PBL #12 Breast cancer – Flashcards
Unlock all answers in this set
Unlock answersquestion
1. Differential diagnoses of breast lump
answer
1. Fbrocystic disease 2. lymphoma- when B or T lymphocytes divide faster than normal cells or live longer than they are supposed to. 3. intraductal papilloma-noncancerous (benign) tumor that grows in a milk duct of the breast. 4. phyllodes tumor-fast growing masses that form from the periductal stromal cells of the breast. 5. fibroadenoma- benign growth in the breast that causes lumpiness and tenderness, most common in pre-menopausal women 6. lipoma- a benign fatty growth that causes a lump 7. abscess-a painful collection of pus under the skin 8. galatocoele- retention cyst containing milk or a milky substance that is usually located in the mammary glands. 9. cyst- most common in pre-menopausal women (women who are still having periods) and those undergoing hormone replacement therapy 3. mastitis (inflammation of the breast) - this can be either breastfeeding mastitis or non-breastfeeding mastitis
question
2. Describe the symptoms and signs of breast cancer
answer
lump, dimpling, nipple displacement, rash, pain in the breast or armpit, swelling beneath the armpit or around the collarbone, fluid leakage. Inflammatory breast cancer: itching, pain, swelling, nipple inversion, warmth and redness, peau d'orange
question
3. Explain the pathology of breast cancer and describe the spread and metastasis of this condition
answer
Herceptin receptors lead to PI3K/AKT pathway? Normal cells undergo apoptosis but protected by PI3K/AKT pathway. However, mutation causes the pathway to be on permanently, rendering the cell immortal The inherited mutation in BRCA1 or BRCA2 genes can interfere with repair of DNA cross links and DNA double strand breaks (known functions of the encoded protein)[57] These carcinogens cause DNA damage such as DNA cross links and double strand breaks that often require repairs by pathways containing BRCA1 and BRCA2.[58][59] However, mutations in BRCA genes account for only 2 to 3 percent of all breast cancers BRCA1 is expressed in the cells of breast and other tissue, where it helps repair damaged DNA, or destroy cells if DNA cannot be repaired. If BRCA1 itself is damaged, damaged DNA is not repaired properly and this increases risks for cancers Local invasion: Cancer cells invade nearby normal tissue. Intravasation: Cancer cells invade and move through the walls of nearby lymph vessels or blood vessels. Circulation: Cancer cells move through the lymphatic system and the bloodstream to other parts of the body. Arrest and extravasation: Cancer cells arrest, or stop moving, in small blood vessels called capillaries at a distant location. They then invade the walls of the capillaries and migrate into the surrounding tissue (extravasation). Proliferation: Cancer cells multiply at the distant location to form small tumors known as micrometastases. Angiogenesis: Micrometastases stimulate the growth of new blood vessels to obtain a blood supply. A blood supply is needed to obtain the oxygen and nutrients necessary for continued tumor growth.
question
4. Outline normal histologic features of normal female breast

answer
...
