Blk 8B, GU/GYN – Flashcards
Unlock all answers in this set
Unlock answersquestion
Define the following gynecological terms: Amenorrhea Dysmenorrhea Menorrhagia Metrorrhagia Menometrorrhagia
answer
Amenorrhea - lack of period for at least 6 months Dysmenorrhea - painful menstruation, typically involving abdominal cramps Menorrhagia - excessive blood loss at regular intervals Metrorrhagia - irregular timing of blood loss (but normal volume) Menometrorrhagia - excessive blood loss at irregular intervals
question
What is the generalized workup for Dysmenorrhea?
answer
Primary versus Secondary Dysmenorrhea Primary: no pathologic explanation Secondary: attributable to structural or functional abnormalities (e.g. Endometriosis, Adenomyosis, Fibroids, IUD, etc.)
question
What is Endometriosis? What are the presenting symptoms? What is the most common site of involvement? What other sites may be involved? What is a typical appearance when it is seen endoscopically? How is it diagnosed? How is it treated surgically? How is it treated medically?
answer
-Endometriosis = Endometrial glands/stroma that have implanted outside the uterine cavity and walls -Dysmenorrhea/ Pelvic pain, Dyspareunia, Worsens during luteal phase, improves during menses; Asymptomatic in some women; Possibly infertility -Most common site = ovary -Can be located throughout pelvis and abdomen -Can appear as "powder-burn" lesions on the surface of organs; if within the ovary, presents as "chocolate cyst" -Diagnosed based on surgical findings -Surgical Tx: varies from laser ablation or excision to total abdominal hysterectomy with bilateral salpingoophorectomy -Medical Tx: Start with NSAIDs, Oral Contraceptives and Progestins; if they don't work, move on to GnRH agonist
question
What is Adenomyosis? How is it diagnosed? What are the findings in the history? What are the findings in the physical exam? How is it treated?
answer
-Adenomyosis = presence of endometrial glands in uterine myometrium; it is mostly an incidental diagnosis made after hysterectomy as it is typically asymptomatic, but coincides with other uterine pathology -Dx based on a histologic diagnosis (must have a hysterectomy to dx it) -Hx: Often asymptomatic, but may have: Secondary dysmenorrhea, Menorrhagia, or Dyspareunia -PE: Uterus is enlarged; Can be "tender and boggy" -Symptomatic treatment: oral analgesics, NSAIDs, hormonal therapies; Surgery: hysterectomy
question
What are Uterine Fibroids? What are the presenting symptoms? Do they present in singles or multiples? What is their unique histology? What stimulates their growth? How quickly do they grow/degenerate? How likely are they to undergo malignant change?
answer
-Benign tumors of myometrial smooth muscle cells -Present with abnormal uterine bleeding, pelvic pressure, pain, urinary symptoms -Single or multiple -Each fibroid arises from a single cell -Stimulated by estrogen/progesterone -Rapid growth/degeneration -Very unlikely to undergo malignant change
question
What is the differential diagnosis when a woman presents with amenorrhea?
answer
** First rule out pregnancy!! then... -Hypothalamic (GnRH deficiency, possibly due to anorexia or hyperathleticism) -Pituitary (Excessive androgens, hyperprolactinemia or hyperthyroid) -Ovarian (Gonadal dysgenesis, premature ovarian failure, environmental (radiation), tumor) -Outflow tract (Mullerian agenesis, cervical stenosis, uterine synechiae)
question
What is Polycystic Ovary Syndrome (PCOS)? What are the clinical features? How is the name derived? Are the levels of estrogen and progesterone normal? How is it managed?

answer
-Oligomenorrhea/amenorrhea associated with hyperandrogenism without other cause; role of hyperinsulinemia central to pathophysiology -Obesity, Hyperandrogenism (acne, hirsutism, deepened voice, clitoromegaly); Oligo- or amenorrhea; Acanthosis nigricans; Hyperinsulinemia -Ovaries with thickened tunica and multiple small atretic follicles -Low progesterone, Normal estrogen -Management: If pregnancy desired: ovulation induction, if no pregnancy desired: oral contraceptives; Management of androgenic side effects, Weight loss, Insulin sensitizers - metformin
question
How is "infertility" defined? What is Primary versus Secondary Infertility?
answer
Infertility = the inability to conceive after 12 months of unprotected regular intercourse Primary Infertility - never been pregnant Secondary Infertility - has conceived previously and now can not conceive
question
How is fertility affected by age? Why?
answer
Fertility decreases with increasing age (starting at ~30-35) Majority of oocytes are genetically abnormal at the time of ovulation, and it gets worse with age (in 30s, 1/3 are normal; at 36, 1/6 are normal; at 40, 1/9 are normal; at 45, 1/15 are normal)
question
What is the most common etiology of female infertility? What causes it?
answer
Chronic anovulation Causes: PCOS, Hyper/Hypothryroidism, Pituitary Microadenoma (prolactin), FSH is too high or too low
question
What are the risk factors for Tubal Factor Infertility? What are the best diagnostic tools for Tubal Infertility?
answer
(Fallopian tube is where fertilization and early development takes place -- these risk factors make these early steps more difficult) Pelvic inflammatory disease (PID) Adhesions from previous tubal or pelvic surgery Endometriosis Ruptured appendicitis Septic abortion Silent Chlamydia infection Hysterosalpingogram (HSG) is the best imaging modality for tubal infertility. Laparoscopy with chromopertubation is the gold standard.
question
What are the treatment options for infertility due to: Ovarian Factor Uterine Factor Tubal Factor Unexplained Male Factor
answer
Ovarian Factor: Ovarian stimulation (via weight loss, estrogen receptor modulators, gonadotropins, etc) Uterine Factor: Hysteroscopy, myomectomy to remove fibroids or repair congenital malformations Tubal Factor: IVF Unexplained: Intrauterine insemination, IVF Male Factor: Mild - IUI; Severe - IVF with intracytoplasmic sperm injection (ICSI)
question
What is the most common gynecologic cancer? What age is it typically diagnosed at? What is the gynecologic cancer with the highest mortality?
answer
Most common = uterine/endometrial (typically diagnosed ~60 (75% after menopause) Most deadly = ovarian
question
Name 6 risk factors for Endometrial Cancer.
answer
1. Obesity (Adipose cells convert adrenal steroids to estrone; Decrease in SHBG, increased bioavailability of estrogens) 2. Tamoxifen (Selective Estrogen Receptor Modulator - estrogen antagonist in the breast, estrogen agonist in the uterus) 3. Unopposed Estrogen Therapy (unopposed proliferative phase) 4. Infertility 5. Polycystic Ovarian Syndrome 6. Estrogen-Producing Ovarian Tumors
question
What is Lynch Syndrome?
answer
aka HNPCC (Hereditary NonPolyposis Colorectal Cancer) Mutation in mismatch repair gene (MSH2, MLH1, PMS1, or PMS2) 40-60% lifetime risk for endometrial cancer Early onset colon, endometrial, ovarian, uroepithelial cancers
question
What is Endometrial Hyperplasia? How does it present clinically? What is it a risk for? What conditions is it associated with?
answer
-"Overgrowth" of endometrium secondary to prolonged unopposed estrogen -Presents with abnormal uterine bleeding -Considered precursor to endometrial cancer (Presence of cellular atypia increases risk of underlying malignancy) -Associated with: Anovulatory cycles in teens, Granulosa cell tumors of the ovary, PCOS, Adrenal cortical hyperplasia, Unopposed estrogen, Tamoxifen
question
How frequently does Simple Endometrial Hyperplasia progress to Endometrial Cancer? Complex Endometrial Hyperplasia? Simple Atypical Endometrial Hyperplasia? Complex Atypical Endometrial Hyperplasia?
answer
Simple: 1% ("Penny") Complex: 3% ("Nickel") Simple Atypical: 8% ("Dime") Complex Atypical: 29% ("Quarter")
question
How would you manage a pre-menopausal patient with Endometrial Hyperplasia with NO atypia on biopsy? A post-menopausal woman?
answer
Pre-Menopause: Treat with Progestins (Provera, Depo Lupron, Mirena) Resample every 3-6 months Post-Menopause: Treat with Progestins (Provera, Depo Lupron, Mirena) Resample every 3-6 months If bleeding recurs, you can consider a hysterectomy
question
How would you manage a pre-menopausal patient with Endometrial Hyperplasia WITH atypia on biopsy? A post-menopausal woman?
