First Aid-Biochemistry – Flashcards
Unlock all answers in this set
Unlock answersquestion
Purines
answer
A, G 2 Rings ("PUR e A s G old = PUR ines")
question
Pyrimidines
answer
C, T, U 1 ring ("CUT the PY (pie): PY rimidines")
question
Functional groups of the nucleosides
answer
Guanine has a ketone. Thymine has a methyl. Deamination of cytosine makes uracil.
question
AA's necessary for purine synthesis
answer
G lycine A spartate G lutamine
question
Nucleoside
answer
Base + ribose
question
Nucleotide
answer
Base + ribose + phosphate; linked by 3'-5' phosphodiester bond.
question
Deoxyribonucleotide synthesis
answer
Ribonucleotides are synthesized first and are converted to deoxyribonucleotides by ribonucleotide reductase.
question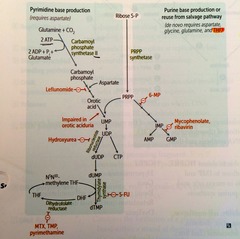
Hydroxyurea
answer
Inhibits ribonucleotide reductase.
question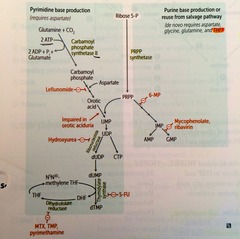
6-mercaptopurine (6-MP)
answer
Blocks de novo purine synthesis. from PRPP to IMP
question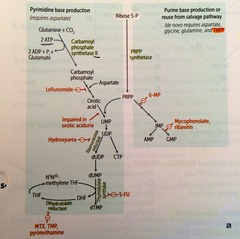
5-Fluorouracil (5-FU)
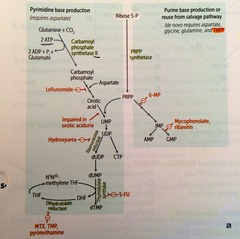
answer
Inhibits thymidilate synthase
question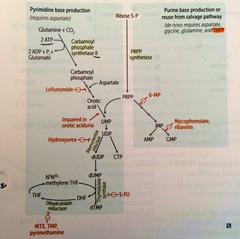
Methotrexate
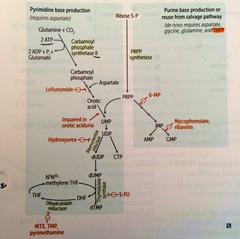
answer
Inhibits dihydrofolate reductase
question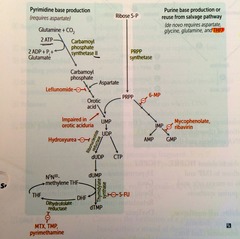
Trimethoprim
answer
Inhibits bacterial dihydrofolate reductase (decr dTMP)
question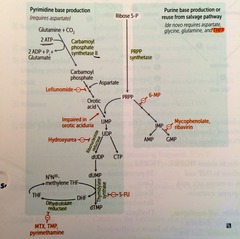
Pyrimethamine
answer
Inhibits DHFR
question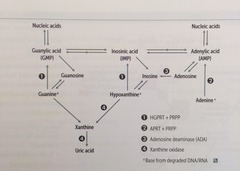
HGPRT
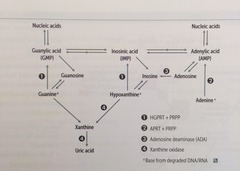
answer
guanine ? GMP hypoxanthine ? IMP deficiency = Lesch-Nyhan Syndrome
question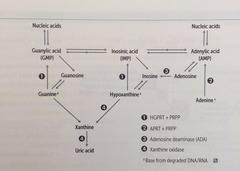
APRT
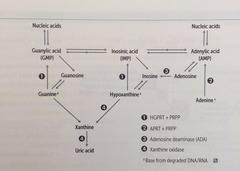
answer
adenine ? AMP
question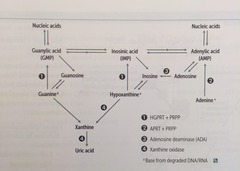
Adenosine Deaminase
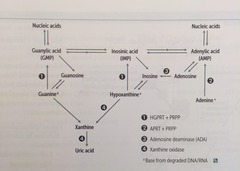
answer
adenosine ? inosine
question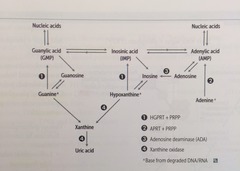
Adenosine Deaminase Deficiency
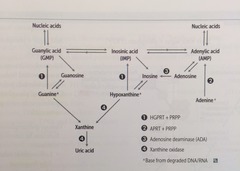
answer
?ATP and dATP inhibit ribonucleotide reductase ? prevents DNA synthesis ? ? lymphocyte count a major cause of AR SCID
question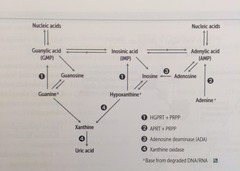
Lesch-Nyhan Syndrome
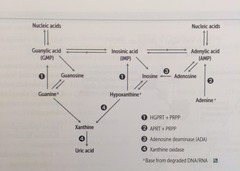
answer
absent HGPRT ? defective purine salvage excess uric acid production, ? de novo purine synthesis MR, self-mutilation, aggression, hyperuricemia, gout, dystonia tx: allopurinol, febuxostat (2nd line) H: hyperuricemia G: gout P: pissed off R: retardation dysTonia
question
Transition vs. transversion
answer
Transition: Substituting purine for purine or pyrimidine for pyrimidine ("TransI tion = I dentical type") Transversion: Substituting purine for pyrimidine or vice versa ("TransV ersion = conV ersion btw types")
question
Genetic code: unambiguous
answer
Each codon specifies only 1 AA.
question
Genetic code: degenerate/redundant
answer
; 1 codon may code for the same AA. (Methionine is encoded by 1 codon: AUG)
question
Genetic code: Commaless, nonoverlapping
answer
Read from a fixed starting point as a continuous sequence of bases. *some viruses are an exception.
question
Genetic code: universal
answer
Genetic code is conserved throughout evolution. *exceptions include mitochondria, archaebacteria, Mycoplasma , and some yeasts
question
Silent mutation
answer
Same AA, often base change in 3rd position of codon (tRNA wobble)
question
Missense mutation
answer
Changed AA (conservative -- new AA is similar in chemical structure) sickle cell disease
question
Nonsense mutation
answer
Change resulting in early stop codon ("Stop the nonsense !")
question
Frame shift mutation
answer
Change resulting in misreading of all nucleotides downstream, usually resulting in a truncated, nonfunctional protein duchenne muscular dystrophy
question
Severity of damage in DNA mutations
answer
frameshift;Nonsense ; missense ;;silent
question
Eukaryotic vs. prokaryotic DNA replication.
answer
Eukaryotic DNA replciation is more complex, but uses many analogous enzymes. In both: DNA replication is semiconservative and involves both continuous and discontinuous (Okazaki fragment) synthesis. For eukaryotes, replication begins at a consensus sequence of base pairs.
question
Origin of replication
answer
Particular sequence in genome where DNA replication begins. May be single (prokaryotes) or multiple (eukaryotes).
question
Single-stranded binding protein
answer
Prevents strands from reannealing.
question
DNA topoisomerases
answer
Create a nick in the helix to relieve supercoils created during replication. *Fluoroquinolones inhibit DNA gyrase (a specific prokaryotic topoisomerase)
question
Primase
answer
Makes an RNA primer on which DNA polymerase III can initiate replication.
question
DNA polymerase III
answer
Prokaryotic only. Elongates leading strand by adding deoxynucleotides to the 3' end. Elongates lagging strand until it reaches primer of preceding fragment. 3'-->5' exonuclease activity "proofreads" each added nucleotide.
question
DNA polymerase I
answer
Prokaryotic only. Degrades RNA primer and fills in the gap w/ DNA. (excises RNA primer w/ 5'-->3' exonuclease)
question
Single strand nucleotide excision repair
answer
Specific endonucleases release the oligonucleotide-containing damaged bases; DNA polymerase and ligase fill and reseal the gap, respectively. repairs bulky helix distorting lesions (mutated in xeroderma pigmentosum)
question
Xeroderma pigmentosum
answer
Mutated single strand nucleotide excision repair gene, which prevents repair of thymidine dimers.; Dry skin w/ melanoma and other cancers ("children of the night").
question
Single strand base excision repair
answer
Specific glycosylases recognize and remove damaged bases and creates AP site (apurinic/apyrimidinic) one or more nucleotides are removed by AP-endonuclease, which cleaves the 5' end. Lyase cleaves the 3' end DNA poly-Beta fill the gap and ligase seals
question
Single strand mismatch repair
answer
Unmethylated, newly synthesized string is recognized, mismatched nucleotides are removed, and the gap is filled and resealed. Mutated in hereditary nonpolyposis colorectal cancer (HNPCC).
question
Double strand nonhomologous end joining
answer
Brings together 2 ends of DNA fragments. No requirement for homology. mutated in ataxia telangiectasia
question
What direction is DNA/RNA made?
