PT Guide to Practice – Flashcards
Unlock all answers in this set
Unlock answersquestion
Primary Care
answer
- the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs - developing a sustained partnership with patients and practicing within the context of family and community. --> first person you see when you have a problem --> PT has direct access
question
Secondary Care
answer
- Patients that were initially treated by other practitioners and then referred to physical therapists. -->If your primary care isn't working, then you go a step up to someone more specific to you. -->This has been our general position as a PT
question
Tertiary Care
answer
- Specialized care provided in specialized settings --> E.g. ICU, inpatient rehab --> provided by physical therapists in highly specialized setting
question
Primary Prevention
answer
- Identify risk factors and implement services to reduce risk in individuals and populations --> Trying to prevent anything from happening right from the start
question
Secondary Prevention
answer
- Prevent or slow the progression of functional decline/disability and enhance activity and participation in chosen life roles in individuals with an identified condition --> Something has happened
question
Tertiary Prevention
answer
- Reduce the degree of disability by restoring-or preventing the deterioration of-skills and independence in patients with chronic health conditions. --> Trying to keep them as independent as possible
question
Primary Prevention Examples
answer
- Encouraging kids/adults to wear bike helmets via farmers' markets, school visits, day care visits, etc. --> We want to prevent injuries before they happen, so do a fall prevention screening. Hand out helmets. We play a role in this
question
Secondary Prevention Examples
answer
- Concussive evaluations, education on concussions and tracking concussions throughout a person's life --> secondary prevention for her son after he had his first concussion
question
Tertiary Prevention Examples
answer
- Treating a patient who has suffered a traumatic brain injury (TBI). Educating the family how to care for that patient including adapting environments according to cognitive impairments, physical impairments, etc. --> If someone suffers a brain injury, you are trying to prevent other injuries/diseases from occurring and further disabling him.
question
Other Roles of PT's (4)
answer
- consultation - education (clients, students, public, PTs, etc.) - critical inquiry - administration
question
Consultation
answer
- Rendering of professional opinion or advice by a physical therapist.
question
Critical Inquiry
answer
- Performing, analyzing and applying research --> Process of applying the principles of scientific methods
question
Administration
answer
- Managing resources effectively & efficiently --> E.g. ensuring reimbursement, budgeting, managing staff, contracts, etc.
question
"Guide Concepts" Four major constructs and concepts inform current physical therapist practice:
answer
- The International Classification of Functioning, Disability, and Health (ICF) and he Biopschosocial Model - Evidence-Based Practice - Professional Values - Quality Assessment
question
Disablement (definition)
answer
- Various impact(s) of chronic and acute conditions on the functioning of specific body systems on the basic human performance and on people's functioning in necessary, usual, expected and personally desired roles of society.
question
Nagi's Disablement Model
answer
- The focus changes from treating a diagnosis to treating the impact of a condition on a person's function and roles --> So say someone had pneumonia and the physician thinks if he gives the right antibiotic everything will be fine. Nagi said wait, the patient was in bed for 2 weeks so the pneumonia has a lot of other problems now. It is more than just treating the pneumonia diagnosis. --> is saying that something is wrong with the body and it is limiting what people can do. (There is a problem and we need to fix it)
question
Four Key Parts of Nagi's Disablement Model
answer
Pathology Impairment Functional Limitation Disability
question
Diagram of Nagi's Disablement Model
answer
- The Model as Nasgi wrote it - Someone has pneumonia and the medical team comes in to try to treat it at the micro level. - They suffer other problems in other parts of the body - This limits their ability to perform basic actions (limits functional limitation)
question
"Nagi's Disablement Model": Pathology
answer
- The interruption of or interference with the normal processes and the efforts of the organism to restore itself to a normal state - The body isn't behaving normally - The body is disrupted out of the homeostatic state.
question
"Nagi's Disablement Model": Impairment
answer
- "Consequence of the Disease" - A loss or abnormality of physiological, psychological, mental, or anatomical structure or function, occurs at the tissue, organ and system level. --> Comes after pathology hits --> think of as a neuromuscular, musculoskeletal, etc.. What is happening at a system level?)
