BRCA – Flashcard
Unlock all answers in this set
Unlock answersquestion
chance of developing breast cancer at some point how many diagnosed in year? die? where is the highest rate how many survivors
answer
1 in 8 230,000/40,000 North America 2.8 million
question
biggest risk factors
answer
age and gender
question
when are mammograms recommended to begin now?
answer
50, not 40
question
what percentage of women with breast cancer have hereditary disease?
answer
5-10%
question
what's the difference between somatic genetic mutations and germline genetic mutations?
answer
somatic is a change, after birth in a gene in one or more non-reproductive cells -; can't be passed to offspring germline is a change that was inherited and occurs in every cell in the body -> increased risk for multiple cancers
question
what's changing about genetic testing of tumors?
answer
now they're really looking at what makes a tumor metastatic
question
what percentage of cancers are hereditary, familial, sporadic?
answer
hereditary: 5-10% familial: 15-20% sporadic: 80%
question
what does familial mean?
answer
it's probably hereditary be we don't understand it completely. probably means there is some environmental component
question
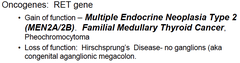
what risk do highly penetrant genes confer?
answer
45-85% lifetime risk of breast cancer
question
what types of genes are associated with cancer?
answer
tumor suppressor and oncogenes
question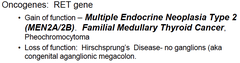
tell me about the oncogenes
answer
gain of function is hereditary Hirschprungs -> stomach doesn't work properly
question
each cell has how many copies of BRCA1 and BRCA2
answer
2
question
what is the most important cancer risk?
answer
hereditary mutations
question
what is the male consequence of BRCA1?
answer
increased breast cancer risk ; pancreatic cancer not as high a factor as BRCA2
question
what is the male consequence of BRCA2?
answer
5-10% will have breast cancer by age 70 (bigger rise than in women) + higher risk for prostate, pancreatic, bladder, bile duct, melanoma
question
what could be the relation between a rare pediatric syndrome and BRCA?
answer
Fanconi Anemia
question
which gene is a Fanconi Anemia gene?
answer
BRCA2 is key in the Fanconi complex for DNA repair
question
what is Fanconi Anemia?
answer
rare AR disease -increased risk of hematological malignancies, skeletal and developmental abnormalities
question
how do children get Fanconi Anemia?
answer
both parents are carriers for BRCA2 -; child has mutations on both alleles on chromosome 13 there is a 25% chance of inheriting 2 copies if both parents are carriers
question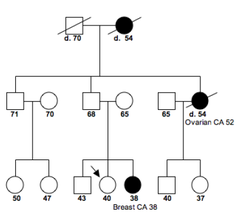
what will a BRCA family pedigree look like? who should you test?
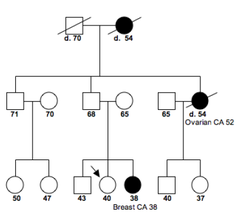
answer
the closest person with the disease
question
what is the overall incidence among all ethnic groups?
answer
1/500-1/800
question
what is the incidence in Ashkenazi Jews?
answer
1/40 - 2.3% have altered BRCA1 or BRCA2
question
what should happen to African-Americans at high risk for breast cancer?
answer
should be tested for BRCA there's not a lot known about the spectrum of mutations and modifiers of risk in this population
question
which patient should you test
answer
individual in the family who is most informative - the person w/ cancer at the youngest age
question
what if the patient has a direct family member with a known familial mutation?
answer
test that first
question
what if the patient is Ashkenazi Jewish?
answer
test the three founder mutations first. If negative, full sequence or multi gene panel
question
what if the patient isn't Ashkenazi Jewish?
answer
full sequencing/deletion ; duplication testing of BRCA1 and BRCA2 (all patients)
question
what is a multi-gene panel and when should you do it?
answer
includes BRCA and other breast cancer related genes do it depending on clinical history (pt and family)
question
why should you test the individual in a family with the disease?
answer
This is because if a mutation is identified then you can test other family members for that mutation. Hereditary breast cancer is an autosomal dominant condition. Once the mutation is identified in the person affected, then if a family member tests positive, they have the genetic predisposition. However, if that family member tests negative, it is a true negative
question
what does a positive result mean?
answer
deleterious mutation identified or a change in an exon [deletion/duplication testing]
question
variant of uncertain significance?
answer
;5% of the time -many are missense mutations -variant tracking can help -check to see if reported with a deleterious mutation
question
negative?
answer
interpretation differs if mutation is known or not if mutation is known in family = real negative = average risks apply if mutation is unknown in family = uninformative result
question
what are the 3 treatments for hereditary breast cancer?
answer
screening chemoprevention surgery
question
what do significantly mutated genes of breast tumors correlate with?
answer
genomic and clinical features
question
is there an antibody against HER-2 protein?
answer
Yeah!
question
what % of cancers are estrogen receptor positive? progesterone receptor positive? what are the chances of responding to chemo if both estrogen and progesterone receptors are present?
answer
75% 65% 70%
question
what does Tamoxifen do?
answer
inhibits estrogen gene transcription used in estrogen receptor positive cancers
question
what risk is associated with moderate penetrance breast cancer genes?
answer
CHEK2, ATM, NBS1, RAD50, BRIP1, and PALB2 doubling
question
DO THE PRACTICE QUESTIONS AT THE END
answer
...