answer
They are both synthesized in the 5'-->3' direction. Remember that the 5' of the incoming nucleotide bears the triphosphate (energy source for bond). The 3' hydroxyl of the nascent chain is the target.
question
3 Types of mRNA
answer
rRNA is the most abundant mRNA is the longest tRNA is the smallest ("R ampant, M assive, T iny")
question
mRNA start codon
answer
AUG (or rarely GUG) ("AUG inAUG urates protein synthesis") In eukaryotes, codes for methionine, which may be removed before translation is completed. In prokaryotes, codes for formyl-methionine (f-Met).
question
mRNA stop codons
answer
UGA, UAA, UAG UGA = U G o A way UAA = U A re A way UAG = U A re G one
question
Promoter
answer
Site where RNA polymerase and multiple other transcription factors bind to DNA upstream from gene locus (AT-rich upstream sequence w/ TATA and CAAT boxes). Mutation here commonly results in dramatic drop in amount of gene transcribed.
question
Enhancer
answer
Stretch of DNA that alters gene expression by binding transcription factors.
question
Silencer
answer
Site where negative regulators (repressors) bind.
question
Eukaryotic RNA polymerases
answer
RNA pol I -- makes rRNA RNA pol II -- makes mRNA RNA pol III -- makes tRNA (I, II, and III are numbered as their products are used in protein synthesis) No proofreading fxns, but can initiate chains. RNA pol II opens DNA at promoter site.
question
Prokaryotic RNA polymerase
answer
One RNA polymerase (a multisubunt complex) makes all of the 3 kinds of RNA.
question
alpha-amantin
answer
Found in death cap mushrooms. Inhibits RNA pol II. severely hepatotoxic if ingested
question
RNA processing (in eukaryotes)
answer
Occurs in nucleus. After transcription: 1.) Capping on 5' end (7-methylguanosine) 2.) Polyadenylation on 3' end (~200 A's) 3.) Splicing out of introns Only processed RNA is transported out of the nucleus.
question
hnRNA vs. mRNA
answer
The initial transcript is called heterogeneous nuclear RNA (hnRNA) The capped and tailed transcript is called mRNA.
question
Polyadenylation signal
answer
AAUAAA
question
Poly-A polymerase does not require...
answer
a template.
question
pre-mRNA splicing (occurs in eukaryotes)
answer
1.) Primary transcript combines w/ snRNPs and other proteins to form spliceosome 2.) Lariat-shaped intermediate is generated 3.) Lariat is released to remove intron precisely and join 2 exons.
question
tRNA structure
answer
75-90 nucleotides, secondary structure, cloverleaf form, anticodon end is opposite 3' aminoacyl end. All tRNAs, both eukaryotic and prokaryotic, have CCA at 3' end along w/ a high percentage of chemically modified bases. The AA is covalently bound to the 3' end of tRNA. T-arm: thymine, pseudouridine, cytosine sequence for tRNA-ribo binding D-arm: dihydrouracil residue for tRNA recognition by the correct aminoacyl-tRNA synthetase acceptor stem: the 3' CCA is the AA aceptor site
question
Charging of tRNA
answer
Aminoacyl-tRNA synthetase (1 per AA, "matchmaker," uses ATP) scrutinizes AA before and after it binds to tRNA. If incorrect, bond is hydrolyzed. The aa-tRNA bond has energy for formation of peptide bond. A mischarged tRNA reads usual codon but inserts wrong AA. Aminoacyl-tRNA synthetase and binding of the charged tRNA to the codon are responsible for accuracy of AA seletion
question
tRNA wobble
answer
Accurate base pairing is required only in the first 2 nucleotide positions of an mRNA codon, so codons differing in the 3rd "wobble" position may code for the same tRNA/aa (due to degeneracy of genetic code).
question
Protein synthesis: initiation
answer
Activated by GTP hydrolysis, initiation factors (eIFs) help assemble the 40S ribosomal subunit w/ the initiator tRNA released when the mRNA and the ribosomal subunit assemble w/ the complex. E ukaryotes: 40S + 60S = 80S (E ven) PrO karyotes: 30S + 50S = 70S (O dd)
question
Protein synthesis: step 1 in elongation
answer
Aminoacyl-tRNA binds to Aa site (except for initiator methionine)
question
Protein synthesis: step 2 in elongation
answer
rRNA catalyzes peptide bond formation, transfers growing polypeptide to amino acid in A site.
question
Protein synthesis: step 3 in elongation
answer
Ribosome advances 3 nucleotides toward the 3' end of RNA, moving peptidyl RNA to P site (translocation)
question
Protein synthesis: termination
answer
stop codon recognized by release factor and completed polypeptide is released from the ribosome
question
Energy requirements of translation
answer
tRNA aminoacylation: ATP --> AMP (2 phosphoanhydride bonds) Loading tRNA onto ribosome: GTP --> GDP Translocation: GTP --> GDP Total energy expenditure = 4 high-energy phosphoanhydride bonds
question
Posttranslational modifications: trimming
answer
Removal of N- or C-terminal propeptides from zymogens to generate mature proteins.
question
Posttranslational modifications: covalent alterations
answer
Phosphorylation, glycosylation, and hydroxylation, methylation, acetylation, ubiquitination
question
CDKs
answer
Cyclin-dependent kinases; constitutive and inactive.
question
Cyclins
answer
Regulatory proteins that control cell cycle events; phase specific; activate CDKs
question
Cyclin-CDK complexes
answer
Must both be activated and inactivated for cell cycle to progress.
question
Tumor suppressors (and the cell cycle)
answer
Rb and p53 normally inhibit G1-to-S progression; mutations in these genes result in unrestrained cell growth.
question
Permanent cells
answer
Remain in G0, regenerate from stem cells. (e.g., neurons, skeletal and cardiac muscle, RBCs)
question
Stable (quiescent) cells
answer
Enter G1 from G0 when stimulated (e.g., Hepatocytes, lymphocytes)
question
Labile cells
answer
Never go to G0, divide rapidly w/ a short G1 (e.g., Bone marrow, gut epithelium, skin, hair follicles)
question
Rough Endoplasmic Reticulum (RER)
answer
Site of synthesis of secretory (exported) proteins and of N-linked oligosaccharide addition to many proteins.
question
Nissl bodies
answer
RER in neurons -- synthesize enzymes (e.g., ChAT) and peptide neurotransmitters.
question
Free ribosomes
answer
unattached to any membrane; site of synthesis of cytosolic and organellar proteins.
question
2 important examples of cells rich in RER
answer
Mucus-secreting goblet cells of the small intestine, Ab-secreting plasma cells.
question
Smooth endoplasmic reticulum (SER)
answer
Site of steroid synthesis and detoxification of drugs and poisons.
question
2 important examples of cells rich in SER
answer
Liver hepatocytes Steroid hormone-producing cells of the adrenal cortex
question
Golgi apparatus: modifies N-oligosaccharides on ____?
answer
Asparagine.
question
Golgi apparatus: adds O-oligosaccharides on ____?
answer
Serine and threonine.
question
Golgi apparatus: adds mannose-6-phosphate to ____? What does this do?
answer
Specific lysosomal proteins --> targets protein to the lysosome.
question
Vesicular trafficking proteins: COPI
answer
Retrograde: Golgi --> ER
question
Vesicular trafficking proteins: COPII
answer
Anterograde: RER -->cis-Golgi
question
Vesicular trafficking proteins: Clathrin
answer
trans-Golgi --> lysosomes, plasma membrane --> endosomes (receptor-mediated endocytosis) LDL receptor activity
question
I-cell disease (inclusion cell dz): genetic/molecular basis?
answer
Inherited lysosomal storage d/o; failure of addition of mannose-6-phosphate to lysosome proteins (enzymes are secreted outside the cell instead of being targeted to the lysosome) Coarse facial features, clouded corneas, restricted joint mvmt, and high plasma levels of lysosomal enzymes. Often fatal in childhood.
question
signal recognition particle
answer
cytosolic ribonucleoprotein traffics proteins from ribosome to RER if defective or absent, proteins build up in cytosol
question
Microtubules
answer
Cylindrical structure composed of a helical array of polymerized dimers of alpha- and beta-tubulin. Each dimer has 2 GTP bound. Incorporated into flagella, cilia, mitotic spindles. Grows slowly, collapses quickly. Also involved in slow axoplasmic transport in neurons.
question
dynein v kinesin
answer
Dynein = retrograde to microtubule (+ -; -) Kinesin = anterograde to MT (- -; +)
question
Drugs that act on microtubules
answer
1.) Mebendazole/thiabendazole (antihelminthic) 2.) Griseofulvin (antifungal) 3.) Vincristine/vinblastine (anti-cancer) 4.) Paclitaxel (anti-breast cancer) 5.) Colchicine (anti-gout) "Microtubules Get Constructed Very Poorly"
question
Chédiak-Higashi syndrome
answer
Microtubule polymerization defect resulting in decr phagocytosis. Results in recurrent pyogenic infxns, partial albinism, and peripheral neuropathy.
