Lecture 6 Respiratory Physiology, Pathophysiology and Anesthesia Management – Flashcards
Unlock all answers in this set
Unlock answersquestion
Which gas law explains the mechanics of breathing?
answer
Boyle's: contraction of the muscles? intra thoracic pressure and ?volume of thoracic cavity
question
Which muscles contract during normal breathing?
answer
Diaphragm ; external intercostals
question
How can only half the diaphragm become paralyzed?
answer
Two domes of the diaphragm separate the abdominal ; thoracic cavities, phrenic nerve injury results in paralysis on only that side.
question
How far does the diaphragm descend during normal breathing? Forceful?
answer
Normal: 1-2 cm Forceful: 10 cm For air to move into the alveoli pressure must be less than atmospheric pressure.
question
What is lung compliance?
answer
Defined as the change in volume divided by the change in pressure. V/P.
question
What is static compliance?
answer
Pressure/volume relationship for a lung when air is not moving. ?: any condition making lungs difficult to inflate, fibrosis, ARDS, obesity, external compression ?: emphysema as elastic tissue is lost, problem will be DEflating lungs
question
What is plateau pressure?
answer
Pressure at end-exhalation, can observe during inspiratory pause on ventilator.
question
What is static compliance?
answer
TV/ (Plateau pressure-PEEP) Normal: 60-100 ml/cm H?O
question
What is dynamic compliance?
answer
TV/ (PIP- PEEP) Compliance of the air in the lung while moving.
question
What forces are responsible for emptying of the lung dying exhalation and have a large role in determination of lung compliance?
answer
lung elastic recoil, surfactant also causes elastic recoil
question
What does LaPlace's Law state?
answer
If surface tension (T) is constant, pressure (P) would ? as radius (r) ?.
question
Do the lungs follow LaPlace's Law?
answer
No, as alveolar radius ?, surface tension also ? so that pressure remains the same. This occurs because of surfactant.
question
What is the role of surfactant in the lungs?
answer
Surfactant will ? the surface tension in the small alveoli, preventing alveolar collapse.
question
What is the resting end-expiratory point?
answer
Outward recoil of the chest wall is balanced by the inward elastic recoil of the lungs.
question
What is Reynold's number?
answer
Predicts when flow will be laminar or turbulent. 4000 turbulent Re= pvd/? (pg 567)
question
Resistance to laminar flow follows what law?
answer
Pousielle's, viscosity, length, distance. Doubling radius decreases resistance 16 times.
question
What amount of O? is utilized by ventilatory muscles in eupneic breathing?
answer
; 5%
question
What are the two major categories of lung disease?
answer
Obstructive: expiratory flow rates ? Restrictive: ? lung volumes ; lung compliance
question
The amount of air that enters ; leaves the body with each breath and contains ?500ml air is?
answer
Tidal volume Vt ? 500ml
question
Equals the respiratory rate multiplied by Vt. RR x Vt= ?
answer
Minute volume MV
question
What is the volume of air remaining in the lungs after maximum expiration called?
answer
Residual volume RV ? 1200ml
question
What is the maximum volume of air inspired from the resting end-expiratory level called?
answer
Inspiratory reserve volume IRV?3000
question
What is the maximum volume of air expired from the resting end-expiratory level called?
answer
Expiratory reserve volume IRV? 1100
question
What is the sum of the four basic lung volumes? IRV+Vt+ERV+RV=
answer
Total Lung Capacity TLC? 5800 Volume of air in the lungs after maximum inspiration (the sum of all volume compartments)
question
What is the maximum volume of air inspired from the end-expiratory level? IRV + Vt=
answer
Inspiratory Capacity IC? 3500
question
What is the maximum volume of air expired from the maximum inspiratory level? IRV+Vt+ERV=
answer
Vital Capacity VC? 4500
question
What is the maximum volume of air remaining in the lungs at the end expiratory level? RV+ERV=
answer
Functional Residual Capacity FRC ? 2300
question
What is the normal respiratory pressure in eupneic breathing? Maximal inspiration ; expiration?
answer
-1 to +1 -90 to ;100
question
What is the volume of conducting airways called?
answer
Dead space, no active gas exchange, ?2ml/kg
question
What are alveoli that are ventilated but not perfused?
