Hand and UE dysfunction: OT eval and intervention – Flashcards
Unlock all answers in this set
Unlock answersquestion
Eval of hand injury
answer
( not necessarily in order of occurrence) 1. Establish rapport & review med hx/ hx of current condition 2. ID ct's occupational profile 3. Gently palpate for pain, adhesions and edema. 4. Use specific tests to elicit symptoms and clarify injury *** 5. Interview ct regarding pain, splints, functional use. 6. Use ADL checklist to uncover ADL dysfunction and set goals 7. Measure outcomes before and after therapy using Quick Disabilities of the Arm, Shoulder, and Hand Questionnaire (Quick DASH).
question
Specific hand testing (ROM and strength)
answer
1. ROM- goniometer 2. Strength: MMT, dynamometer and pinch gauge meter (OA?)
question
Specific hand testing (sensation)
answer
Semmes-weinstein monofilament (typically for nerve compression) 2 pt discrimination (typically nerve laceration and recovery)
question
Specific hand testing (coordination)
answer
O'Conner dexterity test 9 hole peg test Jebesen-Taylor Hand function test MN Rate of Manipulation test Crawford Small Parts Dexterity Test Purdue Pegboard test
question
Fracture healing phases
answer
3 stages: 1. Inflammation (cellular activity needed for healing) 2. Repair (callus for stabilization) 3. Remodeling (deposits bone) Safe time for movement v. protection depends on fracture type, stage of healing, and physician's orders.
question
Boxer's fracture
answer
result of a clenched fist hitting an object with enough force to break the metacarpophalangeal neck, most commonly seen in the fourth and fifth digits
question
Colles fracture
answer
Complete fx distal radius w DORSAL displacement. Most common
question
smith's fracture
answer
Complete fx distal radius with PALMAR displacement
question
Bennet's fracture
answer
Fx of 1st metacarpal base
question
Kienbock's disease
answer
blood supply to lunate disrupted resulting in fracture
question
Nerve injuries associated with wrist fractures
answer
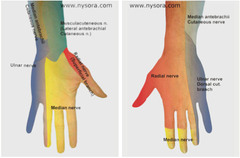
1. Median nerve injury: Carpal tunnel like symptoms such as palmar numbness of 1st digit to half of 4th digit with generalized weakness and pain 2. Ulnar nerve injury: Produces ulnar claw deformity and numbness on ulnar side of hand and 5th-4th digits with generalized weakness and pain
question
General UE fracture OT intervention
answer
1. Orthotic fabrications (materials chosen to fit ct and condition) 2. Modalities for pain relief and tissue healing 3. Therapeutic exercise 4. Home programs
question
Interventions for wrist fractures
answer
- ROM allowed in early phases - Orthotics protect extremity from motion or allow for protected motion - Home program - Exercises - Modalities
question
Exercise interventions for wrist fractures
answer
AROM with wrist extended and fingers flexed Blocking exercises Tendon and nerve gliding Strengthening (theraplast and use of hand exercises)
question
Complications of wrist fractures
answer
Carpal tunnel (compression of median nerve) CRPS
question
Fractures of forearm
answer
Caused by forceful load through outstretched arm 3 types: Type I: nondisplaced, tx with long arm sling Type II: displaced with single fragment, tx non-operatively with immobilization for 2-3 wks and early motion with medical clearance. Type III: comminuted, tx operatively w immobilization and early motion in the 1st post-op week as medically prescribed.
question
General OT interventions for fractures of the forearm
answer
- Orthotics for immobilization as needed - ROM early, within the 1st week - Sling for Type I or for comfort
question
Proximal humeral fracture

answer
Most common fx of upper arm May involve: Articular surface Greater or lesser tuberosity Surgical neck
question
OT Intervention for proximal humeral fracture
answer
1. Orthotics can be worn for support (ex humeral fracture brace) 2. Sling to immobilize fx in nonoperative tx 3. ROM may begin at 2 weeks after nonoperative fracture as medically prescribed * ROM protocol w agressive stretching 4-6 weeks after fx as prescribed by physician 4. Home exercise program * Crucial for return of motion and function * May include sling for comfort and sleeping for first 6 weeks as needed.
