Inhalational Anesthetic Drugs – Flashcards
Unlock all answers in this set
Unlock answersquestion
Definition of General Anesthesia
answer
Reversible, drug-induced state marked by loss of consciousness, analgesia, amnesia, inhibition of reflexes (autonomic & sensory-motor), and reduced skeletal muscle tone.
question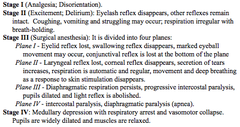
"Signs & Stages" of Anesthesia
answer
Useful concept, but details aren't really relevant. Key Point: Anesthesia has a graded drug action ; disinhibition can be seen.
question
"Balanced" Anesthesia

answer
Typical situation in which multiple drugs are used to induce ; maintain anesthesia.
question
What is the drug class of Inhalational Anesthetics?
answer
Non-Selective CNS Depressants
question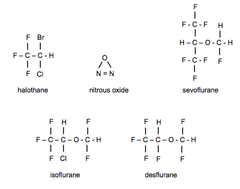
Structures of Inhalational Anesthetics
answer
All small molecules Except for nitrous oxide, they are all halogenated hydrocarbons (lipid soluble)
question
Administration of Inhalational Anesthesia
answer
Masks Vaporizers Anesthesia Machines
question
Mechanism of Action of Inhalational Anesthetics
answer
Very similar to barbiturates ; IV anesthetics like propofol in their effects on consciousness, background EEG, synaptic transmission at various sites in the CNS, etc. Molecular Mechanism: Idea that they somehow "partition" into the neuron plasma membrane (part in, part out) ; disrupt the normal structure. This is due to their relative fat solubility
question
Meyer-Overton Principle
answer
Anesthetic potency is proportional to fat:water partition coefficient. This is outdated ; has limited use (true up to a point). Problem- much is unexplained. For example, actions of many IV ; inhalational anesthetics are enantiomer-selective, but they have the same PC.
question
Effects of Inhalational Anesthetics on Synaptic Transmission
answer
Prominent effects to *potentiate GABA actions at GABA(a) receptors*, plus actions involving ligand-gated ion channels for other NTs, such as glutamate receptors. GABA(a) receptor does not have a specific high-affinity binding site for the anesthetics, but point mutations of particular amino acids greatly alter drug actions. Nitrous Oxide acts mainly via inhibition of NMDA receptors (but also does the above crap a little bit).
question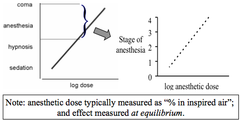
Dose Measurement ; Dose Response Curves of Inhalational Anesthetics
answer
Dose = % in inspired air Measure response at time of peak drug action (equilibrium) CURVE CHARACTERISTICS: 1. Dose-response curves are parallel so you can add agents based on relative potency, as represented by their MAC values. 2. The curves are steep (like other non-selective CNS depressants). 3. Response to anesthetics is greater in the elderly, with hypothermia ; in the presence of other CNS depressants
question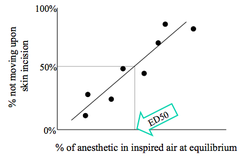
Quantal Dose Response Curves
answer
Method to compare inhalational anesthetics. Graph dose against the % of the population responding.
question
Minimal Alveolar Concentration (MAC)
answer
MAC = ED?? Modern inhalational anesthetics are potent enough so that MAC is achieved when inhaled air includes just a few % of the anesthetic EXCEPT for Nitrous Oxide, which has a MAC of 105%. This means that Nitrous Oxide cannot be used on its own (no room left for O?). *Potency is not related to speed of onset or reversal of anesthetic action.* -This is true for all drugs.
question
Vapor Pressure
answer
Nitrous Oxide is a gas, whereas the rest are volatile liquids that produce some finite vapor pressure according to the temperature
question
Partial Pressures of Inhalational Anesthetics
answer
Each substance equilibrates between the liquid phase ; air according to its solubility and the temperature. This is expressed as the partial pressure exerted by the agent in the blood or tissue.
question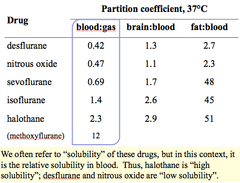
Partition Coefficient
answer
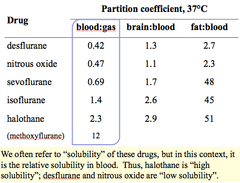
Measures *relative solubility* of the anesthetic in 2 phases at equilibrium. Important PC = *blood:gas partition coefficient* Ex: At equilibrium, more desflurane is in the gas phase than in the blood ("low solubility"). Conversely, more halothane is in the blood than the gas phase ("high solubility"). Note that normally when talking about drugs, solubility refers to the oil:water PC. For these drugs we care about relative solubility in blood.
question
Partial Pressure Gradients During Induction of Anesthesia
answer
Anesthesia must travel from the vaporizer through the machine to the lungs then to the blood then to the brain ; other tissues
question
Anesthetic Concentration
answer
Alveolar Fraction (FA) and Inhaled Fraction (FI) are used because they are easy to measure. FA/FI is used as a measure of equilibration. When FA = FI, equilibrium is reached and no uptake is occurring, i.e. patient is "fully anesthetized" (misnomer- they're just at equilibrium & may/may not be anesthetized based on potency & amount they're inhaling).