answer
Alveolar dead space
question
Alveolar dead space + anatomic dead space=
answer
Volume of dead space % VDS= (PaCo?-PECo?)/ PaCo?
question
What is the respiratory quotient?
answer
Ratio of the amount CO? produced to quantity of O?
question
What two sources supply the lungs with blood?
answer
1- bronchial arteries 2- pulmonary arteries
question
What is the perfusion to zone 1?
answer
Dead space, ventilated but NOT perfused, upper part of lung, alveolar pressure is ;PAP
question
What is the perfusion to zone 2?
answer
Variable flow between vasculature ; alveolar pressure.
question
What is the perfusion to zone 3?
answer
Continuous blood flow, pulmonary ; venous pressure are ; alveolar pressure.
question
Pulmonary Edema
answer
Capillary leak overcomes the compliance of interstitial space and fluid begins to pass to alveoli.
question
How do you treat the occasional negative pressure pulmonary edema that occurs during emergence after extubation?
answer
O?, maintain patent airway, CPAP, fluid therapy to restore depleted intravascular volume.
question
Ventilation is usually 4L/ minute and pulmonary blood flow is usually 5L/minute. What is the V/Q (ventilation/perfusion) ratio?
answer
0.8
question
Which portion of the lungs are generally more compliant?
answer
Dependent regions, non-dependent portions are tented open and less compliant.
question
What are some common causes of V/Q mismatch?
answer
Pulmonary embolus, very high airway pressure, very low cardiac output, airway obstruction, alveolar collapse, pneumonia.
question
Effect of anesthesia on respiratory physiology
answer
-Moving from upright to supine ? FRC - 10% shunt from ? CO, atelectasis -inhaled anesthetics ? effectiveness of hypoxic pulmonary vasoconstriction, ? PaO? ?A-a gradient -Gases bronchodilate - GA ? ventilatory response to CO? ; hypoxia
question
Diffusivity is?
answer
Solubility/ ?molecular weight CO? heavier but 24 times more soluble than O?
question
What are the two ways oxygen can be transported in the blood?
answer
1-physical: dissolved in blood 2- chemical: bound to HGB
question
What does hemoglobin do?
answer
HGB: rapidly ; reversibly binds oxygen, allowing oxygen to be released into the tissues
question
What is hematocrit?
answer
Ratio of volume of blood cells: total volume of blood HGB level of 10g/100ml= 30% HCT Man: HCT 45%, HGB 15 Woman: HCT 39% HGB 13
question
What does the oxyhemoglobin Dissociation Curve show?
answer
Relationship between the PO? of the plasma and the percentage of HGB saturation.
question
What causes shifts to the LEFT of the oxyhemoglobin dissociation curve?
answer
-hypocapnia - ? temperature - alkalosis ?pH - ? 2,3 diphosphoglycerate Results i an increased affinity for HGB for O?
question
What causes shifts to the RIGHT of the oxyhemoglobin dissociation curve?
answer
- hypercapnia - ? temperature -acidosis ? pH (? CO?) - ? 2,3 diphosphglycerate Results in a decreased affinity of HGB for O?
question
What is the P???
answer
PaO? at which 50% of HGB is saturated
question
What is the normal P?? in an adult?
answer
P??= 26-27 mmHG HGB curve to right= ? P?? HGB curve to left= ? P??
question
What is methemoglobinemia? How is it treated?
answer
Iron in ferric, Fe³, instead of norma ferrous, Fe² state. HGB doesn't combine with O? in ferric state. Causes: nitrates, prilocaine Treat: O? therapy & methylene blue
question
What are the three ways blood can transport CO??
answer
1- physical solution 5-10% 2- chemically combined with amino acids of blood proteins 5-10% 3- bicarbonate ions 80-90%
question
What is the Haldane effect?
answer
Blood with oxygenated HGB: right shift Blood with deoxygenated HGB: shift left Allows blood to load more CO? at the tissues where more deoxygenated HGB is present and unload at the lungs.
question
How does the respiratory system work to maintain body pH?
