Radiation Physics Pearls – Roach 2 – Flashcards
Unlock all answers in this set
Unlock answersquestion
There are three major types of brachytherapy implants:
answer
(1) Molds/plaques (2) Interstitial implants (3) Intracavitary implants
question
Type of brachytherapy used for superficial lesions where radioactive sources are placed over skin or orbital lesions
answer
(1) Molds/plaques - used for superficial lesions where radioactive sources are placed over skin or orbital lesions,
question
type of brachytherapy used w/radioactive sources are incased in wire or seeds and inserted in tumor (e.g., prostate),
answer
(2) Interstitial implants - radioactive sources are incased in wire or seeds and inserted in tumor (e.g., prostate),
question
Type of brachytherapy used w/sealed radioactive sources are placed inside a body cavity (e.g., cervix).
answer
(3) Intracavitary implants - sealed radioactive sources are placed inside a body cavity (e.g., cervix). Temporary seed insertion and removal are now performed with computerized afterloaders.
question
High-dose rate (HDR) implants use dose rates of ___ cGy/min. Lower than this is generally termed low dose rate (LDR).
answer
High-dose rate (HDR) implants use dose rates of >20 cGy/min. Lower than this is generally termed low dose rate (LDR).
question
Major radionucleotides used in brachytherapy Radionuclide: I-125 Half-life Photon energy (MeV) HVL (mm Pb) Clinical use
answer
I-125 59.4 days 0.0028 avg 0.025 Permanent prostate implant
question
Major radionucleotides used in brachytherapy Radionuclide Half-life Photon energy (MeV) HVL (mm Pb) Clinical use
answer
Pd-103 17.0 days 0.021 avg 0.008 Permanent prostate implant
question
Major radionucleotides used in brachytherapy Radionuclide: Cs-131 Half-life Photon energy (MeV) HVL (mm Pb) Clinical use
answer
Cs-131 9.7 days 0.029-0.034 0.030 Permanent prostate implant
question
Major radionucleotides used in brachytherapy Radionuclide: Au-198 Half-life Photon energy (MeV) HVL (mm Pb) Clinical use
answer
Au-198 2.7 days 0.412 2.5 Permanent head and neck implant
question
Major radionucleotides used in brachytherapy Radionuclide: Cs-137 Half-life Photon energy (MeV) HVL (mm Pb) Clinical use
answer
Cs-137 30 years 0.662 5.5 Temporary intracavitary implants
question
Major radionucleotides used in brachytherapy Radionuclide: Ir-192 Half-life Photon energy (MeV) HVL (mm Pb) Clinical use
answer
Ir-192 73.8 days 0.38 avg 2.5 Temporary intracavitary or interstitial implants (HDR) for prostate, breast, cervix. Also used for skin
question
Major radionucleotides used in brachytherapy Radionuclide: Co-60 Half-life Photon energy (MeV) HVL (mm Pb) Clinical use
answer
Co-60 5.26 years 1.25 avg 13.07 Older source for teletherapy
question
Major radionucleotides used in brachytherapy Radionuclide: Ra-226 Half-life Photon energy (MeV) HVL (mm Pb) Clinical use
answer
Ra-226 1,622 year 0.83 avg 12 Historical interest
question
Major radionucleotides used in brachytherapy Radionuclide: Rn-222 Half-life Photon energy (MeV) HVL (mm Pb) Clinical use
answer
Rn-222 3.83 days 0.83 avg 12 Temporary implant
question
What law relating distance to dose is of tantamount importance in brachytherapy?
answer
Briefly, this law states that the energy absorbed at a given distance from a point source is inversely proportional to the square of the distance of the source. This is denoted by 1/r^2.
question
What are three ways of quantifying radioactivity:
answer
There are three ways of quantifying radioactivity: (1) mCi (see above), (2) mg-Ra (milligram equivalent of radium) (obsolete), or (3) air-kerma strength (the current standard). Air-kerma strength is the dose rate in air at a specified distance in units of (Gy)(m2)/h.
question
Define Air Kerma Strength
answer
Air-kerma strength is the dose rate in air at a specified distance in units of (Gy)(m2)/h.
question
What are the 3 systems for placing interstitial implants
answer
+Quimby system: radioactive sources are distributed uniformly over volume of tissue leading to nonuniform dose. +Manchester system: radioactive sources are distributed nonuniformly with the goal of ±10% dose uniformity. +Paris system: developed for linear sources of iridium wire; sources are distributed uniformly for a planar implant, but follow a particular pattern for volume implants.
question
Radioactive sources are distributed uniformly over volume of tissue leading to nonuniform dose.
answer
+Quimby system: radioactive sources are distributed uniformly over volume of tissue leading to nonuniform dose. +Manchester system: radioactive sources are distributed nonuniformly with the goal of ±10% dose uniformity. +Paris system: developed for linear sources of iridium wire; sources are distributed uniformly for a planar implant, but follow a particular pattern for volume implants.