answer
Pre-Menopause: Treat with Progestins (Provera, Depo Lupron, Mirena) Resample every 3 months If disease progresses or if there is continued sx, must have a hysterectomy Post-Menopause: Hysterectomy
question
What are the recommended screening protocols for Endometrial Cancer?
answer
No inexpensive, accurate, noninvasive screening test exists Don't screen for it unless the patient has Lynch Syndrome or is symptomatic (abnormal bleeding) For Lynch: recommend annual endometrial sampling (EMB) starting at age 30-35 or 5-10 yrs prior to earliest diagnosis of Lynch-assoc cancer in family
question
What diagnostic test is preferred for post-menopausal bleeding? For irregular vaginal bleeding?
answer
Endometrial Biopsy (for both)
question
What is the difference between Type I and Type II Endometrial Cancer in terms of: Frequency Role of Estrogen Typical Patient Risk Factors Prognosis
answer
Type I (90%) Estrogen related Younger Assoc with obesity, nulliparity, exogenous estrogen, DM, etc. Overall have a good prognosis because you can usually just take away the estrogen Type II (10%) Unrelated to estrogen Multiparous, older and thinner patients More aggressive, poorer prognosis
question
How is endometrial cancer staged? What are the basic stages? How does it affecte treatment?
answer
Surgical Staging Stage 1 - confined to uterus Stage 2 - cervix involved Stage 3 - uterine serosa, adnexa, positive cytology, vaginal metastases, pelvic, aortic node metastases Stage 4 - bladder, bowel, inguinal node and other distant metastases Determine whether or not to take out lymph nodes
question
What are the three most common histological types of Endometrial Cancer? Which is most common? Which has the best prognosis?
answer
1. Endometrioid adenocarcinoma (Type I) 75-80% of cases Overall survival 80-90% **NOTE that "endometrioid" histology does not necessarily indicate Endometrial Cancer -- it can be endometroid adenocarcinoma of the ovary or cervix 2. Papillary serous (Type II) 10% of cases Mode of spread more like ovarian cancer; Many have extra-uterine spread, even with minimal invasion 3. Clear cell (Type II) and Mixed tumors 5% of cases
question
How is Endometrioid Adenocarcinoma staged/described?
answer
FIGO Grading... Grade 1: up to 5% of the tumor is solid (non- morular, non-squamous) Grade 2: 6% to 50% of the tumor is solid (non-morular, non-squamous) Grade 3: >50% of the tumor is solid (non-morular, non-squamous)
question
What is the first thing to rule out when evaluating adnexal masses?
answer
R/O pregnancy and infection!!
question
What factors would increase suspicion that an adnexal mass may be cancer?
answer
Large size (>10 cm) Bilaterality Solid vs. cystic Radiologic appearance: Complex, papillary, ↑ density, ↓ pulsatility of blood flow Age of pt. outside reproductive span Ascites Elevated serum tumor markers (CA125)
question
What does an elevated CA125 level indicate?
answer
Used as a tumor marker for ovarian cancer, but anything that irritates the peritoneal lining will elevate CA125 (In women <50 yo, elevated CA125 is associated with malignancy less than 25% of the time) Gyn Causes: PID, Adenomyosis, Benign ovarian, neoplasm/cyst, Endometriosis, Menstruation, Ovarian hyperstimulation, Fibroids, Cancer Non-Gyn Causes: Hepatitis/liver disease/cirrhosis, Pancreatitis, CHF, Diverticulitis, Lupus, Pneumonia, Mesothelioma, Metastatic cancer
question
What are the indications for surgery on an adnexal mass?
answer
Cyst > 5 cm (persistent) Solid Papillary appearance on sonography Initial size > 10 cm Ascites Age of patient outside reproductive range Torsion or rupture suspected
question
What two neoplasms most frequently metastasize to the ovary? What is the most common method of spread to the ovary?
answer
1. Colon (Krukenberg Tumor = bilateral ovarian metastases by signet ring cells most often of gastric origin -- most common metastatic carcinoma to the ovary) 2. Breast Method of spread = lymphatic
question
What are some protective factors against ovarian cancer?
answer
Pregnancy and anovulation are protective Combined OCP use ≥ 5 continuous years decreases risk 50-80% Tubal ligation/hysterectomy Breast feeding Prophylactic oophorectomy
question
What is Hereditary Breast Ovarian Cancer Syndrome (HBOC)?
answer
10-14% of ovarian cancers due to BRCA1 & 2 mutations (BRCA regulates p53) Autosomal dominant inheritance with 85% penetrance
question
What is the most common method of spread from the cancer from the ovary to other organs?

answer
Peritoneal spread (omentum is almost always involved)
question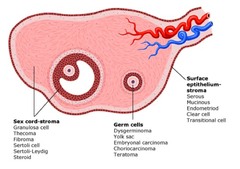
What are the three histological types of Ovarian Cancer? Which is most common? Briefly describe the characteristics of each.
answer
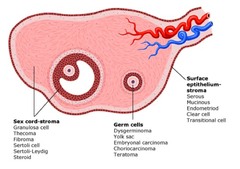
1. Surface Epithelial (85-90%) -Elevated CA125 -Associated with hereditary/genetic syndromes (BRCA or Lynch) -Diagnosed between 40-65 yo -Usually diagnosed at advanced stages due to non-specific symptoms -Types: Serous, Mucinous, Endometrioid, Clear Cell, Transitional Cell 2. Germ Cell -Benign or malignant -Usually diagnosed between 10-30 yo (account for 70% of masses in this age group) -Present with precocious puberty, pain -Very chemosensitive (essentially curable!) 3. Sex Cord (rare) -Seen at any age group but more common in younger women -Present with precocious puberty, hyperandrogenism, pelvic mass/pain -Very chemosensitive -Granulosa cell tumors assoc with uterine hyperplasia/cancer in postmenopausal women (Call-Exner Bodies are pathognomonic)
question
How is Ovarian Cancer Staged? What are the stages?
answer
Like endometrial cancer, ovarian cancer is surgically staged 1 - limited to one or both ovaries 2 - starting to involve the adnexa, uterine serosa or uterus 3 - escaped the pelvis, now in the peritoneum 4 - lung or liver is involved (not just surface of liver, but actually within the liver)
question
How is Ovarian Cancer typically treated?
answer
Surgery (for Staging and Tumor reduction) Chemotherapy (Neoadjuvant or Adjunct, salvage for recurrent disease) Radiation has a limited role
question
What is the recommended screening protocol for ovarian cancer?
answer
No recommended screening tool exists Physical exam doesn't detect before Stage III or IV; no imaging can definitively rule it in or out; no serum marker with sufficiently high sensitivity or specificity, especially in early stage cancer
question
How long is a full term pregnancy? How is gestational age calculated? How is developmental (conceptional) age calculated?
answer
Full-term human pregnancy lasts 37-42 weeks (average is 40 weeks) Calculated from first day of last menstrual period (LMP) Developmental (conceptional) age is 2 weeks less than menstrual age
question
What are the three most common complications of early pregnancy?
answer
Abortion Ectopic Pregnancy Molar Pregnancy
question
What weeks fall in the three trimesters of a pregnancy? Where is the line drawn between "abortion" and "preterm pregnancy"?
answer
0-12 weeks = First Trimester 13-27 weeks = Second Trimester 28-40 weeks = Third Trimester Pregnancy Loss: 0-20 weeks = Abortion 20 - 36+6 weeks = Preterm Delivery (different causes for each)
question
How are the following terms defined: Spontaneous abortion Incomplete abortion Threatened abortion Missed abortion Induced abortion
answer
Spontaneous abortion: "miscarriage"; fetus is only viable in ~30% of pregnancies; may or may not present with sx Incomplete abortion: some of the fetus or placenta is still intact Threatened abortion: pregnancy is in tact, but the cervix is dilated and there is spotting Missed abortion: woman says she's pregnant, US shows fetus, but there is no heartbeat or the fetus isn't growing, just hasn't aborted yet Induced abortion: elective abortion
question
What is the most common GROUP of aneuploidy in spontaneous abortion? What is the single most common trisomy in spontaneous abortion? Is it typically due to maternal or paternal non-disjunction? What is the single most common aneuploidy in abortuses? Is it typically due to maternal or paternal non-disjunction?
