CH. 22: Respiratory Tract Infections, Neoplasms, and Childhood Disorders – Flashcards
Unlock all answers in this set
Unlock answersquestion
Viruses
answer
are the most frequent cause of respiratory tract infections
question
viral infections can damage __________ epithelium, _________ airways, and lead to secondary ________ infections
answer
bronchial; obstruct; bacterial
question
The common cold is a viral infection of the _________ respiratory tract
answer
Upper
question
Anithistamine
answer
Are popular over-the-counter treatment for colds because of their action in drying nasal secrections
question
Rhinitis; paranasal
answer
_______________refers to inflammation of the nasal passages, and sinusitis as inflammation of the ________________ sinuses
question
the lower __________ content in the sinuses facilitates the growth of organisms, impairs local defenses, and alters the function of immune cells
answer
oxygen
question
host antibodies to ________________ and ________________ prevent or ameliorate infection by the influenza virus
answer
hemagglutinin; neuraminidase
question
the influenza virus cause three types of infections:
answer
1. an uncomplicated upper respiratory infection 2. viral pneumonia 3. a respiratory viral infection, followed by a bacterial infection
question
because influenza is so highly contagious prevention relies primarily on _______________
answer
vaccination
question
avian strains of the influenza virus do not usually cause outbreaks of disease in humans unless a ______________ of the virus genome has occurred within an intermediate mammalian host such as a pig
answer
reassortment
question
the term ____________ describes inflammation of parenchymal structures of the lung, such as the alveoli and the bronchioles
answer
pneumonia
question
lobar pneumonia; bronchopneumonia
answer
__________________ refers to consolidation of a part or all of a lung lobe; and ____________________ signifies a patchy consolidation involving more than one lobe.
question
hospital-acquired, or ______________, pneumonia is defined as a lower respiratory tract infection that was not present or incubating on admission to the hospital
answer
nosocomial
question
the term _______________ host usually is applied to persons with a variety of underlying defects in host defenses
answer
immunocompromised
question
___________________disease is a form of bronchopneumonia; infection normally occurs by acquiring the organism from environment
answer
Legionnaire
question
the primary atypical pneumonias are caused by a variety agents, the most common being _____________ pneumonia
answer
mycoplasma
question
_______________is the world's foremost cause of death from a single infectious agent
answer
tuberculosis
question
mycobacteria are similar to other bacterial organisms except for an outer __________ that makes them more resistant to destruction
answer
waxy
question
__________ tuberculosis is a form of the disease that develops in unexposed, and therefore sensitized, persons
answer
primary
question
the most frequently used screening methods for pulmonary tuberculosis are the _______________ tests and chest ___________.
answer
tuberculin skin; x-rays
question
__________________is caused by the dimorphic fungus Histoplasma capsulatum and is one the most common fungal infections in the united states.
answer
histoplasmosis
question
____________ respiratory infections produced pulmonary manifestations that resemble tuberculosis
answer
fungal
question
the number of Americans who develop lung cancer is decreasing primarily because of a decrease in _______________
answer
smoking
question
cigarette smoking causes more than _____________ of cases of lung cancer
answer
80%
question
__________are aggressive, locally invasive, and widely metastatic tumors hat arise from the epithelial lining of major bronchi.
