Emory PA – Dermatology Module – Flashcards
Unlock all answers in this set
Unlock answersquestion
Freckles (Ephelis)
answer
*Pathogenesis*: Increased melanin in basal keratinocytes; *number of melanocytes are normal*
question
Lentigo (plural lentigines)
answer
*Pathogenesis*: *Increased number of melanocytes* *Histology*: Hyperpigmented basal cell layer
question
Melasma

answer
*Basics*: Patchy hyperpigmentation of face *Pathogenesis*: *Increased melanin production, also increased melanocytes in areas of involvement* *Clinical*: Chloasma: mask of pregnancy
question
Nevus

answer
*Gross*: Appearance of nevus cells by location i. Epidermis and upper dermis (Junctional) - Macule ii. Middle dermis (Compound) - Papule or nodule iii. Lower dermis (Intradermal) - Small papule or macule with hair *Histology*: Appearance of nevus cells by location i. Epidermis and upper dermis - Epithelioid in appearance with a cuboidal or oval shape, indistinct cytoplasm and round to oval nucleus and are pigmented ii. Middle dermis - Smaller with a lymphoid appearance and do not contain pigment iii. Lower dermis - Spindle cell appearance resembling fibroblasts
question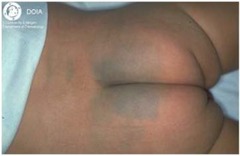
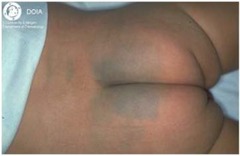
Mongolian Spot
answer
Congenital
question
Melanoma

answer
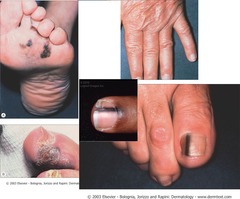
*Basics*: Cancer of melanocytes i. Lentigo maligna: Radial growth, good prognosis ii. Nodular: vertical growth, poor prognosis ii. Acral lentiginous (in Blacks and Asians): palms, soles, nail beds *Pathogenesis*: i. *Familial*: *CDKN2A gene mutated* (encodes three different tumor suppressors with *loss of p16/INK4a* implicated in human melanoma): 40% ii. *Sporadic* melanomas: - BRAF (activating mutation supporting cell growth): 60-70%. Sun-exposed skin. *Treatment*: MEK inhibitor - NRAS (activating mutation supporting cell growth and survival): 10-15%. Sun-exposed skin. - CDKN2A mutated in ~10% of sporadic melanomas. - Receptor Tyrosine Kinase (RTK) c-Kit mutation. Non-sun-exposed. - Epigenetic silencing of PTEN: rare. *Gross*: ABCDE: Asymmetry, Border irregularity, Color variance, Diameter, Evolving *Histology*: Pategoid cells *Prognosis*: Tumor Thickness: as measured from granular layer of epidermis to greatest depth of tumor invasion by using an ocular micrometer as described by Breslow. *Breslow thickness is single most important prognostic factor in primary cutaneous melanoma* (linear relationship between tumor thickness and survival, the more shallow the better) *Treatment*: *B-Raf inhibitors that are specific for the V600 mutations (Vemurafenib) should not be used to treat B-Raf wildtype tumors because it can actually promote tumor growth*
question
Nodular Melanoma

answer
*Pathogenesis*: *Vertical growth from the beginning, Lacks radial growth phase* *Histology*: Well circumscribed proliferation of atypical melanocytes
question
Lentigo Maligna Melanoma

answer
*Basics*: Radial growth, good prognosis. - Lentigo maligna or in-situ melanoma = radial phase. - Lentigo Maligna Melanoma = vertical phase
question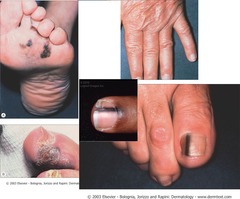
Acral lentiginous
answer
*Basics*: (in Blacks and Asians): palms, soles, nail beds
question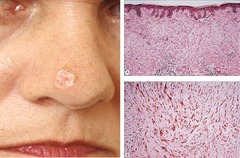
Desmoplastic melanoma
answer
*Histology*: *stains NEGATIVE for HMB-45, but POSITIVE for S-100*
question
Seborrheic keratosis (SK)

