Pharm: Anesthetics, muscle relaxants – Flashcards
Unlock all answers in this set
Unlock answersquestion
Anesthesia
answer
• The state of "general anesthesia" includes: • Analgesia • Amnesia • Loss of consciousness • Suppression of reflexes • Skeletal muscle relaxation Balanced Anesthesia • No single drug is capable of achieving all of the desired goals of anesthesia. • In balanced anesthesia, several drugs are used in combination to produce the anesthetic state. • The onset of inhalational agents is not rapid: patients are usually anesthetized with an IV agent. • Halogenated hydrocarbons are not good analgesics: a supplemental analgesic is required. • Neuromuscular blocking agents are used to provide paralysis adequate for surgical access. • INHALED ANESTHETICS •IV ANESTHETICS
question
Inhaled anesthetics
answer
• Gases --N2O • Volatile halogenated hydrocarbons: Halothane Enflurane Isoflurane Desflurane Sevoflurane Methoxyflurane • Used for the maintenance of anesthesia after administration of an IV agent. COMMON FEATURES • Increase perfusion of brain. • Cause bronchodilation. • Decrease minute ventilation. • Potency correlates with liposolubility. • Rate of onset inversely correlates to blood solubility. • Recovery is due to redistribution from the brain. • The actions of inhaled anesthetics are the consequence of direct interactions with ligand- gated ion channels. • Positive modulation of GABAA and glycine receptors. • Inhibition of nicotinic receptors.
question
IV Anesthetics
answer
Used alone or with other drugs to: • Achieve anesthesia • As components of balanced anesthesia • To sedate patients in ICUs who must be mechanically ventilated for long periods. IV anesthetics include: • Barbiturates • Propofol • Ketamine • Etomidate
question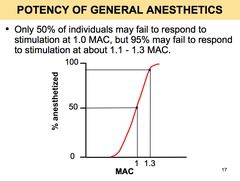
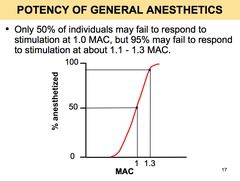
Potency of general anesthetics
answer
• Standard of comparison for potency of general anesthetics: Minimum alveolar concentration (MAC). • MAC is the concentration that results in immobility in 50% of patients when exposed to a noxious stimulus such as surgical incision. • MAC is expressed as % of the alveolar gas mixture. • MAC is low for potent anesthetics and large for less potent agents. • MAC gives no information about the slope of the dose-response curve. • In general, the slopes of the dose- response curves for inhalational anesthetics are steep. • MAC values are additive. • Nitrous oxide can be used as a "carrier" gas, decreasing the anesthetic requirement of other inhaled anesthetics. • 0.7 MAC of isoflurane and 0.3 MAC of nitrous oxide yield 1 MAC.
question
The Meyer-overton correlation
answer
• The potency of an anesthetic can be predicted from its liposolubility. • The oil:gas partition coefficient is a good measure of the liposolubility. • The potency of an anesthetic increases as its solubility in oil increases. • As ? lambda (oil:gas) increases, the MAC decreases.
question
Partition coefficients
answer
• The partition coefficient is the ratio of the concentrations of a compound in one solvent to the concentration in another solvent. • For example, an oil:gas partition coefficient of 19 means that the concentration of anesthetic in oil is 19-fold that present in the alveolar gas when the partial pressure of the anesthetic is identical at both sites.
question
Anesthetic induction
answer
• Anesthesia requires transfer of anesthetic from the alveolar air to the blood and then to the brain. • The rate at which a given concentration of anesthetic in the brain is reached depends on: • Solubility of the anesthetic • Its concentration in the inspired air • Pulmonary ventilation rate • Pulmonary blood flow • Concentration gradient of the anesthetic between arterial and venous blood.