answer
lung cancers
question
Upper Respiratory Viruses in Adults
answer
Common cold Rhinosinusitis Influenza
question
Rhinoviruses (common cold)
answer
Occur in early fall and late spring in persons between ages 5 and 40
question
Parainfluenza viruses (common cold)
answer
Occur in children younger than 3
question
Respiratory syncytial virus
answer
Occur in winter and spring in children younger than 3
question
Coronaviruses and adenoviruses
answer
Occur in winter and spring
question
Rhinosinusitis (Sinusitis)

answer
Infection or allergy obstructs sinus drainage Acute: facial pain, headache, purulent nasal discharge, decreased sense of smell, fever Chronic: nasal obstruction, fullness in the ears, postnasal drip, hoarseness, chronic cough, loss of taste and smell, unpleasant breath, headache
question
what is the greastest source of spread of the common cold
answer
fingers, hand washiing is a preventing measure for
question
nasal mucosa, and conjunctival surface of the eyes
answer
most common portals for entry of the common cold virus
question
rhinitis
answer
inflammation of the nasal passages
question
sinusitis (rhinosinusitis)
answer
inflammation of the paranasal sinuses
question
paranasal sinuses
answer
are air-filled extensions of the respiratory part of the nasal cavities into the frontal, ethmoid, sphenoid, and maxilla bones
question
Acute rhinosinusitis
answer
may be of viral, bacterial, or viral-bacterial etiology. In most cases, bacterial infection is preceded by a viral upper respiratory infection, which in turn leads to inflammation and obstruction of the ostiomeatal complex.
question
Rhinovirus
answer
is the most common viral pathogen. Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis make up the majority of community-acquired bacterial pathogens.
question
chronic rhinosinusitis
answer
are usually a mixture of aerobic and anaerobic bacteria, including Staphylococcus aureus, coagulase-negative Staphylococcus, and anaerobic gram-negative bacilli.
question
The symptoms of acute viral rhinosinusitis often are similar to those of the common cold and allergic rhinitis include
answer
facial pain, headache, purulent nasal discharge, decreased sense of smell, and fever. A history of a preceding common cold and the presence of purulent nasal drainage, pain on bending, unilateral maxillary pain, and pain in the teeth are common findings with involvement of the maxillary sinuses.
question
Acute bacterial rhinosinusitis
answer
is suggested by symptoms that worsen after 5 to 7 days or persist beyond 10 days, or symptoms that are out of proportion to those usually associated with a viral upper respiratory tract infection
question
chronic rhinosinusitis,
answer
the only symptoms may be nasal obstruction, a sense of fullness in the ears, postnasal drip, hoarseness, chronic cough, and loss of taste and smell. Sinus pain often is absent; instead, the person may complain of a headache that is dull and constant.
question
influenza
answer
In the United States, approximately 36,000 persons die each year of influenza-related illness Transmission is by aerosol (3 or more particles) or direct contact Upper respiratory infection (rhinotracheitis) -Like a common cold with profound malaise Viral pneumonia -Fever, tachypnea, tachycardia, cyanosis, hypotension Respiratory viral infection followed by a bacterial infection
question
Treatment of rhinosinusitis
answer
depends on the cause and includes appropriate use of antibiotics, intranasal corticosteroids, mucolytic agents, and symptom relief measures.
question
diagnosis of rhinosinusitis
answer
usually is based on symptom history and a physical examination that includes inspection of the nose and throat. Headache due to sinusitis needs to be differentiated from other types of headache. Sinusitis headache usually is exaggerated by bending forward, coughing, or sneezing..
question
three distinct types of influenza viruses,
answer
designated A, B, and C. Influenza A and B cause epidemics. Influenza C does not cause epidemics, but is responsible for mild upper respiratory infections in children and adults.
question
Hemagglutinin,
answer
for which there are 16 different variants (H1 thru H16), allows the virus to anchor to the surface of epithelial cells in the respiratory tract
question
neuraminidase,
answer
of which there are 9 variants (N1 thru N9), allows for digestion of host secretion and, later, release of viral particles from host cells. For example, an influenza virus circulating worldwide in 2013 was identified as H3N2. Immunity to the surface H and N antigens reduces the likelihood and severity of infection with the influenza virus.
question
Epidemics of influenza A occur when
answer
a process called antigenic drift cause minor changes in the amino acids of the H and N glycoproteins, and generate a new subtype to which the population is only partially protected by cross-reacting antibodies.