question
radioactive sources are distributed nonuniformly with the goal of ±10% dose uniformity.
answer
+Manchester system: radioactive sources are distributed nonuniformly with the goal of ±10% dose uniformity.
question
developed for linear sources of iridium wire; sources are distributed uniformly for a planar implant, but follow a particular pattern for volume implants.
answer
+Paris system: developed for linear sources of iridium wire; sources are distributed uniformly for a planar implant, but follow a particular pattern for volume implants.
question
How is dose sculpted over an area using catheter based brachtherapy?
answer
By positioning sources at a given position for variable periods of time (called dwell times), one can produce conformal dose distributions.
question
In order to perform photon dose calculations, three key variables are important:
answer
In order to perform photon dose calculations, three key variables are important: (1) attenuation (see above) in tissue, (2) inverse square law (see above) or the distance from the radiation source, and (3) photon scattering due to the Compton effect (see above).
question
Generally radiation doses are given in the unit Gray (Gy), which represents ____
answer
Generally radiation doses are given in the unit Gray (Gy), which represents absorbed dose (specifically 1 J/kg of tissue).
question
specific amount of charge collected in one of the beam monitoring ionization chambers =
answer
AMU represents a specific amount of charge collected in one of the beam monitoring ionization chambers.
question
used to convert rectangular fields into square equivalents for ease of calculation;
answer
Equivalent square formula: used to convert rectangular fields into square equivalents for ease of calculation; E = 2XY/(X + Y), where E = equivalent square field size, and X and Y are the initial field dimensions.
question
What is the Equivalent square formula:
answer
Equivalent square formula: E = 2XY/(X + Y), where E = equivalent square field size, and X and Y are the initial field dimensions.
question
used to estimated necessary wedge angle when two beams are arranged at a particular hinge angle to each other in order to produce a more uniform dose distribution;
answer
Wedge/hinge angle formula: used to estimated necessary wedge angle when two beams are arranged at a particular hinge angle to each other in order to produce a more uniform dose distribution; wedge angle = 90° - (hinge angle/2).
question
Wedge Angle Formula =
answer
wedge angle = 90° - (hinge angle/2).
question
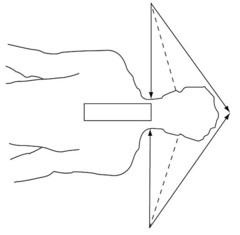
used to calculate the separation between two field edges (e.g., the gap) on the skin when they are matched at a given depth in tissue.
answer
Skin gap formula for matching fields: used to calculate the separation between two field edges (e.g., the gap) on the skin when they are matched at a given depth in tissue. Skin gap = (L1/2)*(d/SSD1) + (L2/2)*(d/SSD2). L = length of the field, d = depth of match, SSD = source to surface distance; for isocentric setups substitute SAD for SSD
question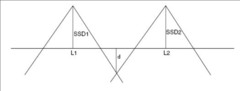
What is the formula for calculating the skin gap?
answer
Skin gap = (L1/2)*(d/SSD1) + (L2/2)*(d/SSD2). L = length of the field, d = depth of match, SSD = source to surface distance; for isocentric setups substitute SAD for SSD
question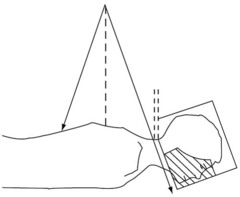
How do you calculate the Collimator angle of cranial field to match the inferior border with the superior border of spine field?
answer
Collimator angle of cranial field to match the inferior border with the superior border of spine field = atan [(1/2 spine field length)/SSD]
question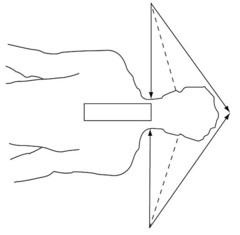
How do you calculate the Couch angle to make superior edge of spine field parallel to inferior border of cranial field ?
answer
Couch angle to make superior edge of spine field parallel to inferior border of cranial field = atan [(1/2 cranial field length)/SAD]
question
Unlike photons, electrons deposit most of their dose at the _____. Also unlike photons, as the energy of electrons >,<,= the percentage of dose deposited at the surface increases.
answer
Unlike photons, electrons deposit most of their dose at the surface. Also unlike photons, as the energy of electrons increases, the percentage of dose deposited at the surface increases.
question
The 4:3:2 rule for electrons refers to _____
answer
The 4:3:2 rule for electrons refers to the fact that the: 90% isodose line for electrons is generally ~MeV/4, 80% isodose line is generally ~MeV/3, & the effective range of electrons is ~MeV/2.
question
The amount of Pb shielding required for electrons may be estimated as _____
answer
The amount of Pb shielding required for electrons may be estimated as MeV/2 (in mm).



