Patho Ch 1 – Flashcards
Unlock all answers in this set
Unlock answersquestion
Cytoplasm/protoplasm
answer
colourless, viscous liquid containing water, nutrients, ions, dissolved gases and waste products: where the cellular work takes place.
question
Organelles
answer
internal cellular structures that perform the work that maintains the cell's life.
question
Nucleus
answer
control centre of the cell, contains all the genetic information and is surrounded by a double membrane.
question
Cell membrane
answer
the semipermeable membrane containing the cell and its components.
question
Lipid bilayer
answer
fatty, double membrane that makes up the cell membrane.
question
Selectively permeable
answer
Ability of the cell to allow passge of some substances in and out of the membrane, allows the cell to maintain homeostasis.
question
Enzymes
answer
Proteins that facilitate chemical reactions in cells.
question
Glucose
answer
Sugar molecule that provides energy.
question
Electrolytes
answer
Chemicals that are charged when dissolved in water, conductors.
question
Diffusion
answer
The movement of solutes from an area of higher concentration to an area of lower concentration.
question
Osmosis
answer
The movement of a solvent or water through a semipermeable membrane from an area of low solute concentration to an area of high solute concentration. (solvent=liquid, solute= dissolved particles)
question
Osmotic pressure
answer
The tendency of water to move by osmosis.
question
Lysis
answer
cell bursting
question
Crenation
answer
cell shrinking
question
Facilitated diffusion
answer
The movement of substances from an area of lower concentration to an area of higher concentration with the assistance of a carrier molecule.
question
Active transport
answer
The movement of a substance from an area of lower concentration to an area of higher concentration, against a concentration gradient.
question
Endocytosis
answer
The process of bringing a substance into a cell.
question
Phagocytosis
answer
Cell eating, solid particles.
question
Pinocytosis
answer
Cell drinking.
question
Exocytosis
answer
The release of materials from the cell.
question
Proliferation
answer
The regulated process by which cells divide and reproduce.
question
Mitosis
answer
Cell division, cell divides into two seperate cells, 4 phases, prophase, metaphase, anaphase and telophase.
question
Prophase
answer
Chromomsomes condense and the nuclear membrane disintegrates.
question
Metaphase
answer
The spindle fibres attach to centromeres and the chromosomes align.
question
Anaphase
answer
The chromosomes seperate and the sister chromatids move to opposite poles.
question
Telophase
answer
The sister chromatids reach opposite poles adn the nuclear envelope begins to reform.
question
Meiosis
answer
Cell division that occurs only in sperm and ova, reduces the chromosome number by half.
question
Differentiation
answer
The process by which cell become specialised in terms of cell type, structure, function and cell cycle.
question
Adaption
answer
Cells attempt to prevent their own death from environmental changes.
question
Atrophy
answer
Cells decrease in size and number because of decreased work demands on the cell, causes of atrophy include, denervation, endocrine hypofunction, inadequate nutrition and ischemia.
question
Hypertrophy
answer
Cells increase in size in an attempt to meet increased work demand, commonly seen in cardiac and skeletal muscle.
question
Hyperplasia
answer
An increase in the number of cells in an organ or tissue, for example, menstruation, liver regeneration, wound healing, and skin warts.
question
Metaplasia
answer
The process in which one adult cell is replaced by another cell type, usually initiated by chronic irritation and inflammation. Metaplastic changes can be seen in ciliary changes that occur in the respiratory tract because of chronic smoking or vitamin A deficiency. Does not lead to cancerous changes, however if the stimulus is not removed, concerous changes will likely occur.
question
Dysplasia
answer
Cells mutate into cells of a different size, shape, and appearence. Is reversible by removing the trigger, often precancerous cells. Reproductive and respiratory tracts are common sites because of their increased exposure to carcinogens.
question
Programmed cell death
answer
The process of eliminating unwanted dead cells. Cell death from an irreversible cell injury. Cell injury can occur because of physical agents (for example, mechanical forces, extreme temperature), chemical injury (for example, pollution, lead, and drugs), radiation, biologic agents (for example, viruses, bacteria, and parasites), and nutrirional imbalances.
question
Apoptosis
answer
Normal and controlled cell death, cells condense or shrink.
