Thyroid pathology – Flashcards
Unlock all answers in this set
Unlock answersquestion
Hyperthyroidism
answer
- hypermetabolic state (elevated levels of free T3 and T4), sympathetic NS overstimulation the most common causes: - diffuse toxic hyperplasia (Graves d.) - - 80%toxic multinodular goiter (Plumer d.) - toxic (hyperfunctional) adenoma
question
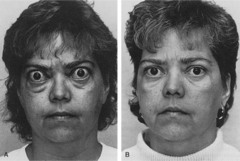
Hyperthyroidism clinical symptoms
answer
- heat intolerance, sweating - tachycardia, palpitations, cardiomegaly, arrhythmias - thyrotoxic cardiomyopathy - ocular changes (exophthalmos: wide-eyed, staring gaze) - neuromuscular system myopathy (proximal muscle weakness, atrophy of skeletal muscle) - tremor, hyperactivity - emotional lability - inability to concentrate - insomnia - GI system (hypermotility, diarrhea) - skin (soft, warm) - weight loss (increased appetite) - osteoporosis (bone resorption)
question
Graves disease

answer
- 2- 4 decade - F>M 10:1 - 1.5-2% of women - the most common endogenous hyperthyroidism - thyroid symetric enlargement > 60g, (toxic) + ophthalmopathy + pretibial myxedema (dermopathy)
question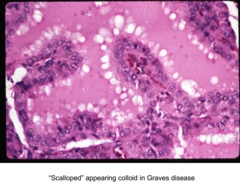
Graves disease histology
answer
- tall cells, crowded, small papillae, scalloped margins
question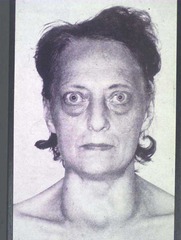
Graves disease symptoms triad
answer
- diffusely enlarged gland, - infiltrative ophthalmopathy with exopthalmos - and infiltrative dermopathy / pretibial myxedema (thickening and induration of shin, seen late in disease in 5-10%) (also cardiac hypertrophy with ischemic changes)
question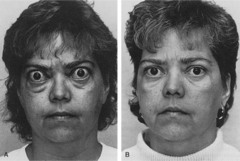
Opthalmopathy causes
answer
- displacement of the eyeball - the volume of retroorbital connective tissue is increased: - fatty tissue hyperplasia - infiltration by mononuclear cells (limf. T) - oedema of muscles - accumulation of ECM components : glycosaminoglycans - associated with high titer of anti-TSH antibodies
question
Graves disease lab findings
answer
- increased T3/T4 - increased uptake of radioactive iodine - decreased TSH
question
Graves disease antibodies
answer
autoantibodies: - long-acting thyroid stimulator (LATS): IgG that stimulates thyroid function (similar to but slower than TSH) (i.e. long-acting); specific for Graves' disease - thyroid stimulating immunoglobulins other than LATS also stimulate TSH rec. - TSH binding inhibitor immunoglobulins (have either a stimulatory or inhibitory effect) - antibody production probably due to primary T cell autoimmunity
question
Graves disease increased risk
answer
increased risk for other autoimmune diseases: - lupus erythematosus - pernicious anemia - type I diabetes - Addison disease
question
Hypothyroidism
answer
- decreased T3, T4 production - prevalence icreases with age (subclinical) - F>M 10:1
question
Hypothyroidism causes
answer
- iodine deficiency - radiation (to the neck), surgical ablation - Hashimoto thyroiditis (autoimmune) - drugs (lithium) - inborn errors - rare - suprathyroid (hypothalamic, deficient TSH)
question
Dietary iodine deficiency
answer
- iodine deficiency - low level of T3, T4 - TSH level rises - hypertrophy and hyperplasia of thyroid follicular cells - enlargement of thyroid gland (goiter) - T3, T4 production rises - euthyroid state - if the compensatory respose is not adequate (iodine deficiency is to high) - goiter + hypothyroidism (congenital)
question
Cretinism

answer