answer
-Autosomal trisomy -Trisomy 16 -- Maternal non-disjunction (95%) -Turner (45,X) -- 80% loss of Paternal chromosome
question
What maternal diseases would put a fetus at risk for spontaneous abortion? Uterine factors? Common exposures?
answer
Maternal: Thyroid disease, Diabetes (insulin-dependent), Chronic hypertension (later losses), Collagen vascular diseases Uterine: Intrauterine synechiae (adhesions), Mullerian anomalies, Fibroids, Incompetent cervix Common exposures: Radiation, Alcohol, Tobacco, Caffeine
question
What are the options for managing spontaneous abortion?
answer
Expectant (let the body expel the fetus on its own) Medical (medically induce an abortion, e.g. misoprostol) Surgical (physically take out the fetus with dilation and curettage)
question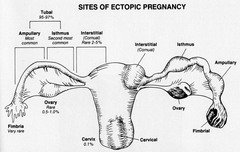
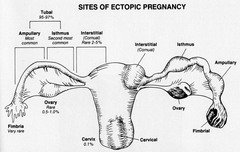
How is Ectopic Pregnancy defined? What are the risk factors for having an Ectopic Pregnancy? What are the presenting symptoms?
answer
Definition: any pregnancy implanted outside of endometrial cavity Risk Factors: Previous pelvic infection, Previous tubal surgery, Intrauterine device in place, Previous tubal pregnancy Sx: abdominal pain, amenorrhea, vaginal bleeding, dizziness, pregnancy sx
question
What are the treatment options for an ectopic pregnancy?
answer
Surgical: Laparoscopy with salpingectomy or salpingotomy Medical: Methotrexate (single or multiple dose)
question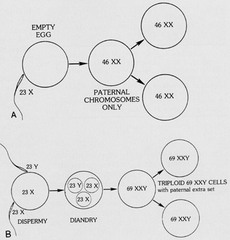
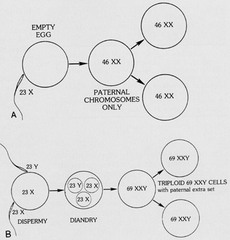
What is a Molar Pregnancy (Hydatiform Mole)?
answer
Definition: an abnormal form of pregnancy, wherein a non-viable, fertilized egg implants in the uterus, and thereby converts normal pregnancy processes into pathological ones; Can persist and develop into gestational trophoblastic disease (GTD) A complete mole is caused by a single sperm combining with an egg which has lost its DNA (the sperm then reduplicates forming a "complete" 46 chromosome set). The genotype is typically 46,XX (diploid) due to subsequent mitosis of the fertilizing sperm -- trophoblastic proliferation, cystic villi, no fetal tissue A partial mole occurs when an egg is fertilized by two sperm or by one sperm which reduplicates itself yielding the genotypes of 69,XXY (triploid) or 92,XXXY (quadraploid)
question
What is the clinical presentation of a molar pregnancy? What are the risk factors?
answer
Clinical Presentation: Vaginal bleeding Uterine size discrepant from dates Hypertension Hyperemesis Thyroid dysfunction Theca lutein cysts of ovaries Risk Factors: Maternal age 40 yr Asian ethnicity Prior molar pregnancy Low socioeconomic status (nutritional factors ??)
question
What is the follow-up for molar pregnancy?
answer
MUST follow hCG until it declines to zero! If you miss a little bit in the evacuation, hCG will lower for a little while, plateau, then rise again as the molar tissue recurs
question
What are the four most common complications of late pregnancy?
answer
Hypertensive Disorders of pregnancy Preterm Labor Fetal death/Stillbirth Amniotic Fluid Abnormalities
question
How are the following terms defined: Chronic Hypertension Preeclampsia/Eclampsia Gestational Hypertension
answer
HTN = systolic >140 or diastolic >90 Chronic hypertension Present before conception, dx before 20 wk, or persists > 6 wk postpartum Preeclampsia/Eclampsia Hypertension appearing after 20 wk gestation in association with edema and proteinuria Gestational hypertension Hypertension appearing after 20 wk with no other evidence of preeclampsia
question
What are the risk factors for developing Preeclampsia?
answer
Nulliparas Maternal age 35 African-Americans Low socioeconomic status Multiple gestations Obesity
question
What are the placental features in preeclampsia?
answer
-Small placenta -Infarcts of the placenta -frequently multiple and large -Abnormal development of the villi -- called "Accelerated maturation of villi" (note that it isn't accelerated, it's actually that they are too immature)
question
Which systems are typically affected by Preeclampsia?
answer
CNS: arteriolar thrombosis, microinfarcts, petechial hemorrhages, grand mal seizures Pulmonary: pulmonary edema, ARDS Cardiovascular: depleted intravascular volume Liver: hepatocellular damage, hemorrhage, rupture Renal: decreased GFR, swollen and leaky glomerular capillaries, acute tubular necrosis Hematologic: low platelets, hemolytic anemia, DIC Placental: poor intervillous blood flow, infarctions, IUGR (intrauterine growth restriction)
question
What are the diagnostic criteria for Severe Preeclampsia?
answer
Systolic bp >160 mm Hg or diastolic bp >110 mm Hg Proteinuria > 5 g/day Serum creatinine > 1.2 mg/dL Elevated liver enzymes Thrombocytopenia (plt <100,000/mm3) Pulmonary edema Oliguria (in infant or in mother) IUGR (intrauterine growth restriction -- infant not growing appropriately)
question
How is Preeclampsia managed?
answer
Delivery is the only cure Control hypertension: hydralazine, labetolol, nifedipine Prevent seizures: parenteral magnesium sulfate Optimize fetal outcome
question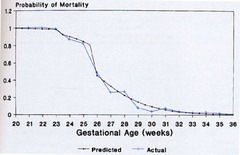
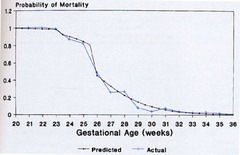
At what age does infant death due to prematurity begin to drop?
answer
24 weeks is the borderline of when an infant can survive -- every passing week in the womb improves survivability
question
What are the maternal risk factors for going into premature labor? What are the genetic factors that play into preterm labor?
answer
Maternal Low maternal weight gain Low socioeconomic status Substance abuse Young maternal age Psychologic stress Previous preterm labor Genetic Collagen defects Uterine anomalies
question
What happens when there is a Premature Rupture of Membranes (PROM)?
answer
Loss of mechanical barrier to infection Release of prostaglandins secondary to inflammatory changes Majority will deliver within 48 hours of PROM Management dependent on suspicion of intra-amniotic infection
question
How do corticosteroids administered to a mother in preterm labor help fetal lung development?
answer
Type 2 alveolar cells produce surfactant Corticosteroids enhance surfactant production Increase neonatal lung compliance Decreased alveolar protein leakage Stabilization of cellular architecture REQUIRES 48 HOURS FOR OPTIMAL EFFECT
question
What are "tocolytic agents"? What are some examples?
answer
Tocolytic = labor repressant Beta-mimetics: β₂ receptors cause uterine relaxation Magnesium sulfate: unknown, presumed interference with Ca++ role in contractile apparatus Ca++ channel blockers: block cellular entry of Ca++, reducing contractility Prostaglandin synthetase inhibitors (not used after 32 weeks) Note that each has significant side effects!
question
What is the definition of a Stillbirth? What are some typical causes?
answer
Definition: antepartum or intrapartum death of fetus > 500g Fetal Causes: Chromosomal abnormalities, Other structural anomalies, Non-immune hydrops (heart-failure), Infection Placental Causes: Abruption, Fetal-maternal hemorrhage, Cord accident, Placental insufficiency, Intrapartum asphyxia, Twin transfusion syndrome, Chorioamnionitis Maternal Causes: Antiphospholipid antibodies, Diabetes, Hypertension, Trauma, Sepsis, Uterine rupture (tearing in uterine wall), Postdates pregnancy (Unexplained in 25-30% cases)
question
What are the two kinds of Amniotic Fluid abnormalities? What are the etiologies of each?
