Pharm SG 8 – Flashcards
Unlock all answers in this set
Unlock answersquestion
type 2 diabetes
answer
-An FPG concentration of 126 mg/dL or higher on more than one occasion -An elevated HbA1c - High BMI with central obesity -Age greater than 40 -Family history of diabetes -Mexican American descent. hyperglycemia (including increased thirst and lethargy), recurrent monilial infections, hypertriglyceridemia, and indications of CVD (hypertension) also are typical in patients with type 2 diabetes
question
current criteria for diagnosis of diabetes mellitus?
answer
*HbA1C >_ 6.5%* or *FBG >_ 126 [7mM] *(no caloric intake in 6hrs) or *2hr Plasma Glucose >_ 200 (11.1)* during OGTT [75g glucose] or *symptoms + RPG >_ 200 (11.1) *
question
Target goals for blood glucose, blood pressure, lipids
answer
-HbA1C < 7%. -FPG < 130 mg/dL -Postprandial glucose concentrations < 180 mg/dL -Blood pressure < 130/80 mm Hg -LDL 40 mg/dL for men and > 50 for women -Triglycerides < 150 mg/dL
question
Step by Step Type 2 Diabetes management goals: -HbA1C < 7%. -FPG < 130 mg/dL -Postprandial glucose concentrations < 180 mg/dL
answer
*Step 1* - Metformin Therapy + Lifestyle Intervention *Step 2* - If lifestyle intervention and metformin fail to achieve HbA1C consider adding insulin] *Step 3* - If we do not meet glycemic goals we start or intensify insulin tx. Insulin is the most effective medication in lowering glycemia. It can decrease any level of elevated HbA1C to, or close to, the therapeutic goal. Unlike the other blood glucose-lowering medications, there is *no maximum dose of insulin beyond which a therapeutic effect will not occur* Large doses may be needed - 1unit/kg or greater
question
Note that in step 2
answer
The consensus is to choose either insulin or a sulfonylurea other than glyburide or chlorpropamide (glyburide and chlorpropamide are associated with a greater risk of hypoglycemia than newer sulfonylureas such as glimepiride and glipizide.)
question
What are the criteria for instituting insulin therapy in type 2 diabetes
answer
Insulin therapy is usually tried after lifestyle modification and other antihyperglycemic agents have failed We use insulin as Initial Therapy only when: -HbA1c > 10 -FPG> 250 -RPG >300 consistently -Ketonuria, polyuria, polydipsia, weight loss are present After the symptoms are relieved and glucose levels decrease, oral agents can be tried, and insulin may be discontinued if oral agents are sufficient to control blood glucose
question
How should *metformin therapy* be monitored Advantage: Weight Loss Insulin: - or decreases AE: GI side effects. Rarely lactic acidosis. Contraindicated with renal insufficiency.
answer
perform* SMBG and have an HbA1c test* performed quarterly until she achieves consistent values <7%. Initially, it is important to follow potential GI adverse effects. Although *lactic acidosis* is unlikely, The patient should be warned to bring to the attention of her physician any sudden symptoms of shortness of breath, weakness, and malaise. -Initial and periodic monitoring of hematologic parameters (e.g., hemoglobin/hematocrit and red blood cell indices) and renal function (serum creatinine) should be performed, at least on an annual basis
question
Type 1 Diabetes
answer
consistent with type 1 diabetes, in particular, include the relatively acute onset of symptoms in association with a major life event (moving away from home), ketones in the urine, negative family history, and a relatively young age at onset.
question
Goals of Therapy in Type 1 Diabetes
answer
prevention of acute and chronic complications. Lowering blood glucose concentrations through intensive insulin therapy in persons with type 1 diabetes slows or *prevents the development of microvascular complications*. The ADA recommends an HbA1c goal of less than 7% for patients in general and an individual goal as close to normal as possible ( insulin adjustments, education, clinical support Goal : Hba1c as close to normal with rare hypoglycemic complications
question
A physiological insulin regimen
answer
In the nondiabetic individual, the pancreas secretes boluses of insulin in response to snacks and meals. Between meals and throughout the *night*, the pancreas secretes *small amounts of insulin* that are sufficient to *suppress lipolysis and hepatic glucose output (basal insulin)*.
