CCFP – Flashcard
Unlock all answers in this set
Unlock answersquestion
What is Beck's Triad? What condition is it seen with?
answer
1) Hypotension 2) Distended Jugular Veins 3) Muffled Heart Sounds Cardiac Tamponade
question
What are the four indications for endotracheal intubation in order of urgency?
answer
1) Obtain/Maintain an airway 2) Optimize oxygenation and/or ventilation 3) Failure to protect the airway 4) Predicted clinical course
question
What is the toxic dose of lidocaine with epinephrine?
answer
5-7 mg/kg
question
What are common symptoms associated with migraine without aura?
answer
Remember the POUND mnemonic: Pulsatile Onset (4-72 hours) Unilateral Nausea or vomiting Disabling intensity In the primary care setting 4 out of 5 of the above symptoms is associated with a 92% probability of migraine, 62% with 3 out of 5 and 18% with 2/5 Other symptoms include exacerbation with physical activity, photosensitivity, and sensitivity to noise or smell First Aid for the Family Medicine Boards 2 e.
question
What is an aura in the setting of migraine? What are some examples of aura in "classic migraine"?
answer
An aura is a reversible symptom indicative of focal cerebral dysfunction. Examples include gradual onset and spread of scotomas, scintillations, and/or hemianopic visual field defects; unilateral parenthesias or numbness; unilateral weakness; and speech disturbances First Aid for the Family Medicine Boards 2 e.
question
What is the differential diagnosis of migraine?
answer
Other forms of headache (tension, cluster) Intracranial mass Temporal Arteritis Sinusitis Subarachnoid Hemmorrhage Pseudotumour Cerebri (Idiopathic Intracranial Hypertension) Transient Ischemic Attack (TIA) First Aid for the Family Medicine Boards 2 e.
question
What classes of medications can be used for the acute and prophylactic management of migraine?
answer
Acute: NSAIDs Acetaminophen Triptans Ergotamines Narcotics Anti-emetics Prophylaxis: Beta-blockers Calcium Channel Blockers Tricyclic Antidepressants Anticonvulsants Methysergide First Aid for the Family Medicine Boards 2 e.
question
What is the most common type of headache?
answer
Tension Headache First Aid for the Family Medicine Boards 2 e.
question
What are the typical symptoms of a tension headache?
answer
Bandlike distribution of pain in the frontal and occipital regions Exacerbated by stress, fatigue, glare or noise Contraction of the scalp and posterior neck muscles Normal neurological exam First Aid for the Family Medicine Boards 2 e.
question
What is the acute and prophylactic treatment of tension headaches?
answer
Acute: Aspirin NSAIDs Ergotamines Prophylaxis: Tricyclic Antidepressants SSRIs Beta Blockers Relaxation Techniques First Aid for the Family Medicine Boards 2 e.
question
What are the symptoms of cluster headache?
answer
Recurrent, unilateral, excruciating peri-orbital headache Lasts 15 minutes to 3 hours Headaches are non-pulsatile, constant and frequently occur at night Associated Horner syndrome Ipsilateral conjunctival injection Lacrimation Nasal congestion Clusters typically take place in groups over days to weeks (occur at the same time of day in the same location) Normal neurological exam First Aid for the Family Medicine Boards 2 e.
question
What is the differential for cluster headaches?
answer
Migraine Glaucoma Sinusitis Uveitis Trigeminal Neuralgia First Aid for the Family Medicine Boards 2 e.
question
What is the acute and prophylactic treatment of cluster headache?
answer
Acute: 100% O2 Triptans Ergotamine Intranasal Lidocaine Butorphanol Prophylaxis: Avoid triggers (alcohol, stress, and medications causing vasodilation) For short term prevention of recurrences a prednisone taper can be considered Ergotamines Valproate CCBs Lithium Methysergide First Aid for the Family Medicine Boards 2 e.
question
What are two potential complications arising from cluster headaches?
answer
Horner Syndrome Suicide (from intolerable pain) First Aid for the Family Medicine Boards 2 e.
question
How will you treat a suspected analgesic overuse headache (acute and prophylactic)?
answer
Discontinue all analgesics causing the rebound headaches Acute: Triptans Prednisone Ergotamines Prophylaxis: TCAs SSRIs Beta-blockers Anticonvulsants Avoid headache triggers Stretching, aerobic exercise and relaxation techniques may be of benefit First Aid for the Family Medicine Boards 2 e.
question
What proportion of patients with analgesic overuse headache will relapse into analgesic overuse patterns?
answer
1/3 of patients First Aid for the Family Medicine Boards 2 e.
question
What is the time cut-off for determining whether a post-traumatic headache is acute or chronic?
answer
Acute cases last less than 8 weeks and typically begin 8 weeks. First Aid for the Family Medicine Boards 2 e.
question
What is Temporal Arteritis?
answer
A treatable neurological emergency characterized by sub-acute inflammation of the external carotid arterial system and vertebral arteries First Aid for the Family Medicine Boards 2 e.
question
What is the most common patient population to develop Temporal Arteritis?
answer
Women over 50 years of age First Aid for the Family Medicine Boards 2 e.
question
Want are some symptoms and exam findings seen in Temporal Arteritis?
answer
New temporal or diffuse headache with associated transient visual loss, jaw claudication, and scalp tenderness Temporal arteries that are dilated, tender, thickened, or non-pulsatile Pale optic disc on affected side on fundoscopy (rare) Cranial neuropathies (rare) PMR symptoms may also be present including: Fever Myalgias Malaise Anorexia Anemia Weight Loss Tenderness and stiffness in the shoulders and hips First Aid for the Family Medicine Boards 2 e.
question
What percentage of patients with Temporal Arteritis have Polymyalgia Rheumatica?
answer
50% First Aid for the Family Medicine Boards 2 e.
question
What is the treatment for Temporal Arteritis?