question
Necrosis
answer
Cell death following injury, disease or failure of blood supply, cells swell and burst.
question
Ischemia
answer
Decreased blood flow to tissues or an organ, causing a shortage of oxygen and nutrients needed cellular metabolism.
question
Liquefaction necrosis
answer
Occurs when caustic enzymes dissolve and liquefy necrotic cells, most common site is the brain because it contains a plentiful supply of these enzymes.
question
Caseous necrosis
answer
The necrotic cells disintegrate, but the cellular debris remains in the are for months or years, cottage cheese-like appearance. Most commonly pulmonary tuberculosis.
question
Fat necrosis
answer
Lipase enzymes break downintracellular triglycerides into free fatty acids, which then combine with Mg, Na, and Ca and form soaps. Opaque, chalky appearance.
question
Coagulative necrosis
answer
Results from an interruption in blood flow, the pH drops, acidosis, denaturing the cells enzymes. Most often occurs in the kidneys, heart, and adrenal glands.
question
Gangrene
answer
A from of coagulative necrosis, combination of impaired blood flow and bacterial invasion. Usually occurs in the legs, because of arteriosclerosis (arteries hardening) or in the gastrointenstinal tract.
question
Dry gangrene
answer
Bacterial presence is minimal and the skin has a dry, dark brown, or black appearance.
question
Wet gangrene
answer
Occurs with liquefaction necrosis, extensive damage by bacteria and white blood cells produces a liquid wound. Occurs in the extremeties and internal organs.
question
Gas gangrene
answer
Develops because of presence of Clostridium (an anaerobic bacterium). Potentially fatal. Bacerium releases toxins that destroy surrounding cells, infection spreads rapidly. The gas bubbles underneath the skin in bubbles.
question
Free radicals
answer
Injurious, unstable agents that can cause cell death, unstable atom with odd number of electrons. Free radicals have been linked to cancer and aging.
question
Neoplasm
answer
Tumor. When cellular proliferation goes wrong. A cellular growth does not respond to normal regulatory processes, usually because of mutation.
question
Cancer
answer
The disease state associated with a neoplasm/tumor. Rapid uncontrolled proliferation and a loss of differentiation.
question
Carcinogenesis
answer
The process by which cancer develops. Three phases, initiation, promotion, and progression.
question
Initiation
answer
Invovles the exposure of the cell to the substance or event that causes DNA damage or mutation. Chemical, viruses, or radiation. The mutation can become permanent and hence be passed on to future generations.
question
Promotion
answer
Mutated cells are exposed to factors that promote growth. Nicotin, hormones, or nitrates. Can be reversible. May occur just after initiation or years later.
question
Progression
answer
Tumor invades, metastasizes (spreads), and becomes drug resistant. Permanent or irreversible.
question
Oncogenes
answer
A gene that has the potential to cause cancer. Activate cell division and embryonic development.
question
Anaplasia
answer
The of cell differentiation that occurs with cancer.
question
Benign
answer
Type of neoplasm. Less anaplastic, differentiated tumors that are producing more rapidly than normal cells. Cause fewer problems. Benign cells are often encapsulated and unable to metatasize.
question
Malignant
answer
Type of neoplasm. More anaplastic, undifferentiated, nonfunctioning cells that are reproducing rapidly. Often penetrate surrounding tissue and spread to secondary sites.
question
Cancer: clinical manifestations
answer
Anemia (red blood cell deficiency), due to blood borne cancers, chronic bleeding, malnutrition, chemotherapy, or radiation. Cachexia (wasting, dramatic weight loss and muscle atrophy), due to malnutrition. Fatigue, due to parasitic nature of tumor, anemia, malnutrition, stress, anxiety, chemotherapy. Infection increased risk due to bone marrow depression, chemotherapy and stress. leukopenia (decrease in white blood cells/leukocytes) side effect of radiation and chemotherapy. Thrombocytopenia (low platelet levels) side effect of radiation and chemotherapy. Pain, due to tissue pressure, obstructions, tissue invasion, visceral stretching, tissue destruction and inflammation.