answer
*Basics*: Benign squamous proliferation; common tumor in the elderly. *Gross*: Raised, discolored plaques on the extremities or face; often has a coin-like, waxy, 'stuck-on' appearance. *Histology*: Characterized by keratin pseudocysts *Clinical*: *Leser-Trelat Sign*: sudden onset of multiple seborrheic keratosis and suggests underlying carcinoma of the GI tract.
question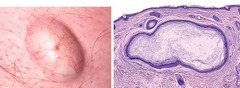
Epithelial Inclusion Cyst
answer
*Gross*: *Multiple epidermal cysts* on the face and scalp ! *Clinical*: *Gardner Syndrome*: rare autosomal dominant condition associated with *familial adenomatous polyposis*
question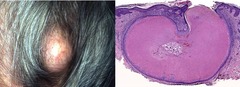
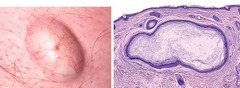
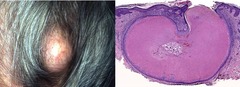
Pilar Cyst
answer
*Basics*: *Most common cyst of the scalp* *Histology*: No granular cell layer before you get to keratin.
question
Dermatofibroma

answer
*Basics*: Firm brown to tan (many other colors as well) papule or nodule that may become flatter with time *Clinical*: "Dimple sign" pinching results in central dimpling. Lower legs of young, middle-aged women.
question
Dermatofibrosarcoma protuberans

answer
*Basics*: Flesh-colored or red-brown irregular nodule on the trunk and proximal extremities of middle-aged adults *Histology*: Radial arrangement of fibroblasts resembling a *pinwheel, referred to as storiform*. Thinning of overlying epidermis. *Clinical*: Trunk and proximal extremities of middle-aged adults.
question
Lipoma

answer
*Basics*: Benign fat tumor *Gross*: indistinguishable from normal fat *Histology*: Encapsulated tumor composed of normal fat cells (with lots of blood vessels - angiolipoma)
question
Neurofibroma
answer
*Basics*: Neurofibromatosis - Autosomal dominant with 1 in 3000 live births *Gross*: Flesh colored rubbery papules or nodules *Histology*: Poorly circumscribed dermal proliferation.
question
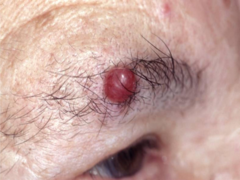
Pyogenic Granuloma

answer
*Basics*: AKA Lobular Capillary Hemangioma. MISNOMER - These are not pyogenic (pus forming) and not granulomas. Benign vascular neoplasm *Gross*: Dome-shaped papule or nodule, Yellow to red, with moist to scaly surface, Most common locations are head, neck, and fingers. May involve gingival mucosa particularly in pregnant females
question
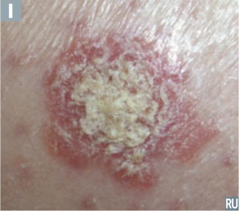
Actinic Keratosis (AK)
answer
*Gross*: - Erythematous, scaly, rough papules or plaques +/- adherent yellow crust. - May produce a "cutaneous horn". *Histology*: Basal cell layer atypia (dysplasia)
question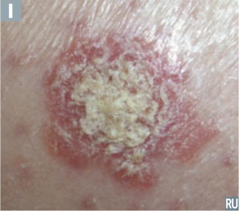
Squamous Cell Carcinoma
answer
*Basics*: Second most common skin cancer. *Pathogenesis*: Most common cause is DNA damage due to ultraviolet radiation leading to p53 mutations. In the absence of functional p53, UV damage does not initiate cell cycle arrest. *Histology*: - Well-differentiated: Intracellular bridges forming keratin. - Poorly-differentiated: Dyskeratotic cells
question
Keratoacanthoma