answer
Prednisone 60 mg daily for 1-2 months then slow taper Monitoring of symptoms and ESR Aspirin (reduces risk of stroke and visual loss) First Aid for the Family Medicine Boards 2 e.
question
What percent of untreated Temporal Arteritis will suffer permanent vision loss?
answer
50%, with 1/2 of those affected patients experiencing bilateral loss Untreated patients are also at increased risk of cranial neuropathy, TIA, stroke, and thoracic artery aneurysm First Aid for the Family Medicine Boards 2 e.
question
What symptoms and exam findings would you expect to see in Benign/Idiopathic Intracranial Hypertension?
answer
Diffuse headaches worse with straining Associated visual loss Diplopia Transient visual obscurations Limited abduction of one or both eyes (CN VI palsy) Decreased LOC Papilledema on fundoscopy Increased physiological blind spot Decreased visual fields and visual acuity (severe cases) First Aid for the Family Medicine Boards 2 e.
question
If you're clinically suspecting Idiopathic Intracranial Hypertension what tests must be included in your workup? What findings would you expect to see?
answer
To evaluate a concern for increased ICP a CT/MRI and LP must be done Head CT or MRI may be normal or may show small ventricles or an empty sella LP shows elevated opening pressure with a normal CSF profile CT angiography or MRV should show no dural sinus thrombosis First Aid for the Family Medicine Boards 2 e.
question
What are the most common risk factors for developing Idiopathic Intracranial Hypertension?
answer
Remember the 4 F's: Fat Female Fertile Forty (usually under 40) Similar risk factors for cholelithiasis First Aid for the Family Medicine Boards 2 e.
question
What is the treatment for Idiopathic Intracranial Hypertension?
answer
Acetazolamide +/- diuretic Discontinue contributing medications or excessive vitamin A Weight loss Repeated LPs or lumboperitoneal shunting for refractory cases First Aid for the Family Medicine Boards 2 e.
question
What percentage of tear drainage is accomplished by the upper collecting system?
answer
25% The majority is accomplished by the lower system (75%), however, damage to the upper can still cause clinically significant dysfunction Dr. T. Buglass
question
You see a patient with an acute red, painful eye with a dilated pupil, what is the first condition you should rule out?
answer
Acute angle closure glaucoma If you see the same presentation with a constricted pupil think anterior uveitis Dr. T. Buglass
question
What are two situations where getting a visual acuity should not be your first priority in a patient with an ocular complaint?
answer
A visual acuity should be documented on all patients with an ocular complaint but can be delayed if there is: 1) Chemical burn - start irrigation immediately 2) Severe trauma - hyphema, lacerated globe, etc.) Dr. J. Cross
question
When should you avoid using fluorescein during an ocular examination?
answer
All patients should get fluorescein staining as part of a complete ocular examination except for pediatric patients with obvious purulent conjunctivitis Remember to remove contact lenses first as fluorescein will cause permanent staining Dr. J. Cross
question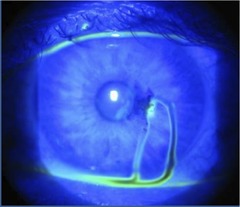
You add fluorescein to the eye with the patient sitting upright and see this, what is the name of this test? What does it represent? What is the next step in management?
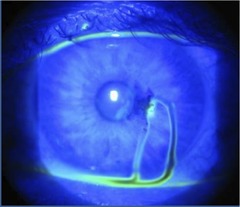
answer
Seidl's test (in this case it's positive), this represents a full thickness corneal perforation and warrants an immediate ophthalmology consult Dr. J. Cross
question
What is causing these vertical corneal abrasions? How will you confirm and treat?
answer
A sub-tarsal foreign body, always remember to evert the eyelids (upper and lower) with a Q-tip (consider double eversion with a paperclip), if foreign body is present try to remove by gently wiping with a Q-tip Dr. J. Cross
question
What must be excluded with a conjunctival abrasion/foreign body?
answer
An intra-ocular foreign body with orbital X-ray or CT scan, consider the same if there is a corneal abrasion and a history of the patient pounding metal on metal Dr. J. Cross
question
What is the diagnosis? What symptoms and exam findings would you expect? How would you treat this patient?
answer
Welder's Flash Symptoms include: Decreased vision Injected conjunctiva Diffuse punctate corneal lesions with a discrete lower border (protected by the lower lid) Treat with topical NSAIDs, erythromycin ointment/drops (consider ciprofloxacin for prophylaxis in contact lens wearers, consider ophthalmology referral), no role for cycloplegics Dr. J. Cross
question
When should corneal abrasions be referred to ophthalmology?
answer
"Large" abrasions Obscuring central visual axis Increasing in size or worsening symptoms on follow up Developing corneal infiltrate or ulcer Post-Lasik abrasions Dr. J. Cross
question
Patient had Lasik 7 years ago and is now presenting with eye pain following trauma? What is the most important diagnosis to exclude? What is the treatment of choice for this condition?
answer
Lasik flap dislocation (can occur up to 14 years after Lasik procedure), this should be referred immediately to ophthalmology for stromal scraping +/- flap replacement Dr. J. Cross
question
Patient is known to smoke crack cocaine regularly, what is the pathophysiology of development of corneal abrasions in patients with crack eye?

