Flashcards About Test on Dermatology
Unlock all answers in this set
Unlock answersquestion
Seborrheic Dermatitis (dandruff)

answer
1. Affects 3-5% of population 2. Caused by Malassezia furfur 3. Common associations -Parkinsons disease -AIDs and AIDs related complex 4. scaly, yellowish, greasy dermatitis 5 Locations -Scalp (dandruff), eyebrows, nasal creases -called cradle cap in newborns
question
Seborrheic Dermatitis Therapy
answer
Shampoo-selenium sulfide, zinc pyrithione; may need higher prescription doses of these over the counter shampoos the mainstay of treatment includes topical anti-fungal agents alone or in combination with topical steroids.
question
Pityriasis Rosea

answer
1. Initially presents as a single, large, oval, scaly, rose colored plaque on the trunk -called the herald patch -frequently misdiagnosed as ringworm 2. days or weeks later, a papular eruption develops on the trunk -rash follows the lines of cleavage (xmas tree distribution) -lesions tend to be pruritic -rash remits spontaneously in 2-10 weeks
question
Pityriasis Rosea Therapy
answer
Antihistamines control pruritis; UV light therapy hastens resolution Viral exanthems are usually asymptomatic and self-limited, and therapy usually is not required
question
Psoriasis

answer
1. Epidemiology -afflicts 1-3% of the world population -strong human leukocyte antigen (HLA) relationship -Peak age at onset is bimodal --adolescents and 60 years of age -no gender difference 2. Pathogenesis -Unregulated proliferation of keratinocytes --genetic factors involved in 30% of cases --aggravating factors ---Streptococcal pharyngitis ---HIV (sudden onset of Psoriasis is high suspicious of HIV) ---Drugs (lithium, Beta blockers, NSAIDs) ---scratching the skin -Microcirculatory changes in superficial papillary dermis 3. Well demarcated, flat, elevated salmon colored plaques -covered by adherent white to silver colored scales --pinpoint areas of bleeding occur when scales are scraped off --rash commonly develops in areas of trauma (elbows, lower back) called Koebners phenomenon 4. pitting of the nails 5. Microscopic findings -hyperkeratosis and parakeratosis -Elongation of rete pegs --downward extension of basal layer -Extension of the papillary dermis close to the surface epithelium --blood vessels in dermis rupture when scales are picked off (Auspitz sign) -Neutrophil collections in the stratum corneum --Called Munro micro abscesses Approximately 5 percent of patients with psoriasis develop an arthritis that, although it bears similarities to rheumatoid arthritis, seems to be different from it.
question
Psoriasis Treatment modalities
answer
Initial treatment of psoriasis is followed by long-term maintenance therapy. Greater than 10% body surface area, or severe involvement of the scalp, hands, or feet, may require phototherapy, systemic immunosuppressive (corticosteroids) or retinoid therapies. Systemic treatment Methotrexate, cyclosporin can lead to initial improvement of psoriasis with a rebound worsening upon steroid taper, and should be avoided.
question
Lichen simplex chronicus

answer
Lichen simplex chronicus is a response to persistent, vigorous rubbing, and results entirely from rubbing what at first was normal skin. Clinically, lichen simplex chronicus is a hyperpigmented keratotic plaque whose surface shows accentuation of normal skin markings. It is found always within easy reach of the hands, which are skilled at rubbing and at using an adjunctive object (such as a hairbrush or a towel) to do the job.
question
Lichen simplex chronicus therapy
answer
for lesions that are extragenital, use super or ultrapotent topical corticosteroids
question
Atopic Dermatitis (Eczema)

answer
1. Type I IgE-mediated hypersensitivity reaction 2. Dermatitis in children -dry skin and eczema on cheeks and extensor and flexural surfaces 3. Dermatitis in adults -dry skin and eczema on hands, eyelids, elbows, and knees A condition of persons of any age, but particularly children with a genetic proclivity for allergic rhinitis and conjunctivitis, and allergic asthma. Intense pruritus induces patients to rub the skin intensely and to scratch furiously, the resultant factitious lesions being erythematous, often scaly, macules, patches, papules, and plaques that tend to become lichenified, eroded, ulcerated, and crusted.
question
Atopic Dermatitis (Eczema) therapy
answer
There are two likely-related pathophysiologic mechanisms underlying the disease: skin inflammation and impaired skin barrier. Both must be targeted by effective therapy. 1. Avoid rugs, irritants that produce a rash 2. Apply moistening agents (emollients) to the skin 3. Topical corticosteroids -low potency for the face -medium to high potency for other sites
question
Dyshidrosis (hand eczema)

answer
A pruritic papular and vesicular inflammatory process of unknown cause that tends to affect the sides of fingers and toes, as well as palms and soles. The name "dyshidrotic" is misleading; the condition has no relation whatever to eccrine glands or to sweating.
question
Dyshidrosis (hand eczema) therapy
answer
Hand dermatitis may be difficult to treat due to the thickened skin surface of the hands and the frequent exposure of the hands to irritants and potentially exacerbating factors. The therapeutic strategy is to eliminate any external cause and to control the cutaneous inflammation. Management is typically through topically applied medications. For severe cases, systemic immunosuppression may be necessary. All patients with hand dermatitis, independent of the clinical type, have reduced tolerance to irritants. Avoidance of irritants, including wetness, and frequent use of moisturizers are important.
question
Vitiligo