- when hypothyroidism begins in infancy or early childhood - endemic dietary iodine deficiency (mountainous areas) - Himalayas, China today: supplementation of food with iodine
question
Cretinism symptoms

answer
- severe mental retardation - impaired development of skeletal system (short stature), coarse facial features - protruding tongue - umbilical hernia
question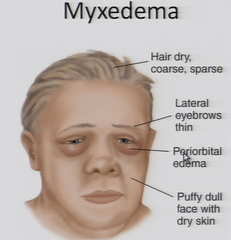
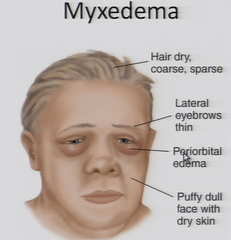
Myxedema
answer
- when hypothyroidism begins in adult - slowing of mental and physical activity - fatigue, apathy, listlessness - depression-like state - cold-intolerance, pale, dry skin - overweight, high cholesterol level - constipation (decreased sympathetic activity) - accumulation of glycosaminglycans in subcutaneous tissue: oedema, enlargment of the tongue, deep voice
question
Myxedema lab
answer
- serum TSH - high - T3, T4 - low
question
Thyroiditis types
answer
- Hashimoto thyroiditis (autoimmune) - Riedel thyroiditis - de Quervain thyroiditis (subacute)
question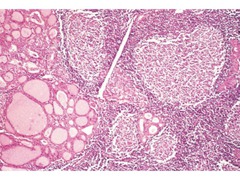
Hashimoto's thyroiditis
answer
- def: autoimmune disease: goiter + circulating antibodies: anti-thyroid peroxidase and anti-thyroglobulin - also called Hashimoto's disease, struma lymphomatosa, lymphocytic thyroiditis - 90-95% in women (4-6 decade) - can occur in children - most common cause of hypothyroidism in iodine-sufficient areas of the world - most common cause of nonendemic goiter in children
question
Hashimoto incidence
answer
- clusters in families - more common in Whites than Blacks or Japanese cause: breakdown in self-tolerance to thyroid auto-antigens
question
Hashimoto clinical presentation
answer
- goiter - painless - gradual thyroid failure due to autoimmune destruction - initially: transient hyperthyroidism - diffuse enlargment, pale, firm - intact capsule - associated with HLA-DR5 (goitrous form), HLA-DR3 (atrophic form)
question
Hashimoto risks
answer
- may coexist with SLE, rheumatoid arthritis, Sjogren's syndrome, pernicious anemia, type 1 diabetes, Graves' disease, chronic active hepatitis, adrenal insufficiency - MALT lymphomas of GI tract (80:1 relative risk), other B cell lymphomas - associated with well differentiated thyroid cancer may evolve into thyroid lymphoma
question
Hashimoto antibodies
answer
- anti-TSH (specific for Hashimoto's and Graves' disease) - anti-TG (less sensitive but similar specificity as anti-thryoid peroxidase) - anti-thyroid peroxidase (sensitive but not specific: 20% of adult women without disease have these antibodies) - anti-iodine transporter (rare) -note: anti-TSH antibodies block the TSH receptor in Hashimoto's disease but stimulate the TSH receptor in Graves' disease
question
Hashimoto treatment
answer
- at the beginning: no treatment needed - thyroid hormone for hypothyroidism - subtotal thyroidectomy to relieve mass effect - rarely progresses to lymphoma
question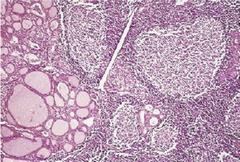
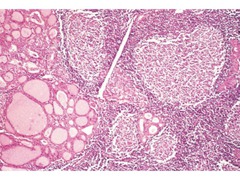
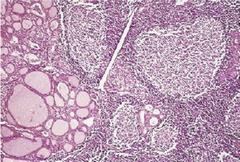
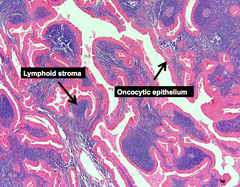
Hashimoto histology
answer
- extensive lymphocytic infiltrate with germinal center formation - lymphocytes: predominantly T cells and plasma cells (polyclonal) - atrophic follicles with abundant Hürthle cells/oncocytes - reduced colloid - fibrosis may be increased but does not extend beyond capsule - single giant cells may be seen - later little thyroid parenchyma is present