question
"Nagi's Disablement Model": Function
answer
- Those activities identified by an individual as essential to support physical, social, and psychological well-being and to create a personal sense of a meaningful life. --> the essential things you need to do daily things --> ADL - activities of daily living
question
ADL
answer
activities of daily living - e.g. dishes, brush teeth, get dressed, bathroom - the things you need to do in your house
question
"Nagi's Disablement Model": Functional Limitation
answer
- A restriction of the ability to perform a physical action, activity, or task in an efficient typically expected or competent manner - - at the level of the whole person - -
question
"Nagi's Disablement Model": Disability
answer
- The inability or restricted ability to perform actions, tasks and activities related to required self care, home management, work, community and leisure roles in the individuals sociocultural context and physical environment. --> Things that happen outside of the patients home. --> Can they go to work, visit friends for coffee, see kid play baseball, get work done, get up and down the curb, walk your dog --> how does this affect her role in society
question
EXAMPLE of patient w/ multiple sclerosis Pathology, Impairment, Functional Limitation, Disbility
answer
- Pathology: Multiple Sclerosis - Impairment: Decreased strength, decreased muscle tone, impaired sensation - Functional Limitation: Inability to walk, inability to speak clearly - Disability: Cannot care for herself, cannot fulfill "traditional roles" as mother and grandmother
question
Class Example: 27 Year Old Jill w/ ACL Rupture
answer
- Pathology: ACL Rupture - Impairment: (impairments that happen in the body because of the rupture; how body systems are effected). Decreased strength (musculoskeltal), decreased ROM, pain (nervous system), edema (lymphatic system, integumentary), decreased aerobic capcity/endurance (cardiovascular), decreased balance, - Functional limitations (in the home by herself, how can she take care of herself): inability to go up and down stairs, difficulty bathing, getting dressed, grab things out of her closet/the fridge, walking, cooking (Walking is kind of controversial) - Disability - driving
question
In June 2008, the APTA House of Delegates officially endorsed the ______________
answer
World Health Organization's (WHO) International Classification of Functioning, Disability and Heath (ICF)
question
ICF Terminology: Health
answer
a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity
question
Benefits of WHO's International Classification of Functioning, Disability, and Health (ICF)
answer
- Improves communication - Considers all factors relevant to person's health - More comprehensive - Helps understand consequences of pt condition - Clinically and research applicability --> Want all therapists to use the same terms so we have a clear understanding of each other's language.
question
Diagnoses are important for defining the cause and prognosis, but identifying...
answer
- the limitations of function is often the information used to plan and implement interventions - When they wanted to go from a disablement model to an ablement model, they wanted to see how they can improve a person's life.
question
Simplistic version (figure) of the ICF model.
answer
- Up top we have a health condition (kind of replaces "pathology") - Because of the health condition, we have impairments at the body structure and functions (impairments is still there). How is a person's A;P different - Third word is activity instead of function. What does that person need to do on a day to day basis to take care of themselves - Last work is participation. How can they participate in society. What is their ability to participate --> Can see transition from disablement to ablement --> The WHO is recognizing environmental and personal factors (epigenetics) Two people with the same exact health condition can have totally different outcomes. Ex) Someone who hates going to work will influence how fast they get better versus someone who is very motivated and wants to get back to their job
question
More complex version (figure) of to show the structure of the ICF model.
answer
- Be able to draw this model and explain each component!!
question
ICF Terminology: Body Structures and Body Functions
answer
Changes that occur to the anatomy and physiology of the body based on the state of the individual's health
question
ICF Terminology: Activity
answer
- The ability to perform day to day basic needs; activities of daily living (ADLs).
question
ICF Terminology: Participation
answer
The ability to perform roles in society; instrumental activities of daily living (IADLs).
question
ICF Terminology: Capacity
answer
The ability to perform the skill in a controlled environment.
question
ICF Terminology: Performance
answer
The ability to perform in the skill in a variety of environments.
question
ICF Terminology: Functioning
answer
Encompasses all body functions and structures, activities and participation.
question
ICF Terminology: Disability
answer
Encompasses impairments of body functions and structures, activity limitations and participation restrictions.
question
T/F: Functioning and disability exist along a continuum of health
answer
True
question
ICF Terminology: Contextual Factors
answer
- Includes external environment factors and personal factors - influence how disability is experienced by the individual
question
ICF Terminology: External Environment
answer
Social support, Characteristics of the home environment, legal structures, climate, terrain.
question
ICF Terminology: Personal Factors
answer
Age, Education, Past experiences, Behaviors, etc.