answer
*Treatment*: Preferred treatment is surgical excision
question
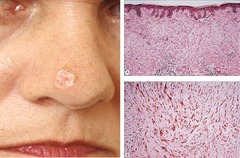
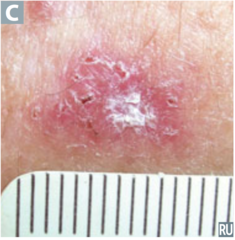
Nodular (Classic) Basal Cell Carcinoma

answer
*Pathogenesis*: Mutation in *PTCH* or human homologue of the Drosophilia developmental gene patched. - Basal cell carcinomas are commonly associated with inactivating mutations in PTCH (Gorlin syndrome) and activating mutations in SMO (either leading to increased GLI1 expression, and subsequent cyclin D expression). The absence of PTCH causes constitutive activation of SMO, leading to the development of basal cell carcinoma. *Gross*: - Nodular growth on the face, especially the nose. - Pearly papule with telangiectasias, central depression or crater with a rolled border - "Rodent ulcer" *Histology*: Clefting, palisading.
question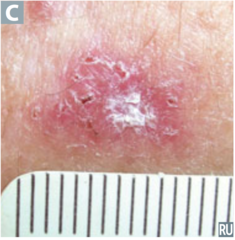
Superficial BCC
answer
*Clinical*: Trunk
question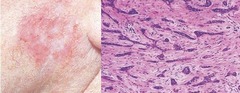
Morpheaform BCC
answer
*Gross*: Ivory-white, scar-appearing plaque
question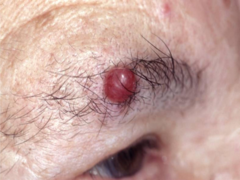
Merkel Cell Carcinoma
answer
*Basics*: Merkel cells are essential in light touch reception. Merkel cell carcinomas are very aggressive. *Gross*: Pink-to-blue-to-red-brown nodule. *Treatment*: X-ray shown only to reduce lymph node metastasis and local recurrence, does not affect mortality.
question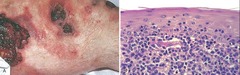
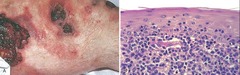
Mycosis Fungiodes
answer
*Gross*: Scaly red-brown patches or scaling plaques resembling psoriasis or fungating nodules *Histology*: Sezary-Lutzner cells (helper T-cells) that form band-like aggregates within the superficial dermis and invade epidermis as single cells and small clusters (Pautrier microabscesses)
question
DX: Molluscum Contagiosum Symptoms: Skin bumps- painless, although they may be itchy, red, swollen and/or sore. Appearance: small white, pink, or flesh-colored raised bumps or growths with a dimple or pit in the center. Discrete pearly papules with central umbilication. The bumps are usually smooth and firm. In most people, the growths range from about the size of a pinhead to as large as a pencil eraser (2 to 5 millimeters in diameter). The bumps may appear anywhere on the body, alone or in groups. DX: Based on Appearance. Causative agent: poxvirus Transmission: Skin to skin. May be sexually transmitted. RX: self limited. May take up to 2 years for natural resolution. Cryotherapy. Topical acids. Curettage. CO2 lased. Aldara/Zyclara. Veregen.
answer
...
question
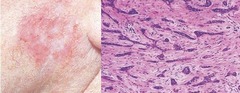
Tinea Corporis Symptoms: Dermatophyte infection of the glabrous skin. Presents with an expanding circular or serpigenous scale. Symptoms include itch or burning. Causative agent: Can be caused by many different organisms. DX: KOH preparation hyphae will be present. Fungal culture colonies take 2 weeks to grow. Biopsy. Wood's Light examination (only Microsporum canis will fluoresce in humans). Transmission: Can be infected by a variety of sources including pets. RX: Topical Antifungals BID application for 2-4 weeks. Oral Antifungals for more severe infections. Notes: Avoid Steroids
answer
...
question
Tinea Capitis Symptoms: Loss of hair in affected area. Hair follicle appears thin a brittle on plucking. Kerion formation occasional. DX: appearance and suspicion. Can take a hair sample with plucking in center of affected area. Causative agents: Trichphyton tonsurans. Microsporum canis. Usually treated with oral agents as infection is of both scalp and hair. Use topical antifungal while awaiting cultures if concern of alopecia or pt will loose all hair!
answer
...
question
Tinea Pedis Often coexists with Tinea unguium. Symptoms: Fungal rash on feet and or nails showing spreading edge. DX: skin scraping at parameter of rash. RX: Treatment is topical for skin. Treatment for nails: Lamisil oral and topical. Sporonox. Penlac - topical. Vinegar soaks
answer
...
question
DX: Tinea Versicolor Symptoms: spreading rash Most common on the trunk, but can spread to extremities Causative agents: Malassezia furfur or Pityrosporum ovale. DX: skin scraping for culture. RX: prevention, topical antifungals and in severe cases a course of oral antifungals. Notes: Avoid steroid usage
answer
...
question
DX: Tinea Cruris Symptoms: often looks like Tinea pedis. DX: skin scraping. RX: Topical Antifungals BID application for 2-4 weeks. Oral Antifungals for more severe infections. Notes: Avoid Steroids.
answer
...