answer
Hydramnios (Polyhydramnios) (AFI >90th %ile) -Excessive production: Maternal diabetes, Twins -Impaired swallowing: Neurologic disorders -GI obstruction: Intestinal atresia Oligohydramnios (AFI <10th %ile) -Impaired production: Uteroplacental insufficiency, Renal dysplasias -Fetal renal obstruction -Leaking amniotic membranes
question
What is the most common gynecological cancer *worldwide*? What is the most common histology? What is the most common cause?
answer
Cervical cancer is #1 gyn ca worldwide, 3rd in US (most common STD!) 95% are squamous cell cancer 95% caused by Human Papilloma Virus
question
How are the subtypes of Human Papilloma Virus differentiated from each other? What are the 2 most common strains of HPV that are considered "low risk"? What clinical manifestation are they associated with? What are the 2 most common strains of HPV that are considered "high risk"? What clinical manifestation are they associated with? What strands does the HPV vaccine protect against?
answer
Differentiated based on L1, E6, and E7 gene sequences Low risk = 6, 11 = Genital warts High risk = 16, 18 = Cervical cancer HPV Vaccine contains the L1 protein from four types of HPV (16, 18, 6, 11)
question
What risk factors are associated with precancerous changes and cancer of cervix?
answer
Human papillomavirus (HPV) infection Sexual activity: multiple partners; begun at an early age Parity Human immunodeficiency virus (HIV) Immunosuppressed status Smoking History of other sexually transmitted diseases -e.g., Herpes simplex, Chlamydia, bacterial vaginosis Oral contraceptive use Low socioeconomic status Poor diet-e.g., vitamin deficiency Alcoholism
question
Describe the natural history of the HPV infection.
answer
Exposure to HPV occurs with intimate sexual contact ↓ HPV is either removed by host immune system or persists (5%) ↓ ** HPV replicates in nucleus of host cells producing E6 and E7 proteins ** ↓ ** Tumor suppressor genes are inactivated ** ↓ Dysplastic epithelial growth either regresses or progresses: referred to as Cervical Intraepithelial Neoplasia
question
What age group is at highest risk for HPV infection? What age group is at highest risk for developing cervical cancer from HPV?
answer
Get infected in 20s, but don't develop cancer til 50s -- takes a long time to develop cancer!
question
What screening method is used for HPV? What is the next step if the test is abnormal? What happens next if those are abnormal?
answer
Pap smear used to screen for cervical epithelial abnormalities (liquid based test used more commonly than conventional smear) Abnormal results lead to colposcopy (look for aceto-white lesions) and directed biopsies Abnormal histologic results lead to treatment (ablative or excisional) All abnormal results require follow-up!
question
What are the cervical cancer screening guidelines?
answer
All women should have a pap smear at age 21 From ages 21 to 29, pap smear every 2 years After age 30, if 3 consecutive normal pap smears, screen every 3 years with some exceptions Risk factors that require more frequent screening: HIV infection Immunosuppression DES (diethystilbestrol) exposure Previous h/o CIN 2, 3 or cancer Discontinue pap smears between ages 65-70 if 3 consecutively normal pap smears with no abnormalities in the last 10 years Pap smears are NOT required if a patient has had a hysterectomy with removal of cervix as long as the patient did not have CIN 2, 3 or cancer
question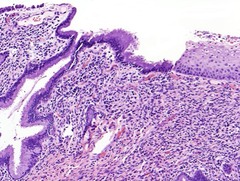
What part of the cervix is most susceptible to HPV?
answer
Transformation zone (squamocolumnar junction): Metaplastic squamous cells predisposed to HPV infection
question
25 year old woman, G1P0, 12 weeks pregnant Chief complaint: Vaginal itching and thick white "cottage cheese" discharge. What is your proposed diagnosis? What would you expect to see on colposcopy? What predisposes to this? What would you expect to see on histology?
answer
Candida infection Thick, curd-like discharge Predispose: Diabetes mellitus, Antibiotics, Pregnancy, Immunocompromised state Histo: Epithelial cell clusters arranged around pseudohyphae "Shish kebab" look
question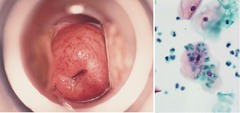
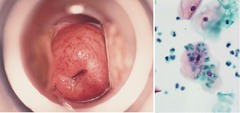
32 year old woman Chief complaint: Copious yellow discharge Exam: "Strawberry cervix" and abundant yellow discharge What is your proposed diagnosis? What would you expect to see on histology?
answer
Trichomonas vaginalis (flagellate protozoan) T vaginalis are oval or pear shaped and have a small pale nucleus, and green cytoplasm with red granules, Flagella is difficult to visualize in PAP smear
question
When a woman has dysplasia on a pap smear, how is the dysplasia characterized?

answer
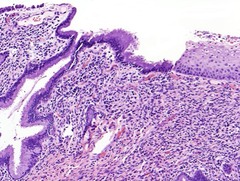
Low grade (LSIL) = Mild dysplasia (CIN 1) -Dysplastic changes involving the lower third of the epithelium -The most superficial cells show extensive HPV changes or Koilocytes (perinuclear halo, nuclear enlargement, hyperchromasia and wrinkling) or High grade (HISL) = Moderate dysplasia (CIN2) or Severe dysplasia/CIS (CIN3) -Dysplastic changes involve up to half of the epithelial thickness (moderate dysplasia or CIN 2) -Dysplastic changes involve more than half of the epithelium ( Severe dysplasia or CIN 3) -Dysplastic changes involve the entire thickness of the epithelium (Severe dysplasia /Carcinoma in situ or CIN 3/CIS)
question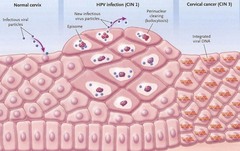
What is the basic life cycle of the HPV virus in the cervix?
answer
Virus enters metabolically active cells (metaplastic sq. cells, transformation zone) ↓ Low grade lesions (LSIL, CIN 1), many koilocytes & complete virus particles ↓ High grade lesions (HSIL, CIN 2 & 3), few koilocytes, viral DNA integrated into host
question
What hormonal factors are risks for breast cancer? What are some other risk factors?
answer
Early Menarche Late menopause Nulliparity Age at 1st childbirth: after age 30 Estrogen replacement therapy/oral contraceptive High estrogen High progesterone Other risk factors: Family history of breast cancer in 1st° relative (especially if bilateral, premenopausal) Personal hx of breast, colon, uterus or ovarian cancer BRCA Radiation (atomic bomb, xray, radiation therapy) Fibrocystic disease
question
What is the recommended screening for breast cancer?
answer
Breast self-examination: monthly after age 20 Physician breast exam: yearly after age 20 Mammography a. Baseline at 35-40 b. Yearly or every other year at 40-50 c. Yearly over 50 If family member with breast ca => Shift screening to 5 years prior to the first diagnosis of the youngest family member
question
What is a mammogram best at detecting? What are the primary signs of breast cancer (as seen on mammogram)?
answer
Mammograms are used to screen for NONPALPABLE masses If a palpable mass is present, a negative mammogram does NOT preclude biopsy Primary signs of Breast cancer: Microcalcifications (clusters) Stellate mass
question
What is the role of Estrogen and Progesterone Receptors in Breast Cancer prognosis?
answer
Any time you biopsy a breast cancer mass, always stain it for estrogen and progesteron receptors (and the HER oncogene)! Estrogen Receptor Protein (ERP): 2/3 pt's are ERP +ve (postmenopausal more likely to be positive) -- 2/3 of those will respond to endocrine therapy
question
What is the single most important factor when assessing prognosis (recurrence and survival) in a patient with breast cancer? What are some other important factors?
answer
(1) Axillary node involvement (2) Tumor size (3) Estrogen and progesterone receptor positivity (better prognosis) (4) HER-2/NEU oncogene (5) Pathology: tubular, medullary and colloid cancers have a better prognosis (6) Histologic grade Grade 1: Well differentiated Grade 2: Moderately differentiated Grade 3: Poorly differentiated
question
What are the two most common histological types of invasive breast cancer?
answer
1. Infiltrating ductal cancer: 70% of breast cancer 2. Infiltrating lobular carcinoma: 5-10%
question
What is done to prevent recurrence of breast cancer?
answer
Radiation therapy is important to prevent recurrence in the chest wall at the mastectomy site
question
What is the most common site of distant metastasis of breast cancer?