question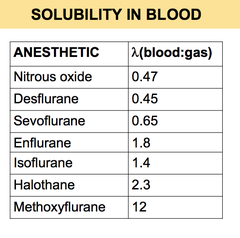
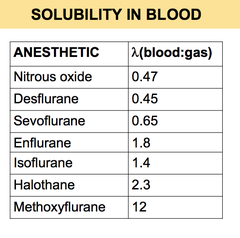
Solubility in blood
answer
• The blood:gas partition coefficient (?) is a useful index of solubility. • It defines the relative solubility of an anesthetic in the blood compared to air. • When an anesthetic with low solubility in blood diffuses from the lung into the arterial blood the arterial tension of the anesthetic rises quickly. • Conversely, if an anesthetic has high solubility in blood, more molecules of the anesthetic will dissolve in blood before the partial pressure changes significantly. • Consequently, the arterial tension of the gas increases less rapidly. • Therefore there is an inverse relationship between the blood solubility of an anesthetic and the rate of rise of its tension in arterial blood. • A low blood:gas partition coefficient determines a faster onset of anesthesia.
question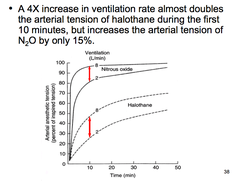
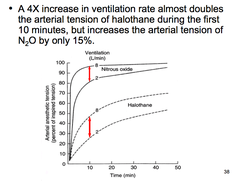
Ventilation rate
answer
• The rate of rise of anesthetic gas tension in arterial blood is directly dependent on both the rate and depth of ventilation. • But the magnitude of the effect depends on the blood:gas partition coefficient. • If the anesthetic has low blood solubility, an increase in pulmonary ventilation will cause only a slight increase in arterial tension • If the anesthetic has moderate or high blood solubility an increase in pulmonary ventilation will cause a significant increase in arterial tension.
question
Pulmonary blood flow
answer
• An increase in pulmonary blood flow (increased cardiac output) slows the rate of rise in arterial tension. • This is because increased pulmonary blood flow exposes a larger volume of blood to the anesthetic. • Blood "capacity" increases and tension rises slowly. Arteriovenous concentration gradient: • This is dependent mainly on uptake of the anesthetic by the tissues. • Uptake by tissues slows down the onset.
question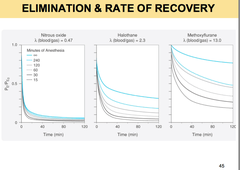
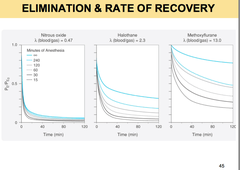
Elimination of inhalation anesthetics
answer
• Elimination of inhalational anesthetics is largely the reverse process of uptake. • For agents with low blood and tissue solubility, recovery from anesthesia mirrors anesthetic induction, regardless of the duration of anesthetic administration. • For agents with high blood and tissue solubility, recovery is a function of the duration of anesthetic administration. • This is because the anesthetic accumulated in fat will prevent blood (and therefore alveolar) partial pressures from falling rapidly.
question
Cardiovascular effects of inhaled anesthetics
answer
• Most inhaled anesthetics decrease blood pressure moderately. • Nitrous oxide is less likely to lower blood pressure than are other inhaled anesthetics. • Halothane, and to a lesser extent, isoflurane sensitize the myocardium to circulating catecholamines, which may lead to ventricular arrhythmias.
question
Respiratory effects of anesthetics
answer
• All volatile anesthetics are respiratory depressants: they reduce the response to CO2. • Nitrous oxide is the least depressant. • Most inhaled anesthetics are bronchodilators. • Halothane and sevoflurane are drugs of choice in patients with airway problems. • Desflurane is pungent.
question
CNS effects of anesthetics
answer
• Increase cerebral blood flow and therefore intracranial pressure. • Undesirable in patients who already have increased intracranial pressure because of brain tumor or head injury. • N2O increases blood flow the least. • Enflurane at high concentrations may cause tonic-clonic movements. • N2O has low anesthetic potency, but exerts marked analgesic and amnesic actions.