question
OT Intervention for proximal neck humeral fracture
answer
With a nondisplaced fracture of the humeral neck, support from a sling and supervised exercise lead to the most desirable outcome A sling without supervised ROM would result in decreased ROM and possible frozen shoulder.
question
Cummulative Trauma disorder (CTD)
answer
Also called overuse syndrome and repetitive strain injury Trauma to soft tissue caused by repeated force. Only a mechanism of injury, not a dx. Work-related risk factors: repetition, high force, direct pressure, vibration, cold environment, female gender, prolonged static position Symptoms: muscle fatigue, pain, chronic inflammation, sensory impairment, decreased ability to work.
question
Cummulative Trauma disorder (CTD) diagnoses
answer
- Tendonitis - Nerve compression syndrome - Myofascial pain - Cervical, thoracic and lumbar OA or nerve root impingement - Thoracic outlet syndrome - Rotator cuff tear - Bursitis - Epicondylitis - Cubital tunnel syndrome - Carpal tunnel syndrome - De Quervain syndrome
question
5 grades of Cummulative Trauma disorder (CTD) according to severity
answer
Grade I- pain after activity resolves quickly Grade II- pain during activity, resolves when activity stopped Grade III- pain persists after activity, affects work productivity, weakness and sensory loss Grade IV- Use of extremity results in pain up to 75% of time, work is limited Grade V- unrelenting pain, unable to work
question
Cummulative Trauma disorder (CTD) OT intervention components
answer
1. Acute phase 2. Sub acute phase 3. Return to work 4. Functional capacity evaluation 5. Work hardening
question
Cummulative Trauma disorder (CTD): OT intervention- acute phase
answer
Reduction of inflammation and pain through: Static splinting Ice Contrast baths Ultrasound Iontophoresis Estim
question
Cummulative Trauma disorder (CTD): OT intervention- subacute phase
answer
Slow stretching Myofascial release Progressive resistive exercise as tolerated Proper body mechanics Education on id of triggers Return to scute phase tx with flareups Static splint during activities that cause pain
question
Cummulative Trauma disorder (CTD): OT intervention- Return to work
answer
- Assess job site, tools used and body positioning - Therapy using: a work simulator weight well elastic bands functional activities strengthening activities
question
Extensor and flexor tendon surgical repair: OT intervention goals
answer
**Early mobilization** 1. Increase tendon excursion (distance a tendon travels upon movement of a joint) 2. prevent adhesions 3. increase ROM 4. Improve strength 5. facilitate resumption of meaningful roles/occupations/activities
question
Flexor tendon injury protocols
answer
Early mobilization protocol: within days after surgery to prevent adhesions, promote tendon gliding and excursion *These protocols are more appropriate for adults, who are able to follow directions and adhere to instructions.* 1. Duran protocol 2. Kleinert protocol include home exercise program *Electrical stimulation and ultrasound are not used on tendon injuries until 6-8 weeks postinjury*
question
controlled passive motion
answer
Joints may only be moved passively in this controlled-movement flexor tendon protocol. Because this is a flexor tendon repair, extension needs to closely guarded to prevent flexor tendon rupture The distal interphalangeal joint and proximal interphalangeal joint can be passively extended if the other joints of the digit are flexed to initiate tendon glide and prevent scarring of the tendon
question
Duran protocol

answer
early PROM program dorsal blocking splint Strengthening/ work/leisure NOT initiated until late phase of repair surgery (8-12 weeks)
question
Kleinert protocol

answer
active extension of digits, passive flexion via traction (rubber band) Strengthening/ work/leisure NOT initiated until late phase of repair surgery (8-12 weeks)
question
Flexor tendon injury Immobilization protocol
answer
for patients unable to care for themselves or cannot ensure post-op safety. Sometimes used with children Splinting to prevent rupture. *Repaired tendon is at its weakest 10-12 days post-op*
question
Flexor tendon injury complications
answer
Nerve laceration Edema Pain *ADL dysfunction should be assessed with ADL checklist Impaired muscle action in flexion and deviation of wrist
question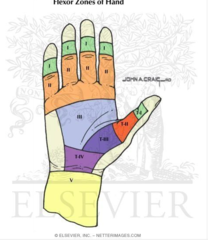
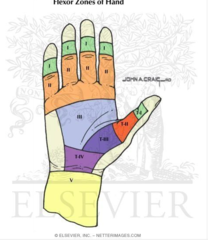
Flexor tendon anatomy
answer
2 long and thin muscles tendons: 1. Flexor digitorum superficials (FDS) 2. Flexor digitorum profundus (FDP) Glide and run under tight pulley system. Nerve supply: M, R ; U branches ZONES 1-4 in hand (4 over transverse carpal ligament). 5 beyond wrist.