answer
Works along with the kidneys and the buffer systems to balance the acids & bases of the blood. Respiratory system can rapidly compensate for metabolic acidosis or alkalosis by changing alveolar ventilation. -Changes in the blood H ion content affect chemoreceptors - Chemoreceptors ? or ? alveolar ventilation - PaCO? is altered within minutes.
question
What are volatile acids?
answer
-Exhaled CO? from lungs - 24,000 mEq/day, excreted through lungs -50 mEq from food, excreted by kidneys
question
How is respiratory alkalosis or acidosis treated in the mechanically ventilated patient?
answer
? rate for alkalosis ? rate for acidosis
question
Why shouldn't you give bicarbonate in respiratory acidosis?
answer
Bicarbonate can dissociate to CO? worsening acidosis.
question
What generate the spontaneous respiratory rhythm?
answer
Medullary respiratory center (under floor of 4th ventricle)
question
What centers does the pons contain?
answer
Apneustic: lower pons Pneumotaxic: upper pons
question
What are three respiratory reflexes elicited by stretch receptors?
answer
Hering Breur inflation: large ; small airways- cease respiration, Hering Breur deflation: J receptors, hyperpnea Paradoxical reflex of Head: stretch receptors in lung, inspiration (newborn)
question
What are J receptors?
answer
Vascular receptors that initiate lung responses "Juxtapulmonary capillary"
question
What two important inputs are the primary chemical control of breathing?
answer
Arterial Cerebral Spinal Fluid: not directly exposed to arterial blood due to BBB, but CO? is rapidly diffusible through BBB, so changes transmitted in ?2 minutes
question
What physical findings are found in the COPD patient?
answer
-Pulsus paradoxus in 2/3 -? in CO from ?catecholamine release - Enhanced HR response -? GFR, renal plasma flow
question
What are the hallmark signs of COPD?
answer
-Exercise limitation - Chronic productive cough
question
What are the characteristics of someone with chronic bronchitis AKA "blue bloater"?
answer
- overweight, dusky extremities - PaO? 45 -cor pulmonale - copious sputum ; cough - cardiomegaly
question
What are the characteristics of someone with chonic emphysema AKA "pink puffer"?
answer
- thin, emaciated, anxious - PaO? ;60 - PaCO? normal - dyspnea - small heart, low flat diaphragm
question
Preoperative Evaluation of the COPD patient
answer
- Supplemental O? if PaO² ; 60 or cor pulmonale - Assess for ? respiratory effort, altered breathing, abnormal heart sounds, productive cough -B agonists are mainstay treatment
question
Anesthesia management ; COPD
answer
- Regional Anesthesia: may be safer than GA, do not use above T6, risk of ? expiratory reserve volume -GA ? A:a difference -Muscle relaxant ?20% FRC
question
What are some respiratory considerations when COPD patient under GA?
answer
- If N?O is used bullae may enlarge ; rupture, contraindicated - Slower diffusion times cause longer induction ; emergence - Require ? Vt -Use caution with PEEP, PEEPe ; PEEPi decreases work of breathing - May require longer mechanical ventilation
question
Postoperative care in COPD
answer
- Encourage ambulation - IS with peak inflation for 3-5 seconds reexpands alveoli
question
Asthma is defined as...
answer
chronic inflammation disorder of the airways. - bronchoconstriction - hyper-irritability of tracheobronchial tree - air-way remodeling - immune mediated inflammatory response
question
Key hallmarks of asthma are..
answer
- Recurrent wheezing - Dyspnea/tachypnea -Cough -Chest tightness -Symptoms worse with exercise
question
What is status asthmaticus?
answer
Severe obstruction lasting for day or weeks.
question
What will diagnostic testing for asthma show?
answer
- ? in FEV? of more than 15% p bronchodilator - Respiratory alkalosis -Eosinophilia
question
What will you see in an anesthetized asthmatic patient during an attack?
answer
Wheezing, mucous, high inspiratory pressures, blunted CO? waveform, hypoxemia
question
What are 3 risk reduction strategies used in the asthmatic patient?
answer
1- review meds ; control 2- provide meds to improve lung function possibly oral systemic corticosteroids 3- If on high dose steroids, give 100mg hydrocortisone every 8 hours IV during surgical period the wean within 24 hours postop.