question
DX: Tinea Profunda: "Majocchi's Granuloma" Symptoms: Dermal infection of dermatophytes. Usually clears temporarily with topical antifungals but readily returns. DX same as for any Tinea (skin scraping), but is best diagnosed with a dermal biopsy. RX: oral antifungals necessary
answer
...
question
Erythrasma Symptoms: Erythematous rash in intertrigenal spaces. Causative agent: Corynebacterium minutissimum. DX: Wood's light will flouresce a coral red color. RX: Topical antibiotics and occassionally topical steroids.
answer
...
question
Impetigo. Two Types: Superficial [most common] & Bullous. Symptoms: honey-colored crusts on denuded skin with an erythematous base. Causative agent: Group A B-hemolytic streptococci and / or Staphylococcus aureus. DX: Diagnosis by clinical evaluation of rash. Bacterial cultures. Biopsy RX: Topical-Mupirocin ointment 2% (Bactroban). Altabax (Retapamulin) Oral- erythromycin. dicloxacillin Notes: Most common skin infection in children
answer
...
question
Candidal Intertrigo Symptoms: Beefy red appearance with satellite lesions peripherally RX: Treatment is with anti-yeast topical preparations, and oral agents in severe cases Notes: Candida organisms are part of the skin's normal flora that can over colonize in certain settings
answer
...
question
Scabies Symptoms: Very Very pruritic, more often at night. Appearance: Causative agent: Infestation of mite Sarcoptes scabeii var. hominis Transmission: direct skin to skin contact. Not every contact results in transmission. DX: highlighter test absorbs in dry mite burrows. Scraping shows mite eggs and feces. Biopsy. Clinical suspicion. Incubation/life cycle: Life cycle last 30 days. Incubation may be up to 14 days. RX: Must treat with two rounds of meds to treat infestation and then eggs! prevent reinfestation- wash everything with both rounds of treatment in HOT water. Permethrin (Acticin or Elimite) antiscabacide 2 treatments, 7-10 days apart. Oral Antihistimines. Topical Steroids. Oral prednisone. Ivermectin (pet heart worm preventative)
answer
...
question
Pediculosis Capitus "lice" Symptoms: intense itch of scalp Causative agent: Peduculus humanus var.capitis Transmission: Highly infectious particularly among people with poor hygiene, and/or with long hair. Secondary infection can occur Diagnosis: Can be seen by naked eye. Clinical demonstration of actual lice, or nits attached to the hair shaft. Nits will not move, are attached to hair shaft. RX: Lindane 1% shampoo for adults. Permethrin 1% cream rinse for adults or children. Cutting of the hair or shaving the scalp also helpful though not always practical
answer
...
question
Herpes labialis: "cold sore/ feer blister" Symptoms: prodrome of tingling, burning, itching, pain or numbness secondary to nerve damage. Vessicles on lips appear as long as 24-48hrs after prodrome. Initial infection usually is the worst outbreak. Sores develop as blisters that erode, crust, and heal spontaneously over 7-10 days Causative agent: Herpes simplex virus type 1 primarily but can be caused by type II. Transmission: direct moist skin contact. DX: clinical appearance and history. Tzanck smear to evaluate for Giant cells Tissue culture. RX: Topical--Denavir ointment. Acyclovir ointment. Oral-- Acyclovir 400-800mg 3-5 times a day for 3-7 days. Valtrex 500mg TID for 3-5 days or 2g BID (can be used as abortive therapy with prodrome 2g 12hrs apart). Famvir 500mg TID for 3-5 days.
answer
...
question
Herpes Progenitalis: "Genital herpes" The second most common sexually transmitted disease in the USA Symptoms: prodrome of tingling, burning, itching, pain or numbness secondary to nerve damage. Vessicles on lips appear as long as 24-48hrs after prodrome. Initial infection usually is the worst outbreak. Sores develop as blisters that erode, crust, and heal spontaneously over 7-10 days Causative agent: herpes simplex virus Type II, but can also be caused by Type I depending upon source of inoculation. RX: Topical--Denavir ointment. Acyclovir ointment. Oral-- Acyclovir 400-800mg 3-5 times a day for 3-7 days. Valtrex 500mg TID for 3-5 days or 2g BID (can be used as abortive therapy with prodrome 2g 12hrs apart). Famvir 500mg TID for 3-5 days.
answer
...
question
Herpes Simplex Symptoms: Herpetic vessicles in an extragenital or an extraoral site of skin infection. Herpetic Whitlow - infection at or around the cuticle of the finger, painful, highly transmissable Causative agent: Can be caused by either Type I or Type II.
answer
...
question