answer
Bone (70%) 90% are lytic, which puts the patient at risk for pain, fractures, etc (then liver, then lungs)
question
What treatment modalities are available for breast cancer?
answer
(1) Surgery Control of local and regional disease Excision of single metastasis (**don't need to do a mastectomy if the lump is ≤4cm!!) Make sure to do a sentinel node biopsy (2) Radiation therapy Prevent local recurrence after lumpectomy Prevent chest wall recurrence in high risk patients after mastectomy Palliation of symptomatic metastasis: bone, brain, spinal cord (3) Hormonal Therapy Adjuvant therapy Treatment of metastatic disease (4) Chemotherapy Adjuvant therapy Treatment of metastatic disease (Get as much out of hormonal therapy as you can because once you start chemo, the lifespan is limited) (Taxol, Taxotere, Adriamycin, Cyclophosphamide) (5) Monoclonal antibody (Herceptin targets HER) Adjuvant therapy Treatment of metastatic disease ** Note that both Adriamycin and Herceptin are heart toxic, and should NEVER be given together!
question
What are the different formulations of oral contraceptive pills? What is the mechanism of action? What effect do they have on early pregnancy? How quickly does fertility return after stopping OCPs?
answer
1. Estrogen + Progestin (may be monophasic or phasic - work equally well) 2. Progestin only (use in women in whom estrogen is contraindicated, e.g. pregnancy) Mechanism: Gonadotropin secretion is blunted (E+P effect) Thickens cervical mucus (P effect) Slows tubal secretions and peristalis (P effect) Atrophies the endometrial lining (P effect) No effect on early pregnancy Fertility returns w/in 3 months
question
What are the non-contraceptive benefits of Oral Contraceptive Pills?
answer
Can relieve: Irregular cycles Dysmenorrhea Menorrhagia Anemia Functional ovarian cysts PMDD Cancer reduction: Ovarian Endometrial Colorectal Prevention of: Bone loss Fibrocystic/benign breast disease Pelvic inflammatory disease (PID) Ectopic pregnancy Treatment of: Acne Hirsutism Perimenopausal symptoms
question
What are the side effects of Oral Contraceptive Pills?
answer
Nausea Breast tenderness ?Weight gain Elevated BP (in some women) Breakthrough bleeding Headaches Mood swings
question
In which patients should Oral Contraceptive Pills be avoided? How does the WHO classify who can and can not take OCPs?
answer
**Oral contraceptives are safe until age 50-55 in healthy women with no risk factors for cardiovascular disease or thromboembolic disease (clots)** WHO Classification: Category 1: No obstacle to use Category 2: Benefits generally outweigh the risks Category 3: Risks generally outweigh the benefits (women have HTN, DM, smoke or are breastfeeding) Category 4: Unacceptable health risks (hx of ischemic heart disease, stroke, DVT, PE, HTN >180/110, Smoking >20 cigs/day and age >34 years, Migraines with focal neurological symptoms or current breast cancer) => Categories 1 and 2 CAN take OCPs, Categories 3 and 4 can NOT
question
What is the mechanism of action of the injectable contraceptive Depot medroxyprogesterone acetate (DMPA)? What is the efficacy? How quickly does fertility return? What are the typical side effects?
answer
Mechanism of Action -Progesterone-only method -Acts primarily by inhibiting ovulation -Thickens cervical mucous -Atrophies endometrium Efficacy: Extremely high Fertility: 50% of women conceive w/in 10 months of discontinuing DMPA; May be delayed up to 18 months in a small proportion of women Side Effects: Irregular bleeding, weight gain, bone loss
question
What is the mechanism of action of the implantable contraception Implanon? What is the efficacy? How quickly does fertility return? What are the typical side effects?
answer
Mechanism of Action: Acts primarily by inhibiting ovulation (also thickens cervical mucous and atrophies endometrium) Efficacy: Typical 1 year failure rate 0.05% Return of Fertility is rapid after removal Side Effects: breakthrough bleeding
question
What is the mechanism of action of Intrauterine Devices (IUDs)? What are the contraindications to using an IUD? What are some of the side effects?
answer
Mechanism of Action: -Inhibition of sperm migration and viability -Change in transport speed of the ovum -Damage to or destruction of the ovum (pre-fertilization) -Post-fertilization effects before implantation, may occur such as damage to or destruction of the fertilized ovum -Endometrial suppression (Mirena only) -Changes to the amount and viscosity of cervical mucus (Mirena only) Contraindications: -Pregnancy -Current or recent pelvic inflammatory disease -Sexually transmitted infection -Cervicities -Unevaluated irregular vaginal bleeding -Malignancy of genital tract -Abnormal uterine cavity -Wilson's disease (Paragard only - the copper one) Side effects: Irregular vaginal bleeding (Mirena cause oligo/amenorrhea, Paragard causes menorrhagia); IUD expulsion; Pelvic inflammatory disease (only in the first 21 days after placement); "Missing Strings" -may require hysteroscope or laparoscope to remove
question
What are the options for Emergency Contraception?
answer
Not just the "morning-after pill" - hormonal emergency contraception can be given up to 3-5 days after unprotected intercourse -Combined oral contraceptive formulations -Dedicated progestin-only formulation: Plan B®, Ella Paragard IUD
question
How are the following words defined: Climacteric Peri-menopause Menopause Premature Ovarian Failure
answer
Climacteric: Transition phase from reproductive stage to non-reproductive stage - regression of ovarian function Peri-menopause: Time between irregular menses and permanent cessation of menstruation. Median age - 47.5 years old Median duration - 4 years Menopause: Permanent cessation of menstruation caused by ovarian failure (12 months of amenorrhea) Mean age in U.S. - 51 (unchanged for centuries) Premature Ovarian Failure: Ovarian failure before age 40 (Implications = infertility and hypoestrogen state)
question
What factors influence menopause?
answer
*Genetics (Strongest determinate) Abnormalities on the long arm of X chromosome associated with POF Smoking (menopause 2 years earlier than nonsmokers!) Surgical menopause Precocious puberty Left-handedness Socioeconomic class Obesity
question
What are the lab findings associated with menopause?
answer
Low inhibin (first sign of decreasing ovarian function) Low Estradiol (decreased estradiol releases the hypothalamus from negative feedback inhibition which leads to the rise in FSH) FSH >40 (FSH elevation in the face of low E2 is diagnostic of menopause)
question
How is the diagnosis of menopause made?
answer
Clinical Signs and Symptoms -Irregular menses -Amenorrhea -Vasomotor instability, mood changes, impaired sleep Laboratory -FSH > 40
question
What are hot flashes (how do women typically describe them)? When do they typically occur in the progression of menopause? What is their etiology? What is their natural progression? What can trigger them? What can relieve them? How are they treated?
answer
Hot Flashes = Pressure in head, increased warmth to head and trunk; Last 30 seconds to 5 minutes; Frequently occur at night (Note that they are NOT pathognomonic for menopause!) Occur in early menopause (first 5 years -- includes the climacteric, perimenopause and menopause itself) Etiology: Decrease in circulating estrogen levels causes changes in the thermoregulatory center in hypothalamus; Severity relating to rapidity of change (Obesity is protective due to increased peripheral conversion of androgens and decrease SHBG) Often resolve without treatment in 2-5 years Triggers: Alcohol, Caffeine, Diet Pills, Spicy Foods, Hot Food, Hot Tubs, Saunas, Hot Shower, Hot Beds, Hot Rooms, Hot Weather, Smoking Relieve: Exercise Treat with Estrogen replacement
question
What are the absolute contraindications of Estrogen Replacement Therapy?
answer
Undiagnosed vaginal bleeding Breast cancer - H/O, suspected, current Endometrial cancer- < 5 years Active venous clot Active liver disease (Note that with a uterus, combination therapy is indicated)
question
How is mid-postmenopausal symptoms defined? What causes them?
answer
5-10 yrs after menopause When body tissues that previously had estrogen effect have now been without E long enough to manifest symptoms. (Not all women develop these symptoms. But those that do develop symptoms will have their symptoms progress over time without treatment.)
question
Which tissues are affected by Mid-Postmenopausal Symptoms? Why?