question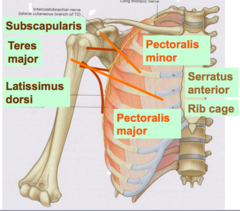
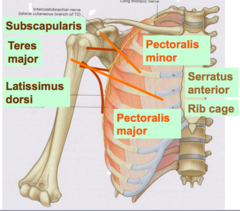
6. Describe the anatomy of the pectoral region and axilla, pectoralis major and minor origin, insertion and actions
answer
Pectoralis Major Origin: middle ½ clavicle, sternum, rib 1-5 Insertion: lateral lip of bicipital groove of humerous Action: adduction, medial rotation of arm Pectoralis Minor Origin: rib 3-5 Insertion: coracoid process of scapular Action: draw the scapular down / lift up the ribs
question
7. Explain how to investigate a breast lump, including the process of triple assessment
answer
Triple assessment: 1. clinical examinations for discoloration, lumps, dimpling, rash, contour, nipple displacement, lymph node enlargement. 2. Imaging- mammorgram/ultrasound 3. needle biopsy(to find out ER/PR/HER2 status
question
8. Describe briefly how DNA replicates within the cell cycle and describe the types of errors that can occur, their consequences and how these may be repaired
answer
1.A cell grows (G1), 2. continues to grow as it copies its DNA (S), DNA is separated by DNA helices which breaks the hydrogen bonds, forming a replication fork. DNA polymerase III codes from 5 prime to 3 prime, leading strand. RNA primase lays down RNA primers, then DNA polymerase III lays down new DNA. DNA polymerase I lays replaces primers with DNA. 3..grows more as it completes preparations for cell division (G2) 4. mitosis (M phase) Repair mechanism: Mismatch repair- The mismatch repair system detects and excises mismatched bases in newly replicated DNA, which is distinguished from the parental strand because it has not yet been methylated. MutS binds to the mismatched base, followed by MutL. The binding of MutL activates MutH, which cleaves the unmodified strand opposite a site of methylation. MutS and MutL, together with a helicase and an exonuclease, then excise the portion of the unmodified strand that contains the mismatch. The gap is then filled by DNA polymerase and sealed by ligase. Post -replication repair- The presence of a thymine dimer blocks replication, but DNA polymerase can bypass the lesion and reinitiate replication at a new site downstream of the dimer. The result is a gap opposite the dimer in the newly synthesized DNA strand. In recombinational repair, this gap is filled by recombination with the undamaged parental strand. Although this leaves a gap in the previously intact parental strand, the gap can be filled by the actions of polymerase and ligase, using the intact daughter strand as a template. Two intact DNA molecules are thus formed, and the remaining thymine dimer eventually can be removed by excision repair. Base excision repair-Base excision repair (BER), which repairs damage to a single base caused by oxidation, alkylation, hydrolysis, or deamination. The damaged base is removed by a DNA glycosylase. The "missing tooth" is then recognized by an enzyme called AP endonuclease, which cuts the phosphodiester bond. The missing part is then resynthesized by a DNA polymerase, and a DNA ligase performs the final nick-sealing step. Nucleotide excision repair-recognizes bulky, helix-distorting lesions such as pyrimidine dimers and 6,4 photoproducts. A specialized form of NER known as transcription-coupled repair deploys NER enzymes to genes that are being actively transcribed.
question
9. Outline cell cycle control mechanisms and their relevance to tumor development
answer
Two checkpoints: 1. between G2 and M 2. between G1 and S. In normal cells the Checkpoints are regulated by proteins known as cyclins and cyclin dependent kinases. Cyclins and cyclin dependent kinases have to be present at particular levels and form particular complexes for the cell to progress beyond the Checkpoints. During S phase, the cell can undergo apoptosis in trying to repair its DNA. Proto-oncogene: A normal cellular gene that has the potential to become an oncogene. Most proto-oncogenes are believed to function in cell growth and differentiation. e.g. HER2, BRAF, SIS, MYC Tumor suppressor genes: A gene whose protein product inhibits cell division, thereby preventing the uncontrolled cell growth that contributes to cancer. Tumor suppressor genes prevent uncontrolled cell division and therefore prevent cancer development.TP53 inhibit CDK(G1 cyclin-dependent kinase activity. RB1 act inhibit transcription of genes encoding proteins required for DNA synthesis.
question
10. define the term 'malignancy' and describe the mechanisms that lead to changes in oncogenes, tumor suppressor genes, and chromosomes with particular reference to the pathogenesis of cancer
answer
A carcinogen is any agent directly involved in causing cancer. Carcinogens may damage the DNA in the cells and induce uncontrolled cell division ultimately leading to the formation of tumors. 1. Chemical- smoking, coal 2. physical(UV light), 3. viral- 3a. Parts of the genome of DNA cancer viruses can be integrated in the genome of the host As a consequence there may be e.g. an inactivation of a tumor suppressor gene. The 3b. provirus does not contain an oncogene. it inserts itself next to c-myc. The strong promoter of the ALV causes uncontrolled cell proliferation and therefore tumorigenesis. 3c. The provirus contains an oncogene originally picked up by the host. 3d. translocation: CML: Fusion protein between ABL (9) and BCR (22) produces an oncogene with enhanced tyrosine kinase activity that leads to increased cell division and therefore tumorigenesis. Burkitt's lymphoma 4.heritable- TP53, BRCA1, 2 genes, Retinoblastoma is caused by a mutation in the tumour suppressor gene RB1.