question
Extensor tendon anatomy

answer
3 muscles tendons: 1. Extensor digitorum (communis) (EDC) 2. Extensor indicis proprius (EIP) 3. Extensor digiti minimi (EDM) Tendons cross wrist dorsally under extensor retinaculum Separate into 8 compartments to prevent bowstringing Digits: ZONES 1-6 in hand, 7 in wrist Thumb: ZONES 1-4 in thumb, 5 over wrist.
question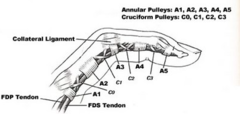
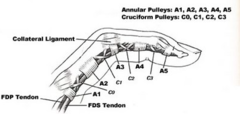
Flexor tendon pulleys: anatomy
answer
FDS and FDP tendons slide and run under tight pulley system. * Pulleys on flexor side prevent bowstringing: - A1 A2 A3 A4 and C1 C2 C3 C4
question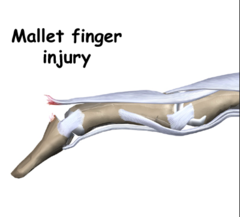
extensor tendon injuries: Zone 1 ; 2
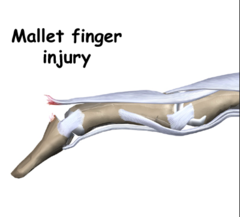
answer
*Mallet finger* 0-6 weeks DIP extension splint
question
Mallet finger

answer
client is unable to extend the distal interphalangeal (DIP) joint but can move it into extension passively 0-6 weeks DIP extension splint The client should not move the DIP at all for 6 weeks to protect the tendon Gripping activities can damage the tendon further initially The DIP terminal tendon is delicate and requires continuous splinting to prevent extensor lag of the tendon
question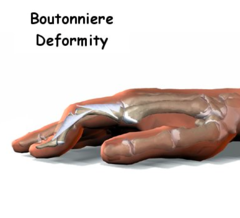
extensor tendon injuries: Zone 3 ; 4
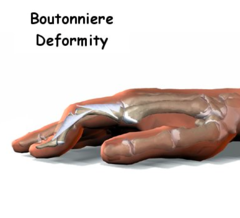
answer
*Boutonniere deformity* 0-4 weeks PIP extension splint (DIP free) AROM of DIP while in splint 4-6 weeks begin AROM of DIP and flexion of digits to DPC
question
extensor tendon injuries: Zone 5, 6 ; 7
answer
0-2 weeks volar wrist splint, mcps in 0-10 flexion and IP full extension 2-3: shorten splint to allow flexion/ extension of IP 4 weeks: remove splint to begin MCP active flexion and extension 5 weeks: AROM wrist. wear splint inbtwn exercises
question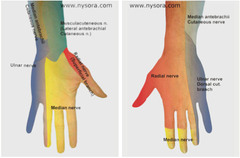
Radial nerve injury/laceration
answer
High lesions at level of humorous Posture of hand is wrist drop Possible lack of finger and thumb extension inability to extend digits to release objects difficulty with manipulation
question
Radial nerve injury/laceration NON-OP: OT intervention
answer
1. WRIST COCK-UP SPLINT W DYNAMIC EXTENSION 2. PROM and AROM 3. Sensory education if needed 4. home program 5. activity modification Isotonic strengthening exercises upon muscle reinnervation (isotonic: exercises that isolate a particular muscle or muscle group to increase strength or improve performance)
question
Radial nerve injury/laceration POST-OP: OT intervention
answer
STATIC WRIST EXT SPLINT 30* After 4 weeks: Adjust splint to 10*/20* extension
question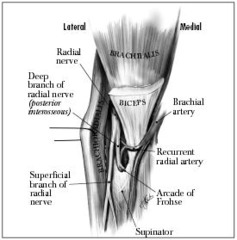
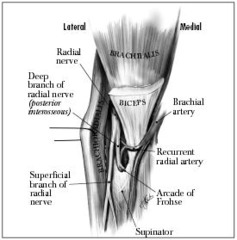
Radial tunnel syndrome
answer
Entrapment of radial nerve. The "radial tunnel" is the region from the humeroradial joint past the proximal origin of the supinator muscle Symptoms include burning pain in lateral forearm
question
Radial tunnel syndrome NON-OP: OT intervention
answer
1. LONG ARM SPLINT: elbow flexed, forearm supinated, wrist neutral 2. Massage/ TENS for pain 3. Pain free ROM 4. Nerve glides 5. Activity modification ** Avoid forceful wrist extension and supination
question
Radial tunnel syndrome POST-OP: OT intervention
answer