question
Cilia structure
answer
9 + 2 arrangement of MT's.
question
Axonemal dynein
answer
ATPase that links peripheral 9 doublets and causes bending of cilium by differential sliding of doublets.
question
Kartagener's syndrome
answer
Immotile cilia due to a dynein arm defect. Results in male and female infertility (sperm/fallopian cillia immotile) inc risk of ectopic preg, bronchiectasis, and recurrent sinusitis (bacteria and particles not pushed out); associated w/ situs inversus.
question
Actin and myosin
answer
Microvilli, Muscle contraction, Cytokinesis, Adherens jxn actins long, structural polymers myosins dimeric, ATP driven motor that move on actin
question
Microtubules (what structures are they found in?)
answer
Cilia Flagella Mitotic spindle Neurons Centrioles axonal trafficking
question
Intermediate filaments
answer
Vimentin, Desmin, Cytokeratin, lamins, Glial fibrillary acid proteins (GFAP) Neurofilaments
question
Plasma membrane composition
answer
Asymmetric bilayer. Contains chol, phospholipid, sphingolipids, glycolipids, and proteins. High XOL or long saturated FA content --< incr melting temp, decr fluidity.
question
Vimentin stain
answer
Connective tissue intermediate filament
question
Desmin stain
answer
muscle intermediate filament
question
Cytokeratin stain
answer
epithelial cells intermediate filament
question
GFAP stain
answer
neuroglia intermediate filament
question
neurofilament stain
answer
neurons intermediate filament
question
Polymerase chain reaction (PCR): What is it? What are the steps?
answer
Molecular biology laboratory procedure used to amplify a desired fragment of DNA. 1.) Denaturation -- DNA is denatured by heating to generate 2 separate strands. 2.) Annealing -- during cooling, excess premade DNA primers anneal to a specific sequence on each strand to be amplified. 3.) Elongation -- heat-stable DNA polymerase replicates the DNA sequence following each primer 3 steps are repeated multiple times for DNA sequence amplification.
question
Mnemonic for different blotting procedures
answer
"SN oW DR oP " Southern = DNA Northern = RNA Western = Protein
question
Southern blot
answer
A DNA sample is electrophoresed on a gel and then transferred to a filter. The filter is then soaked in a denaturant and subsequently exposed to a labeled DNA probe that recognizes and anneals to its complementary strand. The resulting ds labeled piece of DNA is visualized when the filter is exposed to film.
question
Northern blot
answer
Similar technique [to Southern], except that Northern blotting involves radioactive DNA probe binding to sample RNA . used for mRNA levels: gene expression
question
Western blot.
answer
Sample protein is separated via gel electrophoresis and transferred to a filter. Labeled Ab is used to bind to relevant protein . HIV after +ELIZA
question
Southwestern blot
answer
identifies DNA-binding proteins (ie TFs) uses labeled oligonucleotide probes
question
Microarrays
answer
Thousands of nucleic acid sequences are arranged in grids on glass or silicon. DNA or RNA probes are hybridized to the chip, and a scanner detects the relative amts of complementary binding. Used to profile gene expression levels or to detect single nucleotide polymorphisms (SNPs) and copy number variations (CNV) genotyping, clinical genetic tests, forensic, CA mutations, genetic linkage analysis
question
Enzyme-Linked Immunosorbent Assay (ELISA): What is it? What is it used for? How reliable is it?
answer
A rapid immunologic technique used to test patients blood for direct or indirect evidence of an antigen: direct: test antibody to see if patient antigen present indirect: test antigen to see if pt antibody present ie: test for presence of pt anti-HIV Both the sensitivity and the specificity of a ELISA approach 100%, but both false (+) and false (-) occur.
question
Sodium pump
answer
Na+/K+ ATPase is located in the plasma membrane w/ ATP site on cytoplasmic side. For each ATP consumed, 3 Na+ OUT and 2 K+ IN During cycle, pump is phosphorylated.
question
Ouabain
answer
Inhibits sodium pump (Na+/K+) by binding the K+ site.
question
Cardiac glycosides (digoxin and digitoxin)
answer
Directly inhibit Na+/K+ ATPase, which leads to indirect inhibition of Na+/Ca2+ exchange. ? Ca2+ ? ? cardiac contractility.
question
Type I collagen Where is this type of collagen found?
answer
90% of total Bone, skin, tendon, dentin, fascia, cornea late wound repair Type I = bONE ? production in OI type 1
question
Type II collagen Where is this type of collagen found?
answer
Cartilage (including hyaline), vitreous body, nucleous pulposus. Type II = carTWO lage
question
Type III collagen Where is this type of collagen found?
answer
(Reticulin) Skin, blood vessels, uterus, fetal tissue, granulation tissue ? in uncommon vascular type of ehlers-danlos "ThreE D"
question
Type IV collagen Where is this type of collagen found?
answer
Basement membrane, basal lamina, lens Type IV = Under the floor defect in alport, AB in goodpastures
question
Collagen Synthesis process

answer
1. ? chains translated @ RER to preprocollagen (gly-X-Y, where X and Y are usually pro and lys) 2. specific pro and lys are hydroxylated @ RER (requires vit C, or scurvy if deficiency) 3. glycosylate hydroxylysine residues to form pro-?-chain @ RER, then procollagen triple ? helix forms with hydrogen and disulfide bonding (OI if problem forming triple helix) 4. procollagen exocytosed into extracellular space 5. peptide cleavage of terminal ends to form insoluble tropocollagen 6. many tropocollagens reinforced with covalent lys-hydroxylys cross-linkage to form fibrils (done with copper-containing lysyl oxidase--ehlers-danlos if xlink problem)
question
Ehlers-Danlos syndrome features
answer
Faulty collagen synthesis, causing: 1.) Hyperextensible skin 2.) Tendency to bleed (easy bruising) 3.) Hypermobile joints 6+ types, varying degrees of severity autosomal dominant or recessive may be associated with Joint dislocation, Berry aneurysms, Organ rupture, aortic aneurysm
question
Types of Ehlers-Danlos
answer
hypermobile joint type: most common classical type (joint and skin) mutation type 5 collagen vascular type (vasc and organ rupture) type 3 collagen
question
Osteogenesis imperfecta: most common form
answer
AD: ? production of otherwise normal type I collagen 1.) Multiple fractures w/ minimal trauma; may occur during the birthing process. 2.) Blue sclera due to the translucency of the connective tissue over the choroid. 3.) Hearing loss (abnormal middle ear bones) 4.) Dental imperfections due to lack of dentin
question
Type II osteogenesis imperfecta
answer
Fatal in utero or neonatal period.
question
Menkes Disease
answer
connective tissue disease due to improper copper absorption and transport ?lysyl oxidase activity (the enzyme that x-links collagen) brittle "kinky" hair, growth retardation, hypotonia
question
Alport's syndrome: Due to....? Most common form...?
answer
Due to a variety of gene defects resulting in abnormal type IV collagen. (type IV collage is an imp. strxrl component of the basement membrane of the kidney, ears, and eyes) Most common form is X-linked recessive.
question
Alport's syndrome: Characterized by...? Associated with...?
answer
Characterized by progressive hereditary nephritis and deafness. May be associated w/ ocular disturbances.
question
Elastin
answer
lungs, skin, large arteries, elastic ligaments, vocal cords, ligamenta flava Rich in proline and Glycine, nonhydroxylated forms Tropoelastin w/ fibrillin scaffolding. Broken down by elastase, which is normally inhibited by alpha1-antitrypsin. cross-linking takes place extracellulary and give elastin its elastic properties
question
Marfan's syndrome (cause)
answer
Caused by a defect in fibrillin, a glycoprotein that forms a sheath around elastin
question
Emphysema (one cause)
answer
Can be caused by alpha1-antitrypsin deficiency, resulting in excess elastase activity ? breaks down elastin
question
Fluoresence in situ Hybridization (FISH)
answer
Fluorescent DNA or RNA probe binds to specific gene site of interest. Used for specific localization of genes and direct visualization of anomalies (e.g., microdeletions) at molecular level (when deletion is too small to be visualized by karyotype). Fluorescence = gene is present; no fluorescence = gene has been deleted.
question
Sanger DNA sequencing
answer
Dideoxynucleotides halt DNA polymerization at each base, generating sequences of various lengths that encompass the entire original sequence. Terminated fragments are electrophoresed and the original sequence can be deduced.
question
Cre-lox system in model systems
answer
A gene can be manipulated at specific developmental points using an inducible Cre-lox system with an ABX-controlled promoter (e.g., to study a gene whose deletion causes an embryonic lethal).
question
RNAi
answer
dsRNA is synthesized that is complementary to the mRNA sequence of interest. When transfeccted into human cells, dsRNA separates and promotes degradation of target mRNA, knocking down gene expression.
question
Karyotyping
answer
A process in which metaphase chromosomes are stained, ordered, and numbered according to size, arm-length ratio, and banding pattern. Can be performed on a sample of blood, bone marrow, amniotic fluid, or placental tissue. Used to Dx chromosomal imbalances (e.g., autosomal trisomies, microdeletions, sex chromosome d/o's).