question
Pandemics of influenza A occur when
answer
occur when a process called an antigenic shift causes both the H and N antigens to be replaced through recombination of the RNA segments with those of animal viruses, making all individuals susceptible to the new influenza virus.
question
The influenza viruses can cause three types of infections:
answer
an uncomplicated upper respiratory infection (rhinotracheitis), viral pneumonia, bacterial infection (caused from the respiratory infection)
question
influenza initially establishes upper and lower airway infections. what are signs of the upper and lower?
answer
upper airway infection - kills mucus-secreting, ciliated, and other epithelial cells, leaving gaping holes between the underlying basal cells and allowing extracellular fluid to escape. This is the reason for the rhinorrhea or "runny nose" that is characteristic of this phase of the infection. If the virus spreads to the lower respiratory tract, the infection can cause severe shedding of bronchial and alveolar cells.
question
symptoms in influenza in early stages
answer
abrupt onset of fever and chills malaise muscle aching headache profuse, watery nasal discharger nonproductive cough sore throat
question
viral pneumonia symptoms
answer
occurs as a complication of influenza. develops within 1 day after onset of influenza and rapid onset of fever, tachypnea, tachcardia, cyanosis, and hypotension can cause hypoxia and death
question
Secondary complications of of bacterial pneumonia
answer
typically include sinusitis, otitis media, bronchitis, and bacterial pneumonia.
question
Secondary causes of of bacterial pneumonia
answer
are S. pneumoniae, S. aureus, H. influenzae, and M. catarrhalis.
question
Two antiviral drugs are available for treatment of influenza:
answer
Zanamivir (Relenza) and oseltamivir (Tamiflu) are inhibitors of neuraminidase, the glycoprotein necessary for viral replication and release.
question
pneumonia
answer
describes inflammation of the parenchymal structures of the lung, such as the alveoli and bronchioles. Although antibiotics have significantly reduced the mortality rate from pneumonias,
question
Typical pneumonias
answer
bacteria in the alveoli Lobar: affect an entire lobe of the lung Bronchopneumonia: patchy distribution over more than one lobe
question
Atypical pneumonias
answer
are caused by viral and mycoplasma infections that invade the alveolar septum and the interstitium of the lung
question
community-acquired pneumonia
answer
is used to describe infections from organisms found in the community rather than in the hospital or nursing home. may be either bacterial or viral most common causes of infection causes are from S. pneumoniae, then H. influenzae, S. aureus, and gramnegative bacilli. Less common agents are Mycoplasma pneumoniae, Chlamydia species, and viruses, sometimes called atypical agents.
question
Hospital-acquired, or nosocomial,
answer
pneumonia is defined as a lower respiratory tract infection that was not present or incubating on admission to the hospital. Gram-negative rods (Enterobacteriaceae and Pseudomonas species) and S. aureus are the most common isolates. 14 Many of these organisms have acquired antibiotic resistance and are thus difficult to treat.
question
tuberculosis is more common among what population
answer
among foreingg-born persons with highest incidence and among residents of high-risk congregate settings such as correctional facilities, drug treatment facilities, and homeless shelters
question
tuberulosis is transmitted how and by what organism?
answer
is an airborne infection and is caused by M. tuberculosis mycobacterium. its slow growth, antigenicity, and resistance to detergents, disinfectants, and antibiotics.
question
how is tuberculosis spread?
answer
spread by minute, invisible particles, called droplet nuclei, that are harbored in the respiratory secretions of persons with active tuberculosis. Coughing, sneezing, and talking all create respiratory droplets; these droplets evaporate, leaving the organisms (droplet nuclei), which remain suspended in the air and are circulated by air currents. Thus, living in crowded and confined conditions increases the risk for spread of the disease.
