that occur in patients with long-standing primary hyperparathyroidism. Note the radiolucent lytic areas in the distal phalanges (arrows point to good examples of this). PTH stimulates osteoclastic bone resorption, and patients with osteitis fibrosa cystica can develop pathologic fractures.
question
Adrenocortical adenoma

answer
Adrenocortical adenomas are usually yellow in color because of all the lipid in the tumor cells. They are well-circumscribed and are usually not larger than 2.5 cm in diameter. Most adrenocortical adenomas are actually nonfunctional (do not secrete any hormones). Nonfunctional adrenocortical adenomas are usually incidental findings during imaging studies or at autopsy. Functioning adrenocortical adenomas can produce cortisol (Cushing syndrome), aldosterone (Conn syndrome) or androgenic steroids (Adrenogenital syndromes).
question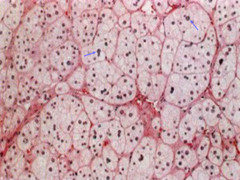
adrenocortical adenoma-histo
answer
The tumor cells look similar to those seen in the normal adrenal cortex. The tumor cells exhibit abundant foamy cytoplasm because of all the lipid they contain. The nuclei are for the most part small and uniform. Some mild nuclear enlargement and pleomorphism is often seen (arrows point to some examples of this). Functional and nonfunctional adenomas cannot be distinguished on the basis of their morphologic features. Determination of whether or not an adenoma is functional and what hormone is being produced is determined by the clinical presentation of the patient and laboratory measurement of hormone levels.
question
Adrenocortical carcinoma-gross

answer
Adrenocortical carcinomas are usually large tumors often exceeding 20cm in diameter (such as this example). These tumors are often variegated (multicolored) because of areas of hemorrhage and necrosis. Adrenocortical carcinomas are more likely to be functional than the adenomas, and are therefore often associated with clinical manifestations of increased hormone secretion (hyperadrenalism).
question
adrenocortical carcinoma-histo
answer
The section on the left reveals significant nuclear enlargement and pleomorphism. The tumor cells do not contain as much lipid as the cells in the adenomas. This may be do to the fact that the tumor cells in the carcinomas are often more actively secreting hormones resulting in some lipid depletion. The arrow on the left is pointing to an atypical mitotic figure (in this case a "tripolar" mitotic figure). Atypical mitotic figures are an indicator of malignancy. The arrow on the right is pointing to an area of tumor necrosis. Tumor necrosis occurs in rapidly growing tumors, which are outgrowing their vascular supply.
question
PCC of the adrenal medulla

answer
Pheochromocytomas arise most commonly ( 90%) within the adrenal medulla. The remainder arise within the extra-adrenal paraganglia most commonly below the diaphragm. Pheochromocytomas are derived from chromaffin cells and these tumors secrete catecholamines, with the major clinical manifestation being hypertension. The hypertension is often episodic and accompanied by other signs and symptoms of catecholamine excess, such as: tachycardia, palpitations, sweating and tremors. The majority of pheochromocytomas are sporadic, but up to 25% are familial. In the familial tumors, many arise in childhood and 50% are bilateral. Most pheochromocytomas are tan in color. The darker areas (yellow arrow) represent areas of hemorrhage. The thin rim of yellow tissue overlying the tumor (white arrow) is the adrenal cortex, which is somewhat attenuated. The blue arrow is pointing to residual adrenal gland not involved by the tumor.
question
PCC- histo