question
Cancer: diagnosis
answer
Specific to type of cancer. Diagnostic procedures may vary depending on type cancer. Purpose is to identify and establish cytology of cancer cells, and to determine the primary site and secondary sites, if any. Screening tests include x-rays, radioisotope scanning, computed topography scans, endoscopies, ultrasonography, magnetic resonance imaging, positron emission tomography scanning, biopsies, and blood tests. Blood tests may include tumor markers, (substances secreted by the cancer cells), for specific cancers.
question
Cancer: diagnosis Grading
answer
Maligant cancer cells are classified on the degree of differentation on a scale of 1 to 4, in order of clinical severity. For example, grade 1 are well differentiated, so less likely to cause problems because they are more like the original tissue. Grade 4 are undifferentiated, they are less like the original tissue are more probable to cause problems.
question
Cancer: diagnosis Staging
answer
TNM staging system, evaluates tumor size, nodal involvement, and metatastic progress.
question
Cancer: treatment
answer
Chemotherapy Radiation Surgery Targeted therapy Hormone therapy Immunotherapy Hyperthermia Stem cell transplants Photodynamic therapy Laser treatment Alternative therapies Goal of treatment may be curative, palliative, or prophylactic.
question
Curative
answer
eradicate the disease
question
Palliative
answer
treat symptoms to increase comfort
question
Prophylactic
answer
prevent the disease
question
Chemotherapy
answer
Involves the administration of a wide range of medications that destroy replicating tumor cells
question
Radiation
answer
The use of ionising radiation to cause cancercellular mutation and interrupt the tumor's blood supply. May be administered internally or externally.
question
Targeted therapy
answer
Uses drugs to identify and attack cancer cells.
question
Hormone therapy
answer
Administering specific hormones thst inhibit the growth of cancer cells.
question
Immunotherapy
answer
Administering specific immune agents (interleukins, interferons) to alter the host's biological response to cancer.
question
Hyperthermia
answer
Delivers heat to a small area of cells or part of the body to destroy tumor cells. Can increase the effectiveness of radiation, immunotherapy, and chemotherapy.
question
Stem cell transplants
answer
May include peripheral blood, bone marrow, or cord blood. Used to restore stem cells in bone marrow destroyed by disease or treatment.
question
Photodynamic therapy
answer
Specific drugs are combined with light to kill cancer cells.
question
Laser
answer
Used to shrink or destroy tumor.
question
Prognosis
answer
Patient's liklehood for surviving the cancer. Dependent on the cancer's ability to metstasize.
question
Remission
answer
Period when the cancer has responded to treatment and is under control.
question
Genetics
answer
The study of heredity.
question
Congenital defects
answer
Birth defects. Usually develop during the prenatal period and are apparent at birth or shortly after.
question
Genes
answer
Carry cellular instruction and information.
question
DNA deoxyribonucleic acid
answer
Long double-stranded chain of nucleotides.
question
Nucleotides
answer
Five-carbon sugar, a phosphate, and one of four nitrogen bases (ctyosine, thymine, guanine, adenine).
question
Autosomes
answer
22 sets of paired chromosomes.
question
Karyotype
answer
A representation of a person's individual set of chromosomes.
question
Phenotype
answer
Physical expression of genes.
question
Allele
answer
One gene with many variants.
question
Homozygous
answer
A person who has identical alleles of each chromosome.
question
Heterozygous
answer
A person who has different alleles of each chromosome.
question
Dominant
answer
More pwerful allele that is expressed.
question
Recessive
answer
Less influential allele.
question
Klinefelter's Syndrome
answer
Example of X-linked disorder.
question
Autosomal dominant disorder
answer
Single gene mutations that are passed from an effected parent to an offspring regardless of sex. Occur with both homozygous and heterozygous allele pairs. Homozygous pair will have a more severe expression of the disorder. Examples include Marfan sydrome and nuerofibromatosis.
question
Marfan Syndrome
answer
Autosomal dominant disorder. Degenerative, generalised disorder of the connective tissue.
question
Marfan syndrome: pathophysiology
answer
Condition results from a single gene mutation on chromosome 15, that leads to elastin and collagen defects.
