Adrenal Insufficiency and Adrenal Replacement Therapy – Flashcards
Unlock all answers in this set
Unlock answersquestion
Addison's disease definition
answer
patients with chronic adrenal insufficiency secondary to AI destruction of the adrenal glands
question
adrenal insufficiency definition
answer
hypofunction of the adrenal cortex with impaired production and secretion of cortisol, aldosterone, and adrenal adrogents
question
clinical manifestations f adreanl insufficiency
answer
*primarily due to the deficiency of cortisol* - essential for survival uring ties of stress
question
two categories of adrenal insufficiency
answer
1. primary - disorder of the adrenal glands - anatomic destruction of these glands 2. secondary (central) - failure of the pituitary to secrete ACTH, leading to dadreanl cortico hypofunciton and eventual atrophy
question
primary adrenal insufficiency etiologies: destruction of the gland (chronic or acute)
answer
1. AI adrenalitis - isolated, sporadic - associated with other AI disorders 2. infectious adrenalitis - think AIDS 3. infiltrative diseases - metastatic cancer - amyloid - sarcoid 4. bilateral massive adreanl hemorrhage 5. surgical resection
question
primary adrenal insufficiency: metabolic defects
answer
1. congenital adrenal hyperplasia - less synth and release of cortisol 2. drug induced - ketaconazole - etomidate - inhbits 11Bhydroxylase activity, the final step in cortisol biosynthesis 3. adrenoleukiodystrophy
question
secondary adrenal insufficiency: suppression of the HPA axis
answer
1. exogenous glucocorticoids - after withdrwal 2. excess endogenous glucocortiocids from a primary adrenal tumor after resection 3. high dose megestrol or chronic opiod use
question
secondary adrenal insufficiency: hypopituitarism or pituitary diseas
answer
adenomas, mets, infection, infiltrative disease trauma aneurysm
question
AI adrenalitis: mechanism
answer
1. cellular and humoral immune mechanisms to do this 2. other endocrine organs also affected in half patients
question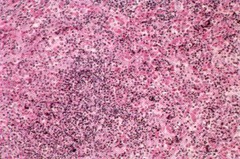
autoimmune adrenalitis histology
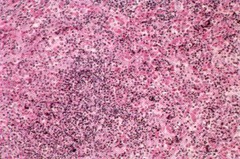
answer
adrenal fibrosis and atrophy associated with lymphocytic infiltration anti-adrenal antibodies found in 70-90% of patients
question
AI adrenalitis: common antibody
answer
anti-21 hydroxylase actiivty;
question
polyglandular AI syndrome
answer
presence of 2+ AI endocrine disorers in one patient is called this
question
polyglandular AI syndrome type I
answer
autoimmune polyendocrinopathy candidasis ectodermal dystrophy (APECED) 1. AR genetics 2. AIRE
question
polyglandular AI syndrome type I clinic
answer
in childhood with either 1. hypoparathyroidism due to AI desruction of the parathyroids or against the calcium sensing surface receptors on the parathyroids - destruction decreases PTH - autoantibody to the surface receptor causes the PTH to shut down even at subnormal Ca levels 2. chornic mucocutaneous candidiasis due to defective T cell mediated antifungal immunity - autoantibodies to IL17 and IL22 impairing the Th17 resposne for fungus
question
so APECED syndrome summary
answer
1. AR - mutation in the AIRE gene 2. primary hypoparathyroidism onset before age of 10 3. chronic mucocutaneous cnadidasis beore the age of 10 4. AI adrenalitis: onset age 10-15 eyars
question
polyglandular AI syndrome type II: aka Schmidts syndrome
answer
much more prevalent 1. priary adrenal insufficiency is major and the initial manifestation 2. half caes are familial but no single mutation implicated 3. can present in 20-40 years
question
polyglandular AI syndrome type II summary
answer
1. half of cases are familial 2 onset in young adults (20-40s) 3. AI adrenalitis with adrenal insuffciency presenting symptom 4. AI thyroid disease 5. T1DM
question
infectious adrenalitis
answer
Tb, fungal, some viral TB is huge cause worldwide in US, more common in HIV/AIDS patients -- CMV with necrotizing adrenalitis -- mycobacterium avium intracellare: this as well *hypotension alone without the other symptoms/signs*
question
bilateral massive spontaneous adrenal hemorrhage: acute
answer
acute destruction of both glands leading to acute primary adreanl insufficiency; *refractory hypertension* but can have 1. acute abdominal pain 2. fever 3. vomiting 4. delerium
question
bilateral massive spontaneous adrenal hemorrhage: chronic
answer
sepsis, burns, trauma + predisposing condition ofr bleeding and thrombosis - anticoags, thrombocytopenia, DIC, antiphospholipid syndrome
question
bbilateral massive spontaneous adrenal hemorrhage: patho
answer
severe stress leading to increased ACTH 1. enhanced adrenal arterial blood flow 2. catecholamine release from the medulla, leading to venoconstrictio nof the central vein 3. high pressure leads to rupture associa
question
Waterhouse Fridericksen syndrome
answer
DIC with bacterial sepsis leading to destruction of the
question
Congenital Adrenal Hyperplasia: what is it
answer
group of AR disorders that abolish the activity of a step essential to the biosynthesis of cortisol - decreased production of cortisol - compensatory increase in ACTH --- the chronic increase in circulating ACTH leads to the hyperplasia, increased production of steroids proximal to enzymatic defect, decreased prodcution of steroid hormone end products distal tot ht edefect
question
pathophys of CAH
answer
1. gene mutations leadto reduction in enzyme activity for cortisol synthesis 2. decreased plasma cortisol, leading to chronically elevated ACTH by pituitarty 3. leads to - adrenal hyperplasia - increased production of steroids proxuimal to defective step - decreased prodcution of the steroids distal to the defect 4. clincial manifestations reflect the resultatn steroid hormone excesses and deficienceis.