1. LONG ARM SPLINT: elbow flexed, forearm supinated, wrist neutral 2 WEEKS * WRIST COCK-UP for another 2 weeks. 2. Passive ; active pronation and supination 3. 3 weeks: hand strengthening, 6 weeks: resistive exercise
question
Radial nerve compression: radial nerve palsy
answer
weakness of extensors to wrist, MCP and thumb. wrist drop May be caused be sleeping position or humeral shaft fx
question
Radial nerve compression: radial nerve palsy non-op OT tx
answer
dynamic extension splint activity modification strengthening or wrist and finger extensors
question
Radial nerve compression: radial nerve palsy Post OP: OT tx
answer
surg: decompression ROM nerve gliding strengthening 6-8 weeks post op ADL and meaningful role activities
question
Anterior interosseous syndrome
answer
Compression of anterior interosseous nerve. (considered part of median nerve) Motor loss involving: 1. Flexor pollicis longus (flex thumb at MCP and IP) 2. Flexor digitorum profundus to index finger (flexion of MCP, PIP ; DIP digits 1-4) 3. Pronator qaudratus (radioulnar pronation) Inference: decreased pinch, decreased wrist pronation?
question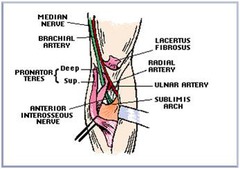
Pronator teres syndrome
answer
Entrapment of median nerve between 2 heads of pronator teres. Similr symptoms to CTS Deep pain proximal forearm with activity. *Positive Tinels sign at the forearm*
question
Pronator syndrome NON-OP: OT intervention
answer
1. SPLINT ELBOW AT 90*-100* flexion, forearm neutral. 2. Gentle prolonged stretching * supination *elbow wrist and finger extension 3. Activity modification * AVOID repetitive forearm rotation with resistance and prolonged elbow flexion
question
Pronator syndrome POST-OP: OT intervention
answer
Surgical decompression 1. HALF CAST 2. AROM all UE joints while wearing cast *Full AROM gained by 8 weeks. 3. nerve glides 4. Strengthening 2 weeks post op. 5. sensory reeducation 6. work/activity modification
question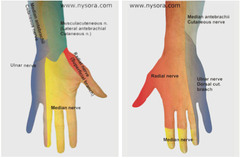
Median nerve injury/laceration
answer
Causes "Ape Hand Deformity". Sensory loss: index, middle and radial side of ring finger Loss of movement: 1. Low lesion: thumb opposition (opponens pollicis) ; abduction (abd pol brevis) ; MCP flexion (flexor pol brevis) index finger MCP and PIP flexion (lumbricals I ; II) 2. high lesion: All of above and FDP ; FPL ( flex tip of index middle fingers and thumb) and FCR (flex radial aspect of wrist) functional loss: loss of thumb opposition and pinch
question
Median nerve injury/laceration splinting considerations
answer
STATIC THENAR WEB SPACER SPLINT/ c bar to prevent thumb adduction contracture
question
Median nerve injury/laceration POST-OP: OT intervention
answer
1. DORSAL PROTECTION SPLINT/BLOCKING SPLINT 4-6 weeks * wrist in 30 flexion if low lesion * include elbow at 90 if hight lesion 2. AROM ; PROM for digits and thumb 2 weeks post-op 3. Tendon gliding exercises 4. Scar massage/ management 5. Strengthening begins at 9 weeks 6. initiate sensory re-education when individual demonstrates level of diminished protective sensation
question
Double crush syndrome
answer
Peripheral nerve trapped in more than 1 location. Intermittent diffuse arm pain and paresthesias with specific postures Paresthesia: sensation of tingling, tickling, pricking, or burning of a person's skin with no apparent long-term physical effect.