Varicella Causative agent: Varicella Zoster Virus (VZV) Symptoms: Prodrome of flu-like symptoms occur. Pruritic rash. "dew drop on a rose petal" Erythematous wheal like base with a small vesicle overlying in an off-center location. Rash usually begins 2-5 days after prodrome of flu-like symptoms occur Transmission: Highly contagious by airborne means. Persons are infectious 2 days before the onset of symptoms and up to 5 days after development of rash. RX: Antivirals--Valtrex, Famvir, Acyclovir. Antiinflammatory drugs. Antibiotics for secondary infection. Oatmeal baths. No treatment is necessary for mild infection NOTES: Pregnant women before 28 weeks gestation should not come into contact with contagious persons, if not previously exposed due to the risk of birth defects. Varicella vaccine is often given in two doses 5 years apart. Has been available since 1995.
answer
...
question
Syphilis- Known as the great imitator Causative agent: Treponema pallidum. The disease is divided into four stages: Primary. Secondary. Latent. Tertiary (late). Transmission: The bacterium can pass through broken skin on parts of the body. Sexual contact. Pregnant women can pass the bacterium to the fetus, which can result in serious mental and physical problems. DX: RPR (rapid plasma reagin) test. VDRL (Venereal Disease Research Laboratory) test. Primary diagnosis is best. A surface scraping from the chancre is taken and examined under a darkfield microscope to detect the organism itself. RX: Penicillin, usually by injection. Repeated blood tests are necessary for at least a year after treatment to monitor possible treatment failure
answer
...
question
Primary syphilis Symptoms: Primary Syphilis Chancre appears within 10 days to 3 months after exposure, but usually within 2-6 weeks. PAINLESS. Usually disappear within a few weeks whether treated or not.
answer
...
question
Secondary syphilis. Symptoms: Rash of flat, red lesions over the whole body (including the palms and soles ). fever. swollen glands. broad-based papules (lumps or warts) in warm, moist sites mucous patches or snail-track ulcers in the mouth, appearing from 3-6 weeks after the chancre develops
answer
...
question
Gonorrhea Symptoms: Creamy or green, pus-like discharge from the penis or vagina. Painful urination. Testicular pain. Painful intercourse. Excessive bleeding during menstrual period or break through bleeding. Can affect mouth/throat/eyes. Causative agent: Neisseria gonorrhoeae. DX: Gram stain of discharge demonstrates organisms. Culture of discharge. Transmission: Spread through sexual contact. Transmitted from mother to fetus causing eye infections. RX: Cefixime. Ceftriaxone. Ciprofloxacin*. Ofloxacin*. Tetracycline. *not during pregnancy
answer
...
question
Condyloma Symptoms: Wart like lesions. Can occur on the genitals, anal region or oral areas of the body. Causative agent: HPV RX: Cryosurgery. Surgical Excision. Laser therapy. Topical Acid Therapy. Imiquimod (Aldara, Zyclara). Veregen. Condylox. Interferon. Candida Antigen Injections. Notes: Certain types have oncogenic potential 16, 18, 31, 33, 35, 45, 52 and 58. Gardisil vaccination protectes uninected people against types 6,11,16 and 18. Used for girls 10-25yo and boys 9-15yo. 6.2 million individuals are infected with genital HPV in the US each year. The most common sexually transmitted disease in the United States
answer
...
question
Psoriasis Different Types: Chronic Plaque Psoriasis. Guttate Psoriasis. Pustular Psoriasis--Palmoplantar pustular (Barber's) & Generalized pustular (von Zumbusch). DX: Family /personal history. Clinical examination. Auspitz sign - Punctate bleeding at site of lifted scale. Koebner phenomenon. Biopsy RX: TOPICAL- Dovonex. Vectical. Tazorac. Steroids. Taclonex. Protopic. Emollients/Occlusion. Tar/Anthralin. ORAL- Methotrexate. Cyclosporine (Neoral). Acitretin (Soriatane). Biologic therapy- Amevive (alefacept).Enbrel (etanercept). Remicade. Humira. ULTRAVIOLET THERAPY- UVB with or without tar topicals. UVA with or without Psoralens. ALTERNATIVES- Intralesional injections of Steroids. Petroleum jelly and Saran wrap. Laser. Intense Pulsed Light (IPL). DRUGS THAT EXACERBATE PSORIASIS-Lithium, Beta Blockers, Antimalarials, Systemic steroids. Notes: Affects 1-3% of the population worldwide. Genetically transmitted. Men and women affected equally. Can be associated with generalized Arthritis. Differential diagnosis: Fungal Infections. Pityriasis Rosea. Cutaneous Lupus. Erythematosus. Drug Eruptions