question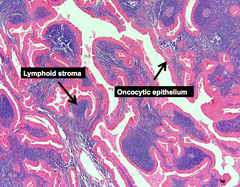
Hürthle cells/oncocytes
answer
An epithelial cell characterized by an excessive amount of mitochondria, resulting in an abundant acidophilic, granular cytoplasm
question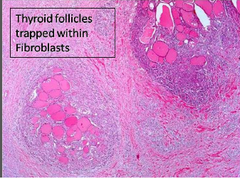
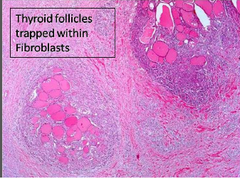
Riedel thyroiditis
answer
- etiology unknown - extensive fibrosis of thyroid and surrounding tissues
question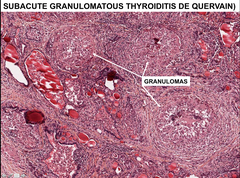
Subacute (de Quervain) thyroiditis
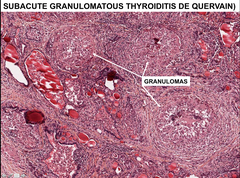
answer
- def: inflammation of thyroid gland with granulomas formation - also called granulomatous thyroiditis - rare (less common than Hashimoto's thyroiditis) - most common cause of thyroid pain - F>M 4:1 - 3-5 decade
question
de Quervain thyroiditis etiology
answer
- may be trigered by systemic viral infection - seasonal incidence - associated with epidemics of measles, mumps, - Coxsackie, adenovirus, upper respiratory infection, influenza - virus-induced tissue damage - lymphocytes T - process is self-limited - after 8 weeks: normal thyroid function
question
de Quervain thyroiditis clinical presentation
answer
- enlarged thyroid (variable), intact capsule - painful swallowing (odynophagia), sore throat, thyroid region tenderness - fever, fatigue, malaise - transient hyperthyroidism at 2-6 weeks
question
de Quervain laboratory findings
answer
- high T3/T4 (initially), elevated sedimentation rate (ESR) and CRP suppression of radioactive iodine uptake
question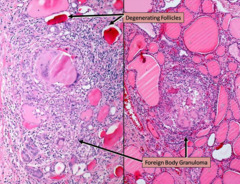
de Quervain thyroiditis histology
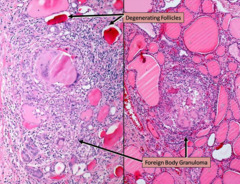
answer
- the foreign body giant cells with destruction of thyroid follicles
question
Solitary nodule in thyroid
answer
- one dominant nodule in multinodular goiter cyst possibilities: - focus of thyroiditis - adenoma (benign neoplasm) - carcinoma (less than 1% of solitary nodules) adenoma>ca 10:1
question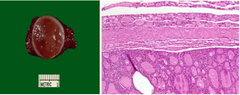
Adenoma (follicular adenoma)
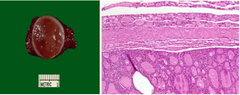
answer
- clinically: nodule difficult to distinguish from dominant nodule of nodular hyperplasia - usually: they are NOT forerunners to carcinoma - majority are nonfunctional (cold) - if functional (toxic adenoma): independent of TSH stimulation - solitary, round encapsulated lesion - well demarcated from the surrounding thyroid - a few cm
question
Adenoma clinical features
answer
- small: asymptomatic (unilateral painless mass) - bigger: difficulty in swallowing - on radionuclide scanning: cold nodule - do not recur, benign
question
Adenoma diagnosis
answer
- only by histological examination, not needle aspiration
question
Thyroid carcinomas incidence
answer
- rare: 1% of all cancer is US - 0.2% of all cancer deaths - estimated 34,000 new cases and 1500 deaths in US in 2007 - increasing incidence (due to new diagnostic practices which detect smaller tumors) - 20 year survival is 90%, because most are indolent papillary carcinomas - F>>M in reproductive age (often estrogen receptor positive, which may explain female predominance) - for other ages (children, >6decade: F=M) - more common in US whites than blacks, for unknown reasons
question
Thyroid carcinomas

answer
- Papillary ca - 80% - Follicular ca - 15% - Medullary ca - 5% - Anaplastic (undifferent.) - less than 5%
question
Thyroid carcinoma treatment
answer