question
11. Briefly describe non-neoplastic alterations of cell growth, distinguishing metaplasia from dysplasia
answer
Metaplasia = One type of epithelium reversibly transforms to another type(e.g. transformation zone in post-menopausal women, acid reflux from the stomach to the esophagus, cells undergo metaplasia, cells that are better equipped to deal with acid.) Dysplasia = cytological atypia(abnormal cell growth) low grade- does not involve the entire thickness of the epithelium. high grade- can be through the entire epithelium, but does not penetrate the basement membrane. synonymous with carcinoma in situ. once the basement membrane has been reached, it becomes invasive carcinoma. (NCR increased, pleomorphic, high mitotic cells)
question
12. Epithelial tumors: squamous: list locations
answer
Squamous epithelium: skin, oropharynx, esophagus, anal canal, vagina, external auditory canal. Tumor may arise from metaplasia e.g. bronchus of smokers.
question
12. Epithelial tumors: glandular epithelium: list their locations
answer
Entire GI tract from stomach to rectum. Lines ducts and acini of glands. Renal tubules, prostate glands. Tumors may arise following metaplasia in gastro-esophagla reflux disease.
question
12. Epithelial tumors: transitional epithelium: list their locations
answer
urothelial tract, i.e. renal pelvis, ureter, bladder and urethra
question
12. List non-epithelial tumors
answer
Non-epithelial tumours: connective tissue tumours lymphohaemopoeitic glial and neuronal tumours Germ cell tumours Embryonal tumours
question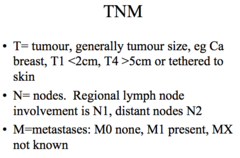
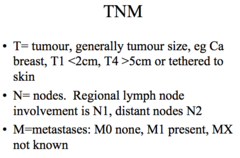
13. describe routes and mechanisms of tumor spread, the principles for staging malignant disease, and explain how histological findings influence prognosis
answer
1. directly into adjacent tissues (eg basal cell Ca of skin) 2. via lymphatics (eg Ca breast, colon) 3. blood vessels (eg renal cell Ca, small cell Ca lung, prostatic Ca, all sarcomas) 4. along nerves (eg Ca pancreas, prostate) 5. across cavities (eg Ca stomach, ovary) no lymph involvement is N0
question
12. Germ cell tumors: location and examples
answer
Tumours formed by the reproductive organs Testis: - Seminoma ( Commonest malignant tumour 25-45y), Good prognosis - Teratoma (Malignant or benign) Ovary - Teratoma (Malignant or benign)
question
14. outline the local, distant and systemic effects of malignancy
answer
Local: Dysplasia may be present in adjacent tissue, Vascular invasion often present, Infiltrative margin, lymph nodes, adjacent organs Distant: distant sites via blood, satellite nodules Systemic: unintentional weight loss, fever, being excessively tired, and changes to the skin.[12] Hodgkin disease, leukemias, and cancers of the liver or kidney can cause a persistent fever of unknown origin
question
16. explain major modes of inheriting including: autosomal dominant autosomal recessive and X-linked dominant and recessive and mitochondrial modes of inheritance and give examples of each
answer
Autosomal Dominant Dominant conditions are expressed in individuals who have just one copy of the mutant allele. Affected males and females have an equal probability of passing on the trait to offspring. thus each offspring has a 50% chance on inheriting the mutant allele. approximately half of the children of affected parents inherit the condition and half do not. Autosomal Dominant Conditions: • Huntington Disease • acondroplasia (short-limbed dwarfism) • polycystic kidney disease Autosomal Recessive when an individual has two copies of the mutant allele. When just one copy of the mutant allele is present, an individual is a carrier of the mutation, but does not develop the condition. Females and males are affected equally by traits transmitted by autosomal recessive inheritance. When two carriers mate, each child has a 25% chance of being homozygous wild-type (unaffected); a 25% chance of being homozygous mutant (affected); or a 50% chance of being heterozygous (unaffected carrier). Affected individuals are indicated by solid black symbols and unaffected carriers are indicated by the half black symbols. Autosomal recessive diseases: • Cystic fibrosis • Tay-Sachs • hemochromatosis • phenylketonuria (PKU) X-linked Recessive X-linked recessive traits are not clinically manifest when there is a normal copy of the gene. All X-linked recessive traits are fully evident in males because they only have one copy of the X chromosome, thus do not have a normal copy of the gene to compensate for the mutant copy!!!!. For that same reason, women are rarely affected by X-linked recessive diseases, however they are affected when they have two copies of the mutant allele. Because the gene is on the X chromosome there is no father to son transmission, but there is father to daughter and mother to daughter and son transmission. If a man is affected with an X-linked recessive condition, all his daughter will inherit one copy of the mutant allele from him. X-linked Recessive Disorders: • Duchenne muscular dystrophy • hemophilia A • X-linked severe combined immune disorder (SCID) • some forms of congenital deafness X-linked Dominant Because the gene is located on the X chromosome, there is no transmission from father to son, but there can be transmission from father to daughter (all daughters of an affected male will be affected since the father has only one X chromosome to transmit). Children of an affected woman have a 50% chance of inheriting the X chromosome with the mutant allele. X-linked dominant disorders are clinically manifest when only one copy of the mutant allele is present.