answer
Lack of pain perception (cocaine is a topical anesthetic) Direct toxic effect Rubbing from smoke irritation Chemical burns Decreased blink rate Dr. J. Cross
question
What are some common symptoms and exam findings of anterior uveitis? When should this patient be referred to ophthalmology?
answer
Pain Red eye/conjunctival injection Tearing Decreased vision Cells and flare in the anterior chamber Limbic injection Irregular pupil (posterior synechiae) WBC clumps on posterior corneal surface Sterile hypopon (severe cases) All cases should be referred to ophthalmology Dr. J. Cross
question
What patients with a corneal foreign body require ophthalmology referral?
answer
Deep corneal stromal foreign body Those involving the central visual axis Dr. J. Cross
question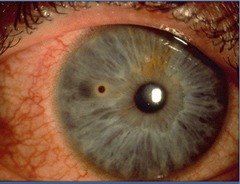
Patient had a corneal foreign body removed yesterday, they have returned today for follow-up, what is the diagnosis? How and when will you treat?
answer
Residual rust ring Wait 24-48 hours to remove (rust solidifies). Remove under slit lamp guidance use 25G needle or eye spud to remove with topical anesthesia Dr. J. Cross
question
What percentage or intra-orbital foreign bodies will be missed on orbital X-ray?
answer
Over 60% of foreign bodies, Orbital CT is the test of choice but can miss organic and small metal foreign bodies, an orbital MRI should be ordered if CT is negative and there is still clinical suspicion Dr. J. Cross
question
What intra-orbital foreign bodies can be left in situ?
answer
BBs Small fragments of metal (excluding copper) Metallic shrapnel Dr. J. Cross
question
What do you need to exclude in this laceration
answer
You need to exclude damage to the globe and the nasolacrimal system, this can be accomplished by checking for pooled tears in the lacrimal duct with fluorescein staining. If there is suspicion of nasolacrimal involvement consult ophthalmology Dr. J. Cross
question
What lacerations in the peri-orbital region should be referred to ophthalmology?
answer
Lid margin involvement Protruding fat Tarsal plate involvement Nasolacrimal injury Dr. J. Cross
question
What length cut-off of conjunctival lacerations can be ignored and treated with topical antibiotics?
answer
Lacerations less than 1 cm can be left alone and treated with topical antibiotics, lacerations > 1 cm need to be referred to ophthalmology for surgical repair Dr. J. Cross
question
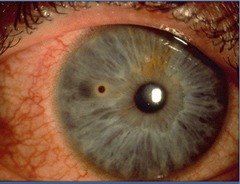
What is the diagnosis? What is the pathophysiology? If caused by an underlying injury what percentage of patients will have increased IOP? What percentage of patients will have a worse re-bleed in the next 7 days?
answer
Hyphema, which is caused by blood in the anterior chamber. If caused by blunt trauma 1/3 will have increased IOP on initial examination. 20-30% of patients will have a worse re-bleed in the next 7 days Dr. J. Cross
question
What is the treatment for hyphema? What patients require admission? How does this differ if it is a pediatric patient?
answer
Elevate the head of the bed to 30º Avoid ASA and NSAIDs Ophthalmology Admit patients if: Re-bleeding Occupying >50% of anterior chamber Decreased vision Non-compliance suspected In all pediatric patients with hyphema, child abuse must be investigated thoroughly
question
What classes of drugs can cause bladder outlet obstruction?
answer
Sympathomimetics or anticholinergics (stimulate alpha-agonistic fibers of the bladder neck)
question
What is Alvarado's score?
answer
A 10-point scoring system used to predict appendicitis. 8 or greater is 96% sensitive, score of 37.3 ºC (1) WBC > 10,000 (2) Left shift >75% PMN's (1)
question
What is the underlying mechanism that causes an allergic reaction? What are the common substances that cause allergic reactions?
answer
Usually IgE mediated - exposure, sensitization, re-exposure triggers reaction Can also be caused by a direct trigger (e.g., contrast dye) Common substances that cause allergies include: Insect stings Medications Latex Food (e.g., peanuts, tree nuts [walnuts, hazelnuts, almonds, cashews, pecans], shellfish/fish, milk, eggs, and wheat) Family Medicine Notes, 3 e. (2015)
question
What are the clinical features of an allergic reaction? What are the complications?
answer
The clinical features of an allergic reaction include: General - anxiety, tremor Skin - urticaria, edema, erythema, pruritus Respiratory - SOB, sensation of throat tightness, cough, wheezes, stridor, sneezing Eyes - itching, tearing CVS - hypotension, tachycardia, arrhythmia, MI GI - abdominal pain, nausea/vomiting Some complications resulting from an allergic reaction include: Cardiovascular collapse Airway obstruction Death Family Medicine Notes, 3 e. (2015)
question
What are the principles of emergency management of an anaphylaxis? What is the adult and pediatric doses of epinephrine used?
answer
The principles of emergency management of an allergic reaction include: Remove the causative agent (if possible) ABCs, fluid resuscitation Epinephrine Benadryl 50 mg IV/IM q 4-6 hours Methylprednisolone 50-100 mg IV depending on severity Ventolin if bronchospasm is present Glucagon if the patient is on a beta-blocker and hypotensive The doses of epinephrine used for treating anaphylaxis are as follows: On scene - Epi-pen if available Moderate reaction (minimal airway edema, mild bronchospasm, skin reaction) - Adults: 0.3 - 0.5 mL 1:1000 IM - Pediatrics: 0.01 mL/kg (up to 0.4 mL) 1:1000 IM Severe reaction (laryngeal edema, severe bronchospasm, shock) - Adults: 1 mL 1:10000 IV or ETT - Pediatrics: 0.01 mL/kg IV or ETT Family Medicine Notes, 3 e. (2015)
question
What is the incidence of biphasic reactions following anaphylaxis? What can be used to prevent this?
answer
The incident of a biphasic reaction is 20% Corticosteroids are used to prevent a biphasic reaction Family Medicine Notes, 3 e. (2015)
question
What are the management principles of angioedema/urticaria?
answer
The principles of management of angioedema/urticaria are: Epinephrine Anti-histamines Steroids (may or may not be beneficial) Airway management (if necessary) Family Medicine Notes, 3 e. (2015)
question
What are the principles for post-emergency management of an anaphylactic reaction?