question
Other effects of anesthetics
answer
• N2O exchanges with nitrogen in air-containing cavities in the body. • N2O enters the cavity faster than nitrogen escapes. • Therefore, it increases the volume and/or pressure of the cavity. • N2O should be avoided in the following clinical settings: • Pneumothorax • Obstructed middle ear • Air embolus • Obstructed loop of bowel • Intraocular air bubble • Pulmonary bulla • Intracranial air
question
Hepatotoxicity of anesthetics
answer
Halothane • Some individuals exposed to halothane may develop a potentially severe and life-threatening hepatitis. • There is no specific treatment • Liver transplantation may be required.
question
Nephrotoxicity of anesthetics
answer
• Methoxyflurane has nephrotoxic potential. • Due to fluoride released during metabolism.
question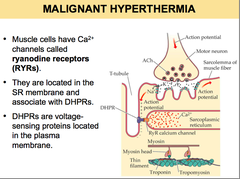
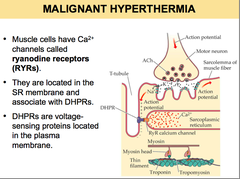
Malignant hyperthermia and anesthetics
answer
• Potentially fatal genetic disorder of skeletal muscle. • Triggered in susceptible individuals by volatile inhalation anesthetics (eg halothane) and depolarizing skeletal muscle relaxants, such as succinylcholine. • Transmitted as an autosomal dominant trait. • Incidence is about 1:12,000. • Malignant hyperthermia is one of the main causes of death due to anesthesia. • The malignant hyperthermia syndrome includes: • Tachycardia • Hypertension • Severe muscle rigidity • Hyperthermia • Hyperkalemia • Acidosis. • Malignant hyperthermia results from altered control of Ca2+ release from the SR. • In most cases, the syndrome is caused by a defect in the ryanodine receptor gene (RYR1). (after diagram): • In response to a depolarization, the DHPRs undergo a conformational change. • This opens RYRs, so that Ca2+ is released from the SR. • Abnormal RYR1 receptors trigger unregulated release of calcium from the SR, which may lead to an acute malignant hyperthermia crisis. • The increased Ca2+ concentration causes sustained muscle contraction which generates heat. • Accelerated levels of aerobic metabolism produce CO2 and deplete O2 and ATP. • A switch to anaerobic metabolism worsens acidosis with the production of lactate. • Energy stores get depleted. • Muscle fibers die leading to hyperkalemia and myoglobinuria. • Dantrolene: blocks Ca2+ release from the sarcoplasmic reticulum. • Measures to reduce body temperature and restore electrolyte and acid-base balance.
question
The caffeine-halothane muscle contracture test
answer
• The most reliable test to establish susceptibility to MH. • A muscle sample is removed from the thigh using anesthesia known NOT to trigger malignant hyperthermia. • Using a dissecting microscope, six to eight small muscle strips are prepared. • A muscle strip is placed in a muscle bath with physiological solution. • The strip is attached to an electrical stimulator which produces twitches every 10 seconds. • The strength of the contraction is measured.
question
Chronic toxicity of anesthetics
answer
Hematotoxicity • ProlongedexposuretoN2Odecreases methionine synthase activity and causes megaloblastic anemia. • Potentialoccupationalhazardforstaff working in poorly ventilated dental operating suites.
question
IV anesthetics
answer
Barbiturates Propofol Ketamine Etomidate
question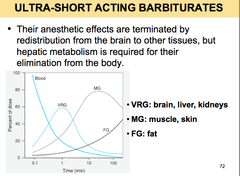
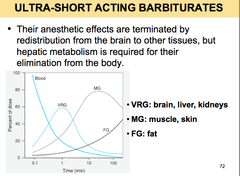
Ultra-short acting barbiturates
answer
Thiopental and Methohexital • Used for induction of anesthesia and for short surgical procedures.