answer
1. Common in blacks 2. Automimmune destruction of melanocytes -causes localized to extensive areas of skin depigmentation and whitening of hair that follows loss of melanocytes from the bulb of follicles. -In contradistinctinction, albinism is due to deficiency of tyrosinase leadong to absebce of melanin in melanocytes 3. Often associated with other autoimmune conditions -Hashimoto's thyroiditis, hypoparathyroidism and in whitening of hair that follows loss of melanocytes from the bulb of follicles.
question
Vitiligo therapy
answer
The duration of vitiligo is lifelong and its disease course may be difficult to predict. The mainstay of treatment includes topical corticosteroid and calcineurin therapies and narrow-band ultraviolet phototherapy; combined therapy may be most effective.
question
Melasma

answer
1. Macular, hyperpigmented lesions on the forehead and cheeks, vertically and horizontally, distributed symmetrically -very common 2. Female predominance; exacerbated )melanocytes produce more melanin) by: -Oral Contraceptives -Pregnancy -Sunlight 3. Although the pigmentation usually fades after pregnancy or withdrawal of OCPs, it may persist indefinitely.
question
Melasma therapy
answer
Treatment of melasma involves topical drugs, superficial procedures (such as chemical peels), and photoprotection. First-line treatment is a triple combination topical therapy, including hydroquinone (bleaching agent) to skin, retinoid cream, and corticosteroids.
question
Seborrhea keratosis

answer
1. Epidemiology -Most common benign tumor in old people (>50 years of age) 2. Benign pigmented epidermal tumor -coin like, macular to raised verrucoid lesion with stuck on appearance -extremities and shoulders most common sites -occur commonly on the face of elderly pts 3. Leser-Trelat sign -raid increase in number of keratoses -phenotypic marker for stomach adenocarcinoma
question
Seborrhea keratosis therapy
answer
Curettage, cryotherapy, and laser surgery are all efficacious.
question
Tinea Corporis (body ringworm)

answer
1. Sometimes called ringworm 2. May have history of exposure to cat or dog 3. One or more lesions may be present 4. Typically are annular with an elevated red, scaly border -tendency for central clearing In all cases, Trichophyton rubrum is a common cause. Diagnosis can easily be made by identifying fungal hyphae in a KOH preparation of a superficial scraping of affected skin.
question
Tinea Corporis (body ringworm) treatment
answer
Topical antifungals: clotrimazole, miconazole, are first-line therapy. -Can use oral terbinafine as an alternative
question
Tinea Cruris (Jock Itch)

answer
1. Frequently also have tinea pedis infection of feet or toenails 2. Both are areas for excessive sweating 3. Rash in not annular but has elevated, scaly borders 4. Scrotum is involved In all cases, Trichophyton rubrum is a common cause. Diagnosis can easily be made by identifying fungal hyphae in a KOH preparation of a superficial scraping of affected skin.
question
Tinea Cruris (Jock Itch) treatment
answer
Topical antifungals: clotrimazole, miconazole, are first-line therapy. -Can use oral terbinafine as an alternative
question
Tinea Manuum & Tinea Pedis

answer
1. Most common site of infection 2. most common in patients with sweaty feet 3. Macerated scaling rash between the toes 4. Elderly people have diffuse plantar scaling -moccasin appearance Most often presenting with asymptomatic scaling. May progress to fissuring in toe web spaces. Common cofactor in lower leg cellulitis. Itching, burning, and stinging of interdigital web, scaling palms, and soles. In all cases, Trichophyton rubrum is a common cause. Diagnosis can easily be made by identifying fungal hyphae in a KOH preparation of a superficial scraping of affected skin.
question
Tinea Manuum & Tinea Pedis (Athletes foot) treatment
answer
Topical antifungals: clotrimazole, miconazole, are first-line therapy. -Can use oral terbinafine as an alternative
question
Tinea Versicolor (Pityriasis Versicolor)

answer
Tinea versicolor is Tinea with alteration of skin pigmentation. Woods lamp accentuates the color variation in the skin. Caused by Malassezia furfur -In hypo-pigmented type, fungus-derived acids inhibit tyrosinase in melanocytes from synthesizing melanin (decrease in melanin synthesis.). -In hyper-pigmented type, fungus induces enlargement of melanosomes in melanocytes along the basal cell layer (enlargement of melanosomes). Affected skin does not tan (white spots); normal skin does. -Lesions become hyperpigmented and scaley in the winter months KOH findings -Hypo and Hyper-pigmented areas have the organism. -Short hyphae have the appearance of spaghetti -Yeasts have the appearance of meatballs.
question
Tinea Versicolor (Pityriasis Versicolor) treatment
answer
Best Treatment is oral ketoconazole. Topical Selenium sulfide shampoo (2%) is the most economical therapy.
question
discoid lupus erythematosus

answer
Localized red plaques, usually on the face Scaling, follicular plugging, atrophy, dyspigmentation, and telangiectasia of involved areas. Itching weakness, malaise, fever, and weight loss. redness and scaling is widespread. histology distinctive. Photosensitive. It may be impossible to identify the cause of exfoliating erythroderma early in the course of the disease
question
discoid lupus erythematosus therapy
answer
topical therapy includes cool to tepid baths and application of mid potency corticosteroids under wet dressings.
question
Mycosis fungoides (Cutaneous T Cell Lymphoma)

answer
Localized or generalized erythematous scaling patches and plaques. Involves neoplastic peripheral CD4 T helper cells. Usually involves adults 40-60 years of age. 1. Begins in the skin (rash to plaque to nodular masses) -progresses to lymph nodes, ling, liver, and spleen 2. Groups of neoplastic cells in the epidermis are called Pautrier's microabcesses.
question
Mycosis fungoides (Cutaneous T Cell Lymphoma) Therapy
answer
Therapy of cutaneous T-cell lymphoma often requires specialized knowledge, and for this reason it is often appropriate to refer such patients to a medical center with specialized knowledge in the management of CTCL.
question
Actinic Keratosis (solar)