question
Tuberculosis
answer
World's foremost cause of death from a single infectious agent Causes 26% of avoidable deaths in developing countries Drug-resistant forms Mycobacterium tuberculosis hominis -Aerobic -Protective waxy capsule -Can stay alive in "suspended animation" for years
question
Ghon focus
answer
1. is the development of a graywhite, circumscribed granulomatous lesion, the result of a cell-mediated immune response in an immunocompetent person. 2. contains the tubercle bacilli, modified macrophages, and other immune cells. It is usually located in the subpleural area of the upper segments of the lower lobes or in the lower segments of the upper lobe.
question
Ghon complex
answer
Nodules in lung tissue and lymph nodes Caseous necrosis inside nodules Calcium may deposit in the fatty area of necrosis Visible on x-rays
question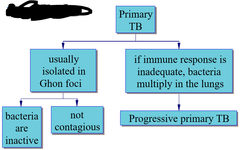
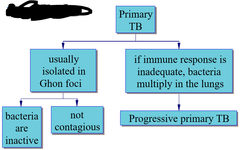
Primary TB
answer
1. is a form of the disease that develops in previously unexposed, and therefore unsensitized, persons. 2. is initiated as a result of inhaling droplet nuclei that contain the tubercle bacillus 3. are asymptomatic and go on to develop latent tuberculosis infection in which T lymphocytes and macrophages surround the organism in granulomas that limit their spread. Individuals with latent tuberculosis do not have active disease and cannot transmit the organism to others.
question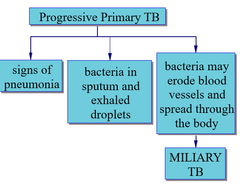
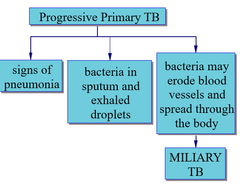
Miliary TB
answer
1. may erode into a blood vessel, giving rise to hematogenic dissemination. 2. describes minute lesions, resembling millet seeds, resulting from this type of dissemination that can involve almost any organ, particularly the brain, meninges, liver, kidney, and bone marrow.
question
Initial TB Infection

answer
Macrophages begin a cell-mediated immune response Takes 3-6 weeks to develop positive TB test Results in a granulomatous lesion or Ghon focus containing Macrophages T cells Inactive TB bacteria
question
Secondary TB represents either
answer
1. Reinfection from inhaled droplet nuclei 2. Reactivation of a previously healed primary lesion 3. Immediate cell-mediated response walls off infection in airways 4. Bacteria damage tissues in the airways, creating cavities 5. Signs of chronic pneumonia: gradual destruction of lung tissue "6. Consumption": eventually fatal if untreated
question
Secondary Tuberculosis (TB) symptoms
answer
1. commonly present with low-grade fevers, night sweats, easy fatigability, anorexia, and weight loss. 2. A cough initially is dry but later becomes productive with purulent and sometimes blood-tinged sputum. 3. Dyspnea and orthopnea develop as the disease advances.
question
The partial immunity that follows primary tuberculosis
answer
normally affords protection against reinfection and helps localize the disease should reactivation occur.
question
diagnosis of TB
answer
1. identified by culture sputum or DNA 2. X-ray Tuberculin skin test
question
TB treatment
answer
eliminating the tubercle bacilli while preventing the spread of infection and development of drug-resistant forms of the disease.
question
The basic principles of tuberculosis treatment are:
answer
(1) to administer multiple dr (2) to add at least two new drugs when treatment failure is suspected, (3) to provide the safest and most effective therapy in the shortest period of time, and (4) to ensure adherence to therapy.
question
latent tuberculosis infection
answer
1. are asymptomatic 2. from Primary TB in which T lymphocytes and macrophages surround the organism in granulomas that limit their spread. 3. Individuals do not have active disease and cannot transmit the organism to others.
question
Fungal Infections
answer
1. most are asymptomatic, can be severe or even fatal in persons immunodeficiencies or heavy exposure
question
Types of Fungal infections
answer
yeasts and molds
question
Yeasts
answer
are round and grow by budding.