question
Genetic terms: Codominance
answer
both alleles in heterozygote contribute to phenotype blood groups alpha-1 antitrypsin def
question
Genetic terms: Variable expression
answer
phenotype varies among people with same genotype NF1 have varying disease severity
question
Genetic terms: Incomplete penetrance
answer
Not all individuals w/ a mutant genotype show the mutant phenotype. BRCA 1 do not always cause breast and ovarian CA
question
Genetic terms: Pleiotropy
answer
single gene ? multiple phenotypic effects. PKU ? light skin, MR, musty body odor
question
Genetic terms: Loss of heterozygosity
answer
If a patient inherits or develops a mutation in a tumor suppressor gene, the complementary allele must also be deleted/mutated before cancer develops. This is NOT true of oncogenes. RB requires 2 hits
question
Genetic terms: Dominant negative mutation
answer
Exerts a dominant effect . A heterozygote produces a nonfxnl altered protein that also prevents the normal gene product from functioning. TF mutation?nonfxn, but still bind preventing wild type binding
question
Genetic terms: Linkage disequilibrium
answer
Tendency for certain alleles at 2 linked loci to occur together more often than expected by chance. Measured in a population, not in a family, and often varies in different populations.
question
Genetic terms: Mosaicism
answer
Occurs when cells in the body have distinct genetic makeup (e.g., lyonization -- random X inactivation in females) mitotic error after fertilization somatic: propagates through multiple tissues and organs gonadal: mutation only in egg or sperm mcCune-albright: lethal if mutation is somatic, can survive if mosaic
question
Genetic terms: Locus heterogeneity
answer
Mutations at DIFFERENT loci can produce the SAME phenotype albinism
question
Allelic heterogeneity
answer
different MUTATIONS @ SAME loci can give same phenotype ?-thalassemia
question
Genetic terms: Heteroplasmy
answer
Presence of both normal and mutated mtDNA, resulting in variable expression in mitochondrial inherited dz's.
question
Genetic terms: Uniparental disomy
answer
Offspring receives 2 copies of a chromosome from 1 parent and no copies from the other parent. heterodisomy (heterozygous) indicates meiosis 1 error isodisomy: meiosis 2 error or post zygotic chrom duplication of one pair, and loss of the other origninal pair euploid (correct # of chromosomes!) normal phenotype suspect if pt presents with AR disease and only 1 parent is carrier
question
Hardy-Weinberg equilibrium
answer
If a population is in H-W equilibrium and p and q are separate alleles, then: p² + 2pq + q? = 1 p + q = 1 prevalence of an X-linked recessive dz in males = q and in females = q² assumes: no mutation @locus natural selection NOT occurring completely random mating no net migration
question
Imprinting (def.)
answer
At a single locus, only 1 allele is active; the other is inactive (imprinted/inactivated by methylation). Deletion of the single active allele --> dz Most common example: Prader-Willi and Angelman's syndromes due to mutation/deletion @ chromosome 15 (can also result from uniparental disomy)
question
Prader-Willi Syndrome
answer
MATERNAL imprinting: mom's genes imprinted/silent + dad's deleted/mutated @ chromosome 15 Mental retardation, hyperphagia, obesity,, hypogonadism, hypotonia. 25% dute to maternal uniparental disomy
question
Angelman's syndrome
answer
PATERNAL imprinting: dad's genes imprinted/silent + mom's mutated/deleted @ chromosome 15 inappropriate laughter ("happy puppet") severe MR, seizures, ataxia 5% paternal uniparental disomy
question
Autosomal dominant
answer
structural gene defect often pleiotropic FHx crucial to dx
question
Autosomal recessive
answer
enzyme defect more severe than dominant may only be seen in 1 generation presents in childhood
question
X-linked dominant.
answer
females transmit to 50% of sons and daughters males transmit to all daughters but no sons Hypophosphatemic rickets
question
Hypophosphatemic rickets
answer
X-linked dominant dz Formerly known as vitamin D-resistant rickets ? phosphate wasting at proximal tubule rickets-like presentation
question
Mitochondrial inheritance.
answer
Transmitted only thru mother. All offspring of affected females may show signs of dz. Variable expression in population or family due to heteroplasmy. mitochondrial myopathies
question
Mitochondrial myopathies
answer
rare, present with myopathy, lactic acidosis, and CNS disease 2nd to failure of oxidative phos mm bx shows "ragged red fibers" mitochondrial inheritance
question
Achondroplasia
answer
AD! Cell-signaling defect of fibroblasts growth factor (FGF) receptor 3. dwarfism; short limbs, but head and trunk are normal size. Associated w/ advanced paternal age.
question
ADPKD
answer
AD! Formerly known as adult polycystic kidney dz. bilateral, massive enlargement of kidneys due to multiple large cysts. 85% cases are due to a mutation in PKD1 @ chrom16 remainder due to PKD2 @ chrom4 Associated w/ polycystic liver dz, berry aneurysms, mitral valve prolapse
question
Familial adenomatous polyposis
answer
AD! Colon becomes covered w/ adenomatous polyps after puberty. Progresses to colon cancer unless resected. mutation @ APC gene on chrom 5 "5 letters in 'polyp' "
question
Familial hypercholesterolemia
answer
AD! Elevated LDL due to defective or absent LDL receptor. severe atherosclerotis early in life tendon xanthomas (classically in the Achilles tendon)
question
Hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome)
answer
AD! Inherited d/o of blood vessels. Findings: telangiectasia, recurrent epistaxis, skin discolorations, AVMs, GI bleeding, hematuria
question
Hereditary spherocytosis
answer
AD! spectrin or ankyrin defect hemolytic anemia, ? MCHC Splenectomy is curative.
question
Huntington's dz
answer
AD! depression, progressive dementia, choreiform mvmts, caudate atrophy, and ? GABA and ACh in the brain Chrom 4 ; trinucleotide repeat d/o: (CAG) "Hunting 4 food"
question
Marfan's syndrome
answer
AD! Fibrillin-1 gene mutation ? connective tissue d/o affecting skeleton, heart, and eyes. tall w/ long extremities, pectus excavatum, hyperextensive joints, arachnodactyly cystic medial necrosis of aorta ? aortic incompetence and dissecting aortic aneurysms, floppy mitral valve Subluxation of the lenses upward and temporally
question
Multiple endocrine neoplasias (MEN)
answer
AD! Several distinct syndromes (I, 2A, 2B) characterized by familial tumors of endocrine glands, including those of the pancreas, parathyroid, thyroid, and adrenal medula Men 2A and 2B associated w/ ret gene.
question
Neurofibromatosis type 1 (von Recklinghausen's dz)
answer
AD, 100% penetrance but variable expression café-au-lait spots, cutaneous neurofibromas NF 1 on chrom17 "17 letters in "von Recklinghausen" "
question
Neurofibromatosis type 2
answer
AD! Bilateral acoustic schwannomas, juvenile cataracts, meningiomas, ependymomas NF2 gene on chrom22 "type 2 = 22"
question
Tuberous sclerosis
answer
AD, Incomplete penetrance, variable presentation neurocutaneous + multi=organ involvement numerous benign hamartomas
question
von Hippel-Lindau dz
answer
AD! deleted VHL tumor suppressor @ chrom 3 numerous tumors, benign and malignant "Von Hippel-Lindau = 3 words for chromosome 3"
question
Autosomal recessive dz's (list)
answer
Albinism ARPKD Cystic fibrosis Glycogen storage dz's Hemochromatosis Mucopolysaccharidoses (except Hunter's), Sphingolipidoses (except Fabry's) Kartageners Phenylketonuria Sickle cell anemias Thalassemias Wilsons disease
question
Genetics of Cystic fibrosis
answer
Autosomal-recessive defect in CFTR gene on chromosome 7, commonly deletion of Phe 508. *Most common lethal genetic dz of Caucasians
question
CF genetics, pathophys
answer
AR defect @ CFTR gene on chrom7 (often Phe508 deletion) CFTR channel actively secretes Cl- into lungs and GI tract, and actively reabsorbs Cl- from sweat. misfolded protein ? retained in RER ? ? Cl (and H2O) secretion ? ? intracell Cl ? compensate ? Na reab via epi Na channels ? ? H20 reab ? abnrl thick mucus and negative transepi potential diff
question
"Other" problems in CF (besides those that result directly from defective Cl- channel)
answer
Recurrent pulmonary infxns (Pseudomonas), chronic bronchitis, bronchiectasis-;reticulonodular pattern on CXR pancreatic insufficiency (malabsorption and steatorrhea), meconium ileus in newborns, nasal polyps Infertility in males due to bilateral absence of vas deferens. Fat-soluble vitamin deficiencies (A, D, E, K). Can present as failure to thrive in infancy.
question
Dx of CF?
answer
Incr concentration of Cl- ions in sweat test (;60 meq/L) can present with contraction alkalosis and ?K (ECF like taking loop diuretic) bc ECF loss of H2O/Na and concomitant renal K/H wasting
question
Tx for CF?