answer
1. associated with prolonged UV light exposure 2. Precursor (squamous dysplasia) of squamous cell carcinoma. -Squamous cancer occurs in 2-5% of cases 3. Hyperkeratotic, pearly gray white appearance -occurs on face, back of neck, dorsum of hands/forearms -commonly recurs when scraped off
question
Actinic Keratosis (solar) treatment
answer
1. protection of skin with sunscreen 2. Topical Therapy - 5-fluorouracil 3. Cryotherapy
question
Bowen Disease
answer
1. Leukoplakia involving the shaft of the penis and scrotum -patients usually > 35 years old -associated with human papillomavirus (HPV) type 16 2. Precursor for invasive squamous cell carcinoma (10% of cases) 3. Association with other types of visceral cancer
question
Exatramammary Paget's disease
answer
Red, crusted vulvar lesion Intraepithelial adenocarcnioma -tumor derives from primitive epithelial progenitor cells -Malignant Paget's cells contain Mucin --Mucin is periodic acid-Schiff (PAS) positive -spreads along the epithelium --rarely invades the dermis
question
Intertrigo
answer
1. Infection caused by Candida albicans 2. Erythmatous rash in body folds -KOH shows pseudohyphae and yeast 3. Examples -rash under pendulous breast, diaper rash
question
Intertrigo treatment
answer
Topical antifungals: clotrimazole, miconazole, are first-line therapy.
question
Erythrasma
answer
skin disease that causes brown, scaly skin patches in the intertriginous areas (skin fold areas - e.g. armpit, groin, under breast). caused by the Gram-positive bacterium Corynebacterium minutissimum prevalent among diabetics and the obese The patches of erythrasma are initially pink, but progress quickly to become brown and scaly (as skin starts to shed), which are classically sharply demarcated
question
Erythrasma Treatment
answer
Erythrasma is treated with topical fusidic acid, or systemic macrolides(erythromycin or azithromycin).
question
Herpes Simplex

answer
virus remains latent in sensory ganglia recurrent vesicles that ulcerate Tzanck preparation: scraping removed from the base of an ulcer; see multinucleate squamous cells with eosinophilic intranuclear inclusions(A nonliving mass, such as a droplet of fat, in the cytoplasm of a cell)
question
Herpes Simplex Treatment
answer
acyclovir (decreases recurrences)
question
Herpes Zoster (Chickenpox, shingles)

answer
1. Chickenpox -all stages of development are simultaneously present -pt is infectious 1 week before the rash appears until 4-5 days after the vesicles become crusted 2. Shingles -occurs in 10-20% of people, incidence increases with age and in pts with cancer and AIDs -prodrome of radicular pain and itching before rash occurs -eruption characterized by groups of vesicles on an erythematous base --rash follows sensory dermatomes --like varicella, pustules form that rupture, causing crusting and weeping
question
Herpes Zoster (Chickenpox, shingles) treatment
answer
1. prevention with previous immunization for varicella 2. prevention with zoster vaccine (reduces infection rate by 50%) 3. Analgesics commensurate with amount of pain 4. Immunocompromised pts are often treated with acyclovir before the rash has erupted
question
Rubeola (Measles)
answer
1. RNA paramyxovirus 2. Prodrome includes fever, cough, runny nose, conjunctivitis 3. Koplik spots (white spots overlying an erythmatous base) develop on the buccal mucosa 4. Maculopapular rash develops afer the Kopli spots disappear -Cytotoxic T cell damage of endothelial cells containing the virus -Typically begins in the head and then to the trunk and extremities -Tends to become confluent on face and trunk but discrete on extremities 5. Complications -Giant cell pneumonia -Acute appendicitis in children -Otitis media -Encephalitis, used to cause death before immunization -not teratogenic
question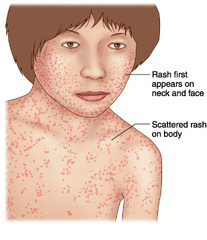
Rubella (German measles or three-day measles)
answer
1. RNA toga virus(caused by the rubella virus) -produces 3 day measles 2. Forchheimer's spots -Dusky red spots that develop on posterior soft/hard palate -Develop at the beginning of the rash 3. Maculopapular rash lasts 3 days -Pinkish, red maculopapular eruption -begins at the hairline and rapidly spreads cephalocaudally -Unlike Rubeola, the macules and papules are discrete and do not become confluent -fades in 3 days 4. Vaccination has reduced incidence of Rubella
question
Erythema infectiosum

answer
1. Caused by Parvovirus B19 (DNA virus) 2. Most often occurs in school age children -often occurs in epidemics 3. Confluent net-like erythema type of rash -begins in the cheeks (slapped cheek appearance) -extends to the trunk and proximal extremities 4. Polyarthritis common in adults
question
Scarlet fever

answer
1. Caused by Streptococcus pyogenes that produce an erythrogenic toxin 2. patients are febrile and have a sore throat due to streptococcal pharyngitis 3. An erythematous rash develops that involves the skin and tongue -it initially occurs on the face and neck before spreading to toher parts of the body -it spares the mouth by producing conspicuous pallor -It has a sandpapery feeling -the tongue is covered by a white exudate studded with prominent red papillae -The rash begins to fade after 6 days and desquamonation (peeling) begins, which may last up to 10 days -the white exudate on the tongue disappears; tongue is beefy red, hence the term "strawberry tongue" 4. Increased risk for developing post streptococcal glomerulonenephritis
question
Scarlet fever treatment
answer
penicillin V
question
Rocky Mountain spotted fever