question
Molds
answer
form tubular structures called hyphae and grow by branching and forming spores
question
Some fungi are dimorphic,
answer
1. meaning that they grow as yeasts at body temperatures and as molds at room temperatures. 2. most common are Histoplasma capsulatum, Coccidioides immitis, and Blastomyces dermatitidis.
question
A simple classification of mycoses (diseases caused by fungi) divides into 4 categories:
answer
superficial cutaneous subcutaneous deep (systemic) mycoses.
question
The superficial, cutaneous, or subcutaneous mycoses cause disease of
answer
the skin, hair, and nails.
question
Deep fungal infections may produce
answer
1. pulmonary and systemic infections and are sometimes fatal. 2. caused by virulent fungi that live freely, typically in soil or decaying organic matter and frequently in specific geographic regions.
question
Tuberculosis
answer
1. is a chronic respiratory infection caused by the bacterium M. tuberculosis. 2. The destructiveness of the disease results from the cell-mediated hypersensitivity response that the bacillus evokes rather than its inherent destructive capabilities.
question
The treatment of tuberculosis
answer
focuses on eliminating the tuberculosis bacilli from infected persons and eliminating its spread, requires multiple medications and has been complicated by outbreaks of drug-resistant forms of the disease.
question
Infections caused by the fungi H. capsulatum (histoplasmosis), C. immitis (coccidioidomycosis), and B. dermatitidis (blastomycosis) produce
answer
? pulmonary manifestations that resemble tuberculosis. These infections are common but seldom serious unless they produce progressive destruction of lung tissue or the infection disseminates to organs and tissues outside the lungs.
question
Lung Cancer
answer
1. Bronchogenic carcinoma a. Arises from epithelial cells lining the lungs b. Small cell lung cancer c. Non-small cell lung cancer -Large cell carcinoma -Squamous cell -Adenocarcinoma
question
Manifestations of Lung Cancer
answer
1. Changes in organ function (organ damage, inflammation, and failure) 2. Local effects of tumors (e.g., compression of nerves or veins, gastrointestinal obstruction) 3. Ectopic hormones secreted by tumor cells (paraneoplastic disorders) 4. Nonspecific signs of tissue breakdown (e.g., protein wasting, bone breakdown)
question
Respiratory Distress Syndrome

answer
1. Lack of surfactant; infants are not strong enough to inflate their alveoli 2. Protein-rich fluid leaks into the alveoli and further blocks oxygen uptake 3. Treatment with mechanical ventilation may cause bronchopulmonary dysplasia and chronic respiratory insufficiency
question
Four histologic types account for most primary lung cancers:
answer
1. adenocarcinoma (males 37%, females 47%), 2. squamous cell lung carcinoma (males 32%, females 25%), 3. large cell carcinoma (males 18%, females 10%) 4. small cell carcinoma (males 14%, females 18%).
question
For therapeutic purposes such as staging and treatment, lung cancers are further identified as
answer
non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC).
question
SCLC (small cell lung cancer)
answer
usually metastasize by the time of diagnosis and usually treated with chemotherapy
question
Non-Small Cell Lung Cancers (NSCLC) include
answer
1. Squamous cell carcinoma, related to smoking history 2. adenocarcinoma is the most common sub- type of lung cancer in North America, associated with cigarette smoking is weaker than for squamous cell carcinoma. 3. Large cell carcinomas, poor prognosis
question
manifestations of lung cancer can be divided into 3 categories based on:
answer
(1) those due to involvement of the lung and adjacent structures; (2) the effects of local spread and metastasis; and (3) nonmetastatic paraneoplastic manifestations.
question
earliest symptoms of lung cancer
answer
are chronic cough, shortness of breath, and wheezing because of airway irritation and obstruction.
question
superior vena cava syndrome
answer
an uncommon complication occurs in some persons with mediastinal involvement. Interruption of blood flow in this vessel usually results from compression by the tumor or involved lymph nodes.