question
15. outline genetic factors important in the development of breast cancer
answer
Herceptin receptors lead to PI3K/AKT pathway? Normal cells undergo apoptosis but protected by PI3K/AKT pathway. However, mutation causes the pathway to be on permanently, rendering the cell immortal The inherited mutation in BRCA1 or BRCA2 genes can interfere with repair of DNA cross links and DNA double strand breaks (known functions of the encoded protein)[57] These carcinogens cause DNA damage such as DNA cross links and double strand breaks that often require repairs by pathways containing BRCA1 and BRCA2.[58][59] However, mutations in BRCA genes account for only 2 to 3 percent of all breast cancers BRCA1 is expressed in the cells of breast and other tissue, where it helps repair damaged DNA, or destroy cells if DNA cannot be repaired. If BRCA1 itself is damaged, damaged DNA is not repaired properly and this increases risks for cancers
question
17. know what is meant by variable penetrance and expression in single gene disorders
answer
Penetrance- The fraction of individuals with a genotype known to cause a disease who have any signs or symptoms of the disease Expression- Variation in the severity of a disorder in individuals who have inherited the same disease alleles (the extent to which a genetic defect is expressed) Variable expression- the extent to which a genotype exhibits its phenotypic expression
question
18. discuss the principles of radiotherapy and chemotherapy, differentiating between cytotoxic chemotherapy and other form of chemotherapy including the problems of unwanted effects and what measures may be employed to minimize their impact
answer
Radiation: (also internal radiotherapy or brachytherapy) Direct or indirect DNA damage. Photons or charged particals present in the radiation source ionizes water molecules producing free radicals (OH radicals) Free radicals in turn ionize the atoms present in the DNA molecule. Generally normal cells have excellent repair mechanisms but cancer cells are have diminished ability to repair the damages and hence continue to produce cells with the damage. These cells, which have the damaged DNA, will either die or reproduce slowly. Limitations: Tumours outgrow their blood supply and tissues become relatively hypoxic. The more hypoxic the tumour is the greater the resistance to radiotherapy. Fixation of oxygen plays a very important role in causing permanent damage to the DNA. Acute: damage to epithelial surfaces of the skin, mouth, pharynx and bowel mucosa cause soreness, diarrhoea and nausea. Odema & erythema: swelling of the soft tissues is encountered during radiotherapy. Red rashes are seen in the area of treatment. The patient is given steroids to reduce swelling Infertility: The gonads are very sensitive to radiation. They will be unable to produce gametes following the radiotherapy Fibrosis, hair loss, dryness, fetal damage Chemotherapy drugs exert their effect by inhibiting one or more of the steps involved in cell division Cytotoxic drugs non-selectively kill rapidly growing cells Cells damaged by chemotherapy die by induction of apoptosis Some tumours are defective in their ability to repair DNA cannot repopulate after cytotoxic injury Some tumours are highly proliferative relative to normal cells eg. High grade NHL chemotherapy side effects: Nausea and vomiting Alopecia Bone marrow suppression Life threatening, day 7-10 Dose limiting toxicity for most chemotherapy drugs Anaemia/neutropenia/thrombocytopenia Susceptible to unusual infections e.g.herpes encephalitis, mycoplasma pneumonia, fungal infections Mucositis Peripheral sensory neuropathy Diarrhoea/constipation Nephrotoxicity
question
19. outline the principles of management of early and late breast cancer in pre and postmenopausal women, mentioning the role of surgery, chemotherapy, radiotherapy and hormonal therapy
answer
Medical, radiation, surgical Curative- e.g. removing the lump, getting rid of the cancer Radical- removal of the cancer, lymph nodes, muscles, etc. Adjuvant- added on to the curative procedure. e.g. chemotherapy that follows surgery neoadjuvant- treatment given before the final treatment( chemotherapy, reduce the size of the tumor before surgery) palliative- prolonging life by doing symptom control(but cannot get rid of the cancer) important to identify the aim. curative or palliative
question
Where does the breast gland lie?