answer
N-acetylcysteine to loosen mucous plugs (cleaves disulfide bonds w/in mucous glycoproteins). dornase alfa (DNAse) to clear PMN debris
question
X-linked recessive disease list
answer
"Be Wise, Fool's GOLD Heeds Silly HOpe" Bruton's agammaglobulinemia Wiskott-Aldrich syndrome Fabry disease G6PD deficiency Ocular albinism Lesch-Nyhan syndrome Duchenne's (and Becker's) muscular dystrophy Hemophilia A and B Hunter's syndrome Ornithine transcarbamylase deficiency
question
Duchenne's muscular dystrophy features
answer
X-linked recessive frame-shift mutation ? truncated dystrophin protein ? accelerated muscle breakdown. Weakness begins in pelvic girdle mm and progresses superiorly, Pseudohypertrophy of calf muscles due to fibrofatty replacement of muscle, gower maneuver dilated cardiomyopathy is common cause of death Onset before 5 yrs of age. ? CPK and aldolase western blot and muscle biopsy confirm
question
Becker's muscular dystrophy
answer
X-linked POINT mutation @ dystrophin gene Less severe than Duchenne's Onset in adolescence or early adulthood.
question
Dystrophin gene (DMD )
answer
(associated w/ Duchenne's and Becker's muscular dystrophies) The longest known human gene ? ? rate of spontaneous mutation. Dystrophin helps anchor muscle fibers, primarily in skeletal and cardiac muscle: connects intracellular cytoskeleton (actin) to transmembrane proteins alpha, beta dystroglycan (connected to ECM) loss causes myonecrosis
question
myotonic type 1 muscular dystrophy
answer
CTG repeat @ DMPK gene?abnrl expression of myotonin protein kinase myotonia, muscle wasting, frontal balding, cataracts, testicular atrophy, arrythmias
question
Fragile X syndrome
answer
X-linked defect affecting the methylation and expression @ FMR1 gene, CGG trinucleotide repeat Macro-orchidism post-puberty (enlarged testes), long face w/ a large jaw, large everted ears, autism, mitral valve prolapse "fragile X = Xtra large testes, ears, jaw"
question
Trinucleotide repeat expansion dz's
answer
HUNTing for MY FRIED eggs (X) huntingtons: CAG myotonic dystrophy: CTG friedreich ataxia: GAA fragile X: CGG
question
D own syndrome findings
answer
Mental retardation flat facies prominent epicanthal folds single palmar crease gap btw 1st 2 toes duodenal atresia hirschsprungs congenital heart (most commonly septum primum-type ASD) brushfield spots ? risk of ALL, AML, Alzheimer's dz (> 35 yrs of age)
question
Down syndrome genetic cause
answer
1:700 95% meiotic nondisjunction of homologous chromosomes 5% Robertsonian translocation 1% mosaicism (no maternal association, post fert mitotic error)
question
Down syndrome preg screen
answer
1st tri: US + labs nuchal translucency + hypoplastic nasal bone ? PAPP-A, ? free B-hCG 2nd tri: quad screen ? AFP, ? B-hCG, ? estriol, ? inhibin A
question
Edward's syndrome findings
answer
trisomy 18, 1:8000 Severe mental retardation Rocker-bottom feet micrognathia Low-set ears Clenched hands Prominent occiput Congenital heart dz Death usually occurs w/in 1 yr of birth. "Edwards, Ears, Election (18)"
question
Edwards Syndrome: Labs
answer
first tri: ?PAPP-A, ?free B-hCG quad: ? all AFP, B-hCG, estriol, ?/nrl inhibin A
question
P atau's syndrome Findings?
answer
trisomy 13, 1:15000 Severe mental retardation Rocker-bottom feet Microphthalmia Microcephaly Cleft lip/palate holoProsencephaly Polydactyly Congenital heart dz Death usually occurs w/in 1 yr of birth. "P: Patau, liP/Palate, holoProsencephaly, Polydactlyly, Puberty (13)"
question
Patau Syndrome labs
answer
first tri screen: ?free B-hCG, PAPP-A +nucal translucency
question
Robertsonian translocation
answer
13, 14, 15, 21, and 22 One of the most common types of translocation. Occurs when the long arms of two acrocentric chromosomes (chromosomes w/ the centromeres near the ends) fuse at the centromere and the 2 short arms are lost.
question
Robertsonian translocation: balanced vs. unbalanced translocations?
answer
Balanced translocations normally do not cause any abnormal phenotype. Unbalanced translocations can result in miscarriage, stillbirth, and chromosomal imbalance (e.g., Down syndrome, Patau's syndrome).
question
Cri-du-chat syndrome
answer
Congenital microdeletion of short arm of Chr 5 (46,XX or XY,5p-) Microcephaly Moderate to severe mental retardation, High-pitched crying/mewing Epicanthal folds Cardiac abnormalities (VSD)
question
Williams syndrome
answer
Congenital microdeletion of long arm of Chr 7 (deleted region includes elastin gene) Distinctive "elfin" facies Mental retardation hypercalcemia, ? sensitivity to vitD Well-developed verbal skills Cheerful disposition Extreme friendliness w/ strangers Cardiovascular problems "williams founded in 1793"
question
22q11 deletion syndromes
answer
"CATCH-22" : aberrant development of 3rd and 4th branchial pouches Variable presentation, including: Cleft palate Abnormal facies Thymic aplasia ? T-cell deficiency Cardiac defects Hypocalcemia secondary to parathyroid aplasia 22q11 microdeletion ie DiGeorge, Velocardiofacial syndromes
question
DiGeorge syndrome
answer
thymic, parathyroid, and cardiac defects. 22q11 deletion syndrome
question
Velocardiofacial syndrome
answer
palate, facial, and cardiac defects. 22q11 deletion syndrome
question
Water soluble vitamin deficiencies
answer
water-soluble vitamins: all vitBs + vitC All wash out easily from body except B12 and folate/B9 (stored in liver). B-complex deficiencies often result in dermatitis, glossitis, and diarrhea.
question
Vitamin A (retinol): fxn? use? where is it found?
answer
liver and leafy vegetables Antioxidant; constituent of visual pigments (retinal). essential for diff of epi cells to special tissue (panc, mucus-secreting cells) prevents squamous metaplasia. used to tx measles, AML M3
question
Vitamin A (retinol) deficiency?
answer
Night blindness (nyctalopia), dry, scaly skin (xerosis cutis) alopecia corneal degen (keratomalacia) immune suppression
question
Vitamin A (retinol) excess?
answer
Arthralgias skin changes ( scaliness) alopecia cerebral edema pseduotumor cerebri osteoporosis hepatic abnrl Teratogenic (cleft palate, cardiac abnormalities).
question
Vitamin B1: fxn?
answer
=thiamine TPP: a cofactor for several dehydrogenase enzymes 1.) Pyruvate dehydrogenase (link glycolysis to TCA) 2.) alpha-ketoglutarate dehydrogenase (TCA cycle) 3.) Transketolase (HMP shunt) 4.) Branched-chain ketoacid dehydrogenase "ATP: ?-Ketoglutarate, Transketolase, Pyruvate dehydrogenase"
question
Vitamin B1 deficiency
answer
impaired glucose breakdown?atp depletion worsened by glucose infusion, high aerobic tissues (brain, heart) affected first Wernicke-Korsakoff syndrome and beriberi Seen in malnutrition as well as alcoholism (secondary to malnutrition and malabsorption). dx by ? RBC transketolase activity following B1 administration
question
Wernicke-Korsakoff syndrome
answer
Due to Vitamin B1 (thiamine) deficiency Triad: confusion, ophthalmoplegia, ataxia +confabulation, personality change, memory loss (permanant) damage to the medial dorsal nucleus of thalmus, mammilllary bodies
question
Beri-beri
answer
Due to Vitamin B1 (thiamine) deficiency. Dry beriberi - polyneuritis, symmetrical muscle wasting. Wet beriberi - high-output cardiac failure (dilated cardiomyopathy), edema.
question
Vitamin B2: fxn?
answer
= riboflavin component of FAD, DMN cofactor in redox rxns eg: the succinate dehydrogenase rxn in TCA
question
Vitamin B2 deficiency?
answer
=riboflavin "the 2 Cs of vitB2" Cheilosis (inflammation of lips, scaling and fissures at corners of mouth), Corneal vascularization
question
Vitamin B3: fxn?
answer
=niacin Constituent of NAD+, NADP+ used in redox rxns Derived from tryptophan Synthesis requires vitaminB2 and B6. tx dyslipidemia, lower VLDL and raises HDL
question
Vitamin B3 deficiency?
answer
=niacin Glossitis Severe deficiency leads to pellagra Pellagra: dermatitis, dementia, diarrhea can be caused by Hartnup dz (? tryptophan absorption), malignant carcinoid syndrome (? tryptophan metabolism), and isoniazid (? vitamin B6)
question
Vitamin B3 excess?
answer
=niacin Facial flushing (due to pharmacologic doses for Tx of hyperlipidemia) from prostaglandin, not histamine hyperglycemia, hyperuricemia
question
Vitamin B5: fxn and deficiency?
answer
=pantothenate component of coenzyme A cofactor for acyl transfer and FA synthesis deficiency: Dermatitis enteritis alopecia adrenal insufficiency
question
Vitamin B6 fxn?
answer
=pyridoxine Converted to PLP, a cofactor used in: transamination rxns (e.g., ALT and AST) decarboxylation rxns glycogen phosphorylase syn of cystathionine, heme, niacin, histamine, NT (serotonin, epi, NE, dopa, GABA)
question
Vitamin B6 deficiency?
answer
=pyridoxine Convulsions hyperirritability peripheral neuropathy (deficiency inducible by INH and BCP) sideroblastic anemia bc impaired Hb syn and Fe excess
question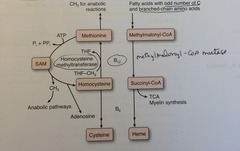
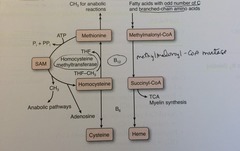
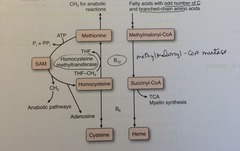
B12: fxn?