question
When a client reports dual sites of impingement of a single nerve without a history of trauma, what condition is MOST likely the cause?
answer
Over time, diminished blood flow to a peripheral nerve can result in serial impingements, called double crush syndrome
question
Double crush syndrome NON-OP: OT intervention
answer
1. Treat according to each nerve injury or syndrome, avoiding movements or postures that aggravate symptoms. 2. Nerve gliding exercises 3. Exercises for scapular stability 4. Posture and core trunk strengthening
question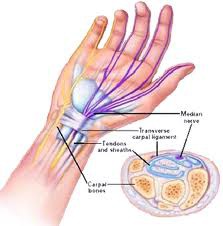
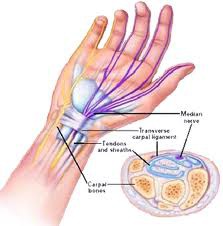
Carpal tunnel syndrome
answer
Entrapment of MEDIAN NERVE in carpal tunnel. Most common nerve compression. Sensory impairment along median nerve distribution: numbness and tingling in thumb, index and middle finger. Motor impairment: decreased fine motor coordination * advanced cases: Adductor pollicis atrophy (thenar eminence, ADDucts thumb)
question
Carpal tunnel syndrome specific evaluation
answer
*Positive Tinels sign at wrist. Postive phalen's sign* 1. Tinel's sign 2. Phalen's test 3. Moberg Pickup test: timed test of picking up, holding, manipulating, and id-ing small objects. * Used with children and cognitively impaired adults to test median nerve function 4. Semmes-weinstein: monofilament test for loss of sensation
question
Tinel's sign
answer
tap median nerve at wrist to elicit symptoms
question
Phalen's test
answer
hold wrist in full flexion for 1 min to elicit changes in sensation
question
Carpal tunnel syndrome NON-OP: OT intervention
answer
1. CARPAL TUNNEL SPLINT or WRIST COCK-UP at 10-20* wrist extension. - Prefab splint okay if wrist position adjustable 2. Nerve ; tendon gliding 3. Activity modification - ergonomic keyboard 4. Client education - avoid activities that aggravate 5. Postural training and proximal conditioning exercises.