question
diagnosis of lung cancer is based on
answer
1. a careful history and physical examination and 2. on other tests such as chest radiography, bronchoscopy, cytologic studies (Papanicolaou [Pap] test) of the sputum or bronchial washings, percutaneous needle biopsy of lung tissue, and scalene lymph node biopsy. 3. Computed tomographic scans, MRI studies, and ultrasonography are used to locate lesions and evaluate the extent of the disease. 4. Positron emission tomography (PET) is a noninvasive alternative for identifying metastatic lesions in the mediastinum or distant sites.
question
Define the term paraneoplastic and cite three paraneoplastic manifestations of lung cancer
answer
Paraneoplastic syndromes are incompletely understood patterns of organ dysfunction related to immune-mediated or secretory effects neoplasia (see Chapter 7). They include hypercalcemia from secretion of parathyroidlike peptide, Cushing syndrome from ACTH secretion, SIADH, neuromuscular syndromes (e.g., Eaton-Lambert syndrome), and hematologic disorders (e.g., migratory thrombophlebitis, nonbacterial endocarditis, disseminated intravascular coagulation).
question
Treatment methods for NSCLC
answer
include surgery, radiation therapy, and systemic chemotherapy.
question
Therapy for SCLC is based on
answer
chemotherapy and radiation therapy.
question
Acute respiratory diseases
answer
are the most common cause of illness in infancy and childhood.
question
Respiratory Obstruction in Children
answer
1. increased airway resistance a. Extrathoracic airways (upper airways) -Prolonged inspiration; inspirational stridor -Inspiratory retractions as ribs are moved outward and body wall does not expand with rib cage 2. Intrathoracic airways (lower airways) -Prolonged expiration with wheezing -Rib cage retractions as ribs are pulled inward, but air does not leave lungs
question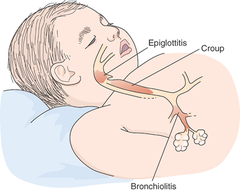
Upper airway Obstructive disorders
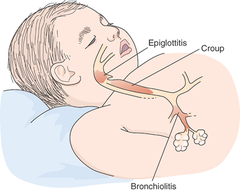
answer
croup epiglottitis
question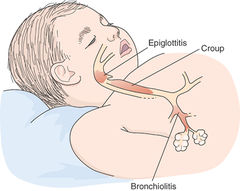
Lower Airway Obstructive disorders
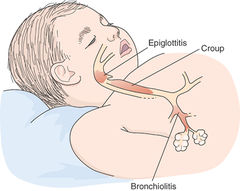
answer
acute bronchilitis
question
Lung development may be divided into four characteristic stages:
answer
1. the embryonic stage = 0-6 weeks of gestation 2. pseudoglandular stage = 6-16 canalicular stage = 6-16 3. Terminal sac (saccular) stage = 24 weeks to birth 4. alveolar stages = 32 weeks to 8 years
question
The first three stages of lung development are devoted to development of the conducting airways, what are they?
answer
-embryonic stage = 0-6 weeks of gestation -pseudoglandular stage = 6-16 -canalicular stage = 6-16
question
last two stages of lung development are devoted to what and what are they called?
answer
-Terminal sac (saccular) stage = 24 weeks to birth -alveolar stages = 32 weeks to 8 years -devoted to the development of the gas exchange portion of the lung. By the 25th to 28th weeks, sufficient terminal sacs are present to permit survival. Before this time, the premature lungs are incapable of adequate gas exchange.
question
Paraneoplastic syndromes are incompletely understood patterns of organ dysfunction related to
answer
immune-mediatedor secretory effects neoplasia. -include hypercalcemia from secretion of parathyroidlike peptide, Cushing syndrome from ACTH secretion, SIADH, neuromuscular syndromes (e.g., Eaton-Lambert syndrome), and hematologic disorders (e.g., migratory thrombophlebitis, nonbacterial endocarditis, disseminated intravascular coagulation).