question
"Steps" for Equilibration of a Volatile Anesthetic During Induction (; Factors to Consider)
answer
1. Delivery to alveoli (pulmonary ventilation) 2. Equilibration between air ; blood (permeability through alveolar-capillary membranes, pulmonary blood flow) 3. *Establish tension in the blood (blood:gas PC) - this is the driving force for the next step* -Less soluble in blood = achieve tension quicker 4. Equilibration between blood ; tissue (blood flow to tissue, tissue permeability, BBB, blood:tissue PC). Anesthetics have excellent fat solubility (cross membranes easily) ; CNS has high blood flow. 5. Establish tension in the tissue (tissue:gas PC). *This correlates with drug effect.*
question
Key Points About Equilibration***
answer
The rate-limiting step for equilibration of inhalational anesthetics between inspired air ; brain during induction of anesthesia is *establishing tension in the blood, which is determined by the blood:gas PC.*
question
Characteristics of Anesthetics with a Large Blood:Gas PC
answer
Dissolve readily in blood Require a relatively large concentration to produce a reasonable partial pressure Equilibrate *slowly* Ex: Halothane
question
Characteristics of Anesthetics with a Small Blood:Gas PC
answer
Dissolve poorly in blood Require a relatively small concentration to produce a reasonable partial pressure Equilibrate *rapidly* Ex: Nitrous oxide, Desflurane
question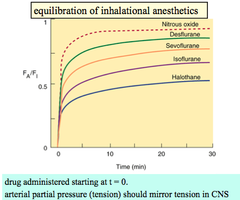
Equilibration of Various Inhalational Anesthetics
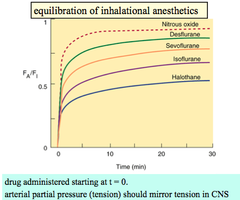
answer
1.0 FA/FI = Fully equilibrated
question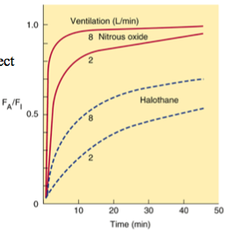
How can you speed the induction of anesthesia in order to get the patient anesthetized more quickly?
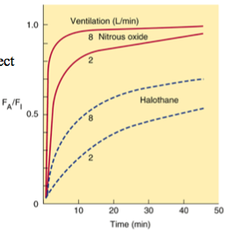
answer
Increasing minute volume (delivering the drug faster) has a large effect on the rate of equilibrium for agents most soluble in the blood (e.g. halothane), and much less effect on the least soluble anesthetics (e.g. nitrous oxide) This is kind of like a loading dose. It can also be changed by changing ventilation.
question
Distribution to Organs
answer
There are different rates for equilibration in different organs due to differing relative blood flows. "High blood flow" organs, including the CNS, equilibrate the fastest. Tissues like fat ; CT take much longer- usually longer than the duration of anesthesia. During a typical anesthesia, blood, brain ; lean body mass have equilibrated, but fat ; CT has not.
question
"Uptake" of anesthesia
answer
Refers to the arterial-venous gradient in partial pressure of the anesthetic.
question
Elimination of Inhalational Anesthetics
answer
Recovery from anesthesia is due to exhalation of the drug, which is the result of the same processes that drove induction of anesthesia. Thus, recovery is fast for nitrous oxide ; slower for halothane.
question
Elimination of Nitrous Oxide
answer
Elimination of nitrous oxide is so rapid that alveolar oxygen ; CO? are diluted. The resulting *diffusion hypoxia* is prevented by providing 100% oxygen for the first few minutes of recovery.
question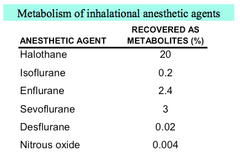
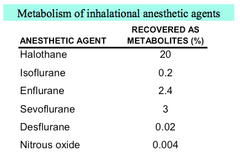
Biotransformation
answer
Does occur. Not important for termination of anesthesia, but for the toxicity of anesthetics. Especially important for halothane, which is associated with hepatic toxicity.
question
Other Actions of Anesthetics
answer
*Analgesia* - Nitrous oxide (action at NMDA-type glutamate receptors) *Depressed Respiration* - expected effects of non-selective CNS depressant (results in ? PaCO?) *CV System* - ? vascular resistance ? ? BP ; CO. Cerebral blood flow may be increased (2° to ? PCO?). Halothane sensitizes the myocardium to catecholamines *Hepatic ; Renal Function* are impaired 2° to ? blood flow. Halothane is associated with life-threatening drug-induced hepatitis (immune-mediated). *Malignant Hyperthermia*
question
Malignant Hyperthermia
answer
Autosomal dominant disorder of skeletal muscle that may occur in susceptible individuals undergoing general anesthesia with volatile agents ; muscle relaxants (especially succinylcholine). Signs: Hyperthermia, muscle rigidity, hypertension, tachycardia Onset within minutes ; can be rapidly fatal. Difficult to treat
question![[Drug Interactions & Other Influences that Increase the Anesthetic Effect (? MAC)] [Drug Interactions & Other Influences that Increase the Anesthetic Effect (? MAC)]](https://studyhippo.com/wp-content/uploads/2018/03/drug-interactions-other-influences-that-increase-the-anesthetic-effect-e28693-mac.png)
[Drug Interactions ; Other Influences that Increase the Anesthetic Effect (? MAC)]
![[Drug Interactions & Other Influences that Increase the Anesthetic Effect (? MAC)] [Drug Interactions & Other Influences that Increase the Anesthetic Effect (? MAC)]](https://studyhippo.com/wp-content/uploads/2018/03/drug-interactions-other-influences-that-increase-the-anesthetic-effect-e28693-mac.png)
answer
He said this was just "FYI"
question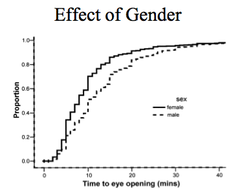
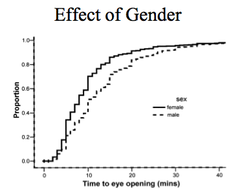
Gender ; MAC
answer
Women recover faster than men from anesthesia
question
["Second Gas Effect"]
answer
Prob don't need to know.