answer
1. caused by exposure to tick bite in an endemic area 2. An influenza-like prodrome followed by chills, fever, severe headache, and myalgias; occasionally delirium and coma 3. Red macular rash appears between the 2nd and 6th days of the fever, first on the wrists and ankles and then spreading centrally; it may become petechial. 4. Serial serological examinations by indirect fluorescent antibody confirm the diagnosis retrospectively.
question
Rocky Mountain spotted fever treatment
answer
Empiric treatment with doxycycline for 3 days is recommended
question
Syphilis

answer
An inflammatory process, caused by the spirochete Treponema pallidum. evolve through three stages 1. primary (typified usually by a solitary chancre) 2. secondary (characterized by widespread macules and papules on skin and mucous membranes in conjunction with signs and symptoms of systemic disease) 3. tertiary (manifested by gummas in the skin and destructive lesions also in the bones, eyes, brain, and elsewhere, resulting in debilitation and often death).
question
Syphilis treatment
answer
The treatment of syphilis is based on the duration of infection and the organ systems involved. Five groups can be distinguished: primary, secondary, or early syphilis of less than 1 year's duration
question
Porphyria cutanea tarda (PCT)

answer
1. Genetic or acquired disease disease involving porphyrin metabolism. 2. Deficiency of uroporphyrinogen decarboxylase -urine is wine-red color on voiding -Uroporphyrin I is increased in urine 3. Precipitating factors -Hepatitis C -Excessive alcohol intake -Oral contraceptive pills (OCPs) -Iron 4. Clinical findings -Photosensitive bullous skin lesions --Caused by porphyrin metabolites deposited on the skin --patients avoid light -Hyperpigmentation, fragile skin, hypertrichosis
question
Porphyria cutanea tarda (PCT) treament
answer
1. avoid alcohol, OCPs 2, Phlebotomy (decrease iron) 3. Chloroquine
question
Impetigo

answer
1. Most often caused by Staphylococcus aureus -Streptococcus pyogenes second most common cause 2. Rash usually begins at the face -Vesicles and pustules rupture to form honey colored, crusted lesions 3. Bullae commonly occur
question
Impetigo Treatment
answer
Mupirocin ointment + dicloxacillin
question
Allergic contact dermatitis

answer
1. Type IV hypersensitivity reaction 2. Poisen Ivy, nickel in jewelry
question
Allergic contact dermatitis treatment
answer
1. Avoid irritants, drugs that produce a rash 2. apply moistening agents (emollients) to skin 3. Topical corticosteroids
question
Urticaria (hives)

answer
1. Pruritic elevations of the skin . Eruptions of evanescent wheals or hives. May or may not itch. -most often due to mast cell release of histamine -Type I IgE-mediated reactions associated with certain exposure, allergens: ---Certain foods (peanuts) ---Insect bites (fire ants) ---Drugs (Penicillin, morphine, aspirin, laxative) ---Emotional stress ---Hepatitis B (part of the serum sickness prodrome) ----this is a type III hypersensitivity reaction 2. Dermatographism -occurs in the upper dermis -Urticaria develops in areas of mechanical pressure on the skin (you can scratch things into a pts skin)
question
Urticaria treatment
answer
Most incidents are acute and self limited over a period of 1-2 weeks 1. Discontinue the offending drug 2. Avoid aspirin and other NSAIDs 3. Antihistamines 4. Tricyclic drugs (e.g. doxepin) 5. Systemic steroids
question
Angioedema

answer
the rapid swelling (edema) of the dermis, subcutaneous tissue, mucosa and submucosal tissues. It is very similar to urticaria.
question
Angioedema treatment
answer
Cases where angioedema progresses rapidly should be treated as a medical emergency, as airway obstruction and suffocation can occur. Epinephrine may be life-saving when the cause of angioedema is allergic
question
Acne Vulgaris

answer
1. Chronic inflammation of the pilosebaceous unit 2. Most common disease seen by dermatologist 3.Begins at an early age (9-11) 4. Increases in severity in teen years 5. Clinical lesions -inflammatory papules, pustules, nodules, cysts 6. Non inflamed comedomes -Plugging of the outlet of a hair follicle by keratin debris -Open comedone is called a blackhead -Closed come dome is called a whitehead 7. Inflammatory type -abnormal keratinization of the follicular epithelium -Increased sebum production (androgen dependent) -Bacterial lipase )Propionibacterium acnes) produces irritating fatty acids --produces the inflammatory reaction
question
Acne Vulgaris treatment
answer
1. topical agents -topical retinoid + benzoyl peroxide 2. Systemic antibiotics -tetracycline (first choice) 3. Systemic retinoids -isotretinoin (decreases follicular keratinization, sebum production, bacterial count) 4. Hormonal therapy -oral contraceptives (women; reduce testosterone levels); anti androgens
question
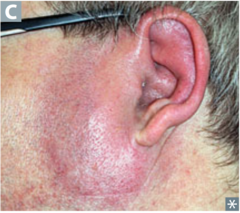
Acne rosacea (Rosacea)

answer
The term "acne rosacea" is a synonym for rosacea, however some individuals may have almost no acne comedones associated with their rosacea 1. Inflammatory reaction of the pilosebaceous untis of facial skin -casual relationship with a mite (Demodex folliculorum) 2. Pustules and flushing of the cheeks -Exacerbated by drinking alcohol, stress, or eating spicy foods 3. Sebacceous gland hyperplasia -Produces enlargement of the nose (rhinophyma)
question
Acne rosacea treatment
answer
1. topical metronidazole gel 2. Systemic treatment -Isotretinoin -Tetracycline
question
Folliculitis