answer
Genitourinary Symptoms are most common -Stress incontinence -Urge incontinence -Vaginal atrophy The urinary and genital tracts develop from a common precursor - UROGENITAL SINUS Therefore the urethra and trigone of the bladder contain estrogen receptors like the genital tract. As the levels of estrogen decreases post menopause the collagen content of these tissues decrease the epithelial layer regresses and the urethra thins.
question
What is the difference between the following terms: -Stress incontinence -Urge incontinence -Vaginal atrophy How are they treated?
answer
Stress incontinence = Involuntary leakage of urine in response to physical exertion, sneezing, or coughing (due to urethral hypermobility) Treatment: Estrogen; α-adrenergics - increase sphincter tone; Exercises - Kegel; Surgery Urge incontinence = Strong desire to pass urine with the inability to control it (etiology unknown) Treatment: Behavioral therapy; Anticholinergics Vaginal atrophy = Thin, dry epithelium of the vagina resulting in smaller diameter, splits and tears easily, dypareunia (due to lack of estrogen secretion) Treatment: Estrogen (oral/transdermal/vaginal)
question
How are "Late Post-Menopausal Diseases" defined? What kinds of diseases fall into this category?
answer
> 10 years after menopause Cardiovascular disease Osteoporosis Breast Cancer Dementia
question
What are the risks for cardiovascular disease in women? Are women or men more predisposed to Myocardial Infarction? What is the role of Hormone Replacement Therapy (HRT)?
answer
Risk Factors: Personal history of coronary heart disease (CHD); Age over 55; Dyslipidemia; Family history; Diabetes mellitus; Smoking; Hypertension; Peripheral artery disease In any age matched group, MEN are more likely than women to have MI HRT has positive effects on lipids (lowers LDL, raises HDL, decreases cholesterol, increases TGs), but there is no data to support the use of estrogen in the treatment or prevention of CHD*
question
What effect does Hormone Replacement Therapy (HRT) have on the rates of breast cancer?
answer
Observational studies have shown an increased risk of breast cancer with HRT (↑ risk of invasive breast cancer, ↑ nodal involvement, ↑ mortality)
question
What effect does Hormone Replacement Therapy (HRT) have on dementia?
answer
Clinical trials have failed to show that estrogen prevents dementia
question
What effect does Hormone Replacement Therapy (HRT) have on colon cancer?
answer
Decreases rates of colon cancer
question
What effect does Hormone Replacement Therapy (HRT) have on osteoporosis?
answer
Decreases rate of osteoporosis
question
What is short term therapy with Estrogen indicated? When is long term therapy with Estrogen indcated?
answer
Short-term HRT is indicated for treatment of severe hot flashes. Long-term HRT is indicated for: 1. Refractory osteoporosis treatment 2. Dyspareunia (Topical)
question
Briefly discuss the anatomy of the breast. Where do most cancers originate? Briefly discuss the histology of the breast.

answer
Anatomy: -6-10 major segmental duct systems that emerge at nipple. -Successive duct branching into small terminal duct lobular units (TDLU), where most cancers originate. -Supporting stroma: fat, connective tissue and blood vessels. Histology: Ducts and lobules composed of 2 cell types: -Myoepithelial cells - contractile, milk ejection -Epithelial cells - milk production - cancer Stroma: -Dense fibroconnective tissue - sarcomas of the breast -Adipose tissue -Blood vessels
question
What are the different categories of benign breast diseases? Why is it important to distinguish between these categories?
answer
Nonproliferative Diseases -Inflammatory Conditions (Acute Mastitis, Duct Ectasia) -Fibrocystic Changes Proliferative (Premalignant) -Without Atypia Usual Ductal Hyperplasia, Sclerosing Adenosis, Intraductal Papilloma, Fibroadenoma) -With Atypia (Atypical ductal hyperplasia (ADH) and Atypical lobular hyperplasia (ALH)) Important to distinguih because of risk of developing cancer: Nonproliferative < Proliferative without Atypia < Proliferative with Atypia
question
Briefly describe the different kinds of Nonproliferative Benign Breast Diseases.
answer
1. Inflammatory conditions -Acute mastitis - usually during lactation, bacterial infection, erythema and swelling can mimic inflammatory breast cancer -Duct ectasia - dilatation of ducts, inspissated secretions, inflammation of lobules; secretions get stuck, and the ducts dilate 2. Fibrocystic changes: Lumpy, sometimes tender breasts, very common; Composed of cysts (fluid filled sacs, tender), fibrosis, adenosis
question
Briefly describe the different kinds of Proliferative (without Atypia) Benign Breast Diseases.
answer
1. Usual ductal hyperplasia - several cell layers with mixed cell population, ER+ 2. Sclerosing adenosis - proliferation of glands within a fibrotic stroma, microcalcifications 3. Intraductal papilloma - growth inside duct, can cause nipple discharge 4. Fibroadenoma - most common benign growth, not precancerous, see both epithelium and glands
question
Briefly describe the different kinds of Proliferative (with Atypia) Benign Breast Diseases.
answer
1. Atypical ductal hyperplasia (ADH) 2. Atypical lobular hyperplasia (ALH)
question
What gene is mos frequently indicated in hereditary breast cancer? How frequently is breast cancer hereditary as opposed to sporadic?
answer
-BRCA1 and 2 account for ¹/₂ of hereditary breast cancers (Mutant gene defective in DNA repair) -Hereditary: 5-10% of all cases; Sporadic: 90-95% of cases
question
What are the two pathological classifications of Breast Cancer?
answer
In Situ (cells confined to the duct system, curable by surgery) 1. Lobular carcinoma in situ (LCIS) - less common (E-cadherin negative) 2. Ductal carcinoma in situ (DCIS) - more common Invasive (cells invade outside duct basement membrane into stroma and potentially into blood vessels (systemic spread) - Requires surgery and systemic therapy) 1. Infiltrating "ductal" carcinoma, NOS (10 yr survival) 2. Infiltrating carcinoma, Tubular (good prognosis) 3. Infiltrating carcinoma, Mucinous (good prognosis) 4. Infiltrating carcinoma, Medullary (good prognosis) 5. Infiltrating carcinoma, Lobular Classic
question
What is the name of the part of the endometrium that is influenced by pregnancy? When does it appear? What is its role?

answer
Decidua (hormonally influenced by pregnancy, modified fibroblasts) Appears 28 days post menstrual Acts as a physical and immunologic barrier
question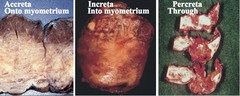
What is Placenta Creta? What are the different types?
answer
(1) Abnormally deep implantation -onto the myometrium, ACCRETA -into the myometrium, INCRETA -through the myometrium, PERCRETA or (2) Implantation in an area of deficient or absent decidua (endometrium) -lower uterine segment -cornu of uterus -scar, previous c-section, myomectomy -leiomyoma
question
What is Placenta Previa? What are the risks?

answer
Abnormally low implantation - may be "complete", "partial", or "low lying" Risk of antenatal, painless vaginal bleeding Must have C-section delivery because the baby can not be delivered through the placenta (risk of bleeding is too high)
question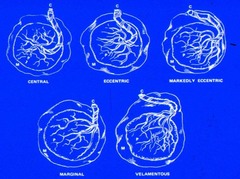
What is Velamentous Insertion of the Umbilical Cord? What are the associated risks?
answer
Abnormal insertion of the umbilical cord that leaves some of the major vessels unprotected Risk: Increased risk for thrombosis or rupture of the unprotected vessels
question
What problems are associated with decreased or absent umbilical cord spiraling? Increased spiraling?