question
Carpal tunnel syndrome POST-OP: OT intervention
answer
* May not need therapy 1. May require wound care and scar mobilization 2. Splinting for those who sleep with wrist flexed 3. AROM wrist, thumb and fingers 1-2 days post op 4. Nerve ; tendon gliding exercises 5. Strengthening: 3-6 weeks post op
question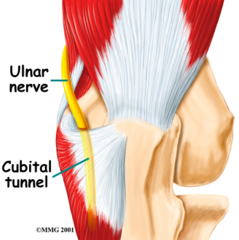
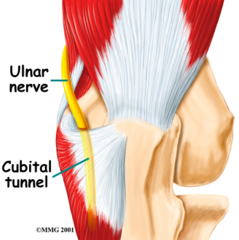
Cubital tunnel syndrome
answer
2nd most common nerve compression proximal ULNAR NERVE compression at the elbow btwn the medial epicondyle and olecranon process. Caused by leaning on elbow and extreme elbow flexion. Pain at elbow with extreme elbow flexion Positive Tinel's sign at elbow Numbness/weakness along ulnar distribution Motor impairment: decreased power grip and pinch strength due to weakness in intrinsic hand muscles: 1. dorsal/palmar interossi (ADD/ABD fingers at MCP) 2. adductor pollicis (thumb ADD) 3. flexor carpi ulnaris (wrist flexion and ulnar deviation)
question
Cubital tunnel syndrome NON-OP: OT intervention
answer
1. ELBOW SPLINT or positioning at 30-60* flexion 3 weeks 2. Edema control 3. Pain management 4. Ulnar nerve gliding 5. Proximal conditioning activities 6. Posture and ergonomic training
question
Cubital tunnel syndrome POST-OP: OT intervention
answer
decompression or transposition Protection phase: 1 day to 3 weeks 1. SPLINT ELBOW at 70-90* flexion 2. wound care 3. edema control 4. pain management 5. AROM of uninvolved joints 6. Teach one handed ADLS Active phase: starting at 3 weeks * Discontinue splint 1. Elbow ROM 2. Ulnar nerve gliding 3. desensitization techniques 4. strengthening at 4 weeks
question
Claw deformity: Ulnar nerve laceration/compression

answer
Ulnar nerve compression or lesion at the wrist or above Positive *Froment's sign*: flexion of thumb IP when lateral pinch attempted. Causes include: ganglion, neuritis, arthritis Sensory loss: along ulnar distribution. If on dorsal side of hand, injury is proximal to Guyon's canal Motor loss: intrinsic ulnar innervated muscles, loss of power grip and pinch strength. Results in: MCP hyperextension IP flexion hand arches flattened.
question
Claw deformity:Ulnar nerve laceration/injury specific evaluation
answer
1. *Froment's sign*: flexion of thumb IP when lateral pinch attempted. 2. *Wartenberg's sign*: 5th finger ABDucted from 4th finger 3. *Jeanne's sign*: hyperextension of thumb MCP 4. Semmes-weinstein
question
Froment's sign is
answer
Flexion of thumb IP when lateral pinch attempted. Froment's sign occurs when the flexor pollicis longus compensates for a weak or paralyzed adductor pollicis and flexor pollicis brevis. When a client attempts to pinch, the interphalangeal joint of the thumb flexes more than usual.
question
Claw deformity: Ulnar nerve laceration/injury NON-OP: OT intervention
answer
also see median nerve repair 1. ULNAR NERVE PALSY/ANTICLAW SPLINT - dynamic PIP extension if PIP flexion contractures present. 2. Padded antivibration glove can be used during activity to prevent further irritation 3. Activity modification: - ergonomic handles, gel pads, pad handles of vibrating equipment 4. Ct education: avoid postures and activities that aggravate (ulnar deviation w wrist flexion)
question
Claw deformity: Ulnar nerve laceration/injury POST-OP: OT intervention

answer
also see median nerve repair 1. Bulky dressing 3-10 days 2. DORSAL BLOCKING SPLINT discontinue at 6 weeks, use until muscle function returns 3. Wound care and scar mobilization 4. Sensory desensitization when wound is healed and stitches removed 5. AROM of wrist and hand at 6 weeks. may resume ADLS and begin strengthening 6. Sensory reeducation 10-12 weeks post surg- once protective sensation returns * Tendon transfer if nerve doesn't regenerate with 1 year.
question
Sensory reeducation after nerve injury
answer
- Protective reeducation: educate cts to visually compensate for sensory loss and avoid working with machinery and temperatures below 60* - Discriminative education: vision- tactile matching process in which cts id objects without vision - Sensory recovery: begins with pain perception and progresses to vibration, moving touch, and constant touch. - Desensitization: applying different textures and tactile stimulation to reeducate nervous system.
question
sensation return after nerve injury
answer
In the realm of nerve healing and testing, the order in which recovery occurs is one-point moving, one-point discrimination, two-point moving, and finally two-point discrimination.