answer
2/3 on the pectoralis major 1/3 on the serratus anterior
question
What is polymastia(supernumerary breast), polythelia, asmastia? gynecomastia?
answer
polymastia is presence of multiple breasts. polythelia accessory nipples asmastia- no breast development gynecomastia- breast hypertrophy in males after puberty
question
Breast cancer cause, signs & symptoms, investigations, test findings, management
answer
Cause: genetic, environmental Signs & symptoms: lumps, discoloration, nipple inversion, dimpling etc. Enlarged lymph nodes in the axilla, subclavicular line. Investigations: Triple assessment includes clinical examination, imaging and needle biopsy. Mammogram will show large, jagged dense within the breast. Management: medication-Tamoxifen, aromatase inhibitor, Hepcitin, depending on the receptor status of the patient. Surgery- non-adjuvant chemotherapy if needed, assess for sentinal nodes, prior to surgery.
question
what is a wide local excision
answer
surgical procedure to remove a small area of diseased or problematic tissue with a margin of normal tissue. This procedure is commonly performed on the breast and to skin lesions, but can be used on any area of the body. The tissue removed is examined under a microscope to confirm the type of lesion and to grade malignant tumours. This examination also determines if all of the lesion has been removed without leaving any behind
question
What is metaplasia? dysplasia? hyperchromatic nuclei? pleomorphic nucleI?
answer
Metaplasia = One type of epithelium transforms to another type(can lead to some problems in the future, e.g. lungs, smoking) Dysplasia = cytological atypia(unstable cellular status) Hyperchromatic nuclei = dark blue Pleomorphic nuclei = many different shapes(usually it's dividing fast)
question
What is prominant nucleoli? mitotically active? high NCR? lymphovascular invasion?
answer
Prominent nucleoli = fast cell division Mitotically active = fast cell division High NCR = nuclear/cytoplasmic ratio(huge nucleus in cancer) Lymphovascular invasion = tumour cells enter vessels
question
Describe the steps and role of CDK(G1 cyclin-dependent kinase ) in the cell cycle
answer
1. Growth factor signaling 2. expression of early response genes 3. G1 cyclin-dependent kinase(CDK) activity. p53 inhibits CDK! 4. transcription of genes encoding proteins required fro DNA synthesis. Rb inhibits this process!
question
hormonal treatment: breast cancer
answer
1. Selective oestrogen receptor modulators (SERMS), Tamoxifen, Raloxifene 2. Aromatase inhibitors, Arimidex Letrozole 3.Ovarian suppression, Oophorectomy GnRH analogues 4Progestogens
question
what do administer for bowel cancer?
answer
glivec
question
what is -oma? -carcinoma? -sarcoma? Melanoma? Granuloma? lymphoma?
answer
1. neoplasm: new growth, loosely applied, doctors generally mean cancer when they use it. 2. -carcinoma:suffix applied to malignant epithelial tumors 3. -sarcoma:suffix applied to malignant connective tissue tumors(causing destruction, can kill patients) 4.-oma: suffix applied to a lump 5.Melanoma: malignant melanocytic lesion 6.Granuloma: inflammation with giant cells(nothing to do malignancy) 7.Lymphoma: malignancy of lymphoid tissue
question
Breast cancer: complications
answer
Metastasizing cancer drains into the lymph nodes and cause blockage of the lymph in the lymphatic vessels, causing lymphedema.