question
Propofol
answer
• Most popular IV anesthetic. • Postoperative vomiting is uncommon. • Propofol is antiemetic. • Used for induction and maintenance of anesthesia. • Produces no analgesia. • Rapidly metabolized in the liver. • Causes hypotension. • Greater negative inotropic effects on the heart than other IV anesthetics.
question
Ketamine
answer
• Produces dissociative anesthesia, characterized by catatonia, amnesia and analgesia, with or without loss of consciousness. • Mechanism of action may involve blockade of NMDA receptors. • Only IV anesthetic that possesses both analgesic properties and the ability to produce CV stimulation. • Increases cerebral blood flow, oxygen consumption and intracranial pressure. • Causes disorientation, sensory and perceptual illusions, and vivid dreams ('emergence phenomena'). • Diazepam, midazolam, or propofol reduce the incidence of these phenomena.
question
Neuroepileptic-opioid combinations
answer
Neuroleptic-Opioid Combinations • When a potent opioid analgesic, such as fentanyl, is combined with a neuroleptic such as droperidol, neurolept analgesia is established. • Neurolept analgesia can be converted to neurolept anesthesia by the concurrent administration of 65% N2O in O2.
question
Anesthetics and adjuvants
answer
Adjuvant drugs provide additional effects that are desirable during surgery but are not necessarily provided by the general anesthetics. • Benzodiazepines. For their anxiolytic and anterograde amnesic properties. • Opioids. For analgesia. • Neuromuscular blockers. To achieve muscle relaxation. • Antiemetics, eg ondansetron. To prevent possible aspiration of stomach contents. • Antimuscarinics, eg scopolamine • For its amnesic effects • To prevent salivation and bronchial secretions • To protect the heart from bradycardia caused by inhalation agents and neuromuscular blockers.
question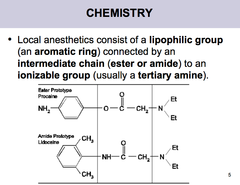
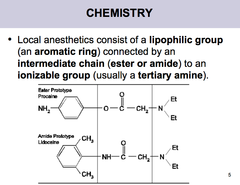
Local Anesthetics
answer
• Block nerve conduction of sensory impulses from the periphery to the CNS. • Abolish sensation (and in higher concentrations motor activity) in a limited area of the body without producing unconsciousness. • Ester links (as in procaine) are more prone to hydrolysis than amide links, therefore esters usually have a shorter duration of action. • Local anesthetics are weak bases with pK values around 8.0 - 9.0. • Therefore the larger fraction in the body fluids at physiologic pH will be the cationic form. • The cationic form is the most active form at the receptor site. • But the uncharged form is important for penetration of biologic membranes.
question
Local anesthetics- Prolongation of action by vasoconstrictors
answer
• Procedures that keep the drug at the nerve prolong the period of anesthesia. • Cocaine itself constricts blood vessels by potentiating the action of norepinephrine; therefore, it prevents its own absorption. • In clinical practice, preparations of local anesthetics often contain a vasoconstrictor, usually epinephrine. • Vasoconstrictors reduce systemic absorption of local anesthetics by decreasing blood flow > Neuronal uptake of the drug is enhanced. • Systemic toxic effects of the drug are reduced. • Also, in spinal anesthesia, epinephrine acts on ?2-adrenoceptors, which inhibit release of substance P. • The vasoconstrictor may cause untoward reactions: There may be delayed wound healing, tissue edema, or necrosis.
question
Metabolism and excretion of local anesthetics
answer
• Ester-linked local anesthetics are metabolized by tissue and plasma esterases (pseudocholinesterases). • Amide-linked local anesthetics are in general degraded by liver microsomal cytochrome P450.
question
Local anesthetics- MOA
answer
MECHANISM OF ACTION • Local anesthetics block voltage-gated sodium channels. • Local anesthetics bind to receptors near the intracellular end of the channel and block the channel. • Sufficient concentrations of a local anesthetic applied to a nerve fiber abolish action potentials.