answer
The principles for post-emergency management of anaphylaxis includes: Consider 4 day course of prednisone + diphenhydramine Remain with someone who can provide adequate supervision x 48 hours If uncertain cause refer to allergist Ensure patient has Epi-pen and knows how to use it (inject into outer thigh muscle at first sign of swelling of throat, tongue or other reaction (e.g., breathlessness) Make sure they have enough Epi-pens available for use (e.g., school, car, work, etc.) If Epi-pen is used see MD immediately Suggest medic alert bracelet Document allergy in chart Family Medicine Notes, 3 e. (2015)
question
What are the 4 main principles for treatment of allergic rhinitis? What options are available for pharmacological treatment?
answer
The 4 main principles of allergic rhinitis include: 1) Appropriate explanation, sources of allergens 2) Allergen avoidance 3) Pharmacological treatment 4) Immunotherapy Pharmacotherapy includes: Antihistamines (oral [less effective for runny nose], nasal spray, eye drops [equally effective compared to oral therapy for allergic conjunctivitis]) Decongestants - oral or topical Sodium cromoglycate - nasal spray or eye drops Corticosteroids - intranasal (less effective for non-eosinophilic rhinitis) or oral (very effective if other methods fail) Family Medicine Notes, 3 e. (2015)
question
What are the clinical criteria to diagnose chronic fatigue syndrome?
answer
To diagnose chronic fatigue syndrome the patient must have: Clinically evaluated fatigue that is unexplained x 6 months Symptoms not alleviated by rest Symptoms that impact function They must also have ≥ 4 of the following: Impaired short term memory/concentration leading to decreased function New headache Sore throat Tender cervical/axillary lymph nodes Muscle pain Multi-joint pain without any swelling/erythema Unrefreshing sleep Post-exertional malaise > 24 hours Family Medicine Notes, 3 e. (2015)
question
What is the differential of fatigue?
answer
The differential for fatigue can be remembered with the mnemonic SO FATIGUED: Substance abuse Obstructive sleep apnea Failure (CHF) Anemia Tumor (malignancy) Infection (e.g., TB) GI (e.g., malabsorption) Uremia Endocrine (e.g., DM, hypothyroid) Depression Family Medicine Notes, 3 e. (2015)
question
What is the differential of fatigue by system?
answer
The differential of fatigue by system includes: Cardiorespiratory - CHF, COPD, OSA Endocrine - DM, hypothyroid, Addison's Gastrointestinal - Celiac disease, chronic liver disease, biliary cirrhosis, malignancy Hematology - Anemia, autoimmune, hemochromatosis, iron deficiency, lymphoma/leukemia Infection - HIV, viral, mononucleosis, viral hepatitis MSK - Rheumatoid arthritis Neurologic - MS, myasthenia gravis, Parkinson's, amyotrophic lateral sclerosis (ALS) Other - Malignancy, lupus Family Medicine Notes, 3 e. (2015)
question
What are some red flags on history for evaluation of fatigue?
answer
Red flags on history when evaluating fatigue include: Fever Weight loss Night sweats Neurologic deficit Family Medicine Notes, 3 e. (2015)
question
What are some point on history that should be taken when evaluating fatigue?
answer
Important historical points when evaluating fatigue include: Level of activity Differentiate between decreased motivation and decreased ability/mental fatigue Onset, duration, timing (a.m., p.m.), exertional Sleep habits, sex, eating, bowels, exercise Associated symptoms (pain, palpitations, syncope, dizziness, SOB, nausea/vomiting, fever, bleeding, cold intolerance, mood) EXCLUDE NEW MEDICATIONS (e.g., amiodarone, anti-histamine, anti-depressants, BP medications, anti-epileptic, herbals) Alcohol/drug use Family Medicine Notes, 3 e. (2015)
question
What is the differential diagnosis for anxiety?
answer
The differential diagnosis for anxiety includes: Endocrinology - hyper/hypothyroid, hypoglycemia, adrenal insufficiency, menopause Cardiovascular - CHF, arrhythmia, mitral valve prolapse, angina Respiratory - asthma, COPD, pneumonia, pulmonary embolism Metabolic - DM, porphyria CNS - vestibular dysfunction, temporal lobe epilepsy, migraines, dementia, neoplasm GI - peptic ulcer, IBS Hematology - vitamin B12 deficiency, anemia Exposure/drugs - lead, stimulants (caffeine, nicotine), EtOH, illicit drugs Psychiatric - psychosis, depression, hypochondriasis, substance abuse Family Medicine Notes, 3 e. (2015)
question
What is the prevalence of anxiety? Is it more pre-dominant in males or females? What are some risk factors for developing anxiety?
answer
Lifetime prevalence of anxiety is 10-30%, more common in females than males Risk factors include: Family history Childhood/adolescent anxiety (including marked shyness) Stress Abuse Family Medicine Notes, 3 e. (2015)
question
What should be included in a work-up for anxiety to rule out other causes?
answer
A thorough work-up for anxiety would include: CBC Fasting blood glucose Lipids Electrolytes Bilirubin Creatinine Urinanalysis TSH Vitamin B12 Drug screen (if warranted) ECG (if > 40 years old) Family Medicine Notes, 3 e. (2015)
question
What are some of the main components of cognitive behavioural therapy (CBT) for anxiety?
answer
Some of the main components of CBT for anxiety include: 1) Exposure - encourage patients to face fears, learn corrective experience, extinction of fear through repeated exposures 2) Safety response inhibition - restrict usual anxiety-reducing behaviours (e.g., escape, need for reassurance) 3) Cognitive strategies - cognitive restructuring, behavioural experiments 4) Arousal management - relaxation and breathing control skills to help control increased anxiety levels 5) Surrender of safety signals - patient relinquishes safety signals (e.g., presence of a companion, knowledge of location of nearest exit) Family Medicine Notes, 3 e. (2015)
question
What are the diagnostic criteria for generalized anxiety disorder?