question
Preoperative evaluation of asthmatic patient
answer
- atropine or robinul exhibit mild bronchodilating effects and are effective 20-30 minutes before surgery
question
Intraoperative management of asthmatic
answer
-Regional safer -Propofol or ketamine for induction -Avoid atracurium (histamine release), B blockers (bronchoconstrict such as esmolol or labetalol -caution with emergence ; extubation
question
Pregnancy ; astham
answer
- Treat, albuterol is preffered -Inhaled steroids are safer - don't use H? blockers -ephedrine for vasopressor
question
Pulmonary Artery Hypertension
answer
- Caused by ?in vascular tone and the growth & proliferation of pulmonary vascular smooth muscle - 90% small vessel obliterated in lungs - ECG enlarged R atrium, R ventricle hypertrophy - Anesthesia management: vasodilator agents
question
Cor Pulmonale or Pulmonary Heart Disease
answer
- PAH advanced into R ventricle hypertrophy, dilation and cardiac decompensation - Hypertrophy of smooth muscle in tunica media= irreversible ? in PVR - R sided cath for diagnosis (usually also has COPD)
question
What are some clinical signs of cor pulmonale?
answer
-? JVD -Cardiac heave - widely split S?, S? gallop & presence of S? -Pulmonic or tricuspid murmur - hepatomegaly, ascites - large, hypertrophic R heart
question
Treatment & anesthesia management in cor pulmonale?
answer
Goals: ? workload of heart, reduce PVR, prevent ? in PAP, avoid major hemodynamic changes Anesthesia: keep well oxygenated, avoid acidosis, avoid vasoconstrictors, avoid ? sympathetic tone, avoid hypothermia
question
Pulmonary embolism
answer
PE is the impaction of a dislodged thrombus into the pulmonary vascular bed. - contributing factors: stasis of blood flow, venous injury, hyper coagulation (Virchow triad) - moderate hypoxemia without CO? retention
question
What are some S/S of PE?
answer
- Dyspnea of sudden onset -tachypnea, tachycardia - hypotension - cyanosis - neck vein distention - chest pain, syncope - cough, hemoptysis
question
Surgery with PE
answer
-Usually to place umbrella filter -use high FIO? -may need continuos catecholamines - Induction with etomidate or ketamine (hemodynamically stable) -Detection under GA: decreasing PETCO? and tachycardia followed by ? in SaO? and arterial hypoxemia -ECG: right axis deviation, R BBB, peaked T waves
question
Pulmonary edema
answer
-Excess fluid in interstitial and air-filled spaces of lung -High pressure & ? permeability (Starling) -Nearly always accompanied by preexisting disease - Upper airway obstruction, laryngospasm after extubation (observe longer than 60-90 mins) - Pink, frothy expectorations - Basilar crackles on auscultation - Rapid, shallow breathing - Pleural effusion, "whited out", "butterfly" CXR
question
Anesthesia Management of Pulmonary Edema
answer
- high FiO? - PEEP or CPAP or intubation - Vasodilators, diuretics, inotropes, steroids - Morphine frequently used , preload reducer & venodilatory -Furosemide, ?left atrial pressure, diuresis
question
Aspiration Pneumonitis
answer
- Adds 15 days to hospital stay, $22,000 1:3000 anesthetics - stomach contents into lung -induction,intubation or emergence -chemical, mechanical or bacterial - arterial hypoxemia, tachypnea, tachycardia, HTN, cyanosis - ABG & CXR
question
Anesthesia Management in Aspiration Pneumonitis
answer
-bicitra 15-30 minutes preop -famotidine or other H? blocker 45-60 mins prep - if aspiration during induction, tilt head to side, rapid suction of mouth & pharynx -early PEEP - condition of patient 2 hours post aspiration is prognostic of eventual course
question
ARDS
answer
- history or noxious event? interval of hours to days of normal lung function post event? rapid onset and progression to dyspnea, severe hypoxia, stiff non-compliant lungs - 50-70% mortality 90% in gram negative septic shock - Risk factors: shock, trauma, pulmonary infection, inflammatory disease, exposure to narcs/barbs, CNS disease, aspiration, metabolic events -cytokines & phospholipids - treat, O?, antibiotics, replace fluids, help heart
question
Anesthesia Management of ARDS
answer
- PIP, PEEP (barotrauma from prolonged high PEEP) - in general lower PEEP 6-8ml/kg and lower Vt - A-line for ABG's, lactic acid level -hypovolemic/ hemodynamically unstable - CO, filling pressures of heart -consider drug metabolism (multiple organs struggling) -continual precordial breath sounds
question
Noncytotoxic Drug Induced Pulmonary Disease
answer
- Over 100 drugs produce adverse effects on lungs - Amiodarone- severe pulmonary toxicity, accumulates in lung, non-productive cough, weight loss, dyspnea, fever, hypoxemia, usually after 2 months of administration - Gold salts used in RA, hypersensitivity in lungs, 6hr to 1month post administration
question
Cytotoxic Drug Induced Pulmonary Disease
answer
- Chronic pneumonitis ; fibrosis: direct cytotoxic effect on endothelial, interstitial or alveolar epithelial cells ?inflammatory response? deposits fibrin?interstitial inflammation - Hypersensitivity Lung disease: bleomycin, methotrexate, procarbazine -Noncardiogenic Pulmonary Edema: anti-neoplastic agents, bleomycin (lowest possible O?)