question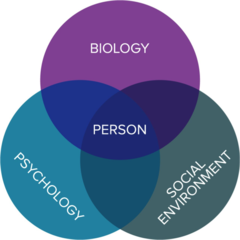
The biopsychosocial model of health (figure)
answer
- According to this model, a person's health status is determined by the interplay of the person's status in the biological, psychological, and social domains. - For example, 2 people with the same pathology who have different levels of motivation and different levels of socioeconomic resources might have very different outcomes in terms of functional status and level of participation. All o f these things interact in order to make up a person. -->We look to treat a person as a whole, which means all three of these. --> All influence each other
question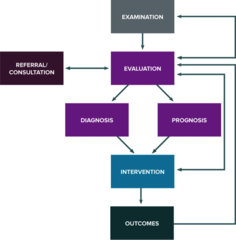
The Physical Therapist Patient/Client Management Model contains the following elements: **KNOW THESES**
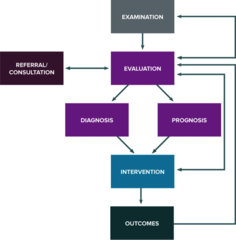
answer
- Examination - Evaluation - Diagnosis - Prognosis - Intervention - Outcomes
question
The physical therapist's "examination" includes:
answer
- History - Systems review - Tests ; Measures *The objective is to determine if the patient will be treated effectively and efficiently by a physical therapist.
question
Patient Management: Examination HISTORY may include:
answer
Chief complaint Medical/surgical history Employment history Living environment General health status Social ; health habits Family history Current condition Social history *Functional status *Activity level Medications Clinical tests -->NEED to ask functional status and activity level Need to know their typical physical activity level
question
Patient Management: Examination SYSTEMS REVIEW
answer
- Brief, "hands-on" examination - Two Parts: (1) the anatomical and physiological status of the cardiovascular/pulmonary, integumentary, musculoskeletal, and neuromuscular systems (2) the communication ability, affect, cognition, language, and learning style of the individual - the assessment of orientation (person, place, time), learning preferences, expected emotional/behavioral responses --> what is good to go, what I don't need to really worry about --> Determining what you don't need to spend a lot of time on
question
T/F We will learn a 3 minute screen
answer
True - This includes height and weight b/c of the obesity epidemic (obese people take longer to heal)
question
(1) Cardiovascular/pulmonary system:
answer
(1) HR, BP, RR, edema assessment of heart rate, respiratory rate, blood pressure, and edema
question
(2) Integumentary system
answer
(2) skin integrity, skin color, presence of scar formation
question
(3) Musculoskeletal system:
answer
(3) gross symmetry, gross ROM, gross strength, height ; weight
question
(4) Neuromuscular system:
answer
(4) gross coordinated movement (balance, locomotion, transfers and transitions)
question
T/F Just because you have seen someone once, doesn't mean you shorten your examination
answer
True
question
Patient Management: Examination TEST & MEASURES
answer
- Means of gathering data about the patient/client - Therapist has a diagnostic hypothesis from the history & systems review that may be further investigated by specific tests & measures. --> confirm or reject a hypothesis about the factors that contribute to making the individual's current level of function less than optimal --> Can we gather data to support our hypothesis
question
"Tests and Measures" are used to:
answer
- Rule in or out causes of impairment ; functional limitations - Identify and characterize a pathology, impairments, functional limitations - Establish diagnosis and prognosis, select intervention and document changes in patient status - To indicate achievement of goals/outcomes and assure timely and appropriate discharge.
question
Each "test and measure" includes:
answer
- A general definition and purpose - Clinical indications - Specific tests and measures - Tools used to gather data - Data generated
question
Reexamination
answer
- Used to modify or redirect interventions and evaluate progress toward goals/outcomes
question
Patient Management: Evaluation
answer
Clinical judgments based on the synthesis of all of the information
question
The "evaluation" reflects the
answer
- Chronic nature of problem - Multi-site or system involvement - Pre-existing conditions - Stability of the condition --> occurs at the start of care and continues throughout the episode of care
question
In an "evaluation" PT's must consider the:
answer
- Severity and complexity of current impairment, prolonged impairments, functional limitations and disability - Living environment and discharge plans - Social supports
question
"PT's as being the Gatekeepers"
answer
- Where is this patient going to go when they leave (e.g.. Want you out of acute-care in 3 days) - PT's play a big role in this because they look at the whole model - Need to look at the whole and then make recommendation
question
Patient Management: Diagnosis
answer
- Label used to identify the impact of a condition on function at the level of the system (particularly the movement system for PT's) and at the level of the whole person - Indicates the primary dysfunctions toward which the PT directs interventions
question
How to write a diagnosis?
answer
- This patient has a gait abnormality because of muscle weakness. - Try to do more than just say a shoulder bursitis. How does the shoulder bursitis effect the person - This will direct your interventions
question
Patient Management: Prognosis
answer
- The determination of the predicted optimal level of improvement in function and the amount of time needed to reach that level. (How well you will improve and about how long it will take)
question
Patient potential
answer
- What is the highest level of function that is likely to be habitual? - Motivation of the patient
question
T/F Never say a patient is un-motivated
answer
True
question
Patient Management: Intervention
answer
- Coordination, communication, & documentation - Patient/Client related instruction - Procedural interventions (9 categories) --> Intervention includes 3 main things
question
Physical therapist interventions are organized into 9 categories:
answer
- (1) Patient instruction - Airway clearance techniques - Assistive technology - Biophysical agents - Functional training in a variety of environments - Integumentary Repair/Protection - Manual therapy - Motor function training - Therapeutic exercise
question
Patient/Client related instruction ---> What do we instruct?