answer
The diagnostic criteria for GAD are: Uncontrollable and excessive worry occurring more days than not for at least 6 months about a number of everyday, ordinary experiences or activities AND 3 or more of the following symptoms (SICK FM): Sleep disturbance Irritable Concentration poor or mind goes blank Keyed up or restless or on edge Fatigued easily Muscle tension Family Medicine Notes, 3 e. (2015)
question
What is the principle of management for GAD? What are some treatment options? How long should they be continued for? What is the relapse rate?
answer
The main principle of management is CBT ± pharmacological management Some options for medications include: First Line: Duloxetine 60-120 mg Escitalopram 10-20 mg Paroxetine 20-60 mg Sertraline 50-200 mg Venlafaxine 75-375 mg Second Line: Bupropion 150-300 mg Imipramine 150-300 mg Quetiapine 25-50 mg It is recommended patients continue on treatment for > 1 year, the relapse rate is 20-40% Family Medicine Notes, 3 e. (2015)
question
Before what gestational age is a pregnancy loss considered an abortion? What are the main categories of spontaneous abortion and what defines them?
answer
Abortion is said to have occurred if pregnancy loss has occurred before 20 weeks gestation The different categories of spontaneous abortion include: Inevitable - cervix dilated, no products expelled Incomplete - some but not all products expelled, retained products Complete - all products of conception expelled Missed - fetal demise but no uterine activity Recurrent/Habitual - ≥ 3 consecutive pregnancy losses Septic - spontaneous abortion complicated by uterine infection Family Medicine Notes, 3 e. (2015)
question
What percent of pregnancies will have bleeding before 20 weeks GA? What percent of all pregnancies will end in spontaneous abortion?
answer
20% of pregnancies will have bleeding before 20 weeks gestation 10% of all known pregnancies will end in spontaneous abortion Family Medicine Notes, 3 e. (2015)
question
What are the risk factors for a spontaneous abortion?
answer
Risk factors for spontaneous abortion include: Advanced maternal age Thrombophilia, autoimmune disease (anti-phospholipid antibody syndrome Infection (BV, HSV, toxoplasmosis, listeriosis, chlamydia, HIV, syphilis, parvovirus B19, malaria, rubella, gonnorhea, CMV) Previous SA Conception within 3-6 months of previous delivery Intrauterine device Multiple previous therapeutic abortions Uterine abnormalities (adhesions, leiomyoma) Teratogen use (misoprostol, retinoids, MTX, NSAIDs) Smoking, cocaine, EtOH, heavy caffeine use, toxin exposure (arsenic, lead, ethylene glycol, carbon disulfide, heavy metals, organic solvents) Family Medicine Notes, 3 e. (2015)
question
What investigations should be ordered for a suspected spontaneous abortion?
answer
Investigations that should be ordered include: ß-HCG (increase in 66% within 48 hours - likely viable) CBC Group and screen (If Rh negative administer Anti-D) Pelvic U/S (FHR, tissue, free fluid) Consider gonnorhea and chlamydia Family Medicine Notes, 3 e. (2015)
question
What is the differential diagnosis of a spontaneous abortion?
answer
The differential diagnosis of SA includes: Cervical abnormality (e.g. polyp, malignancy, friability, trauma) Ectopic pregnancy Infection Molar pregnancy Sub-chorionic hemmorhage Vaginal trauma Family Medicine Notes, 3 e. (2015)
question
What are the principles of management of a spontaneous abortion?
answer
The principles of management of a SA include: Expectant management (effective 82-96% of the time within 2 weeks) Misoprostol 800 mcg PV and then repeat in 24-72 hours later if no bleeding (PO less effective and more side effects) WinRho if Rh- Vacuum aspiration if hemodynamically unstable (e.g. peritoneal signs) or septic (e.g., fever), or by patient choice (risks include uterine adhesions, anesthetic risks, effective 97% of the time and often has less bleeding) Family Medicine Notes, 3 e. (2015)
question
What is the dose of WinRho for a patient having a spontaneous abortion if they are Rh- and the fetus is < 12 weeks GA? What about if ≥ 12 weeks GA?
answer
The dose of WinRho for Rh- women having a spontaneous abortion is 120 mcg IM if they are less than 12 weeks GA. The dose is increased to 300 mcg if the GA is ≥ 12 weeks Family Medicine Notes, 3 e. (2015)
question
If you are clinically suspecting a septic abortion what antibiotics should you initiate? What are the common bacteria that cause a septic abortion
answer
If you clinically suspect a septic abortion IV broad spectrum antibiotics should be initiated such as clindamycin and gentamicin The most common bacteria causing a septic abortion include S. aureus, gram negative bacilli and gram positive cocci Family Medicine Notes, 3 e. (2015)
question
What are the indications for induction of labour?
answer
The indications for induction of labour include: Overdue/post-dates - offered to patients between 41-42 weeks GA (due to increased risk of poor blood supply and still birth > 42 weeks, **reliable dates are essential) Pre-eclampsia (increased BP, proteinuria, swelling of hands/feet) IUGR/decreased fetal movement Maternal conditions (e.g., DMII, renal/pulmonary disease, pregnancy induced HTN) Spontaneous ROM Other (e.g., antiphospholipid antibody syndrome, chorioamnionitis, abruption, fetal death) The following are NOT indications for induction of labour: Macrosomia (III-D) Patient preference (III-D) Family Medicine Notes, 3 e. (2015)
question
What are the risks of induction of labour?
answer
The risks of induction of labour include: Increased risk of operative vaginal delivery and C/S Abnormal FHR Uterine rupture Cord prolapse Wrong dates leading to pre-term delivery of infant Family Medicine Notes, 3 e. (2015)
question
What are the contraindications to induction of labour?