question
Pulmonary Oxygen Toxicity
answer
-Prolonged duration of O?, ;50% for 24 hours - Excessive production of free O? radicals -? O?, antineoplastic agents, age, previous radiotherapy of thorax, combination chemotherapy -Acute: type 1 cells, Chronic: type 2 cells - substernal chest pain, tachypnea, non productive cough
question
Sarcoidosis
answer
-Multisystemic disorder non-caseating epithelioid-cell granulomas, 90% involves lungs - cor pulmonale - lymph node involvement - treat with corticosteroids
question
Flail chest
answer
- chest trauma, multiple rib fractures -paradoxical movement of the chest wall at the site of fracture -hypoventilation, hypercapnia, alveolar collapse - pain control, intercostal nerve block, IS, PEEP - no wide swings in pleural pressure with vented patient
question
Simple Pneumothorax
answer
- no communication with the atmosphere - no shift of mediastinum or hemidiaphragm - catheter aspiration or tube thoracotomy - observe
question
Communicating Pneumothorax
answer
- communcation with atmosphere "sucking chest wound" - cover with occlusive dressing - tension pneumo possible - O?, thoracotomy, intubate ; ventilate
question
Tension Pneumothorax
answer
- Air progressively accumulates under pressure within the pleural cavity - Mediastinum shifts to opposite side - ?CO, ? BP, ?CVP - hypotension, hypoxemia tachycardia, ? airway pressures - Lethal, decompression of chest to treat, 16-18g angiocath into 2nd or 3rd intercostal space
question
Hemothorax
answer
- accumulation of blood in pleural cavity - evacuate blood, thoracostomy - spontaneous (rupture of alveoli), traumatic (rib fracture) or iatrogenic (line placement, barotrauma, high airway pressures) - no nitrous unless chest tube is present, never in closed pneumo
question
Atelectasis
answer
- collapse of pulmonary tissue, no gas exchange - first few minutes of GA, lasts hours to days due to loss of diaphragmatic tone - use Vt 6-10 ml/kg, PEEP and vital capacity maneuvers (30 cm H?O held for 10 seconds in alveoli)
question
Pleural Effusion
answer
- abnormal accumulation of fluid in the pleural space - Causes: block lymph drainage, cardiac failure, reduced plasma colloid osmotic pressure, infection -thoracostomy, thoracentesis, pleurodesis - tetracyline through chest tube= adhesion formation and fusion of membranes
question
Pectus Excavatum
answer
- funnel chest, depression of sternum - Reduced TLC
question
Pectus Carinatum
answer
-longitudinal protrusion of the sternum -displaced sternum, corrected surgically
question
Kyphoscoliosis
answer
-accentuated posterior curvature of spine - lateral bending and rotation of vertebral column - cervical scoliosis= difficult airway - ;60° curve = ? pulmonary function - ? lung volumes ; chest wall compliance, V/Q mismatch, hypoxemia, ?PAP, ?work of breathing, abnormal response to CO?