- surgery: lobectomy, subtotal thyroidectomy or total thyroidectomy - post-operative radio-iodine therapy - can assess for recurrence with serum thyroglobulin levels, calcitonin (medullary carcinoma)
question
Papillary carcinoma of thyroid
answer
80% of thyroid carcinomas 70% women of reproductive age (2-5decade) occult tumors in 6% at autopsy (1-10 mm) 46% multicentric 14% with nodal metastases occult tumors in up to 24% with other thyroid disease
question
Papillary carcinoma of thyroid risk factors
answer
Risk factors: - ionizing radiation before age 20 (for acne-tonsillitis, tinea capitis, enlarged thymus) - post-Chernobyl - particularly children, or after exposure to nuclear explosions at Marshall Islands - Hashimoto's thyroiditis (possibly) - (FAP) Familial adenomatous polyposis
question
Papillary carcinoma of thyroid clinical presentation
answer
- painless nodule or mass on the neck - cervical node (usually cold on scan) - can be diagnosed by FNA - at presentation: 67% in thyroid only, in 13% thyroid and cervical nodes - nodal involvement is often not clinically apparent due to small size and similar consistency - nodal metastases may undergo cystic change and resemble branchial cleft cyst
question
Papillary carcinoma of thyroid gross features

answer
- solid, white, firm - solitary / multifocal often - encapsulated (10%) or infiltrative - variable cysts, fibrosis, calcification
question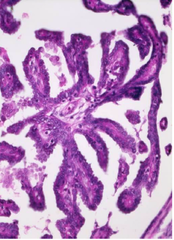
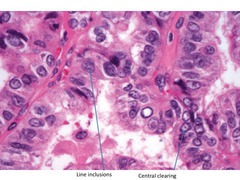
Papillary carcinoma of thyroid histology
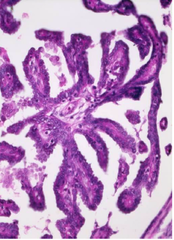
answer
- papillae with fibrovascular cores associated with follicles - papillae lined by cuboidal cells - overlapping nuclei, with finely dispersed optically clear chromatin (also called ground-glass, Orphan-Annie nuclei) - eosinophilic intranuclear inclusions (cytoplasmic invaginations) - nuclear longitudinal grooves (represent folding of redundant nuclear membrane, present in almost every high power field)
question
Orphan-Annie cells
answer
- characteristic for papillary carcinoma of thyroid - nuclei with uniform staining, which appear empty
question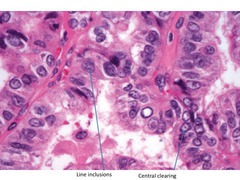
Characteristics in cells in papillary carcinoma of thyroid
answer
- Orphan Annie cells - Eosinophilic intranuclear inclusions - Nuclear longitudinal grooves
question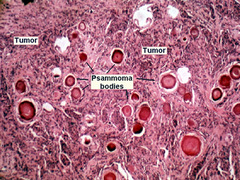
Psammoma bodies
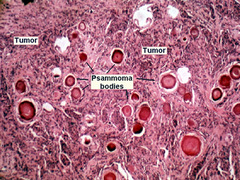
answer
- round collection of calcium, seen microscopically - in papillary stalk - due to tumor cells necrosis (calcification) - fairly specific for papillary carcinoma (although may be present in metastatic carcinoma to thyroid) Note: presence of psammoma body in neck or cervical lymph node means papillary thyroid carcinoma must be ruled out
question
Papillary thyroid carcinoma clinical features
answer
- asymptomatic thyroid nodule - „cold" nodule on radionuclide scanning - enlarged cervical lymph node - advanced disease: hoarseness, dysphagia, cough lung meta - rare (10%) - good prognosis (even with lymph node meta) - 10 years - 95%
question
Follicular carcinoma
answer
- ca. with follicular differentiation - no papillary nuclear features - 15% of thyroid ca. and 25-40% in iodide-deficient areas - usually solitary - usually "cold" on radionuclide scan - F>M 3:1, (older than PC): 40-50's
question
Follicular carcinoma of thyroid risk factors
answer
- radiation exposure - iodine deficiency - older age * does not arise from preexisting adenomas!