answer
. Note how the tumor cells are arranged into very discrete rounded nests circumscribed by fibrovascular trabeculae (area inside the yellow oval is a good example of this). This growth pattern is referred to as "zellballen" and is the most characteristic histologic feature of a pheochromocytoma. Approximately 10% of pheochromocytomas arising in the adrenal medulla are malignant, whereas 20-40% of pheochromocytomas arising in the extra-adrenal paraganglia are malignant. The histologic features of a pheochromocytoma are not a reliable predictor of the tumor's biologic behavior, so that the diagnosis of malignancy in pheochromocytomas is based exclusively on the presence of metastases.
question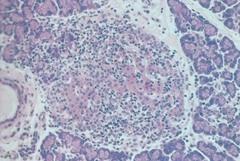
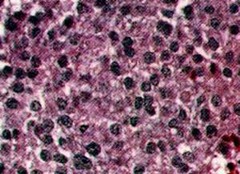
Insulitis of pancreas - Type 1 DM
answer
Section of pancreas showing an islet exhibiting insulitis. The islet is infiltrated by lymphocytes, which is referred to as "insulitis." Insulitis is seen in patients with Type 1 diabetes. Type 1 diabetes is the result of an autoimmune disorder directed against the -cells of the pancreatic islets
question
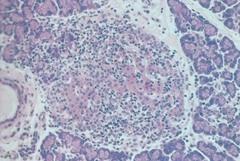
Amyloidosis of pancreas - type 2 DM
answer
Section of pancreas exhibiting an islet involved by amyloidosis. Amyloidosis of the pancreatic islets is seen in patients with Type 2 diabetes. The amyloid results from the deposition of amylin fibrils. Amylin is a peptide, which is secreted along with insulin by the -cells. Insulin resistance in Type 2 diabetes resulting in a sustained increased demand for insulin secretion underlies the amyloidosis. In long-standing cases of Type 2 diabetes, amyloid may largely obliterate some of the islets (as seen in this example) and contribute to the insulin deficiency seen later in the course in many cases of Type 2 diabetes.
question
Islet cell tumor

answer
Cross section of pancreas exhibiting an islet cell tumor. The islet cell tumor in this case is an insulinoma. Insulinomas, as the name implies, autonomously secrete insulin. Insulinomas are the most common type of islet cell tumor comprising approximately 80% of the islet cell tumors
question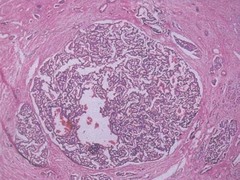
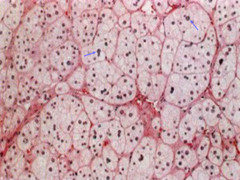
Insulinoma- histo
answer
Islet cell tumors are most commonly composed of cords or nests of relatively small, uniform, round to oval tumor cells. Insulinomas, as well as the other islet cell tumors, can be benign or malignant. Approximately 90% of insulinomas are benign. Islet cell tumors, even when malignant, do not usually exhibit much anaplasia, so it may be difficult at times histologically to determine whether the tumor is benign or malignant. Signs of malignancy include local invasion, as well as lymphatic or blood vessel invasion.
question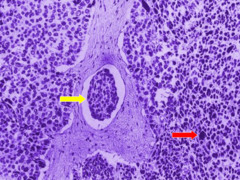
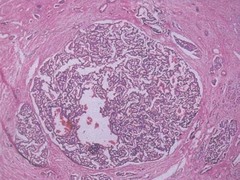
Malignant insulinoma
answer
Malignant insulinoma composed of relatively small basophilic staining tumor cells. Mild anaplasia is evident in this malignant insulinoma (red arrow points to an enlarged hyperchromatic nucleus). Lymphatic invasion is present (yellow arrow is pointing to a nest of tumor within a lymphatic space) indicating the sinister intent of this tumor. Approximately 10% of insulinomas are malignant.
question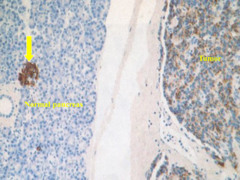
Islet cell tumor showing immunoperoxidase stain for insulin
answer
Immunoperoxidase stain for insulin. Normal pancreas is on the left side of the field, and an islet cell tumor is on the right side of the field. The yellow arrow is pointing to an islet of Langerhans in the normal pancreas, which is strongly positive for insulin. The islet cell tumor on the right is positive for insulin indicating that it is an insulinoma. Insulinomas can in some cases secrete enough insulin to result in attacks of hypoglycemia. The attacks of hypoglycemia are often precipitated by fasting or exercise and can cause a variety of symptoms, including: sweating, nervousness, hunger, confusion, and sometimes progressing to stupor and coma if the hypoglycemia is severe enough.