question
Guyon's canal
answer
Ulnar nerve compression at the wrist. Numbness and tingling on Ulnar side of hand Positive tinels sign at Guyon's canal
question
Guyon's canal non-op OT tx
answer
splint wrist in neutral activity modification
question
Guyon's canal post op OT tx
answer
decompression surgery edema control AROM Nerve gliding strengthening 2-4 wks- focus on power grip sensory reeducation
question
Lateral epicondylitis
answer
Tennis elbow Degeneration of tendon origin as result of repetitive micro trauma. Overuse of wrist extensors *especially ECRB (wrist extension and ABD/radial deviation)
question
medial epicondylitis
answer
Golfer's elbow Degeneration of tendon origin as result of repetitive micro trauma. Overuse of wrist flexors.
question
Lateral and medial epicondylitis OT tx (non-op)
answer
Elbow strap, wrist splint ice/deep friction massage stretching activity/work modification when pain decreases, add strengthening * begin isometric then progress to isotonic and eccentric
question
de Quervain syndrome

answer
Caused by cumulative trauma resulting in tenosynovitis of the thumb muscle tendon unit and tendons in the 1st dorsal compartment of the wrist. Specific movement causes: - Repetitive thumb ABDuction with wrist ulnar deviation - CMC OA - Scaphoid fracture - Intersection syndrome - Radial nerve neuritis Activities: Keyboarding, piano playing, knitting, racket sports.
question
de Quervain syndrome NON-OP: OT intervention
answer
Medical tx: corticosteriod injections 1. FOREARM BASED SPICA SPLINT: wrist in neutral and thumb radially abducted for 3 weeks. SOFT SPLINT after 3 weeks. 2. Activity modification (avoid pinch) 3. After 3 weeks, isometric exercise 4. Education on computer ergonomics 5. Strengthening activities
question
de Quervain syndrome POST-OP: OT intervention
answer
Med tx: surgical release of 1st dorsal compartment 1. FOREARM BASED SPICA SPLINT: wrist at 20* extension, thumb radially abducted for 3 weeks. 2. Gentle ROM 3. Tendon gliding 4. Grip and pinch strengthening at 2 weeks 5. Scar management and desensitization techniques
question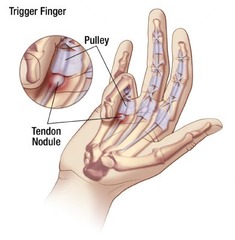
Digital stenosing tenosynovitis (trigger finger)
answer
Sheath inflammation or nodules of A1 pulley (finger flexors) Caused by repetition and the use of tools too far apart
question
Digital stenosing tenosynovitis (trigger finger) OT tx

answer
HAND BASED SPLINT mcp at 0* for 3-6 weeks or surgically release A1 pulley To rest the tendon and prevent snapping as the tendon pulls through the finger pulleys, the MCP joint is blocked by splinting, then gentle pull through with bending and straightening of the distal and proximal interphalangeal joints is recommended 20 times every 2 hours while the client is awake Making a full fist without the splint on will increase tendon inflammation and edema. Reduce use of excessive gripping force, prevent contact stress, and implement task rotation
question
Dupuytren's disease
answer
fascia of palm and digits becomes contracted. develops cords extending to digits Surgical release is required
question
Dupuytren's disease: OT intervention
answer
wound care edema control splinting in extension A/PROM and progress to strengthening when wounds are healed Scare management purposeful and occupation based tasks emphasizing grip and release.