question
Marfan syndrome: clinical manifestations
answer
Increased height. Long extremeties. Arachnodactyly, long spider-like fingers. Sternum defects, funnel chest or pigeon breast. Chest asymmetry. Spine deformaties, scoliosis or kyphosis. Flat feet. Hypotonia and increased joint flexibility. Highly arched palate, crowded teeth, small lower jaw. Thin, narrow face. Nearsightedness and lens displacement. Valvular defects. Coarctation of the aorta.
question
Marfan syndrome: complications
answer
Weak joints and ligaments that are prone to injury. Cataracts. Retinal detachment. Severe mitral regurgitation. Spontaneous pneumothorax (collapsed lung). Inguinal hernia.
question
Marfan syndrome: diagnosis/ diagnostics
answer
History and physical examination. Skin biopsy, would be positive for fibrillin. X-rays, would confirm skeletal abnormalities. Echocardiogram, would revel cardiac abnormality. DNA anlaysis for the gene.
question
Marfan syndrom: treatment
answer
Focuses on relieving symptoms. Surgical repair of aneurysms and valvular defects. Surgical correction of occular deformities. Steroid and sex hormone therapy to aid in closure of long bones. Beta-adrenergic blockers to limit complications from cardiac deformaties. Bracing and physical therapy for mild scoliosis, and surgical correction for severe cases.
question
Neurofibromatosis

answer
Autosomal dominant disorder. An inherited condition involving neurogenic ( nervous system) tumors that arise from Schwann cells and other similiar cells, 30% to 50% cases do occur spontaneously. 2 types. There is an increased incidence of learning disabilities and seizure disorders. Ocular problems, scoliosis, and bone defects.
question
Type 1 Neurofibromatosis
answer
Caused by a mutation on chromosome 17. Cutaneous legions that may include raised lumps, cafe au lait spots, and freckling.
question
Type 2 Neurofibromatosis
answer
Caused by a mutation on chromosome 22. Involves bilateral acoustic (cranial nerve 8) tumors that cause hearing loss.
question
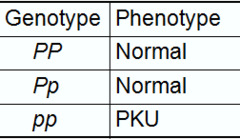
Autosomal recessive disorder
answer
Single gene mutation passed from an affected parent to an offspring regardless of sex, occur only in homozygous allele pairs. Those with heterozygous pairs are carriers only and display no symptoms. Early onset, e.g. Tay-Sachs disease and phenylketonuria (PKU).
question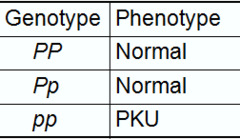
Phenylketonuria PKU
answer
Autosomal recessive disorder. Mutation on chromosome 12 that creates a deficiency of the enzyme, phenlalanine hydroxylase. Leads to central nervous system damage through toxic levels of phenylalanine in the blood. If untreated leads to severe intellectual diability. Newborns are routinely screened for PKU because symptoms develop slowly and can go undetected.
question
PKU Phenylketonuria, clinical manifestations
answer
Failure to meet milestones Microcephaly Progressive neurological decline Seizures Hyperactivity Electrocardiograph (EKG) abnormalities Learning disability Mousy-smelling urine, skin, hair, and sweat Eczema
question
PKU Phenylketonuria, treatment
answer
Consumption of a diet low in phenylalanine Special infant formulas. Avoid proteins Minimise starches
question
Tay-Sachs disease
answer
Autosomal recessive disorder Caused by defective gene on chromosome 15, effects those of Jewish decent. 1 in 27 is a carrier. Deficiency or absence hexosaminidase A, an enzyme that metabolises certain lipids called gangliosides. Lipids accumulate in lysosomes of nerve cells and progressively destroy and demyelinate nerve cells. Progressive motor and nerve deterioration, causing death by 5 years old.
question
Tay-Sachs disease, clinical manifestations
answer
Occur at 3 to 10 months Exaggerated Moro reflex (startle reflex) at birth Apathy to loud sounds by 3 to 6 months old Inability to sit up, lift head, or grasp objects Difficulty turning over Progressive vision loss Deafness and blindness Seizure activity Paralysis Spasticity Pneumonia
question
Tay-Sachs disease, treatment
answer
Diagnosed by history and physical, deficient serum and amniotic hexosaminidase A levels. No cure. Treatments are supportive. Parenteral nutrition (tube feeding) pulmonary hygiene (suctioning and postural drainage) Skin care Laxatives Psychological counseling
question
Sex-Linked disorders
answer
On the sex chromosomes. Most are X-linked. Females are frequently carriers of the trait (2 x chromosomes) May be recessive or dominant. E.G. Fragile X syndrome
question
Fragile X syndrome
answer
X-linked dominant disorder Failure to express a protein necessary for neural tube development.