question
state age for expected survival, including the role of type II alveolar cells and their relation to surfactant
answer
By 28 weeks, the terminal sacs are lined with squamous epithelial cells or type I alveolar cells, across which gas exchange takes place. Scattered among the squamous epithelial cells are rounded secretory epithelial cells-type II alveolar cells. Type II alveolar cells
question
what week do Type II alveolar cells begin to develop in an embryo and what are the functions of the cells?
answer
-begin to develop at approximately 24 weeks. -produce surfactant, a substance capable of lowering the surface tension of the air-alveoli interface
question
causes and manifestations of respiratory distress syndrome (RDS)
answer
The type II alveolar cells that produce surfactant do not begin to mature until approximately the 25th to 28th weeks of gestation; consequently, many premature infants are born with poorly functioning type II alveolar cells and have difficulty producing sufficient amounts of surfactant.
question
Respiratory distress syndrome (RDS), also known

answer
as hyaline membrane disease, is one of the most common causes of respiratory disease in premature infants. In these infants, pulmonary immaturity, together with surfactant deficiency, leads to alveolar collapse
question
Respiratory distress syndrome
answer
is one of the most common causes of respiratory disease in premature infants. In these infants, pulmonary immaturity, together with surfactant deficiency, lead to alveolar collapse.
question
In respiratory disorders that decrease lung compliance
answer
the diaphragm must generate more negative pressure; as a result, the compliant chest wall structures are sucked inward, producing abnormal inward movements of the chest wall during inspiration called retractions.
question
Normally, both an infant's chest wall and lungs are compliant
answer
allowing for small changes in inspiratory pressure to inflate the lung.
question
Children with restrictive lung disorders, such as pulmonary edema or respiratory distress syndrome, breathe at faster or slower rates, and are their respiratory excursions shallow?
answer
breathe at faster rates, and their respiratory excursions are shallow.
question
Grunting
answer
is an audible noise emitted during expiration. An expiratory grunt is common as the child tries to raise the end-expiratory pressure to maintain airway patency and prolong the period of oxygen and carbon dioxide exchange across the alveolar-capillary membrane.
question
Among the respiratory tract infections that affect small children are
answer
1. croup 2. bronchiolitis 3. epiglottitis, a life-threatening supraglottic infection that may cause airway obstruction and asphyxia.
question
Signs of Respiratory Distress and Impending Respiratory Failure in the Infant and Small Child
answer
1. Severe increase in respiratory effort, including severe retractions or grunting, decreased chest movement. 2. Cyanosis that is not relieved by administration of oxygen (40%) 3. Heart rate of 150 per minute or greater and increasing bradycardia 4. Very rapid breathing (rate 60 per minute from birth to 6 months of age, or above 30 per minute in children 6 months to 2 years) 5. Very depressed breathing (rate 20 per minute or below) 6. Retractions of the supraclavicular area, sternum, epigastrium, and intercostal spaces 7. Extreme anxiety and agitation 8. Fatigue 9. Decreased level of consciousness
question
cause and manifestations of respiratory distress syndrome (RDS)
answer
1. Surfactant synthesis is influenced by several hormones, including insulin and cortisol. Insulin tends to inhibit surfactant production; this explains why infants of insulin-dependent diabetic mothers are at increased risk for development of RDS. 2. Cortisol can accelerate maturation of type II cells and formation of surfactant - The reason that premature infants born by cesarean section presumably are at greater risk for development of RDS is that they are not subjected to the stress of vaginal delivery, which is thought to increase the infants' cortisol levels. These observations have led to administration of corticosteroid drugs before delivery to mothers with infants at high risk for development of RDS.
question
Infants with RDS present with multiple signs of respiratory distress, usually within the first 24 hours of birth.