question
Structure-activity characteristics of local anesthetics
answer
• The smaller and more lipophilic the molecule, the faster the onset. • Potency is also positively correlated with lipophilicity. • Liposoluble agents such as tetracaine, bupivacaine and ropivacaine are more potent and have longer durations of action.
question
Clinical pharmacology of local anesthetics
answer
• The choice of local anesthetics for a specific procedure is usually based on the duration of action required. • Procaine and chloroprocaine are short-acting • Lidocaine, mepivacaine, and prilocaine are intermediate-acting. • Tetracaine, bupivacaine, etidocaine and ropivacaine are long-acting.
question
Local anesthetics and toxicity
answer
• Ultimately, local anesthetics are absorbed from the site of administration. • If blood levels rise too high, effects on several organs systems may be observed.
question
CNS and local anesthetics
answer
• CNS stimulation: restlessness and tremor that may proceed to clonic convulsions. • CNS stimulation is followed by CNS depression. Death is usually due to respiratory failure. • More serious toxic reactions: due to convulsions from excessive blood levels. • When large doses must be given, premedication with a benzodiazepine provides significant prophylaxis against seizures.
question
peripheral nervous system and local anesthetics
answer
• At excessively high concentrations, all local anesthetics can be toxic to nerve tissue.
question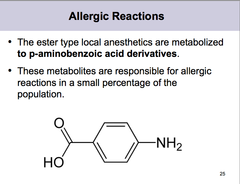
Allergic reactions and local anesthetics
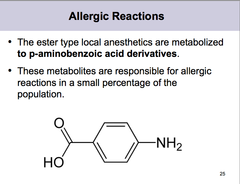
answer
• Amides are not metabolized to p-aminobenzoic acid. • Allergic reactions to agents of the amide group are extremely rare.
question
Management of AE in local anesthetics
answer
• Supportive treatment of the cardiovascular system includes IV fluids and, when appropriate, vasopressors (preferably those that stimulate the myocardium, such as ephedrine). • Convulsions may be controlled with oxygen and by IV diazepam or ultrashort-acting barbiturates, or succinylcholine. • If hypotension occurs, it should be controlled by vasoconstrictors given IM or IV. • Allergic reactions should be treated according to their severity. • Mild cutaneous reactions may be treated with diphenhydramine. • More serious reactions should be treated with epinephrine SC.
question
Drug interactions
answer
• Procaine is hydrolyzed in vivo to produce paraaminobenzoic acid (PABA), which inhibits the action of sulfonamides. • Large doses should not be administered to patients taking sulfonamide drugs.
question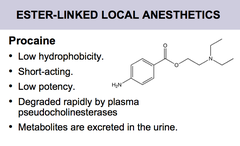
Procaine
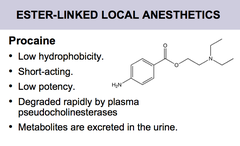
answer
• Primary use: infiltration anesthesia and dental procedures. • Occasionally in diagnostic nerve blocks. • The short-acting homolog of procaine, 2-chloroprocaine, is popular as an obstetric anesthetic.
question
Tetracaine
answer
Tetracaine • High hydrophobicity. • Long-acting. • High potency. • Metabolism is slow, despite its ester link, because it is released slowly from tissues into the bloodstream. • Mainly used in spinal and topical anesthesia. Ester-linked
question
Cocaine
answer
Cocaine • Only naturally-occurring local anesthetic. • Medium potency. • Medium duration of action. • Vasoconstrictive action due to inhibition of catecholamine reuptake. • This is the cause of cocaine's cardiotoxic potential. • Primary uses: ophthalmic anesthesia and as part of the topical anesthetic TAC (tetracaine, adrenaline ; cocaine). This mixture is sometimes used before suturing small cuts. • Because of concern about cocaine toxicity and/or addiction, alternatives such as EMLA are now used. Ester-linked
question
Lidocaine
answer
Amide linked Lidocaine • Most popular local anesthetic. • Moderate hydrophobicity. • Moderate potency. • Rapid onset of action • Medium duration of action. • Low pKa: large fraction of the drug is present in nonionized form at physiologic pH: fast diffusion through membranes and rapid block. • Used in infiltration, peripheral nerve block, epidural, spinal, and topical anesthesia. • It is also a Class I antiarrhythmic.