answer
...
question
Psoriasis vulgaris: "chronic plaque psoriasis" Most common form of psoriasis. Symptoms: Begins as red scaly papules that coalesce to form plaques. Can occur anywhere on the body. Can be congenital.
answer
...
question
Palmoplantar Psoriasis: "Barber's or localized pustular psoriasis" Symptoms: Palms and soles have sterile pustules. Chronic plaque psoriasis can occur elsewhere on the body or not at all. Nail changes are common.
answer
...
question
Guttate Psoriasis Symptoms: Occurs after Streptococcal infection or upper respiratory infection Notes: May be an indication that individual has genetic tendancy towards Chronic Plaque Psoriasis. 30% of Psoriasis patients
answer
...
question
Pustular Psoriasis Generalized: "psoriasis von Zumbusch" Note: Rare. Dermatology emergency due to sluffing off of skin causing dehydration and risk of secondary infection. Patients often require hospitalization Symptoms: Patients also demonstrate constitutional symptoms including fever
answer
...
question
Koebner Phenomenon
answer
Also known as the Isomorphic phenomenon Capacity to reproduce skin lesions at site of local injury: Scratches, Burns, Rubbing, Cutting Occurs in : Psoriasis Lichen planus Flatwarts (verruca plana
question
Types of skin lesions seen in Sarcoidosis.
answer
Lupus pernio Erythema nodosum Scar sarcoid Papules Plaques



