51: Neurotransmission/Neurochemistry – Flashcards
Unlock all answers in this set
Unlock answersquestion
What are some biological challenges that neurons have to overcome?
answer
- need to extend long processes - need to conduct signals over long distances - need to convey information in a polarized unidirectional manner (from sensory to motor components)
question
What are some short-range signaling mechanisms used in the nervous system?
answer
- chemical synapses - autocrine signaling - paracrine signaling
question
How does the nervous system achieve long-distance signaling?
answer
Humoral signaling
question
What type of junction is used in the nervous system for electrical synapses?
answer
Gap Junctions
question
What are the three basic types of cells used in the nervous system?
answer
Neurons Glial Cells Ependymal and endothelial cells
question
What is the function of the glial cell?
answer
To support and maintain neurons
question
What is an astrocyte and why are they important?
answer
A type of glial cell in the brain; major functions include holding the neurons together in proper spatial relationship and inducing the brain capillaries to form tight junctions important in the blood brain barrier. They also play a critical role in regulating metabolism.
question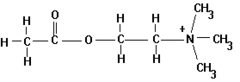
What are the two groups that make up acetylcholine?
answer
- Ester - Ammonium group (permanently charged)
question
What conformation does acetycholine prefer when in an aqueous solution?
answer
Gauche conformation (ester and ammonium only 60 degrees apart)
question
What acetylcholine conformation is preferred for muscarinic binding?
answer
Trans conformation (ammonium and ester group are separated by 180 degrees)
question
What is a cholinergic receptor?
answer
A receptor that is activated by acetylcholine.
question
What are two types of cholinergic receptors?
answer
Nicotinic Muscarinic
question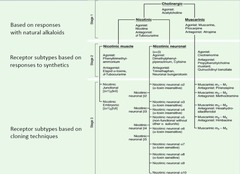
How do we differentiate between nicotinic and muscarinic receptors?
answer
Both are activated by ACh, but nicotinic receptors are ligand-gated channels that respond to nicotine and muscarinic are g-protein coupled receptors that respond to muscarine.
question
What is a muscarinic antagonist?
answer
Atropine
question
What are the two subtypes of nicotinic receptors?
answer
Nicotinic Muscle Nicotinic Neuronal
question
What are the two types of nicotinic muscle receptors?
answer
- Nicotinic junctional (adult) - Nicotinic embryonic (downregulated after birth)
question
Which subinit is different for all of the genetically different nicotinic neuronal receptors?
answer
alpha
question
How many muscarinic receptors have been cloned and how do they differ from one another?
answer
There are 5 and they have different functions and are differentially expressed in tissues.
question
What can be used to differentiate different cholinergic receptor subtypes?
answer
Drugs!
question
What is an agonist for both nicotinic and muscarinic receptors?
answer
ACh
question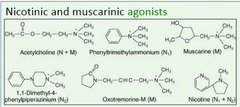
What are two agonists for muscarinic receptors?
answer
Muscarine Oxotremorine-M
question
What is an agonist for nicotinic muscular receptors?
answer
Phenyltrimethylammonium Nicotine
question
What is an agonist for nicotinic neuronal receptors?
answer
Nicotine 1, 1-Dimethyl-4-phenylpiperazinium
question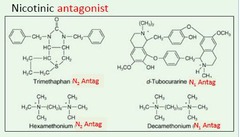
What can muscular nicotinic receptors be inhibited by?
answer
Tubocurarine Decamethonium
question
What can neuronal nicotinic receptors be inhibited by?
answer
Trimethaphan Hexamethonium
question
What are IPSP generated by?
answer
By catecholamines (e.g. dopamine, nor-epi) released by ACh acting on interneurons.
question
Is neurotransmission by autonomic ganglia caused by a single transmitter? Why?
answer
No. There is a fast (initial) EPSP generated by ACh activating nAChR (latency <2msec). This is followed by a slow EPSP generated by ACh activating mAChR (latency ~1sec, duration 30-60 sec). Then there is a late, slow EPSP generated by neuropeptides activating respective GPCR (slow onset; duration several min). IPSPs are also generated by ACh interneuron release of catecholamines.
question
What are some organs that are predominantly sensitive to sympathetic ganglionic blockade?
answer
Arterioles Veins Sweat glands
question
What are some organs that are predominantly sensitive to parasympathetic ganglionic blockade?
answer
Heart Iris Ciliary muscle GI tract Urinary bladder Salivary glands
question
What is the major receptor used by both the sympathetic and parasympathetic ganglia?
answer
nAChR for the production of the initial fast EPSP
question
Where do muscarinic ACh receptors occur in higher densities?
answer
Postsynaptic effector sites (rather than autonomic ganglia).
question
What does ganglionic blockade of the heart result in?
answer
Tachycardia due to the predominance of parasympathetic tone at the ganglia.
question
What does ACh activation of the postsynaptic receptor of the heart result in?
answer
Bradycardia due decreased conduction (AV block at high doses), small negative inotropic action
question
How does receptor subtype affect tissue response to postsynaptic stimulation by ACh?
answer
Activation of mAChRs can be excitatory or inhibitory depending on the receptor subtype and tissue affected.