answer
Absent or decreased spiraling: single umbilical artery, fetal growth problems, aneuploidy, diabetes Increased spiraling: diabetes, preeclampsia, growth restriction, increased risk for torsion, stricture, and intrauterine fetal demise
question
What are the layers of the fetal membrane?
answer
2 layers: Amnion and Chorion Amnion has 5 distinct layers, but is only 0.02-0.5 mm thick (the membranes are thin but strong!) Chorion has 4 layers and measures 0.1-1.5 cm thick (the membranes are thin but strong!) Maternal decidua interfaces with free membranes
question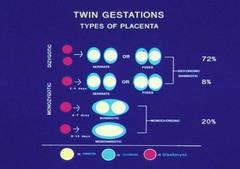
How many amnions and chorions are there for dizygotic twins? Monozygotic twins?
answer
Dizygotic: 2 Amnion, 2 Chorion Monozygotic: 2 Amnion, 2 Chorion or 2 Amnion, 1 Chorion or 1 Amnion, 1 Chorion
question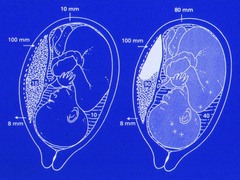
What is Abruptio Placenta?
answer
Clinical diagnosis of antepartum hemorrhage after 20 weeks (vaginal bleeding or concealed) resulting in a retroplacental hematoma May result in uterine pain or tenderness, no relaxation between contractions, and fetal distress or death Note that that part of the placenta will no longer be functional and there will be reduced O₂ transmission, as well as increased pressure on the amniotic sac
question
What effect does maternal diabetes have on the fetus?
answer
Maternal hyperglycemia results in large amount of glucose that crosses placenta => fetal overgrowth, macrosomia, shoulders may be large and difficult to deliver => Cardiomyopathy, hepatomegaly, polycythemia Fetus produces too much insulin => hypoglycemia at birth once maternal source of glucose is gone => increased risk for respiratory distress -Placenta is large (with large vessels), but it is not as functional -Risk of morbidity and mortality increases with poor glucose control, higher in insulin dependent diabetics -Increased in utero fetal demise -Increased congenital malformations -Increased hemoglobin, hyperbilirubinemia and thromboses
question
What are some of the placental causes of prematurity?
answer
Infection (37%) Maternal vascular abnormalities (31%) Mixed infection and vascular abnormalities (8%) Abruption (6%) Chronic villitis (8%) Normal (10%) (Uterine over distention, cervical incompetence, Fetal conditions, IUGR, malformations, Maternal periodontal disease)
question
What are some of the risk factors for prostate cancer? What is the rationale for screening? What are the screening recommendations?
answer
Risk Factors: Advanced Age, African American, Family history (men with prostate, women with breast), Obesity Screening rationale: Prostate ca is usually asymptomatic, by the time there are sx, it is usually far advanced Screening: annually starting at 50; if 1° relative or AA, start at 45; if multiple family members, start at 40 Test PSA at 40, If PSA is: 2.5 - prostate biopsy
question
How do the levels of free Prostate Specific Antigen (PSA) change in Benign Prostate Hyperplasia (BPH)? In Prostate Cancer?
answer
BPH - Higher percent of free PSA 25% or above Prostate cancer - Lower percent of free PSA 10% or lower
question
What is the histology of most Prostate Cancers? How are they staged?
answer
95% of prostate cancers are adenocarcinomas Gleason Scoring: Majority Score + Highest Score = Gleason Score Low grade = 6 (e.g. 3+3) Intermediate = 7 High grade = 8-10
question
What are the treatment options for prostate cancer?
answer
Definitive Local Treatment -Surveillance -Radiotherapy -Radical Prostatectomy Advanced Local Treatment -Combined Hormone and/or chemotherapy with definitive local therapy (Radical prostatectomy or Radiation therapy)
question
Where does Prostate Cancer typically metastasize to?
answer
Pelvic lymph nodes (Obturator, Hypogastric, External iliac) Axial skeleton, ribs Liver or lung in late stages only
question
What are the risk factors for bladder cancer?
answer
Risk Factors: Male:female (3:1) Cigarette Smoking (~50% cases) Occupational exposure (~20% cases) -- Arylamines, Rubber, Aluminum, Leather, Dye, Printing industry Infection - Schistosoma hematobium
question
How does bladder cancer typically present?
answer
Hematuria present in 85% of cases (Gross hematuria, Usually Painless, or Microhematuria) Painful urination Urinary frequency
question
What are the different pathologies of bladder cancer? Which is most common?
answer
Transitional Cell Carcinoma (TCC) - 90% Squamous Cell Carcinoma (SCC) - 7% -85% of cases in Egypt secondary to Bilharzial infection (schistosomiasis) -Chronic irritation Adenocarcioma - 2%
question
What are the treatment options for Bladder Cancer? What are the common sites of metastases?
answer
If Superficial: Surveillance or Intravesical Therapy (BCG) Radical Cystectomy may be indicated Chemotherapy for advanced disease (MVAC) Mets: Lung, Liver, Bone
question
In what part of the kidney is cancer most likely to appear? What type of kidney cancer is most common? What are the risk factors for kidney cancer?
answer
Renal parenchyma 85% Renal Cell Carcinoma (clear cell) is most common Renal pelvis 15% Transitional Cell Carcinoma (TCC) Risk Factors: Male:female 2:1 No racial preference Acquired renal cystic disease of dialysis (40x greater risk!)
question
What syndromes are associated with hereditary Renal Cell Carcinoma?
answer
(1) Von Hippel-Lindau Clear cell renal cell carcinoma (2) Tuberous Sclerosis Clear cell renal cell carcinoma (3) Hereditary papillary renal cell carcinoma Met proto-oncogene mutations 7q 31-34 Encodes hepatocyte growth factor
question
What are the risk factors for Renal Cell Cancer? How does kidney cancer typically present? How common are metastases at presentation? How is the prognosis is there are metastases?
answer
Risk Factors: Obesity, Hypertension, Cigarette Smoking Presentation: Classic Triad = Hematuria (gross or microscopic) + Flank pain + Palpable abdominal mass (Classic triad rarely observed together anymore because once it appear like this, it is fairly advanced -- now it is more commonly picked up incidentally) May also present with paraneoplastic syndromes ("Internist tumor" - hypercalcemia, constitutional symptoms, etc.) 25 - 30% have metastases at diagnosis Median survival 12 - 18 months
question
How are Renal Cysts typically categorized? What kind of follow-up is required for each category?
answer
Bozniak Staging I: Well-defined margin, homogeneous, water dense, no enhancement - normal finding; no follow-up necessary II: Few thin septa (1mm), or multiple septa; require aggressive follow-up IV: Irregular or thickened walls, septa, or solid areas ± enhancement; treat like cancer
question
How is kidney cancer treated?
answer
Depending on the size, try to preserve as much normal kidney as possible... -Partial nephrectomy -Radical nephrectomy -Vena caval thrombectomy If there is a single metastasis, resect it; if more than one, may need systemic therapy
question
What is the most common neoplasm in young men? What are the presenting symptoms?
answer
Testicular Cancer Presentation: Swollen, painless mass in the testis is the most common (may also be painful)
question
Who is typically affected by Testicular Cancer? What are the risk factors?
answer
Bimodal age distribution Risk factors: Undescended testicle Maternal estrogen exposure Contralateral testis tumor Whites 5-6x more common than Blacks 25% subfertile semen parameters
question
What are the typical pathologies of Testicular Cancer? What are the markers for Testicular Cancer? What do they indicate?
answer
Pediatric -Germ cell tumors -Interstitial tumors e.g. Leydig cell Adult -Germ cell tumors: Seminoma or Non-seminoma (Embryonal, Choriocarcinoma, Yolk Sac Tumor) -Lymphoma (Most common over age 50) Markers: βHCG and AFP Embryonal Carcinoma: ±βHCG, ±AFP Seminoma: ±βHCG, -AFP, +LDH Yolk Sac: -βHCG, +AFP Choriocarcinoma: +βHCG, -AFP
question
Where do testicular cancers commonly metastasize to?
answer
Left testicle: periaortic nodes Right testicle: pericaval nodes
question
How is a Low Stage Testicular Seminoma treated? High Stage?
answer
Low Stage -Radiotherapy -2% relapse rate -Follow-up less rigorous High Stage -Chemotherapy as for NSGCT
question
What six important issues need to be addressed when evaluating male factor infertility?
answer
1. Sexual history 2. Pregnancy history 3. Current therapy (oral testosterone makes a man infertile!) 4. Childhood diseases (e.g. torsion, tumor, varicocele, cryptorchidism) 5. Medical or surgical problems (e.g. High fevers/debilitating illnesses, Retroperitoneal surgery Pelvic injury, TURP, Herniorrhaphy (Mesh), Chemotherapy/XRT) 6. Gonadotoxins
question
Why does pyospermia cause infertility?
answer
WBCs are a major source of reactive oxygen species (ROS) Direct damage to sperm Lipid peroxidation via chain reaction Possible sperm DNA damage1
question
What are the two most commonly utilized tests of sperm function?