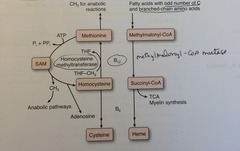
answer
=cobalamin Cofactor for homocysteine methyltransferase (transfers CH3 groups as methylcobalamin) and methylmalonyl-CoA mutase.
question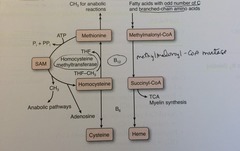
B12 (cobalamin): Deficiency?
answer
=cobalamin Macrocytic, megaloblastic anemia hypersegmented PMNs + neurologic Sx due to abnormal myelin: (paresthesias, subacute combined degeneration of dorsal column, lateral corticospinal and spinocerebellar tracts) Prolonged deficiency leads to irreversible nervous system damage. ? homocysteine AND methylmalonic acid
question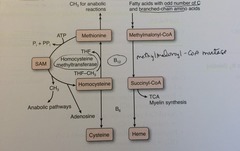
B12: what rxns does it help to proceed?
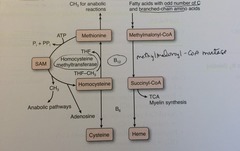
answer
=cobalamin Homocysteine + N-methyl THF --(B12 + homocysteine methyl transferase)--> Methionine + THF Methylmalonyl-CoA --(B12 + methylmalonyl-CoA mutase)--> Succinyl-CoA
question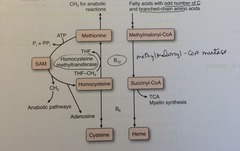
B12: etiology of deficiency?
answer
=cobalamin synthesized only by microorganisms, found in animal products Very large reserve pool (several yrs) stored primarily in liver. Deficiency is usually caused by malabsorption lack of intrinsic factor (pernicious anemia, gastric bypass surgery) absence of terminal ileum (Crohn's dz).
question
vit B9: fxn?
answer
=folic acid Converted to tetrahydrofolate (THF), a coenzyme for 1-carbon transfer/methylation rxns Important for the synthesis of nitrogenous bases in DNA and RNA
question
vit B9: deficiency?
answer
= folic acid Macrocytic, megaloblastic anemia hyperseg PMN glossitis NO neurologic Sx (opposite of vitB12 deficiency). Most common vitamin deficiency in the USA Alcoholism and Pregnancy. ?homocysteine, NORMAL methylmalonic acid
question
vit B9: where is it found?
answer
= folic acid FOLate is from FOLiage (green leaves) absorbed in jejunum
question
Etiology of folic acid deficiency?
answer
SMALL reserve pool stored primarily in liver (eat green leaves!) can be caused by several drugs (e.g., phenytoin, sulfonamides, MTX).
question
S-adenosyl-methionine (SAM): formation?
answer
ATP + methionine --> SAM
question
S-adenosyl-methionine (SAM): fxn?
answer
SAM transfers methyl units. Regeneration of methionine (and thus SAM) is dependent on vitamin B12 and folate. ("SAM the methyl donor man")
question
vit B7: fxn?
answer
biotin Cofactor for carboxylation enzymes: 1.) Pyruvate carboxylase : Pyruvate 3C ? oxaloacetate 4C 2.) Acetyl-CoA carboxylase : Acetyl-CoA 2C ? malonyl-CoA 3C 3.) Propionyl-CoA carboxylase : Propionyl-CoA 3C ? methylmalonyl-CoA 4C
question
vit B7: deficiency?
answer
=biotin Relatively rare. Dermatitis, alopecia, enteritis. Caused by ABX use or excessive ingestion of raw eggs. "AVID in in egg whites AVID ly binds biotin."
question
Vitamin C (ascorbic acid): fxn?
answer
Antioxidant. Also: 1.) Facilitates iron absorption by reducing to Fe2+ 2.) Necessary for hydroxylation of proline and lysine in collagen synthesis 3.) Necessary for dopamine Beta-hydroxylase, which converts dopamine to NE
question
Vitamin C (ascorbic acid): deficiency?
answer
Scurvy: swollen gums bruising anemia hemarthrosis poor wound healing perifollicular and subperiosteal hemorrhages corkscrew hair weak immune response
question
vit C excess
answer
NVD fatigue calcium oxalate nephrolithiasis ?Fe toxicity if transfusions, hemochromatosis
question
Vitamin D: forms?
answer
D2 = ergocalciferol: ingested from plants D3 = cholecalciferol: consumed in milk, formed in sun-exposed skin (basale) 25-OH D3 = storage form 1,25-(OH)2-D3 (calcitriol) = active form
question
Vitamin D: fxn?
answer
Incr intestinal absorption of calcium and phosphate, incr bone resorption
question
Vitamin D: deficiency?
answer
Rickets in children (bending bones, pain, deformity) osteomalacia in adults (soft bones, mm weakness), hypocalcemic tetany. breastfed infants should have oral Vit D ?risk if: low sun, pigmented skin, premie
question
Vitamin D: excess?
answer
Hypercalcemia, hypercalciuria, loss of appetite, stupor Seen in sarcoidosis (? activation of vitamin D by epithelioid macrophages)
question
Vitamin E: fxn?
answer
=tocopherol/tocotrienol Antioxidant (protects erythrocytes and membranes from free-radical damage). can enhance warfarin anticoagulant effects "E is for E rythrocytes"
question
Vitamin E: deficiency?
answer
Incr fragility of erythrocytes (hemolytic anemia) acanthocytosis muscle weakness posterior column and spinocerebellar tract demyelination neuro similar to B12, but no megaloblastic anemia, hyperseg PMN, or ? methylmalonic acid
question
Vitamin K: fxn?
answer
Catalyzes gamma-carboxylation of glutamic acid residues on various proteins concerned w/ blood clotting. activates II, VII, IX, X, protein C and S warfarin antagonizes vitK Synthesized by intestinal flora
question
Vitamin K: deficiency?
answer
Neonatal hemorrhage w/ incr PT and incr aPTT, but normal bleeding time (neonates have sterile intestines and are unable to synthesize vitamin K). Neonates are give vitamin K injection at birth to prevent hemorrhage. Can also occur after prolonged use of broad-spectrum ABX.
question
Zinc: fxn?
answer
Essential for the activity of 100+ enzymes. Important in the formation of Zinc fingers (a transcription motif)
question
Zinc: deficiency?
answer
Delayed wound healing hypogonadism ?adult hair (axillary, facial, pubic) dysgreusia, anosmia acrodermatitis enteropathica (oral/perianal dermatitis) May predispose to alcoholic cirrhosis.
question
Ethanol metabolism: kinetics/breakdown rxn

answer
NAD+ is the limiting reagent. Alcohol dehydrogenase operates via zero-order kinetics.