question
Follicular carcinoma of thyroid metastases
answer
- rare lymphatic spread - spread to lungs, liver, bone, brain via veins (hematogenously)
question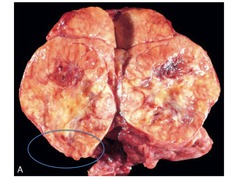
Follicular carcinoma gross features
answer
- gray-tan-pink - usually single encapsulated nodule - focally hemorrhagic - variable fibrosis - calcification rare - larger lesions are often - infiltrative
question
Follicular carcinoma of thyroid histology
answer
- need convincing evidence of invasion of adjacent thyroid parenchyma - complete penetration of the capsule blood vessels invasion (medium sized veins / vessels in or beyond the capsule) - capsule is typically thick with calcification - architectural patterns: follicular or solid - may have nuclear atypia, Hürthle cells, focal spindled areas, mitotic figures - no nuclear features of papillary carcinoma; - no psammoma bodies; no/rare lymphatic invasion
question
Follicular carcinoma of thyroid FNA
answer
- nuclear enlargement, overlapping and crowding - cannot distinguish between follicular adenoma and carcinoma by fine needle aspiration since need evidence of capsular or vascular invasion or invasion of adjacent parenchyma - molecular: Ras mutations in 49%
question
Main difference between follicular adenoma and follicular carcinoma
answer
- in papillary carcinoma the capsule is invaded
question
Follicular carcinoma of thyroid treatment
answer
- total thyroidectomy - radioactive iodine metastasis take up the radioactive iodine - (identification of meta)
question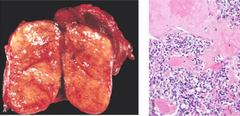
Medullary carcinoma of thyroid
answer
- neuroendocrine tumor derived from C cells (parafollicular cells) of neural crest - secretes calcitonin
question
Medullary carcinoma of thyroid incidence
answer
- 5-10% of thyroid carcinomas - either sporadic (nonhereditary) or hereditary (familial) serum calcitonin - postoperative follow-up
question
Sporadic medullary carcinoma
answer
- 80% - age 40-60 years, solitary - paraneoplastic syndromes (diarrhea from VIP, Cushing's syndrome) - dysphagia and hoarseness (tumor mass)
question
Familial medullary carcinoma
answer
- younger patients (mean: 35 years) - MEN 2A or 2B syndromes, familial medullary - thyroid carcinoma syndrome, von Hippel-Lindau disease or neurofibromatosis (NF) - usually bilateral, multicentric with C cell hyperplasia - usually discovered by screening serum calcitonin - RET oncogene mutational analysis - MEN 2: germ line mutations in RET proto-oncogene
question
Medullary carcinoma histology
answer
- round cell nests - granular cytoplasm - uniform round nuclei with punctate chromatin - amyloid deposits in the stroma (from calcitonin) - prominent vascularity - calcifications - often angiolymphatic invasion - C cell hyperplasia present in familial but not sporadic cases
question
Anaplastic carcinoma of thyroid
answer
- high grade (G3) carcinoma - called: undifferentiated carcinoma, sarcomatoid carcinoma - 2% of thyroid cancers but 40% of thyroid cancer deaths - mean age 65 years - F>M 3:1 - 50% have prior multinodular goiter, 20% have prior differentiated carcinoma - arises as transformation of ca (papillary, follicular or Hürthle cell)
question
Anaplastic carcinoma of thyroid clinical features
answer
- rapidly enlarging, bulky neck mass - invades adjacent structures (hoarseness, dysphagia, dyspnea) - most thyroid sarcoma-like tumors are probably anaplastic carcinomas
question
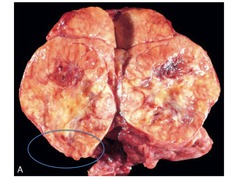
Anaplastic carcinoma of thyroid gross characteristics
answer
- solid tumor - large - areas of necrosis and hemorrhage - invades adjacent structures
question
Anaplastic carcinoma of thyroid treatment
answer
- resistant to all treatments - death usually within 1 year - mean survival 6 months - <10% survive at least 2 years