question
CAH: most common cause
answer
reduced or absence activity of CYP21A2 (21 hydroxylase) - required for both the cortisol synthesis and for the synthesis of aldosterone
question
CAH: 21 hydroxylase: what occurs
answer
1. decreased cortisol production 2. increase in the ACTH chronically 3. increased prodcution of the hormones - DHEA - androstenedione 4. hyperplasia of the adrenal cortex
question
CAH: 21 hydroxylase deficiency in females
answer
signs of excess androgen production so 1. hirsutism 2. ammenorrhea 3. acne *milder forms* severe deficiency: 1. male or sexually ambiguous external genitalia in XX female --- pseudohermaphroditism -- increased adrenal androgen production during the early fetal development
question
CAH: 21 hydroxylase deficiency severe
answer
decreased aldosterone produciton 1. renal salt wasting, volume contration, hypotension, hyperkalemia *only with severe deficiency* decreased cortisol reserve predisposes to the development of adrenal cris: during periods of severe stress
question
other CAD forms: and hallmark
answer
1. 11B hydroxylase deficiecy 2. 17 alpha hydroxylase deficiency hallmark of these is the increase in the production of the weak mineralocorticoid 11 deoxycorticosterone by the zona fasciculata
question
overproduction of 11DOC
answer
1. 11B hydroxylase or 17 alpha hydroxylase deficiencies 2. increased production of 11DOC 3. hypertension and hypokalemia -- similar findings to that of primary hyperaldosteronism -- suppression of renin activity -- suppression of plasma aldo levels -- high levels of DOC
question
differentiating features of 11Bhydroxylase deficiency and 17alpha hydroxylase
answer
11B: increased adrenal production of DOC accompanied by increased androgen production 17a: both adrenal and gonadal production of sex steroid impaired thus: M: DHEA and androstenedione and testicular production of testosterone impaired F: impared ovariean estrogen synthesis
question
in F with 11 B hydroxylase deficiency
answer
hypertension with hypokalemia with suppression of renin and aldo increased DOC increased androgen, so presents similar to 21 hydroxylase (but not with increased DHEA and androstenedione)
question
in M and F with 17alpha hydroxylase/17,20 lyase def
answer
hypertension with hypolkalemia with hypogonadism
question
drugs that block 11B hydroxylase
answer
1. etomidate - anesthetic agent 2. ketoconazzole can lead to primary adrenal insufficiency
question
abiraterone
answer
used for advanced prostate cancer leading to 17a hydroxylase 17,20 lyase blocking this leads to adrenal insufficiency, especially during stress -- can cause hypertension and hypokalemia due to excess DOC production
question
adrenoleukodystrophy
answer
1. X linked 2. defective beta oxidation of fatty acids 3. high concentrations of very long chain fatty acids in the serum 4. progressive neurologic dysfunction 5. primary adreanl insufficiency
question
secondary adrenal insufficiency: important cuases
answer
1. glucocorticoid withdrawal 2. neoplastic diseases 3. inflammatory diseases 4. abrupt onsent secondary failure
question
glucocorticoid withdrwal pathophysiology
answer
1. chronic use of glucocorticoid therapy 2. suppression of CRH and ACTH release 3. ACTH deficiency chronically leads to atrophy of the zona fasciculata and reticularis of the cotex, sparing the glomerulosa -- thus aldo is ok 4. longer duration and higher doses associated with increasd risk
question
glucocorticoid withdrawal recovery
answer
HPA axis can take up to a year; recorvery of hypothalamus and pituitary precede recovery of the zona fasciculata to secrete cortisol
question
neoplastic diseases
answer
1. anything that destroys the pituitary, invades hypothalamus, the stalk, reducing CRH and ACTH can really causes this pituitary macroadenomas are important: loss of the pituitary ACTH reserve tends to occur late, usually after the loss of the reserve of other pituitary hormones
question
inflammatory disease
answer
1. AI hypophysitis - enlargemento f the pituitary with panhypopituitarism - mimics adenomas but the pattern of loss idffers: loss of ACTH occurs early, sometimes as an isolated hormone deficiency
question
AI hypophysitis associated wti
answer
women in the post partum period that
question
abrupt onset secondary adrenal failure
answer
1. rapid destruction of pituitary or injury of the stalk so 1. post partum pituitary necrosis 2. hemorrhage 3. trauma 4. surgery to pituitary they lose ACTH immediately then, they use ACTH for weeks, getting normal cortisol response; this is how long it takes for adrenal cortical atrophy to occur after loss of endogenous ACTH
question
adrenal insufficiency: clinic features of primary and secondary