question
Fomepizole
answer
Inhibits alcohol dehydrogenase antidote for methanol or ethylene glycol poisoning
question
Disulfiram (antabuse)
answer
Inhibits acetaldehyde dehydrogenase (acetaldehyde accumulates, contributing to Sx of hangover)
question
Ethanol in liver
answer
? NADH/NAD+ ratio in liver, causing: pyruvate to lactate ? lactic acidosis oxaloacetate to malate ? inhibits gluconeogenesis ? fasting hypoglycemia glyceraldehyde-3P to glycerol-3P ? combines with FA to make TG ? fatty liver disfavors TCA prodxn of NADH ? ? utilize acetyl-CoA for ketogenisis and lipogenesis ? ketoacidosis, hepatosteatosis
question
Fomepizol v Disulfiram
answer
fomepizol: inhibits alcohol dehydrogenase antidote for methanol/ethylene glycol poisoning disulfiram: inhibits acetaldehyde dehydrogenase ?acetaldehyde ? ? hangover
question
Kwashiorkor
answer
Protein malnutrition ? skin lesions, edema, liver malfxn (fatty change bc ? apolipoprotein synthesis) Malnutrition Edema Anemia Liver (fatty)
question
Marasmus
answer
Total calorie malnutrition ? tissue and mm wasting, loss of subQ fat, and variable edema "Marasmus results in Muscle wasting"
question
Mitochondrial metabolic rxns
answer
Fatty acid oxidation (beta-oxidation) Acetyl-CoA production TCA cycle Oxidative phosphorylation
question
cytoplasmic metabolic rxns
answer
Glycolysis Fatty acid synthesis HMP shunt Protein synthesis (RER) Steroid synthesis (SER) cholesterol syn
question
Metabolism sites: both mitochondria and cytoplasm
answer
Heme synthesis Urea cycle Gluconeogenesis "HUGs take two "
question
Glycolysis What is the rate-limiting enzyme and reg
answer
Phosphofructokinase-1 (PFK-1) inc: AMP, fructose-2,6-bisphosphate dec: ATP, Citrate
question
Gluconeogenesis What is the rate-limiting enzyme and reg
answer
Fructose 1,6 bisphosphatase inc: ATP, acetyl-CoA dec: AMP, fructose-2,6-bisphosphate
question
TCA cycle What is the rate-limiting enzyme and reg
answer
Isocitrate dehydrogenase inc: ADP dec: ATP, NADH
question
Glycogen synthesis What is the rate-limiting enzyme and reg
answer
Glycogen synthase inc: G6P, insulin, cortisol dec: epi, glucagon
question
Glycogenolysis What is the rate-limiting enzyme and reg
answer
Glycogen phosphorylase inc: epi, glucagon, AMP dec: G6P, insulin, ATP
question
HMP shunt What is the rate-limiting enzyme and reg
answer
Glucose-6-phosphate dehydrogenase (G6PD) inc: NADP+ dec: NADPH
question
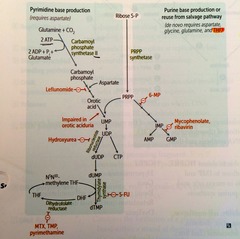
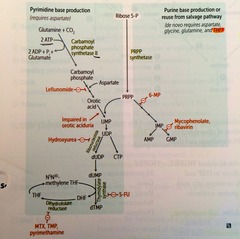
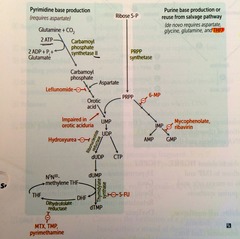
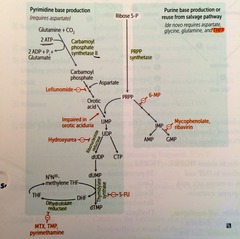
De novo pyrimidine synthesis What is the rate-limiting enzyme?
answer
carbamoyl phosphate synthase II
question
De novo purine synthesis What is the rate-limiting enzyme and reg
answer
Glutamine-PRPP amidotransferase dec: AMP, IMP, GMP
question
Urea cycle What is the rate-limiting enzyme and reg
answer
Carbamoyl phosphate synthetase 1 inc: n-acetylglutamate
question
Fatty acid synthesis What is the rate-limiting enzyme and reg
answer
Acetyl-CoA carboxylase (ACC) inc: insulin, citrate dec: glucagon, palmitoyl-CoA
question
Fatty acid oxidation What is the rate-limiting enzyme and reg
answer
Carnitine acyltransferase I dec: malonyl-CoA
question
Ketogenesis What is the rate-limiting enzyme?
answer
HMG-CoA synthase
question
Cholesterol synthesis What is the rate-limiting enzyme and reg
answer
HMG-CoA reductase inc: insulin, thyroxine dec: glucagon, cholesterol
question
Glycolysis/ATP production: quantitative
answer
Aerobic metabolism of glucose: 32 ATP via malate-aspartate shuttle (heart and liver) 30 ATP via glycerol-3-P shuttle (muscle) Anaerobic glycolysis produces only 2 net ATP per glucose molecule arsenic causes glycolysis to produce zero net ATP
question
Activated carriers: Coenzyme A, lipoamide carry?
answer
Acyl
question
Activated carriers: Tetrahydrofolate carries?
answer
1-carbon units
question
Activated carriers: SAM carries?
answer
CH3 groups
question
Activated carriers: TPP carries?
answer
Aldehydes
question
NAD+ vs. NADPH
answer
NAD+ is generally used in catabolic processes to carry reducing equivalents away as NADH NADPH is used in anabolic processes (steroid and FA synthesis) as a supply of reducing equivalents.
question
NADPH: Product of...? Used in... (4 things)?
answer
Product of the HMP shunt. Used in: 1.) Anabolic processes 2.) Respiratory burst 3.) cytP450 4) glutathione reductase
question
Hexokinase vs. glucokinase: Location?
answer
Hexokinase: ubiquitous. Glucokinase: Liver and Beta-cells of pancreas only.
question
Hexokinase vs. glucokinase: Affinity / Capacity?
answer
Hexokinase: high affinity (low Km), low capacity (low Vmax) Glucokinase: Low affinity (high Km), high capacity (high Vmax)
question
Hexokinase vs. glucokinase: response to insulin?
answer
Hexokinase: uninduced by insulin Glucokinase: induced by insulin
question
Hexokinase vs. glucokinase: Feedback?
answer
Hexokinase: Feedback inhibited by glucose-6-phosphate. Glucokinase: No direct feedback inhibition.
question
Net glycolysis rxtn (cytoplasm)
answer
Glucose + 2 Pi + 2 ADP + 2 NAD+ ? 2 pyruvate + 2 ATP + 2 NADH + 2 H+ + 2H2O
question
Steps in glycolysis that require ATP: Regulation?
answer
glucose-> G6P (hex/glucokinase) G6P inhibit hexokinase, F6P inhibit glucokinase F6P -> F1,6BP (PFK1) -: ATP, citrate +: AMP, F26BP
question
Steps in glycolysis that produce ATP: Regulation?
answer
1,3BPG->3PG (phosphoglycerate kinase) phosphoenolpyruvate->pyruvate (pyruvate kinase) -: ATP, alanine +: F16BP
question
Regulation by fructose-2,6-bisphosphate fasting and fed
answer
fasting: ?glucagon ? ?cAMP ? ?PKA ? ?FBPase2/?PFK2 ? ?gluconeogenesis/?glycolysis fed: ?insulin ? ?cAMP ? ?PKA ? ?PFK2/?FBPase2 ? ?glycolysis/?gluconeogenesis
question
Pyruvate dehydrogenase: net rxn?
answer
Pyruvate + NAD+ + CoA ? acetyl-CoA + CO2 + NADH active in fed state connects glycolysis and TCA
question
Pyruvate dehydrogenase complex: 3 enzymes that require what 5 cofactors?
answer
B1/2/3/5 lipoic acid arsenic inhibits lipoic acid ? vomiting, rice-water stools, garlic breath activated by exercise: ?NAD/NADH ratio, ?ADP, ?Ca similar to ?KG-dehydrogenase complex (same exact cofactors needed)
question
what inhibits PDH
answer
ATP NADH Acetyl-CoA
question
Pyruvate dehydrogenase deficiency: MoA, s/sx, tx
answer
buildup of pyruvate, shunted to lactate (LDH) and alanine (ALT) neuro defects, lactic acidosis, ? serum alanine starting in infancy tx: inc intake of ketogenic nutrients (high fat, inc lysine and leucine)
question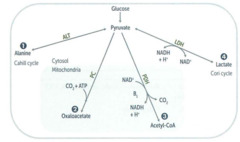
Pyruvate metabolism: Alanine?
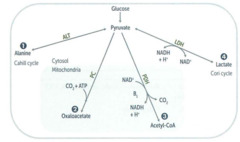
answer
via Alanine aminotransferase + B6 carries amino groups to the liver from muscle
question
Pyruvate metabolism: oxaloacetate?
answer
via Pyruvate carboxylase, + biotin can replenish TCA cycle or be used in gluconeogenesis
question
Pyruvate metabolism: Lactate?
answer
via LDH + B3 End of anaerobic glycolysis major pathway in RBCs, leukocytes, kidney medulla, lens, testes, and cornea
question
Pyruvate metabolism: Acetyl-CoA
answer
via pyruvate dehydrogenase (B1,2,3,5,lipoic acid) transition from glycolysis to the TCA cycle
question
Cori cycle
answer
Allows lactate generated during anaerobic metabolism to undergo hepatic gluconeogenesis and become a source of glucose for muscle/RBCs. This comes at a cost of a net loss of 4 ATP/cycle. Shifts metabolic burden to the liver.
question
Pyruvate --> acetyl-CoA produces what?
answer
1 NADH + 1 CO2
question
The TCA cycle (Krebs) produces what?
answer
3 NADH, 1 FADH2, 2 CO2, 1 GTP per acetyl-CoA = 10 ATP/acetyl-CoA (2x everything per glucose).
question
alpha-ketoglutarate dehydrogenase complex
answer
Part of TCA cycle. Requires the same cofactors as the pyruvate dehydrogenase complex (B1, B2, B3, B5, lipoic acid)
question
Enzymes of TCA (Krebs cycle)
answer
Can I Keep Selling Sex For Money Officer? Citrate Isocitrate alpha-keto-glutarate succinyl CoA succinate fumarate malate oxaloacetate
question
Oxidative phosphorylation poisons: ETC inhibitors?