question
Skier's thumb/ game keeper's thumb

answer
commonly caused by falling while skiing with thumb held in a ski pole
question
skier's thumb non-op OT tx
answer
Thumb splint 4-6 weeks AROM and pinch strengthening 6 weeks ADLs that require opposition and pinch strength
question
skier's thumb post op OT tx
answer
Thumb splint 6 weeks followed by AROM. PROM @ 8 weeks Strengthening @ 10 weeks
question
CPRS
answer
Vasomotor dysfunction as result of abnormal reflex. Type I: develops after noxious event (collets fx) Type II: develops after nerve injury pain disproportionate to an injury that is either sympathetically maintained or independent of sympathetic nervous system
question
CRPS symptoms

answer
pain: Allodynia- sensation misinterpreted as pain Hyperalgia- increased response to painful stimuli Hyperpathia- pain continues after stimulus removed Edema Contractures vasomotor changes and instability: Bluish or red shiny skin Abnormal sweating and hair growth temperature changes Low tolerance for activity
question
OT intervention CRPS
answer
The most recognized treatment of complex regional pain syndrome is a stress loading program and use of the upper extremity in functional activities that promote occupational engagement 1. Gentle pain free AROM for short periods * Blocked exercises, tendon glides 2. Stress loading (ei scrubbing floor) ; Desensitization techniques (ei fluidotherapy) 3. Pain control techniques * TENS * splinting (static, then dynamic as tolerated) * Continuous passive motion 4. Edema control * elevation * massage * AROM * contrast baths (mixed evidence) * compression glove etc 5. ADL- pain free use * Joint protection, energy conservation * splinting to prevent contractors and enable occupational engagement
question
PROCEED WITH CAUTION/AVOID in CRPS tx
answer
- People with CRPS are often cold intolerant- no cold packs - PROM increases pain and swelling and is often contraindicated - joint mobilization - dynamic splinting - casting
question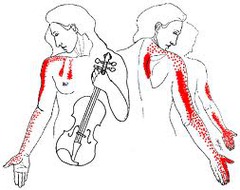
Thoracic outlet syndrome
answer
Compression of the brachial plexus, subclavian artery and vein as it passes under clavicle. May cause a vague, aching pain in the neck, shoulder, arm, or hand. It may also cause pain, numbness, or tingling on the inside of the forearm and the fourth and fifth fingers of the hand. Weakness may occur
question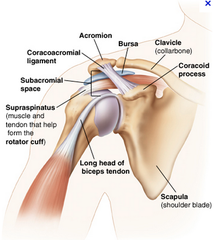
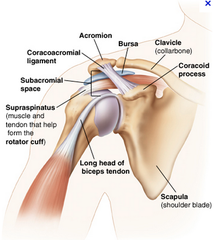
Rotator cuff tendonitis
answer
caused by overuse, weakness of muscles, ligament and capsule tightness ; trauma site of impingement is at coracoacromial arch
question
Rotator cuff tendonitis non-op OT tx
answer
1. Activity modification: *no movement above shoulder level until pain subsides* 2. Ct education on sleeping posture: avoid sleeping w adduction and internal rotation 3. Decrease pain: - positioning - modalities - rest 4. restore pain free ROM 5. Strengthening *below shoulder level* 6. Occupation ; role specific training
question
Rotator cuff tendonitis post-op OT tx
answer
Surg: arthroscopic surgery. open repair for tears 1. PROM 0-6 weeks, progress to AROM 2. decrease pain. start w ice and progress to heat 3. strengthening at 6 weeks: start with isometrics and progress to isotonic below shoulder level 4. activity modification: light ADL and meaningful activities as tolerated 5. leisure and work activities 8-12 weeks post operative
question
Adhesive capsulitis (frozen shoulder)

answer
restricted ROM of shoulder: immobility and inflammation Greatest limitation in shoulder external rotation, then abduction, internal rotation and flexion linked to DM II and parkinson's
question
Adhesive capsulitis non-op OT tx
answer
Encourage use through ADL and role activities PROM Modalities
question
Adhesive capsulitis post-op OT tx
answer
Surg: manipulation and arthroscopic surg PROM immediately Pain relief: modalities Encourage use of extremity for all ADLs and role activities
question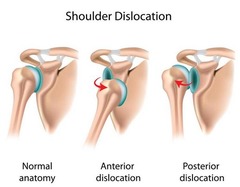
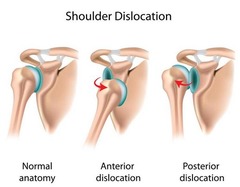
Shoulder dislocations
answer
anterior most common. caused by trauma and overuse
question
Shoulder dislocations OT tx
answer
*avoid combined ABDuction and external rotation w/ anterior dislocation* Regain ROM Pain free ADL and role activities Strengthen RCuff