answer
Occurs in 80-100% of pts 1. weakness 2. weight loss 3. anorexia, nausea, vomiting 4. hypotension (BP< 110/70) occurs in 10-40% of pts 1. abdominal pin 2. diarrhea, constipation 3. sexual dysfuction 4. behaviroal and psychiatric 5. hyponatremia 6. hypoglycemia
question
adrenal insufficiency: clincial features seen only in the chronic primary form
answer
1. hyperpigmentation (90-100%) 2. hyperkalemia 3. hyperchloremic acidoses 4. salt craving
question
when should adrenal insufficiency be on the DD
answer
unexplained (and/or situation here) 1. hypotension 2. hyponatremia 3. hypoglycemia
question
acute adrenal insufficiency: hemodynamics
answer
1. low systemmic vascular resistance with 2. high or normal cardiac output similar to those in septic or anaphylactic shock
question
chronic stable insufficiency hemodynamics
answer
1. CO tends to decline 2. blod pressure are not absolutely low but maybe in the low normal range
question
secondary adrenal insufficiency: hemodynamics
answer
1. reduction in BP 2. normal or increased intravascular tone
question
adrenal insufficiency: hypoglycemeia
answer
only after period of prolonged food deprivation; caused by ipaired hepatic gluconeogenesis; - primary defense against hypoglcemia during prolonged food deprivation
question
adrenal insufficiency: hyponatremia
answer
seen in both secondary and primary forms: 1. cortisol: impairs renal excretion of free water -- SIADH because: cortisol has a tonic inhibitory effect on ADH and secretion and AQP2 expression in the cortical colecting duct so if ust a cortisol disease, then yponatremia without volume contraction (add in the aldo in Addison's, then you get a volume contraction)
question
primary failure and renal issues
answer
1. impaired aldosterone 2. increased loss of sodium 3. volume contraction 4. decreased renal perfusion -- impaired renal excretion of free water 5. thus, hyponatremia that is *associated with volume depletion*
question
summary: hyponatremia in secondary failure vs primary
answer
if failure is secondary (just cortisol bc ACTH doesnt really do much with aldo) then 1. chronic inhibition of ADH is lifted 2. SIADH 3. euvolemia4. normal BUN, serum creatinine, K level primary 1. decreased cortisol lifts the ADH inhibition 2. decreased aldo leads to salt and water wasting, increased K level, eventual volume contraction with consequent hypoperfusion and kidney damage 3. leads to hyponatremia with eleveated BUN, serum creatinine and K, and hyperchloremic acidosis
question
hyperpigmentation
answer
in Addisons due to the increased ACTH - has melanocyte stimulating activity
question
adrenal crisis
answer
1. adrenal insufficiency 2. cardiovascular collapse - BP < 90/60 - tissue underperfusion and ultimate failuire 3. hypotension unresponsive or only partially responsive to volume expansion or pressors
question
clinical features of adrenal crissis
answer
1. often precipitated by acute severe intercurrent illness or other stressful events 2. CV collapse - marked hypotension - refractory to volume loading and pressors - manifestationso f multiple organ underperfusion 3. fever 4. abdominal pain 5. hypoglycemia 6. confusion/delirium *need to give stress doses of GC stat, as this is an emergency*
question
Dx
answer
1. decreased cortisol secretion and/or imparied secretory reserve 2. is it ACTH dependnet
question
8 am plasma cortisol
answer
if > 20 then you can exclude it if < 3 ug/dl, then some evidence, but no diagnsosis; need ACTH stimulation
question
rapid ACTH stimulation test
answer
give the patient a synthetic ACTH prep; then, there are high levels of ACTH in the blood; - reserve capacity of adrenal cortex; - check levels before and after (30 and 60 minutes) - if greater than 20 ul increase then there is a normal response if primary: then there will be little to no incrase due to the facft that ACTH is already high in these pts if secondary: - subnormal incrase (<20), due to adrenal cortex arophic but not completely destroyed
question
ACTH stimulation test in those that are in a special group
answer
if it is an acute issue (like a stalk transection) - the ACTH response may be normal for 3-4 weeks so that you need to wait before the atrophy occurs
question
replacement therapy in pregnancy
answer
hydrocortisone is the agent of choice dont use dexamethasone
question
Tx of CAH
answer
longer acting preps are preferred; this is because there want to suprresss the elebvated ACTH; this leads to the overproduction of androgens and the other things;
question
aldo replacement
answer
not in secondary in those with addisons: reduce salt craving and the need for continuous high salt intake; fludrocortisone;