answer
itching and burning in hairy areas pustules in the hair follicles • Important causes of folliculitis include infection (bacterial, yeast, and viral), friction, medication-induced, or folliculitis associated with pregnancy. • Because Staphylococcus aureus is a common cause of folliculitis, a bacterial culture is always indicated to determine whether methicillin-resistant Staphylococus aureus (MRSA) is present, as this determines appropriate antibiotic treatment.
question
Folliculitis Treatment
answer
Anhydrous ethyl alcohol contain 6.25% aluminum chloride (Xerac AC), applied to lesions and environs, may be helpful, especially for chronic folliculitis of the button. Topical antibiotics are generally ineffective if bacteria have invaded the hair follicle
question
Faruncle (Boil)

answer
A shiny, ill-defined, erythematous nodule with pallor in the center, a deep folliculitis, infection of the hair follicle. It is most commonly caused by infection by the bacterium Staphylococcus aureus, resulting in a painful swollen area on the skin caused by an accumulation of pus and dead tissue
question
Faruncle (Boil) Treatment
answer
A small boil may burst and drain on its own without any assistance.[12] In some instances, however, draining can be encouraged by application of a cloth soaked in warm salt water (warm compresses). Washing and covering the furuncle with antibiotic cream or antiseptic tea tree oil[13] and a bandage also promotes healing.
question
Carbuncle

answer
Individual Faruncles clustered together
question
Carbuncle treatment
answer
Oral antibiotics against the gram positive bacteria is recommended when the boil is larger than 5 cm diameter, or 2 cm proud (tall), or very painful, or appearing to (or actually is) spread to new sites, or entered below the skin into underlying structure, such as causing a painful muscle, bone, ligament or joint, or if the lymph nodes are inflamed. Oral antibiotics will treat the carbuncle and antibiotics should be continued until the carbuncle has healed over.
question
Candidiasis

answer
An inflammatory disease caused by the yeast Candida albicans and manifested clinically as erythematous papules and pustules that may become confluent to form plaques in the case of the former and erosions in the case of the latter. The nail unit may be affected by paronychia and the oral cavity by "thrush." Seen in the diaper region, in between fingers, on the nail, tongue, genitals, mouth
question
Candidiasis treatment
answer
Candidiasis is commonly treated with antimycotics; these antifungal drugs include topical clotrimazole, topical nystatin, fluconazole, and topical ketoconazole.
question
Miliaria

answer
The usual symptoms are burning and itching. The lesions occur on covered areas of the skin, usually the trunk. More common in hot, moist climates. They consist of small, superficial, red, thin-walled, discrete vesicles (miliaria crystallina), papules (miliaria rubra), or vesicopustules or pustules (miliaria pustulosa). The reaction virtually always affects the back in a hospitalized patient.
question
Miliaria Treatment
answer
The patient should keep cool and wear light clothing. Triamcinolone acetonide in Sarna lotion, or a mid-potency corticosteroid in a lotion or cream.
question
Erythema migrans (sign for Lymes disease)

answer
1. Epidemiology -Transmitted by tick bite -Borrelia burgdorferi (spirochete) 2. early disease --Erythema chronicum migrans develops at tick bite site --Pathognomonic, red, expanding lesion with concentric circles (bulls eye lesions) 3. Late disease --Disabling arthritis --Bilateral Bells palsy (highly indicitive of Lymes Disease) --Myocarditis and Pericarditis 4. Diagnosis -ELISA testing as screen -If ELISA positive, use Western blot assay to confirm
question
Erythema migrans (sign for Lymes disease) treatment
answer
Adults-doxycycline, amoxicillin, erythromycin, or ceftriaxone Children-amoxicillin
question
Erythema multiforme

answer
1. Type IV immunologic hypersensititvyt reaction of skin that is triggered by: -infection: Mycoplasma pneumoniae, herpes simplex vius -Drugs: Sulfonamides, penicillin, barbituates, phenytoin 2. Vesicles and bullae have a "targetoid" appearance -located on the palms, soles, and extensor surfaces
question
Erythema multiforme treatment(s)
answer
-treat with systemic corticosteroids -treat triggering infection -discontinue drug
question
Erythema nodosum

answer
1. inflammatory lesion of subcutaneous fat 2. More common in women than men 3. Raised erythematous, painful nodules -ususally located on the anterior portion of the shins 4. Common associations -Tuberculosis -Leprosy -Streptococcal pharyngitis -Yersinia enterocolitis -Sarcoidosis -Ulcerative Colitis -Pregnancy, OCP
question
Erythema nodosum treatment
answer
1. Identify and treat precipiating causes 2. NSAIDs 3. Systemic corticosteroids if severe
question
Cellulitis