question
Name the 2 methods of insulin therapy that are used to achieve similar physiological releases of insulin
answer
1 - *Basal-Bolus Insulin Regimens *consisting of once to twice daily doses of basal insulin coupled with pre-meal doses of rapid or short-acting insulin. 2- *Insulin Pump Therapy* (previously referred to as "continuous subcutaneous infusion of insulin")
question
Basal-Bolus Insulin Regimens (Multiple Daily Injections)
answer
Basal dose comprises 50% of daily dose Best mimic of physio = 1 time daily basal insulin of *glargine* or *detemir*@ morning or bedtime to provide basal insulin levels throughout the day alone with Regular (short act) or LISPRO/ASPART/GLULISINE (rapid) before meals
question
Insulin Pump Therapy (Previously "Continuous Subcutaneous Infusion Of Insulin")
answer
The use of an insulin pump is the most precise way to mimic normal insulin secretion. These systems are portable and designed to deliver various basal amounts of insulin over 24 hours as well as meal-related boluses For meal coverage, the rapid-acting insulin can be given 0 to 15 minutes before eating. The delivery of the bolus can be adjusted depending on the type of food eaten
question
Type 1 Diabetes Dosing 24 units = .5 unit / kg 12 of glargine as basal with 4 at each meal
answer
individuals with type 1 DM require 0.5 to 1.0 U/kg per day of insulin divided into multiple doses. Initial insulin-dosing regimens should be conservative. Approximately 40 - 50% of the insulin should be given as basal insulin. 1. The pre-breakfast (fasting) glucose is primarily determined by the prior bedtime basal insulin. 2. The pre-lunch glucose is a function of the morning rapid-acting insulin 3. The pre-dinner glucose is a function of the morning basal insulin or of the prelunch rapid-acting insulin. 4. The bedtime glucose is a function of the pre-dinner rapid-acting insulin.
question
The Somogyi Effect
answer
nocturnal hypoglycemia could lead to morning fasting hyperglycemia (posthypoglycemic hyperglycemia). It has been Proved it doesnt exist Thus, it appears that nocturnal hypoglycemia does not commonly cause clinically important morning hyperglycemia in patients with diabetes mellitus.
question
The most common cause of prebreakfast hyperglycemia
answer
*waning of the evening or bedtime insulin and/or the dawn phenomenon.* -reduced tissue sensitivity to insulin between 5 am and 8 am, due to spikes of growth hormone released hours before, at the onset of sleep. (not cortisol or catech) -occurs in nearly all diabetic patients
question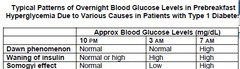
How would you differential diagnosis of pre-breakfast hyperglycemia
answer
self-monitoring of blood glucose at 3 am in addition to the usual bedtime and 7 am measurements. This is required for only a few nights, and when a particular pattern emerges from monitoring blood glucose levels overnight, appropriate therapeutic measures can be taken. - The dawn phenomenon shows an abrupt increase of blood glucose levels between 3 a.m. and 7 a.m. -Waning of exogenous insulin shows a gradual rise of blood glucose levels throughout the night between bedtime and 7 a.m. -If the blood glucose level shows hypoglycemia at 3 a.m., morning hyperglycemia may be due to the Somogyi effect.
question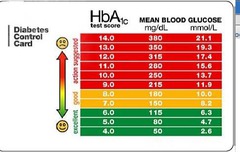
For 5 days straight we have 3 am blood glucose of 110-120 what does this suggest?
answer
Dawn Phenomenon -see table, its hyperglycemia
question
Treatment of Dawn Phenomenon/Waning of Insulin
answer
an increase in the evening dose of the basal insulin or shifting it from dinnertime to bedtime (or both) can be effective.
question
Treatment of Somogyi Effect
answer
Prebreakfast hyperglycemia due to the Somogyi effect can be treated by reducing the dose of either intermediate- or long-acting insulin analog at bedtime -dont go into hypoglycemia
question
Hypertension and diabetes A 5 mmHg reduction in mean diastolic BP can produce a 37% reduction in microvascular complications, and a 10 mmHg reduction in mean systolic BP reduces the risk of MI by 11% and death related to diabetes by 15%.
answer
Hypertension is a major risk factor for both CVD and microvascular complications.* In type 1 diabetes, hypertension is often the result of underlying nephropathy*, while in type 2 diabetes it usually coexists with other cardiometabolic risk factors. If HTN + diabetets: aggressive management -> weight loss + Na restrictuion + Stop Smoking + anti-HTNs Target BP under 130/80 ADA says BP check at every diabetes visit. If over 130/80 (either) you get BP checked another day. If its again over 130/80 confirms hypertension Um pretty sure this is wrong. PreHTN 120-139/80-89 HTN1 140-159/90-99 HTN2 160+/ 100
question
Management
answer
Patients with a systolic blood pressure 130-139 mmHg or a diastolic blood pressure 80-89 mmHg may be given lifestyle therapy alone for a maximum of 3 months, and then if targets are not achieved, patients should be treated with the addition of pharmacological agents. If 140+ or 90+ we add a pharmcological agent
question
Lifestyle mods for HTN
answer
Lifestyle therapy for hypertension consists of weight loss if overweight, DASH-style dietary pattern including reducing sodium and increasing potassium intake, moderation of alcohol intake, and increased physical activity
question
Meds for HTN 140+/90+
answer
Numerous studies have documented the effectiveness of ACEIs and ARBs in delaying the development and progression of nephropathy. Pharmacologic therapy for patients with diabetes and hypertension should include either an ACEI or an ARB. If one class is not tolerated, the other should be substituted. If needed to achieve results a thiazide diuretic should be added to those with an estimated glomerular filtration rate (GFR) (see below) ? 30 ml/min/1.73 m2 and a loop diuretic for those with an estimated GFR < 30 ml/min/1.73 m2.