answer
cyanosis difficulty breathing retraction of chest wall grunting sounds with expiration Tital volume drops (inspiration/expiration) fatigue
question
The basic principles of treatment for infants with suspected RDS focus on the provision of supportive care, including
answer
gentle handling and minimal disturbance. An incubator or radiant warmer is used to prevent hypothermia and increased oxygen consumption. Continuous cardiorespiratory monitoring is needed. Monitoring of blood glucose and prevention of hypoglycemia are also recommended. Oxygen levels can be assessed through an arterial (umbilical) line or by a transcutaneous oxygen sensor.
question
Bronchopulmonary dysplasia (BPD)
answer
-is a chronic lung disease that occurs in infants, usually preterm infants treated with mechanical ventilation or prolonged oxygen supplementation. -primarily a disease of infants weighing less than 1000 g born at less than 28 weeks' gestation, many of whom have little or no lung disease at birth but develop progressive respiratory failure over the first few weeks of life.
question
how may respiratory distress syndrome lead to bronchopulmonary dysplasia (BPD)?
answer
Several clinical features, including immaturity, acquired infections, and malnutrition, may contribute to the development of BPD.
question
Bronchopulmonary dysplasia
answer
is characterized by chronic respiratory distress, persistent hypoxemia when breathing room air, reduced lung compliance, increased airway resistance, and severe expiratory flow limitation.
question
The treatment of BPD includes
answer
nutritional support, maintenance of adequate oxygenation, and prompt treatment of infections. if severe may requires mechanical ventilation and administration of supplemental oxygen.
question
In infants and children, obstruction of the upper airways because of infection tends to
answer
exert its greatest effect during the inspiratory phase of respiration.
question
Grunting - what is the physioligic basis in respiratory distress in infants and small children?
answer
-is common as the child tries to raise the end-expiratory pressure to maintain airway patency and prolong the period of oxygen and carbon dioxide exchange across the alveolar-capillary membrane.
question
Nasal flaring - what is the physioligic basis in respiratory distress in infants and small children?
answer
-(enlargement of the nares) is a method that infants use to take in more air. This method of breathing increases the size of the nares and decreases the resistance of the small airways. - helps reduce the nasal resistance and maintain airway patency. It can be a sign of increased work of breathing and is a significant finding in an infant.
question
Inspiratory retractions - what is the physioligic basis in respiratory distress in infants and small children?
answer
-are abnormal inward movements of the chest wall during inspiration; they may occur intercostally (between the ribs), in the substernal or epigastric area, and in the supraclavicular spaces
question
Stridor- what is the physioligic basis in respiratory distress in infants and small children?
answer
In conditions such as croup, the pressures distal to the point of obstruction must become more negative to overcome the resistance; this causes collapse of the distal airways, and the increased turbulence of air moving through the obstructed airways produces an audible crowing sound called stridor during inspiration.
question
some Upper Airway in Infections in Children
answer
croup spasmodic croup Epiglottitis Laryngotracheobronchitis
question
Croup is characterized and caused by
answer
by inspiratory stridor, hoarseness, and a barking cough. cry of the crow or raven. caused by viruses Viral croup usually is seen in children 3 months to 5 years of age. -usually are preceded by upper respiratory infections that cause rhinorrhea (i.e., runny nose), coryza (i.e., common cold), hoarseness, and a lowgrade fever.
question
some Lower Aireway Infections are
answer
Acute bronchiolitis ; asthma
question
Acute bronchiolitis
answer
- is a viral infection of the lower airways, most commonly caused by the respiratory syncytial virus. - produces inflammatory obstruction of the small airways and necrosis of the cells lining the lower airways. It usually occurs during the first 2 years of life, with a peak incidence between 3 and 6 months of age.
question
Children with impending respiratory failure due to airway or lung disease have signs/symptoms of
answer
- rapid breathing; - retractions, which are more pronounced in the child than in the adult because of higher chest compliance; - nasal flaring; and - grunting during expiration.