answer
infections of the dermis and subcutaneous layers of the skin that are rapidly progressive and are often accompanied by systemic signs, such as fever, leukocytosis, and elevated markers of systemic inflammation. Cellulitis commonly affects the lower extremities, typically affects one limb, and may result from an underlying abscess or trauma. Trauma, surgery, preexisting skin disease, and chronic lymphedema may be risk factors for cellulitis. There is an important non-infectious differential diagnosis of cellulitis, including contact dermatitis, venous stasis dermatitis, deep vein thrombosis, and vasculitis. Venous stasis dermatitis is commonly bilateral, and is not accompanied by signs of systemic inflammation. Most cases of cellulitis are caused by streptococci. Staphylococcus aureus is an important consideration in cases of cellulitis associated with trauma or an underlying abscess.
question
Cellulitis treatment
answer
requires systemic antibiotic therapy.
question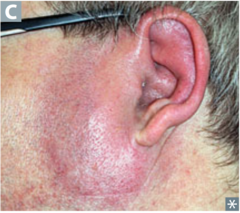
Erysipelas
answer
infections of the dermis and subcutaneous layers of the skin that are rapidly progressive and are often accompanied by systemic signs, such as fever, leukocytosis, and elevated markers of systemic inflammation. Erysipelas affects the lower extremities (76% of cases) but commonly has facial involvement (17%), is sharply demarcated, typically involves more superficial lymphatics within the dermis to give a waxy or intensely superficial edematous appearance.
question
Erysipelas treatment
answer
requires systemic antibiotic therapy.
question
Pemphigus vulgaris (PV)
answer
1. IgG antibodies against intercellular attachment sites (desmosomes) between keratinocytes -type II hypersensitivity rxn 2. Vesicles and bullae develop on skin and oral mucosa 3. Intraepithelial vesicles are located above the basal layer -Basal cells resemble a row of tombstones -Acantholysis of keratinocytes in the vesicle fluid -Positive Nikolsky sign --outer epidermis seperates from the basal layer with minimal pressure
question
Pemphigus vulgaris (PV) treatment
answer
Corticosteroids and other immunosuppressive agents
question
Verruca Vulgaris (Wart)

answer
1. Caused by HPV 2. Common sites are fingers and soles 3. Verrucus papular lesions covered by scales
question
Verruca Vulgaris (Wart) treatment
answer
Physical therapy-cryotherapy with liquid nitrogen Chemotherapy-salicylic acid
question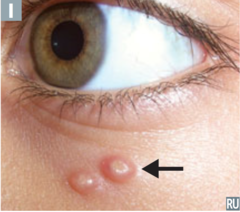
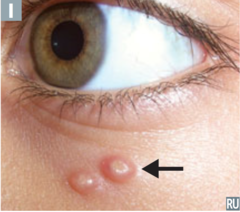
Molluscum contagiosum
answer
1. Caused by a poxvirus (DNA virus) 2. Bowl shaped lesions with central depression filled with keratin -depression contains viral particles called molluscum bodies 3. transmission -can be sexually transmitted in adults (common in AIDS) -Self inoculation by scratching ith infective viral particles out of the crater
question
Molluscum contagiosum treatment
answer
-spontaneous remission occurs in 6 to 9 months if immunocompetent --cell mediated immunity -Cryotherapy
question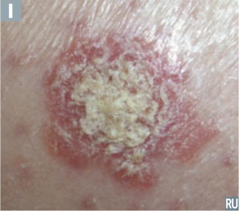
Squamous-cell carcinoma
answer
1. Risk Factors -Excessive exposure to ultraviolet light (most common) -Actinic (solar) keratosis -Arsenic exposure -Scar tissue in a 3rd degree burn -Orifice of chronically draining sinus tract -Immunosuppressive therapy 2. Scaley to nodular lesions -nodules are often ulcerated -majority occur in sun exposed parts of the body --ears, lower lip (most common), dorsum of hands 3. usually well differentiated -minimal risk for metastasis
question
Squamous-cell carcinoma treatment
answer
1. Varies with location and size of the cancer 2. Options include topical 5-fluorouracil, cryotherapy, curettage, and electrodesiccation, surgical excision, radiation (usually in elderly)
question
Basal Cell Carcinoma

answer
1. Caused by chronic exposure to ultraviolet light 2. Raised papule or nodule with a central crater -sides of the crater are surfaced by telangiectatic vessels 3. Occurs in sun exposed areas -inner canthus of the eye, upper lip and higher (most common) 4. Locally aggressive, infiltrating cancer that does not metastasize -Tumor is stromal dependent, hence precluding metastasis -Arises from basal cells infiltrate the underlying dermis 5. Diagnosis -punch biopsy or shave biopsy
question
Basal Cell Carcinoma
answer
1. varies with location and size of the cancer 2. Options include topical 5-fluorouracil, cryotherapy, curettage, and electrodesiccation, surgical excision, radiation (usually in elderly)
question
Melanoma

answer
1. Epidemiology -malignant tumor of melanocytes -most rapidly increasing cancer worldwide --more common in whites than blacks 2. Leading cause of death due to skin cancer 3. Median age of diagnosis is 53 years 4. risk factors -exposure to excessive sunlight (UVA and UVB) at an early age --single most important risk factor -history of family members with melanoma -use of tanning booths -dysplastic nevus syndrome -history of melanoma in first or second degree relative -Xeroderma pigmentosum 5. Radial growth phase -initial phase of invasion -Melanocytes proliferate --laterally within the epidermis --along the dermoepidermal junction --within the papillary dermis 6. Vertical growth phase -Final phase of invasion -malignant cells penetrate the underlying reticular dermis -potential for metastasis 7. Depths of invasion best determines biologic behavior 8. ABCD criteria for malignancy -Assymetry of shape -Border irregularity -Color variation -diameter > 6mm
question
Melanoma prevention and treatment

answer
Prevention: 1. Sunscreen > 15 spf -prevention for UVA and UVB light 2. Protective clothing Treatment: 1. Excision of the entire lesion and surrounding normal tissue -sentinel lymph node biopsy to determine stage 2. More extensive disease -immunotherapy; irradiation
question
Dermatofibroma
answer
1. location: lower extremities 2. Benign, non encapsulated proliferation of spindle cells confined to the dermis 3. Red nodule that umbilicates (has central dimple) when squeezed
question
Dermatofibroma treatment
answer
None, unless a lesion grows to several centimeters in diameter, when simple surgical excision may be indicated.
question
Epidermal inclusion cyst (follicular cysts)