question
If we give ACEi (lisinopril) what should be monitored?
answer
[K+ serum], [creatinine serum], BP for 2-4 weeks after start of ACEi therapy or when increasing dose creatinine slighly up due to small decrease in GFR (up to 35% safe + anticipated so keep them on)
question
Adults with diabetes should be screened annually for serum lipoprotein levels, including triglycerides, total cholesterol, LDL cholesterol, and HDL cholesterol
answer
A total cholesterol level of less than 200 mg/dL, triglyceride level <150 mg/dL, and LDL cholesterol levels maintained at 100 mg/dL or lower are acceptable. Use statins - recommended by ADA in patients over 40yr with 1 or more CVD risk factors -diet, exercise. Weight loss is associated with improvements in insulin sensitivity and glucose control, as well as a reduction in triglycerides, total cholesterol, and LDL cholesterol. Physical activity enhances weight loss and increases HDL cholesterol levels
question
Statins
answer
inhibit HMG-CoA reductase, a key regulatory enzyme for cholesterol biosynthesis. As a result, hepatic cholesterol synthesis declines, surface LDL particle receptors increase, and LDL cholesterol clearance increases -effects are dose dependent, higher doses work more - lower LDL + Trigly, slight increase HDL
question
Statins AE
answer
Biochemical abnormalities in liver function have occurred with the statins. Therefore, it is prudent to evaluate liver function and measure serum transaminase levels periodically Myopathy and rhabdomyolysis (disintegration or dissolution of muscle) have been reported only rarely. In most of these cases, patients usually suffered from renal insufficiency or were taking drugs such as *cyclosporine, itraconazole, erythromycin, gemfibrozil, or niacin. Plasma creatine kinase levels should be determined regularly.*
question
beneficial cardiovascular pleiotropic effects of statins? Pleiotropic effects of a drug are actions other than those for which the agent was specifically developed
answer
Pleiotropic effects of statins include improvement of endothelial dysfunction, increased nitric oxide bioavailability, antioxidant properties, inhibition of inflammatory responses, and stabilization of atherosclerotic plaques. These and several other properties could act in concert with the LDL-lowering effects of statins to exert early as well as lasting cardiovascular protective effects.
question
What is the cause of diabetic gastroparesis? nausea, vomiting, early satiety, bloating, and postprandial fullness. These symptoms can be extremely troubling and result in poor quality of life. The goal of managing patients with DGP is to maintain adequate glycemic control, control upper GI symptoms, ensure adequate hydration and nutrition, improve gastric emptying, and prevent complications such as dehydration, malnutrition, and frequent hospitalizations
answer
autonomic neuropathy of the enteric nervous system --> impaired neural control of gastric function. Marked acute hyperglycemia relaxes the proximal stomach, suppresses the frequency, propagation, and contraction amplitude of antral pressure waves, and stimulates phasic pyloric pressure waves, all of which retard gastric emptying.
question
Drugs for Gastroparesis
answer
prokinetic drugs may be required to control symptoms of diabetic gastroparesis. Several prokinetic drugs have been used successfully in managing the symptoms of gastroparesis. These agents include *metoclopramide, domperidone *(not available in the United States), and *erythromycin.*
question
Diabetic Neuropathy
answer
First line - TCA [NE/5-HT reuptake inhibitors] AE: TCAs is due to their relative affinities for muscarinic, H1, and ?1-adrenergic receptors. Use GABAPENTIN + PREGABALIN if TCAs cannot be tolerated or USE SNRIs [Duloxetine, Velafaxine] especially if depressed Miscellaneous Alternatives -Capsaicin (topical) - Lidocaine (transdermal patch) - Morphine (or equivalents) - Tramadol - Valproate
question
Tertiary Amines
answer
amitriptyline, imipramine) are associated with more severe anticholinergic effects than the secondary amines. Tertiary amines also have the greatest affinity for H1 and a1-adrenergic receptors, resulting in sedation and orthostatic hypotension, respectively
question
The secondary amines
answer
*desipramine and nortriptyline* are less likely to cause sedation, anticholinergic side effects, and orthostatic hypotension, than the tertiary amines