answer
(1) Strict morphology index (SM) - Kruger Morphologic Criteria measures head, neck and tail ratios (2) DNA fragmentation assay (Sperm of infertile men has ↑ level of DNA damage; DNA damage is associated with impaired post fertilization embryo cleavage) These tests are important in determining if fertilization will take place and if the embryo will grow normally
question
What could you infer from finding sperm in the seminal vesicle?
answer
There is an outflow obstruction in the semen pathway, and the semen is being backed up into the seminal vesicle
question
What are the top 3 reasons for male infertility?
answer
1. Varicocele 2. Idiopathic 3. Obstruction
question
What is a Posterior Urethral Valve? What does it cause? Is the obstruction typically complete or partial?
answer
An obstruction of the urethra due to the presence of abnormal valves or folds in the posterior urethra Effects: -Obstruction of the bladder => Increased pressure during voiding and impaired emptying -Eventually causes both bladder and kidney damage from the increased pressure Only partial valves are seen clinically. Complete obstruction results in fetal demise.
question
What is the pathophysiology of the following organs in Posterior Urethral Valve: Kidney Bladder Lung What is the "Pop Out" Mechanism as it relates to Posterior Urethral Valve?
answer
Kidney -Alteration in growth regulation -Production of interstitial fibrosis -Alteration in developmental regulation of the renin-angiotensin system Bladder -Marked increase in growth and connective tissue deposition -Alteration in the local renin-angiotensin system Lung -Impaired growth and maturation -Mechanical or humoral mechanism? Pop Out: A protective mechanism to release pressure in the GU system -- includes Calyceal rupture, Bladder rupture, Bladder diverticulum, Severe unilateral reflux, VURD syndrome
question
What is the presentation of prenatal Posterior Urethral Valve? Presentation at birth? Presentation in a child? What management is recommended for each situation?
answer
Prenatal: In utero hydronephrosis; Bilateral hydronephrosis; Dilated bladder; "Key hole" sign; Oligohydramnios -Management: rarely indicated unless severe oligohydramnios At birth: Varies dependent on renal damage and degree of oligohydramnios -- Septic shock; Pulmonary failure; Renal failure to asymptomatic -Management: Transurethral valve ablation (TUR) (Incise valve to damage leaflet) Child: UTI; Incontinence; Eneuresis; Renal Failure -Management: Primary transurethral valve ablation
question
What is the presentation of Testicular Torsion? What are the two different kinds? Briefly describe them. How is it trated?
answer
Presentation: Acute, severe pain, Nausea and vomiting, Sympathetic response 2 Types: 1) Extravaginal (less common, perinatal only) -Torsion of entire cord proximal to tunica vaginalis attachment -Salvage of torsed testes unlikely -Causes sterility and hormonal insufficiency 2) Intravaginal (pernatal and older - 8-30 y/o) -Torsion distal to tunica vaginalis attachment -Bell-Clapper or horizontal lie predisposes to torsion -Salvage rates are good in first 6 hours, but rapidly decline to 5% in 24 hours Tx with immediate surgery to salvage! If you suspect it, do surgery! Don't even wait for an ultrasound -- you only have a window of 6 hours to salvage the testicle!
question
What are Appendices Epididymis and Appendices Testes? How does torsion of these appendices present?
answer
Appendices are paratesticular attachments that are embryologic remnants: -Appendix testes - Müllerian system -Appendix epididymis - Mesonephros Presentation: Slow, gradual onset over days; Less nausea and vomiting; Pain related to inflammation caused by necrotic structure; "Blue Dot Sign" (see necrotic appendage through scrotum skin) Tx: Anti-inflammatories, Analgesics, Scrotal support
question
What is Epididymal Orchitis? What causes it in children? In young men? In old men? How is it treated?
answer
Infectious process Children - UTI "Young Man's" - STD "Old Guy's" - UTI Treat with antibiotics
question
What is Vesicoureteral Reflux? What does it put the patient at risk for? How does it present? How is it managed?
answer
Flow of urine in a retrograde fashion from the bladder to the kidney with voiding (Ureter fails to collapse with voiding) Risk: Bacteria in bladder gain access to the upper urinary tract (kidney) => Cystitis becomes pyelonephritis => Pyelonephritis results in scarring of kidney => Scarring impairs renal function and predisposes to hypertension Presentation: Prenatal hydronephrosis Systemic illness (Pyelonephritis, Sepsis, Vomiting, Failure to thrive) Sibling screening (it's inherited!) Management: Actively work to find reflux patients Boys with UTI should get Voiding cystourethrogram (VCUG) Girls with febrile UTI or recurrent UTI should get VCUG Confirmed prenatal hydronephrosis should get VCUG ↓ Aggressive management of patients with reflux Prophylaxis (with Abx) or surgery Periodic VCUG for medical management patients
question
What is a common cause of bladder outlet obstruction in adult males? What are the symptoms? What other things might be on your differential diagnosis?
answer
-Benign Prostatic Hyperplasia (most common benign neoplasm in men, and prevalence increases with age) -Symptoms of lower urinary tract may be obstructive (impaired flow, hesitancy, incomplete emptying, intermittency, straining to void, urinary retention / overflow) or irritative (dysuria, urgency, frequency, nocturia, urge incontinence) -DD: UTI, Urethral stricture, Prostate cancer, Bladder Cancer, CIS, Neurogenic bladder (DM, spinal disease), Medication side effects -Management: Watchful waiting + Medical Therapy: 1) α-adrenergic blocking agents (terazosin (Hytrin), doxazosin (Cardura), tamsulosin (Flomax), alfuzosin (Uroxatrol)) 2) 5-α reductase inhibitors (block conversion of Testosterone to DHT) (finasteride (Proscar) (type 2 inhib. only) or dutasteride (Avodart) (type 1 and 2 inhib.))
question
What are the treatment options of Benign Prostatic Hyperplasia? What are the side effects of the drugs?
answer
1. Watchful waiting 2. Medical Therapy a. α-adrenergic blocking agents (terazosin (Hytrin), doxazosin (Cardura), tamsulosin (Flomax), alfuzosin (Uroxatrol)) SE: orthostasis, dizziness, fall risk in elderly, cardiovascular effects, ejac. dysfn b. 5-α reductase inhibitors (block conversion of Testosterone to DHT) (finasteride (Proscar) (type 2 inhib. only) or dutasteride (Avodart) (type 1 and 2 inhib.)) SE: ED, loss of libido, ejac. dysfn, gynecomastia; alters baseline PSA! 3. Minimally invasive procedures (microwave, thermotherapy, radio frequency ablation (TUNA, etc.), stent) 4. Surgery TURP; Open prostatectomy (gland size)
question
What are the different types of Urinary Incontinence?
answer
1. Stress Incontinence bladder neck hypermobility intrinsic sphincteric deficiency neurogenic dysfunction 2. Urge Incontinence unstable bladder, detrusor instability detrusor hyperreflexia 3. Overflow incontinence underactive or atonic detrusor outlet obstruction (male- prostatic disease, urethral stricture) (female- prolapse, post-surgical)
question
How is Urinary Incontinence managed? What are the side effects of the medication?
answer
1. Identify and correct transient factors (delirium, infection, atrophic vaginitis, drug side effect, impaired mobility, fecal impaction) 2. Behavioral Therapy; Devices 3. Medical therapy: Anticholinergic agents: oxybutinin chloride (Ditropan), propantheline bromide (Pro-Banthine), tolterodine tartrate (Detrol), trospium chloride (Sanctura) SE: blurred vision, dry mouth, constipation, cardiac effects, mental status changes, contraindicated in narrow angle glaucoma 4. Surgical Stress: bladder neck suspension, fascial sling, artificial urinary sphincter, urethral bulking agents (collagen, Durasphere) Urge: augmentation cystoplasty, neuroelectrical stimilator systems Overflow: correct obstruction; CIC
question
What is the difference between complicated and uncomplicated urogenital infections?
answer
Uncomplicated: short course therapy; commonly used agents normal anatomy, normal physiology Complicated: longer course therapy abnormal anatomy, abnormal physiology or immunocompromised
question
When is surgical intervention required for kidney stones?
answer
acute infection with obstruction is a surgical emergency; drainage critical; treat stone later!