answer
1. Derived from the epidermis of the hair follicle 2. Locations: Face, base of ears, trunk 3. Cyst wall composed of normal epidermis that produces Keratin -Keratin mixed with lipid rich debris 4. Spontaneous inflammation and rupture may occur
question
Epidermal inclusion cyst (follicular cysts) Treament
answer
None required; surgical excision if necessary
question
Acrochordons (Fibroepithelial polyp aka skin tags)

answer
1. Flesh colored soft tag of skin attached to the body by a narrow stalk 2. Common in the elderly 3. Location: Neck, upper chest, armpit, upper back
question
Acrochordons (Fibroepithelial polyp aka skin tags) Treatment
answer
None required, excise if necessary
question
Lichen planus (LP)

answer
1, Intensely pruritic, scaly, violaceous, flat topped papules -fine white reticular pattern on the surface (called Wickham's striae) -Commonly located on wrists, ankles -nails are commonly dystrophic -Lesions develop in areas of scratching (Koebner's phenomenon) 2. Women more commonly affected than men 3. Oral mucosa is often involved (50% of cases) -Produces a fine. white, net-like lesion (wickham's striae) -slight risk of developing squamous cell carcinoma 4. Association with Hepatitis C
question
Lichen planus (LP) Treatment
answer
1. Topical high-potency corticosteroids 2. Anthistamines 3. Systemic corticosteroids 4. Retinoids 5. Cyclosporine in resistant cases
question
Kaposi's sarcoma

answer
Caused by HHV-8 A systemic disease, which manifests itself in the skin first as violaceous macules and patches that tend to progress to papules and plaques, and sometimes to nodules and tumors, all of which represent hyperplasia of endothelial cells.
question
Karposi's sarcoma Treatment
answer
based on the subtype and the presence of localized versus systemic disease. Localized cutaneous disease can be treated with cryotherapy, intralesional injections of vinblastine, alitretinoin gel, radiotherapy, topical immunotherapy (imiquimod), or surgical excision. Extensive cutaneous disease and/or internal disease may require IV chemotherapy and immunotherapy.
question
Scabies

answer
1. Adult females bore into the stratum corneum -Burrows are visible as dark lines between the fingers, at the wrists, on the nipples, on the scrotum -Females lay eggs at the end of the tunnel --eggs are responsble for the intensly pruritic lesion 2. Scabies in Adults -Disease limed to the webs between the fingers, intertriginous ares -Spares the soles, palms, face and head 3. Scabies in infants -No burrows are present -Pruritic rash occurs on the palms, soles, face or head
question
Scabies Treatment
answer
permethrin cream
question
Pediculus humanus capitis (head louse)

answer
1. Pediculus humanis capitis (head louse) -adults lay eggs (nits) on hair shafts -itching of the scalp
question
Pediculus humanus capitis (head louse) Treatment
answer
Permethrin (kills newly hatched lice)
question
Pediculus humanus corporis (body louse)

answer
1. Adults live on the surafce of skin and breed in the clothing 2. Skin lesions are papular and produce intense itching
question
Pediculus humanus corporis (body louse) treatment
answer
3. Treat the clothing, not the pt -treat clothing with malathion or DDT powder or discard clothes
question
Phthirus pubis (pubic louse, crabs)

answer
Adulst live in the pubic hairs -looks like a crab
question
Phthirus pubis (pubic louse, crabs) Treatment
answer
Permethrin (kills newly hatched lice) or malathion
question
Stevens-Johnson syndrome

answer
1. Recently separated from Erythema multiform as a distinct entity 2. Type IV hypersensitivity reaction that primarily involves the skin and mucous membranes (mouth, genitals) -most cases are idiopathic 3. Erosions develop on the mucous membranes and small blisters develop on purpuric or erythmatous macules on the skin (different than target lesions of EM) 4. it can be fatal 5. Padma Lakshmi had it
question
Toxic epidermal necrolysis syndrome (TENS)

answer
1. Idiosyncratic reaction most commonly drug induced (sulfas, NSAIDS, anticonvulants) 2. May occur alone or overlap with Stevens-Johnson syndrome 3. Characterized by extensive areas erythema, necrosis, and bullous detachment of the epidermis and mucous membranes (exfoliation of skin) 4. Mucous membrane involvement can result in gastrointestinal bleeding, respiratory failure, and genitourinary complications 5. It can be fatal 6. Nikolsky's sign is almost always present in toxic epidermal necrolysis
question
Toxic epidermal necrolysis syndrome (TENS) treatment(s)
answer
1. Teat with systemic corticosteroids 2. Treat triggering infection 3. Discontinue drug
question
Bullous pemphigoid

answer
1. IgA-anti-IgA complexes deposit at the tips of the dermal papillae -produces subepidermal vesicles with neutrophils 2. Strongly correlated with celiac disease -increase in antireticulin and endomysial antibodies
question
Bullous pemphigoid treatment
answer
1. Gluten free diet 2. Dapsone or sulfapyridine
question
Photodermatitis

answer
Ultraviolet light reacts with drugs that have a photosensitizing effect (e.g. tetracycline)
question
Venous Insufficiency

answer
STASIS ULCERS result of chronic venous stasis/edema, venous imcompetence, Hx of DVT, vein removal, or varicose veins; stasis dermatitis develops initially and ulcers are wide but not deep with irregular,undulating edges and clean base.
question
Venous Insufficiency treatment
answer
elevation and compression to enhance venous return
question
Arterial Insufficiency