answer
What do we instruct? (/teach them about?) - Current condition - Specific impairments - Functional limitations or disabilities - Plan of care - Need for enhanced performance - Transition to a different role or setting - Risk factors for developing a problem or dysfunction - Need for health, wellness or fitness programs
question
PT's are responsible for coordination, communication, & documentation across...
answer
...all settings for ALL patients/clients.
question
T/F : Don't forget to write down what you educated your patient on!
answer
True! --> patient was educated on how to use the walker, how the walker was fit for her, safe hand placement on walker --> We explain the medical condition well (the patient was educated on their condition)
question
Patient/Client related instruction ---> Who do we instruct?
answer
Patients/Clients Family members Significant others Caregivers --> - Important to educate family members so that they can help the patient
question
Patient Management: Outcomes
answer
- Outcomes are the results of implementing the intervention that indicate the impact of functioning - What did we change in the patient's ICF model? Documentation is critical. (e.g. G-codes) --> We need to prove that we work and that intervention is making a difference in someone's life Ex. went from doing 2 sit-stands to 5
question
G-codes?
answer
G-codes: Medicare says you need to show how you are impacting function. They created these g-codes to prove that patients are improving. Result of documenting poorly.
question
Patient Management: Episode of Care
answer
All PT services that are: - Provided by a PT or under the supervision of a PT - Provided in unbroken sequence - Related to PT interventions for a given condition (acute care to outpatient care for a THA)
question
Patient Management: "Plan of Care" includes...
answer
- Anticipated goals and outcomes - Predicted level of optimal improvement (predictions in the guide are intended to encompass 80% of the patients within a practice pattern) - Interventions to be utilized - Frequency and duration of intervention - Anticipated discharge plans
question
Patient management: Coordination, communication, & documentation
answer
- Ensures patient receive appropriate, efficient, comprehensive, and effective quality of care. - PT's are responsible for coordination, communication, & documentation across all settings for ALL patients/clients.
question
Patient Management: Discharge
answer
The process of discontinuing interventions in a single episode of care, *when anticipated goals and outcomes have been achieved*.
question
Patient Management: Discontinuation
answer
The process of ending PT services during a single episode of care, when: - Patient declines continued intervention. - Patient is unable to demonstrate progress toward goals and outcomes. - Patient will no longer benefit from PT services.
question
Patient Management: "Episode of Care" may include:
answer
- Transfers between sites, within or across settings - Reclassification of a patient from one preferred practice pattern to another. Reclassification may alter the expected number of visits and alter the episode of care - If reclassification involves a condition or problem that is not related to the initial episode of care, a new episode of care may be initiated.
question
History of The Guide: How was the guide put together?
answer
1992: Florida chapter requested a document to help define practice patterns 1995: Part One approved by APTA and published in PT Journal 1997: Part Two completed and published in PT Journal 2001: 2nd edition of the Guide published.
question
History of the Guide: Part 1 and Part 2
answer
PART ONE: Overview of PT's as health professionals, elements of patient management, tests & measures, and interventions PART TWO: Preferred practice patterns for different conditions - musculoskeletal, neuromuscular, cardiovascular/pulmonary, integumentary ---> Created PT diagnoses. However, they weren't helpful. Long sentences that PT's didn't use
question
What is the intent of the guide? (The Guide (3rd edition))
answer
Description of practice - Outlines the role of the PT in a variety of practice settings - Describes the settings where PTs practice Standardizes terminology - Outlines the clinical decision-making process utilized to determine patient management. - Describes the examination and evaluation process - Explains how interventions are selected by physical therapists - Describes how outcome measures are utilized Resource for academia (faculty and students) Resource for clinicians
question
What doesn't the guide do?
answer
- Provide specific protocols - Serve as clinical guidelines - It is NOT a "cookbook" --> Doesn't tell you what to do step-by-step with a patient
question
Guide (2nd edition) Concepts
answer
- The Disablement Model is used in PT practice - PT's address the needs of patients across a continuum of settings - Five essential elements of patient management
question
Description of PT Practice (what is a PT)
answer
Physical therapists are health care professionals who help individuals maintain, restore, and improve movement, activity, and functioning, thereby enabling optimal performance and enhancing health, well-being and quality of life.