answer
The contraindications to induction of labour are the same as for normal labour/vaginal delivery and include: Previous uterine rupture Fetal transverse lie Placenta previa/vasa previa Invasive cervical cancer Active genital herpes
question
What factors make up the Bishop's score? What is the cut-off for determining if the cervix is favourable?
answer
The Bishop's score is used to determine how favourable the cervix is prior to initiation of induction of labour and involves 5 factors: 1) Dilation (cm): 0 cm (0), 1-2 cm (1), 3-4 cm (2), 5-6 cm (3) 2) Effacement (%): 0-30% (0), 40-50% (1), 60-70% (2), 80% (3) 3) Station: -3 (0), -2 (1), -1/0 (2), +1/+2 (3) 4) Consistency: firm (0), medium (1), soft (2) 5) Position: posterior (0), mid (1), anterior (2) A Bishop's score > 6 indicates a favourable cervix Family Medicine Notes, 3 e. (2015)
question
What are the three main options for inducing labour?
answer
The three main options for inducing labour include: 1) Cervical ripening (Bishop's score 120 seconds), normal FHR then decrease dose If increased uterine activity and NRFHR reposition mother, check BP, initiate/increase IVF, rule out cord prolapse, O2, discontinue oxytocin 3) Artificial rupture of membranes Wait until active labour and head engaged Family Medicine Notes, 3 e. (2015)
question
How should a patient be managed if they are experiencing increased uterine activity while undergoing induction of labour with oxytocin?
answer
In the case of increased uterine activity during induction of labour with oxytocin the following management should take place: If increased uterine activity (5-10 minutes or lasting > 120 seconds), normal FHR then decrease dose If increased uterine activity and NRFHR reposition mother, check BP, initiate/increase IVF, rule out cord prolapse, O2, discontinue oxytocin Family Medicine Notes, 3 e. (2015)
question
Labour at what gestational age is considered pre-term labour? What investigations should be ordered if pre-term labour is suspected?
answer
Pre-term labour is classified as labour occurring at any gestational age between 20-37 weeks Investigations that should be ordered if pre-term labour is suspected include: Fetal fibronectin (positive = > 50 ng/mL, high NPV) Ultrasound for cervical length (cervical length > 30 mm has high NPV for PTL before 34 weeks) A negative fetal fibronectin and cervical length > 30 mm pre-term labour is highly unlikely Family Medicine Notes, 3 e. (2015) Toronto Notes 2011
question
What are the principles of management for pre-term labour (PTL)?
answer
The principles of management for pre-term labour (PTL) include: Betamethasone (if ≤ 34 weeks) 12 mg IM q24 hours x 2 doses No PV exams Bed rest Transfer to tertiary hospital (NICU capabilities) Cervical cerclage (primary cervical incompetence) Tocolytics - usually only used to allow Betamethasone to act and/or transfer the patient to a tertiary care hospital Family Medicine Notes, 3 e. (2015)
question
What tocolytics have the best evidence supporting their use?
answer
Tocolytics that have the best evidence supporting their use include: Calcium channel blockers (Nifedipine) Prostaglandin synthesis inhibitors (Indomethacin) Tocolytics that have no evidence of efficacy include: Nitroglycerin patch (vasodilator and smooth muscle relaxant) Magnesium sulfate Family Medicine Notes, 3 e. (2015)
question
If suspecting premature rupture of membranes (PROM) what should be included in your physical examination? If ≥ 37 weeks GA how will you manage this patient?
answer
If you are suspecting PROM the following should be included in your physical examination: Sterile speculum (rule out cord prolapse, confirm rupture of membranes/presence of amniotic fluid) NO bimanual examinations (risk of introducing infection) If the pregnancy is ≥ 37 weeks and has PROM the following management should occur: Check GBS status (if positive start antibiotics, if unknown/negative start if ROM > 18 hours) If term and GBS negative can wait up to 24 hours before starting induction of labour (risk of sepsis outweighs risk of induction) Family Medicine Notes, 3 e. (2015)
question
What are some tests to determine/confirm if the membranes have ruptured?
answer
Some confirmatory tests for ruptured membranes include: Pooling of fluid in the posterior fornix on speculum exam "Cascade"/gush of fluid from cervix with cough/Valsalva Nitrazine (turns nitrazine paper blue due to increased pH) - low specificity, can be positive with blood, urine, semen "Ferning" under microscopy - high salt in amniotic fluid, fluid evaporates salt residue resembles "fern" leaves Decreased amniotic fluid volume on ultrasound Family Medicine Notes, 3 e. (2015) Toronto Notes 2011
question
What/when is the "grey-zone" for management of PPROM?
answer
The "grey-zone" for management of PPROM occurs between 34-36 weeks when the risk of death to the fetus from sepsis is equal to the risk of death from respiratory complications Toronto Notes 2011
question
What is placental abruption? What is the incidence of placental abruption?
answer
Placental abruption is premature separation of the placenta after 20 weeks gestation The incidence of placental abruption is 1-2% of all pregnancies Family Medicine Notes, 3 e. (2015)
question
What are some risk factors for placental abruption?
answer
The risk factors for placental abruption include: Previous placental abruption (recurrence 5-16%) Hypertension Vascular disease Smoking > 1 PPD Excessive EtOH Multiparity Increased maternal age PPROM Rapid decompression of distended uterus (e.g., polyhydramnios, multiple gestation) Uterine anomalies/fibroids Trauma Family Medicine Notes, 3 e. (2015)
question
What are the signs and symptoms of placental abruption?
answer
The signs and symptoms of placental abruption include: Painful vaginal bleeding Sudden onset, constant pain localized to lower back and uterus Fetal distress Bloody amniotic fluid Fetal demise (15%) Family Medicine Notes, 3 e. (2015)
question
What are the complications associated with placental abruption?