answer
Arterial ulcers are painful, pulses are DIMINISHED OR ABSENT, distal area is cold.
question
Arterial Insufficiency treatment
answer
lifestyle changes (smoking cessation, moderate exercise), debridement if wound is necrotic,wet-to-dry dressings or hydrogels are standard tx because wounds heal better in moist environment, HYDROCOLLOIDS (e.g. DuoDERM) and enzymatic preps
question
diabetic wounds

answer
Due to neuropathy, patients with diabetes have decreased sensation around their feet. As a result, injuries to the superficial layer of skin are not perceived, and progression to ulceration can occur. These patients should be initially evaluated with transcutaneous oxygen pressures and ABIs to determine healing potential. An ABI ratio higher than 0.6 and transcutaneous oxygen measurements greater than 40 mm Hg are usually indicative of adequate vascularity and necessary healing potential
question
diabetic wounds treatment
answer
lifestyle changes (smoking cessation, moderate exercise), debridement if wound is necrotic,wet-to-dry dressings or hydrogels are standard tx because wounds heal better in moist environment, HYDROCOLLOIDS (e.g. DuoDERM) and enzymatic preps
question
Dermatitis medicamentosa
answer
o Etiology: True allergic drug reactions: Amoxicillin, TMP-SMZ, and ampicillin or penicillin are the most common causes of urticarial and maculopapular reactions. o Presentation: Usually, abrupt onset of widespread, symmetric erythematous eruption. May mimic any inflammatory skin condition. A mnemonic for complex eruptions is "DRESS" (DRug Eruption with Eosinophilia and Systemic Symptoms). o Testing: Routinely ordered blood work is of no value in the diagnosis of simple drug eruptions. In complex drug eruptions, the CBC, liver biochemical tests, and renal function tests should be monitored. Skin biopsies may be helpful in making the diagnosis.
question
Dermatitis medicamentosa treatment
answer
• General Measures: Tx systemic manifestations (anemia, icterus, purpura), Antihistamines, Epinephrine for emergency, Systemic corticosteroids for DRESS • Local Measures: SJS/TEN with extensive blistering eruptions resulting in erosions and superficial ulcerations, which demand hospitalization and nursing care as for burn patients, develops in some DRESS patients.
question
Alopecia areata

answer
1. affects both sexes equally 2. Onset most common among young adults 3. Idiopathic 4. Clinical finding -well circumscribed, round to oval patches of hair loss --hair loss may occur on scalp, beard, eyebrows, eyelashes -hairs may have the appearance of exclamation marks -hair loss occurs over a period of weeks -regrowth of hairs occurs over several months -may recur in 1/3 of cases
question
Alopecia areata treatment
answer
Topical-clobetasol
question
Androgenic baldness (male pattern)
answer
o Etiology: the most common form of alopecia, is of genetic predetermination. o Presentation: The earliest changes occur at the anterior portions of the calvarium on either side of the "widow's peak" and on the crown (vertex). The extent of hair loss is variable and unpredictable.
question
Androgenic baldness (male pattern) treatment
answer
Minoxidil OTC topical for recent onset, Finasteride orally, work-up to determine cause if in women
question
Pyogenic granuloma

answer
a rapidly developing vascular lesion usually following minor trauma. This is a very common solitary eroded vascular nodule that bleeds spontaneously or after minor trauma. The lesion has a smooth surface, with or without crusts, with or without erosion. It appears as a bright red, dusky red, violaceous, or brown-black papule with a collar of hyperplastic epidermis at the base and occurs on the fingers, lips, mouth, trunk, and toes
question
Pyogenic granuloma treatment
answer
surgical excision or curettage with electrodesiccation at the base.
question
Spider angioma

answer
a type of telangiectasis[2] found slightly beneath the skin surface, often containing a central red spot and reddish extensions which radiate outwards like a spider's web. They are common and may be benign, presenting in around 10-15% of healthy adults and young children.[3] However, having more than five spider naevi may be a sign of liver disease.
question
Spider angioma treatment
answer
Spider angiomas are asymptomatic and usually resolve spontaneously. This is common in the case of children, although they may take several years to disappear. If the spider angiomas are associated with pregnancy, they may resolve after childbirth. In women taking oral contraceptives, they may resolve after stopping these contraceptives. The spider angiomas associated with liver disease may resolve when liver function increases or when a liver transplant is performed.
question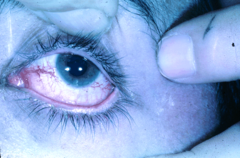
Spider vein (Telangiectasias)
answer
small dilated blood vessels near the surface of the skin or mucous membranes, measuring between 0.5 and 1 millimeter in diameter.They can develop anywhere on the body but are commonly seen on the face around the nose, cheeks, and chin. They can also develop on the legs, specifically on the upper thigh, below the knee joint, and around the ankles. Many patients who suffer with spider veins seek the assistance of physicians who specialize in vein care or peripheral vascular disease. These physicians are called phlebologists or interventional radiologists. Telangiectasia is a component of the CREST variant of scleroderma (CREST is an acronym that stands for calcinosis, Raynaud's phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia.)
question
Spider vein (Telangiectasias) treatment
answer
Sclerotherapy is the "gold standard" and is preferred over laser for eliminating telangiectasiae and smaller varicose leg veins. A sclerosant medication is injected into the diseased vein so it hardens and eventually shrinks away.
question
Cherry angioma
answer
1. tiny, bright red papules -turn brown with time 2. occur in all people > 30 years old
question
Cherry angioma treatment
answer
no treatment is required