question
Anesthetic Management for Kyphoscoliosis
answer
-Assess -Labs, PFT -Blood type ; screen - MAC of 1, opioid infusion ; N?O - possible deliberate hypotension
question
Ankylosing Spondylitis
answer
- Rheumatoid spondylitis - fusion of spinal vertebrae and costovertebral joints - atypical fibrosis of lungs, fixation of thoracic cage
question
Anesthesia Management for Ankylosing Spndylitis
answer
- Upper airway is priority, potential for obstruction - Cervical spine involvement may limit movement -Awake intubation with fiberoptic scope
question
Airway Management M ; M
answer
-Improper face mask technique can cause continued deflation of anesthesia reservoir when APL is closed, indicating leak around mask. Mimimal chest movement ; minimal breath sounds = obstructed airway
question
What does the laryngeal airway protect?
answer
Partially protects the larynx from pharyngeal secretions. Should remain in place until return of airway reflexes.
question
What is done with the ETT cuff after insertion?
answer
-Cuff is inflated with least amount of air necessary to create positive pressure ventilation (minimize pressure transmitted to tracheal mucosa)
question
What is the earliest indicator of bronchial intubation?
answer
? in positive inspiratory pressure
question
What can cause postoperative hoarseness and increase the risk of extubation?
answer
Cuff above the level of the cricoid cartilage.
question
How can you prevent esophageal intubation?
answer
-Direct visualization of the tip of tube through the vocal cords. - Ausculate bilateral breath sounds - No gastric gurgling - ETCO? - CXR
question
What are some indications of bronchial intubation?
answer
- Unilateral breath sounds - hypoxia - inability to palpate cuff in sternal notch - decreased bag compliance - high inspiratory pressures
question
What can large negative intrathoracic pressures in struggling patient with laryngospasm result in?
answer
- Negative pressure pulmonary edema
question
How is the length for a nasal airway determined?
answer
-Measure nares to meatus of ear, should be about 2-4cm longer than oral airway
question
What is the maximum amount of positive pressure ventilation to avoid stomach inflation?
answer
20 cm H?O
question
Why are uncuffed tubes used in children?
answer
Minimize risk of pressure injury ; postintubation croup
question
What are oral tracheal tube size guidelines?
answer
Infant: 3.5 mm 12 cm Child: 4+ (Age/4 )= diameter 14+ (Age/2) = cm EG: 12 year old child 4+ (12/4)= 7mm 4+ (12/2)= 20cm Adult: Female: 7-7.5mm 24cm Male: 7.5-9.0mm 24c
question
In general when is the best time to extubate a patient?
answer
-Either deeply anesthetized or - Fully awake
question
How can you tell if a patient is lightly anesthetized or deeply anesthetized?
answer
Light: any reaction to pharyngeal suctioning Deep: no reaction to pharyngeal suctioning
question
How many mmHG is the ETT cuff inflated to?
answer
- About 20mmHG, higher pressures can lead to necrosis, inflammation, ulceration
question
How can you break a patient out of laryngospasm?
answer
-Gentle positive pressure ventilation - 100% O? - IV lidocaine or succinylcholine
question
Why do we use uncuffed tubes in peds?
answer
Minimize pressure injury and postintubation croup
question
Anatomy of mouth and nose
answer
Warms and humidifies air, resistance 2x compared to exercise
question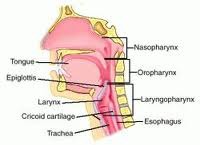
Anatomy of Pharynx
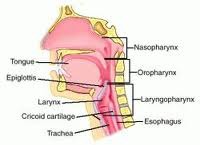
answer
Connects nasal/oral cavity to larynx Nasopharygnx separated by nasopharynx Oropharynx C2-C3 Hypopharynx ends at cricoid cartilage C4-C6 (food and respiration mix)
question
Anatomy of Larynx
answer
C3-C6 separates trachea from esophagus, reflexes exaggerated causes laryngospasm 3 paired (6) cartligages 3 unpaired thyroid, cricoid, aretynoid and epiglottis
question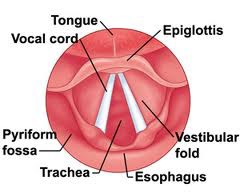
What is the narrowest part of the adult airway?
answer
Vocal cords