answer
Complications of placental abruption can be both fetal and maternal: Fetal: Fatal (25-60%) Prematurity Hypoxia Maternal: Fatal (< 1%) DIC Acute renal failure Anemia Shock Pituitary necrosis (Sheehan syndrome) Amniotic fluid embolism Family Medicine Notes, 3 e. (2015)
question
What is the most common cause of DIC in pregnancy?
answer
Placental abruption is the most common cause of DIC in pregnancy Toronto Notes 2011
question
What is the incidence of uterine rupture? What are risk factors for uterine rupture?
answer
The incidence of uterine rupture is 0.5-0.8% but can be as high as 12% in patients with prior classical C-section incisions The risk factors for uterine rupture include: Previous uterine scar (especially classical incisions) Oxytocin Grand multiparity Previous uterine manipulations Family Medicine Notes, 3 e. (2015)
question
What are the signs and symptoms of uterine rupture? What are some complications of uterine rupture?
answer
The signs and symptoms of uterine rupture include: Prolonged fetal bradycardia (most common presentation) Acute onset of abdominal pain Hyper/hypotonic uterine contractions Vaginal bleed Complications of uterine rupture include: Maternal mortality (1-10%) Hemmorhage/shock DIC Amniotic fluid embolism Fetal distress (mortality 50%) Family Medicine Notes, 3 e. (2015)
question
What is the physiological cause of variable decelerations? What is the "rule of 60's"?
answer
Variable decelerations are caused by cord compression during the 2nd stage and are benign unless repetitive, slow recovery, or associated with FHR anomalies The "rule of 60's" is used to rule out worrisome variable decelerations: Deceleration below 60 bpm Lasting > 60 seconds with a slow return to baseline Drop > 60 bpm below baseline Family Medicine Notes, 3 e. (2015)
question
What is the normal rate of cervical dilation in cm/hour for primagravida and multiparous women? What is the definition of labour dystocia in the 1st stage of labour? What is the definition of dystocia in the 2nd stage of labour?
answer
The normal rate of cervical dilation in primagravidas is 1.2 cm/hour, in multiparous women the rate of cervical dilation is 1.5 cm/hour The definition of labour dystocia in the 1st stage of labour is 1 hour with no descent during active pushing Family Medicine Notes, 3 e. (2015)
question
What is the etiology of labour dystocia in the 2nd stage?
answer
The etiology of labour dystocia in the 2nd stage can be remembered with the "4 P's": 1) Power - most common, contractions hypotonic or incoordinate, inadequate maternal effort 2) Passenger - fetal position, attitude, size, anomalies 3) Passage - pelvis structure, maternal soft tissue factors (septum) 4) Psyche - stress hormones Family Medicine Notes, 3 e. (2015)
question
What are the management principles for labour dystocia?
answer
The management principles for labour dystocia include: Oxytocin augmentation - useful in protraction of dilation or descent if contractions are inadequate If arrest, likely cephalopelvic disproportion (CPD), needs C-section Prolonged latent phase - think maybe false labour or premature/excess use of sedation/analgesia Family Medicine Notes, 3 e. (2015)
question
What is the cause of shoulder dystocia? What is the incidence of shoulder dystocia? What are some risk factors for shoulder dystocia?
answer
The cause of shoulder dystocia is impaction of the anterior shoulder on the pubic symphysis after delivery of the head (often head to body delivery > 60 seconds) The incidence of shoulder dystocia is 1.5% of all deliveries Risk factors for shoulder dystocia include: Obesity Diabetes mellitus Multiparity Macrosomia Prolonged gestation Prolonged 2nd stage Advanced maternal age Male newborn Induction of labour Family Medicine Notes, 3 e. (2015)
question
What is the classic sign that is seen clinically with shoulder dystocia? What are some complications of shoulder dystocia?
answer
The classic sign seen clinically with shoulder dystocia is the "turtle sign" where the head is delivered but retracts against the inferior portion of the pubic symphysis Complications that can occur as a result of shoulder dystocia include: Chest compression by vagina or cord compression by pelvis can lead to hypoxia, death Maternal perineal injury leading to PPH Uterine rupture Newborn brachial plexus injury - Erb's or Klumpke's paralysis Fetal fracture (clavicle, humerus, C-spine) Family Medicine Notes, 3 e. (2015)
question
What nerve roots are affected with Erb's palsy? What nerves are affected with Klumpke's palsy? What are the classical hand positions seen with each of these palsies? What percent of brachial plexus injuries will resolve within 6 months after delivery?
answer
Erb's palsy affects C5-C7 and has the classic "waiter's tip" hand position Klumpke's palsy affects C8-T1 and has the classic "claw hand" position 90% of brachial plexus injuries following delivery will resolve within 6 months Family Medicine Notes, 3 e. (2015)
question
How do you manage a shoulder dystocia?
answer
The approach to managing a shoulder dystocia can be remembered with the mnemonic "ALARMER": Apply suprapubic pressure/Ask for help Legs in full flexion (McRobert's maneuver) Anterior shoulder disimpaction (suprapubic pressure) Release of the posterior shoulder by rotating it anteriorly with hand in the vagina under adequate anesthesia Manual corkscrew (i.e., rotate the fetus by the posterior shoulder until the anterior shoulder emerges from behind the maternal symphysis) Episiotomy Roll over (on hands and knees) Other options include: Cleidotomy (deliberate fracture of the neonatal clavicle) Zavanelli maneuver - replacement of the fetus into the uterine cavity Symphysiotomy Abdominal incision and shoulder disimpaction via hysterotomy - subsequent vaginal delivery Family Medicine Notes, 3 e. (2015)
question
What percent of shoulder dystocia resolves with suprapubic pressure and McRobert's maneuver?
answer
90% of shoulder dystocia cases will resolve with suprapubic pressure and McRobert's maneuver Toronto Notes 2011
question
What is the definition of postpartum hemorrhage (PPH) for vaginal delivery and C-section? What is the incidence of PPH?