question
Prilocaine
answer
Amide-linked Prilocaine • Medium duration of action. • Pharmacological profile similar to lidocaine, except that it causes little vasodilation and can be used without a vasoconstrictor. • May cause methemoglobinemia.
question
Bupivacaine
answer
Amide-linked Bupivacaine • Long duration of action. • High hydrophobicity • High potency • Because of its cardiotoxicity at higher concentrations, bupivacaine is no longer as commonly used. • Racemic mixture of (R)- and (S)-stereoisomers. • The (S)-isomer (levobupivacaine) is less cardiotoxic than the (R)-isomer.
question
Ropivacaine
answer
amide-linked Ropivacaine • Clinical effects similar to those of bupivacaine but is less cardiotoxic.
question
EMLA
answer
Amide-linked EMLA (Eutectic Mixture of Local Anesthetic) • EMLA Cream is an emulsion in which the oil phase is a eutectic mixture of lidocaine and prilocaine in a ratio of 1:1 by weight. • The formulation allows the drugs to penetrate the skin more effectively than other anesthetic creams.
question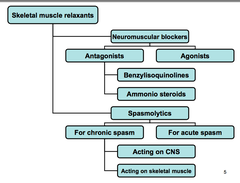
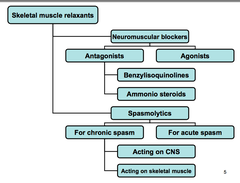
Skeletal muscle relaxants
answer
• Neuromuscular blockers. Used during surgical procedures and in ICUs to cause paralysis. • Spasmolytics. Used to reduce spasticity in a variety of neurologic conditions.
question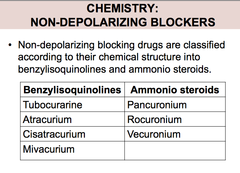
Neuromuscular blockers
answer
2 types: -antagonists (non-depolarizing blockers) -agonists (depolarizing blockers)
question
Depolarizing blockers
answer
• The depolarizing blocker succinylcholine is two acetylcholine molecules linked end-to-end.
question
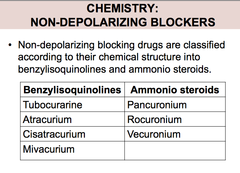
Nondepolarizing blockers
answer
They are competitive antagonists Tubocurarine is the prototype Their action can be overcome by increasing the concentration of acetylcholine in the synapse This can be achieved with neostigmine or edrophonium During anesthesia, nondepolarizing blockers first cause motor weakness Ultimately, skeletal muscles become totally flaccid and inexcitable to stimulation
question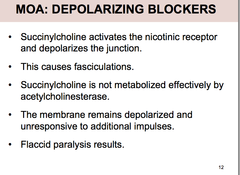
MOA depolarizing blockers
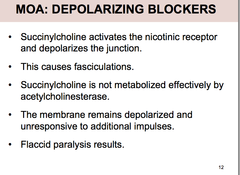
answer
The onset of neuromuscular blockade is very rapid, usually ;1 minute Because of its rapid hydrolysis by plasma pseudocholinesterase, duration of block is 5-10 minutes
question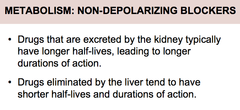
Metabolism of non-depolarizing blockers
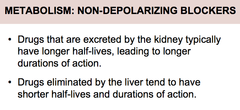
answer
• Atracurium is inactivated by hydrolysis by non- specific plasma esterases and by a spontaneous reaction. • No increase in half-life in patients with renal failure. • One of atracurium metabolites is laudanosine. • Laudanosine, may cause hypotension and seizures. Cisatracurium, a stereoisomer of atracurium forms much less laudanosine Cisatracurium also causes less histamine release Cisatracurium has largely replaced atracurium in clinical practice Mivacurium has short duration of action Hydrolysis by plasma butyrylcholinesterase is the primary mechanism for inactivation. Not dependent on liver or kidney. Rocuronium has the most rapid onset among nondepolarizing blockers Can be used as alternative to succinylcholine for rapid sequence intubation.