question
What is the predominant receptor at the neuromuscular junction?
answer
nAChR, excitation-contraction coupling is fast.
question
What enzyme is responsible for making ACh?
answer
ChAT (choline acetyltransferase)
question
What is ACh made from?
answer
Choline and acetyl coenzyme A
question
What limits ACh synthesis?
answer
Choline uptake into the presynaptic nerve terminal.
question
What is the function of VAChT?
answer
To concentrate ACh (once synthesized) into presynaptic vesicles which is driven by a proton pumping ATPase.
question
What are two sources of choline?
answer
- 50% recycled from hydrolyzed ACh - Breakdown of phosphatidylcholine
question
How is ACh synthesis regulated?
answer
Through coregulation of ChAT and VAChT expression.
question
What is a non-competitive vesicular ACh transporter (VAChT) inhibitor?
answer
Vesamicol
question
What is a non-competitive choline acetyltransferase (ChAT) inhibitor?
answer
Hemicholinium
question
How is ACh broken down?
answer
Breakdown needs to be rapid. This is done by AChE (acetylcholinesterase) at the synapse. ACh + water is broken down into choline + acetate +water. AChE has an anionic site that attracts the positive choline group. Makes serine in active site very active to promote breakdown.
question
How many subunits make up the nAChR?
answer
5 subunits make up each of the 4 transmembrane segments (the alpha subunit is the only repeated one)
question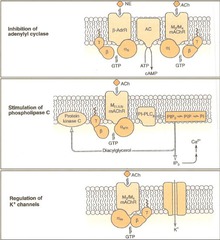
What are the primary biochemical responses mediated by mAChR?
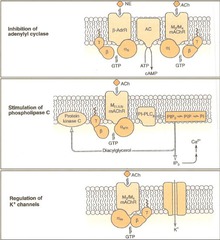
answer
- Inhibition of adenylyl cyclase (decreased cytoplasmic cAMP with M2/M4) - Stimulation of phopholipase C (activation of PLC, DAG, IP3 -->cytoplasmic Ca2+, PKC activation) - Regulation of K+ channels (inhibition of adenyl cyclase and beta/gamma activation of GIRK)
question
What does catechol refer to?
answer
A benzene ring with two -OH groups.
question
What are some catecholamines that are derived from L-Tyrosine?
answer
- Dopamine (convert L-Tyrosine to L-DOPA via tyrosine hydroxylase; then L-DOPA to Dopamine via DOPA decarboxylase) - Norepinephrine (Dopamine to NE via dopamine beta-hydroxylase) - Epinephrine (NE to Epi via phenylethanolamine N-methyltransferase)
question
What is the rate limiting step in catecholamine synthesis?
answer
Tyrosine hydroxylase hydroxylation of tyrosine at the meta position. This is highly regulated by phosphorylation (CaMKII, PKA, PKC).
question
How is norepi degraded?
answer
NE is degraded by monoamine oxidase or catecholamine O-methyl transferase (COMT) to form MHPG or VMA that can be recycled to make more product.
question
What are 3 important amine transporters?
answer
- Norepinephrine transporter (NET) - Dopamine transporter (DAT) - Vesicular membrane transporter (VMAT-2, takes them into vesicles)
question
What is the function of vesicular monoamine transporter 2 (VMAT 2)?
answer
It is an integral membrane protein that transports monoamines (dopamine, NE, serotonin, histamine, etc) from the cellular cytosol into the synaptic vesicles.
question
What determines which neurotransmitter will be put into the vesicle?
answer
The cell surface transporters like NET.
question
Describe what happens during 5-HT (serotonin) and noradrenaline (NA) neurotransmission.

answer
When a nerve impulse arrives at a 5-HT or NA nerve terminal the NT is released from the synaptic vesicle into the synaptic cleft. NT molecules bind to their specific receptors on the post-synaptic membrane and the nerve impulse is propagated or inhibited, depending of the receptor type. 5-HT and NA molecules are then released from their receptors and taken back into the nerve terminal via either the 5-HT or NA re-uptake transporters. 5-HT and NA are degraded by MAO and COMT, these enzymes are found in both the synaptic cleft and the nerve terminal.
question
What happens when selective 5-HT and NA re-uptake inhibitors (SNRIs) are used? Why is this important in depression?
answer
Depression is associated with reduced levels of the monoamines in the brain, such as 5-HT. The selective 5-HT and NA re-uptake inhibitors (SNRIs) are thought to restore the levels of 5-HT and NA in the synaptic cleft by binding at their re-uptake transporters preventing the re-uptake and subsequent degradation of 5-HT and NA. This re-uptake blockade leads to the accumulation of monoamines in the synaptic cleft and the concentration returns to within the normal range. This action of SNRIs is thought to contribute to the alleviation of the symptoms of depression. In the presence of the SNRIs, small amounts of 5-HT and NA continue to be degraded in the synaptic cleft.
question
Why do tricyclic antidepressants (TCAs) have side effects?

answer
TCAs are non-selective inhibitors of amine re-uptake transporters that lead to dry mouth, blurred vision, constipation, urinary retention, and other effects due to off site effects on muscarinic receptors.