answer
The definition of PPH is blood loss at the time of delivery > 500 mL for vaginal delivery and > 1000 mL for C-section, this can occur early in the postpartum period or late (after the first 24 hours up until 6 weeks postpartum) The incidence of PPH is 5-15% of all deliveries Family Medicine Notes, 3 e. (2015)
question
What is the etiology of postpartum hemorrhage?
answer
The etiology of PPH can be remembered with the "4 T's": 1) Tone (most common) - uterine atony occurs within the first 24 hours, can be prevented with oxytocin with delivery of the anterior shoulder, atony can occur with abnormal labour, abruption, grand multiparity, halothane anesthesia 2) Tissue - retained placenta or clot 3) Trauma - laceration of cervix, vagina, uterus; episiotomy, hematoma, uterine rupture 4) Thrombin - coagulopathy (hopefully identified prior to delivery), DIC, ITP, TTP, therapeutic anticoagulation Family Medicine Notes, 3 e. (2015)
question
What are the principles of management of PPH?
answer
The principles of management for PPH include: 1) Resuscitation - ABCs, type and cross 4 U pRBCs, treat underlying cause, 2 large bore IVs 2) Medical: a) Oxytocin 20 U/L in NS continuous infusion b) Ergotamine 0.25 mg IM/IMM q5 min up to 1.25 mg (may exacerbate HTN) c) Hemabate 0.25 mg IM/IMM q15 mins up to 2 mg (contraindicated in CV, pulmonary, renal or hepatic dysfunction) 3) Local - bimanual compression/uterine massage, uterine packing 4) Surgical - D&C, laparotomy with bilateral uterine artery ligation, hysterectomy +/- angiographic embolization Family Medicine Notes, 3 e. (2015)
question
What is the definition of retained placenta? What are the most common etiologies?
answer
The definition of retained placenta is an undelivered placenta after > 30 minutes post delivery of an infant The most common etiologies of retained placenta are: 1) Separated, but not delivered 2) Abnormal implantation affecting separation (e.g., placenta accreta, increta, percreta) Family Medicine Notes, 3 e. (2015)
question
Distinguish between the three types of abnormal placental implantation.
answer
The three types of abnormal placental implantation include: 1) Placenta accreta ("AT the myometrium") 2) Placenta increta ("IN the myometrium") 3) Placenta percreta ("PAST the myometrium") Family Medicine Notes, 3 e. (2015) Toronto Notes 2011
question
What is the definition of postpartum fever? What is the etiology of postpartum fever? What is the empiric antibiotic therapy for wound infections?
answer
The definition of postpartum fever is fever > 38°C on any 2 of the first 10 days postpartum, excluding the first day The etiology of postpartum fever can be remembered with the "6 W's and 1 B": Wind - atelectasis, pneumonia Water - UTI Wound - C/S incision or episiotomy site Walking - Pelvic thrombophlebitis, DVT Womb - endometritis Wonder drugs - e.g., morphine Breast - mastitis, engorgement The empiric antibiotic therapy for wound infections is clindamycin + gentamicin Family Medicine Notes, 3 e. (2015)
question
What is the incidence of postpartum blues? What are the clinical features of the postpartum blues?
answer
The postpartum blues are an extension of normal hormonal changes and adjustment and affects 85% of new mothers The clinical features of the postpartum blues include: Onset day 3-10 postpartum Self-limited, doesn't last longer than 2 weeks (if longer a more thorough assessment for postpartum depression should be completed) Mood lability Depressed affect Tearful Fatigue Sensitive to criticism Irritable Poor concentration Family Medicine Notes, 3 e. (2015)
question
What is the definition of postpartum depression? What is the incidence? If there is a previous history of postpartum depression what is the risk of recurrence? What are some risk factors for developing postpartum depression?
answer
The definition of postpartum depression is a major depressive episode occurring within 4 weeks - 6 months of delivery The incidence is 10% of all mothers, with a 50% recurrence rate if they have had a previous history of postpartum depression Risk factors for postpartum depression include: Personal or family history of depression Prenatal depression or anxiety Stressful life situation Poor support Unwanted pregnancy Colicky or sick infant Suspect if postpartum blues lasting > 2 weeks, symptoms severe or any suicidal/homicidal ideation Family Medicine Notes, 3 e. (2015)
question
What is a scale that can be used in the assessment of postpartum depression? What are the principles of management of postpartum depression?
answer
A screening tool that is available for postpartum depression is the Edinburg postnatal depression scale The principles of management include: Pharmacologic (evidence of no newborn side effects with sertraline, paroxetine and nortriptyline, AVOID fluoxetine) Psychotherapy Supportive care Nurse home visit ECT if refractory Family Medicine Notes, 3 e. (2015)
question
What is Nagele's rule?
answer
Nagele's rule is used to calculate the estimated date of confinement (EDC) using the following: LMP + 7 days - 3 months (add/subtract days if the patient's normal menstrual cycle is longer/shorter than 28 days) Family Medicine Notes, 3 e. (2015)
question
When is routine test of cure required for gonorrhea and chlamydia?
answer
Routine testing to confirm treatment of gonorrhoea and chlamydia is typically not required but should be performed 3-4 weeks following treatment if: 1) If they continue to be symptomatic 2) Suspect non-compliance with treatment 3) Patient is pregnant (lower cure rate in pregnancy) Toronto Notes 2011
question
On microscopy and gram stain what is seen with gonorrhea? What is used to treat gonorrhea in non-pregnant and pregnant patients?
answer
On microscopy gonorrhea appears as gram negative intracellular diplococci Treatment of gonorrhea is with: Single dose of ceftriaxone 250 mg IM Cefixime 400 mg Ciprofloxacin 500 mg If pregnant use cephalosporins or give 2 g spectinomycin IM x 1 (avoid quinolones) Toronto Notes 2011