question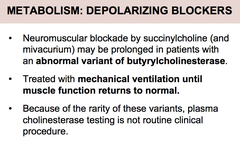
Metabolism: depolarizing blockers
answer
Succinylcholine has extremely short duration of action (5-10 minutes). Due to hydrolysis by butyrylcholinesterase
question
AE of non-depolarizing blockers
answer
Histamine release: Tubocurarine, and to a lesser extent, mivacurium and atracurium may release histamine Antihistamines are useful particularly if given before the neuromuscular blocker Ganglion blockade Tubocurarine may block nicotinic receptors of the autonomic ganglia and the adrenal medulla This causes hypotension and tachycardia Blockade of cardiac M2 receptors The amminosteroid pancuronium causes moderate tachycardia due to blockade of cardiac M2 recepotrs The cardiovascular effects of pancuronium are usually not a problem
question
AE Depolarizing blockers
answer
Succinylcholine activates all autonomic cholinoceptors: Nicotinic receptors in both sympathetic and parasympathetic ganglia Muscarinic receptors in the heart Bradycardia -due to activation of muscarinic receptors Can be prevented by thiopental, atropine, ganglionic blockers and non-depolarizing muscle relaxants Histamine release Succinylcholine has a slight tendency to release histamine Muscle pain -important postoperative complaint -due to damage produced by the unsynchronized contractions of adjacent muscle fibers Hyperkalemia -due to loss of tissue potassium during depolarization -risk is enhanced in pts with burns or muscle trauma -may lead to cardiac arrest or circulatory collapse Increased intraocular pressure- due to extraocular muscle contractions Increased intragastric pressure Fasciculations may increase intragastric pressure May causes emesis and aspiration of gastric contents Malignant hyperthermia -most cases are due to a combination of succinylcholine and a halogenated anesthetic Treatment: DANTROLENE CNS effects- no CNS effects due to their inability to cross the BBB
question
Drugs that enhance neuromuscular blockade
answer
Inhaled anesthetics Aminoglycosides Tetracyclines
question
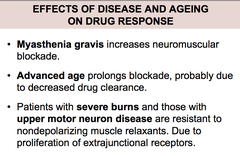
Effects of disease and aging on drug response
answer
Several diseases can decrease or increase the neuromuscular blockade caused by nondepolarizing muscle relaxants
question
Uses of neuromuscular blockers
answer
Surgical relaxation Control of ventilation Treatment of convulsions Prevention of trauma during ECT
question
Spasmolytic drugs
answer
Drugs for chronic spasm --Drugs that act in the CNS --Drugs that act on Skm Drugs for acute spasm
question
Drugs that act in the CNS
answer
--Drugs that act in the CNS -----Diazepam- facilitates action of GABA at GABAA receptors -----Baclofen- GABA agonist at GABAB receptors -----Tizanidine- agonist at alpha2 adrenoceptors in the CNS -----Gabapentin- increases GABA release -----Progabide- GABAA and GABAB agonist -----Glycine- inhibitor amino acid neurotransmitter -----Idrocilamide and riluzole- new agents for the tx of ALS. MOA may involve inhibition of glutamatergic transmission in the CNS
question
Drugs that act on Skeletal muscle
answer
--Drugs that act on Skm -----Dantroline-interferes with the release of Ca2+ by binding to the ryanodine receptor in the SR of skeletal muscle (Also used in malignant hyperthermia) -----botulinum toxin- now finding increased application in the treatment of more generalized spastic disorders, eg cerebral palsy