question
Fragile X syndrome, clinical manifestations
answer
Intellectual, learning and behavioural disabilities Prominent jaw and forehead Long, narrow face with long or large ears Connective tissue abnormalities Large testes Hyperactivity Seizures Speech and language delays Tendency to avoid eye contact
question
Fragile X syndrome, treatment
answer
Diagnosis, positive genetic test No cure Control of individual symptoms Genetic counseling for those with a positive family history Behavioural and psychological support Physical, speech and occupational therapy
question
Multifactorial disorders
answer
Interaction between genes and environment factors May be present at birth, cleft palate Expressed later in life, hypertension
question
Envirinmental factors
answer
Teratogens i.e. infections, chemicals, or radiation
question
Cleft lip and cleft palate

answer
May occur together or seperately Develop in 2nd month of pregnancy Facial structures do not fuse properly Maternal smoking and diabetes are risk factors More prevalent in Native Americans and Asian Americans May be unilateral or bilateral deformities
question
Cleft lip/palate, clinical manifestations
answer
Obvious at birth can be detected with a prenatal ultrasound
question
Cleft lip/palate, treatment
answer
Surgery Speech therapy and feeding devices
question
Chromosomal disorders
answer
Result from alteration in chromosomal duplication or number. Environmental influence in utero ( maternal age, drugs, infections) Trisomy 21 Monosomy X Polysomy X
question
Trisomy X/ Down syndrome
answer
Sponateous chromosomal mutation 3 copies of chromosome 21 Risk increases with greater parental age and environmental teratogen exposure
question
Trisomy X/ Down syndrome, clinical manifestations
answer
Hypotonia Distinctive facial features (low nasal bridge, epicanthic folds, protruding tongue, low-set ears, small open mouth) Single crease on the palm, simian crease White spots on the iris Intellectual disability Congenital heart defects Strabismus and cataracts Poorly developed genetalia Delayed puberty Early death can occur due to cardiac and pulmonary complications Increased susceptability to leukemia and infections Four-dimensional ultrasounds, amniocentesis, and serum hormone levels for detection
question
Trisomy X/ Down syndrome, treatment
answer
No cure Symptom and complication management
question
Monosomy X/ Turner's syndrome

answer
Deletion of part or all of an X chromosome Effects only females Gonadal streaks instead of ovaries Do not menstruate
question
Monosmy X/ Turner's syndrome, clinical manifestations
answer
Short stature Lymphadema of the hands and feet Braod chest with widely spaced nipples Low-set ears Small lower jaw Drooping eyelids Increased weight Small fingernails Webbing of the neck Coarctation of the aorta Horseshoe kidney Visual disturbances Ear infections Hearing loss Reduced bone mass, which increases the risk for fractures
question
Monosomy X/ Turner's syndrome, treatment
answer
Female sex hormones to promote development of secondary sex characteristics and skeletal growth. Growth hormones. Identification is often delayed until late childhood early adolescence, if clinical presentation is more subtle. Chromosomal analysis can confirm Early treatment minimises problems and complications.
question
Polysomy X/ Klinefelter's syndrome

answer
Extra X chromosome XXY chromosome Male Apparent at puberty when testicles fail to mature Infertile
question
Polysomy X/ Klinefelter's syndrome, clinical manifestations
answer
Small penis, prostrate gland, and testicles Sparse facial and body hair Sexual dysfunction Gynecomastia (breasts) Long legs with a short, obese trunk Tall stature Behavioural problems Learning disabilities Increased incidence of pulmonary disease and varicose veins. Can develop osteoporosis and breast cancer.
question
Polysomy X/ Klinefelter's syndrome, treatment
answer
Hormone levels and chromosomal testing, diagnosis Male hormone replacement to promote secondary sex characteristics. Mastectomy in cases of gynecomastia