answer
Directly inhibit electron transport, causing a LOWER proton gradient and block of ATP synthesis: rotenone antimicin A CN CO
question
Oxidative phosphorylation poisons: ATPase inhibitors
answer
Directly inhibit mitochondrial ATPase, causing an INCREASED proton gradient. No ATP is produced b/c electron transport stops: Oligomycin
question
Oxidative phosphorylation proteins: uncoupling agents
answer
Incr permeability of membrane, causing a LOWER proton gradient and incr O2 consumption. ATP synthesis drops, but electron transport continues, produces HEAT: 2,4-DNP, aspirin, thermogenin in brown fat.
question
Gluconeogenesis: irreversible enzymes
answer
Pathway Produces Fresh Glucose Pyruvate carboxylase: mitochondria PEPCK: cytosol F-1.6-BP: cytosol G-6-Pase: ER
question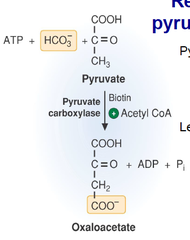
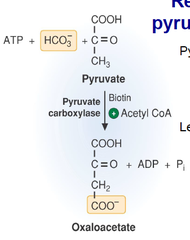
pyruvate carboxylase
answer
gluconeogenesis In mitochondria. Pyruvate --> Oxaloacetate. Requires biotin, ATP Activated by acetyl-CoA.
question
PEPCK

answer
gluconeogenesis In cytosol Oxaloacetate --> phosphoenolpyruvate Requires GTP.
question
F-1,6-BPase
answer
gluconeogenesis cytosol Fructose-1,6-BP --> F6P + citrate - F2,6BP
question
G6Pase
answer
gluconeogenesis In ER G6P --> glucose mm lacks this enzyme so can't participate in gluconeogenesis
question
Fatty acids and gluconeogenesis
answer
Odd-chain FA's yield 1 propionyl-CoA during metabolism, which can enter the TCA cycle as succinyl-CoA, undergo gluconeogenesis, and serve as a glucose source. Even-chain FA's cannot produce new glucose, since they yield only acetyl-CoA equivalents.
question
HMP shunt (pentose phosphate pathway)
answer
Produces NADPH, which is req'd for FA and steroid biosynthesis and for glutathione reduction inside RBCs. also yields ribose for nucleotide synthesis and glycolytic intermediates 2 distinct phases (oxidative and non-oxidative), both of which occur in the CYTOPLASM. No ATP is used or produced.
question
HMP shunt (pentose phosphate pathway): Where does it occur (anatomically)?
answer
Lactating mamary glands, liver, adrenal cortex (sites of FA or steroid synthesis), RBCs
question
HMP shunt (pentose phosphate pathway): reactions

answer
oxidative irreversible, RLS
question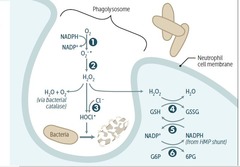
Respiratory burst (oxidative burst)
answer
1. NADPH oxidase: ? in CGD 2. superoxide dismutase 3. MPO (green heme-containing) 4. glutathione peroxidase (+selenium) 5. glutathione reductase (+selenium) 6. G6PD *if have CGD, catalase + organisms can ? H2O2 (s.aureus, aspergillus) **P.aeruginosa generates ROS to kill competing microbes
question
Lactoferrin
answer
protein in secretory fluids and PMNs that inhibits microbial growth via iron chelation
question
Glucose-6-Phosphate dehydrogenase deficiency: molecular explanation?
answer
NADPH is necessary to keep glutathione reducced, which in turn detoxifies free radicals and peroxides. Decr NADPH in RBCs leads to hemolytic anemia due to poor RBC defense against oxidizing agents (e.g., fava beans, sulfonamides, primaquine, antituberculosis drugs). ifxn can also cause hemoysis (free rad via inflam rsp can diffuse into RBC and cause ox damage)
question
Glucose-6-phosphate dehydrogenase deficiency:
answer
X-linked recessive ?G6P dehydrogenase ? ?NADPH ??reduced glutathione ?detoxification of ROS and peroxide RBC: hemolytic anemia, heinz bodies, bite cells flares with ?oxidative injury: antimalarials fava beans sulfonamides anti-TB Rx infection/inflammation more prevalent among blacks Incr malarial resistance
question
Fructose intolerance

answer
AR deficiency in aldolase B Fructose-1-phosphate accumulates, causing a decr in available phosphate, which results in inhibition of glycogenolysis and gluconeogenesis. Hypoglycemia, jaundice, cirrhosis, vomiting. ? intake of both fructose and sucrose (glu + fruc)
question
Essential fructosuria:

answer
AR defect in fructokinase A benign, asymptomatic condition, since fructose doesn't enter cells. Fructose appears in blood and urine (benign)
question
galactosemia:
answer
Absence of galactose-1-phosphate uridyltransferase . Autosomal recessive. Damage is caused by accumulation of toxic substances (including galactitol, which accumulates in the lens of the eye). Failure to thrive, jaundice, hepatomegaly, infantile cataracts, mental retardation. exclude galactose and lactose (galactose + glucose) from diet.
question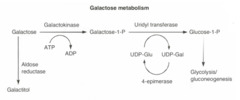
Galactokinase deficiency:
answer
AR deficiency of galactokinase . Galactitol accumulates if galactose is present in diet. Relatively mild condition. Galactose appears in blood and urine, infantile cataracts. May initially present as failure to track objects or to develop a social smile.
question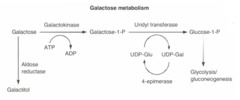
Classic Galactosemia
answer
AR Uridyltransferase deficiency galactitol accumulates in body, lens of eye failure to thrive, jaundice, hepatomegaly, infantile cataracts, MR *e.coli sepsis in neonates!
question
sorbitol

answer
alt method to trap glucose (via aldose reductase) some tissues then convert sorbitol to fructose by sorbitol dehydrogenase def (cataracts, retinopathy, perif neuropathy, seen with chronic hypergly in DM) lens, schwann cells, retina, and kidney only have aldose reductase
question
Lactase deficiency: lactose tolerance test findings
answer
stool dec pH, breath inc H content with lactose tol test biopsy nrl lactose ? glucose + galactose
question
Essential Glucogenic amino acids
answer
MetHisVal *his has no net charge @ body pH, but is basic
question
Essential AA's
answer
glucogenic: Met, His, Val ketogenic: Leu, Lys glu and keto: Phe, Trp, Thr, Ile
question
Acidic AA's
answer
Asp and Glu (negatively charged at body pH)
question
Basic AA's
answer
Arg, Lys, and His. Arg is the most basic, His has no charge at body pH Arg and His required during periods of growth Arg and Lys are elevated in histones
question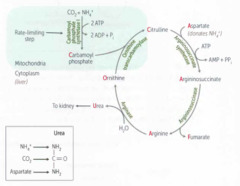
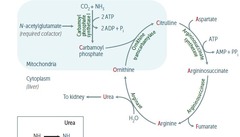
urea cycle
answer
Ordinarily, Careless Crappers Are Also Frivolous About Urination Ornithine Carbamoyl Phosphate Citrulline Aspartate Arginosuccinate Fumarate Urea *N-acetylglutamate required cofactor for Carbamoyl Phosphate Synthetase I
question
What do the atoms of urea come from?
answer
NH3, CO2, aspartate
question
Hyperammonemia
answer
Results in exccess NH4+ ? depletes alpha-ketoglutarate, leading to inhibition of the TCA cycle. Ammonia intoxication : tremor, slurring speech, somnolence, vomiting, cerebral edema, blurring of vision. tx: limit protein. bonzoate or phenylbutryate (both bind AA and lead to excretion may dec levels. lactulose to acidify GI and trap NH4
question
Hyperammonemia: tx
answer
limit protein benzoate or phenylbutryate (both bind AA and lead to excretion may dec levels) lactulose to acidify GI and trap NH4
question
n-acetylglutamate deficiency
answer
cofactor for carbamoyl phosphate synthase 1 cause hyperammonemia same as carbamoyl phosphate synthase 1, but consider if: ? ornithine with nrl urea cylcle enzyme suggestive
question
ornithine transcarbamylase def
answer
most common urea cycle disorder X-R (others AR) first few days of life excess carbamoyl phosphate converted to orotic acid (pyrimidine synthesis pathway) ? orotic acid in blood and urine, ? BUN, sx hyperammonia no megaloblastic anemia (vs orotic aciduria)
question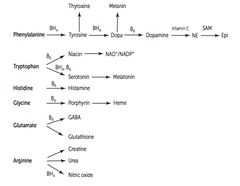
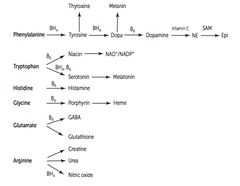
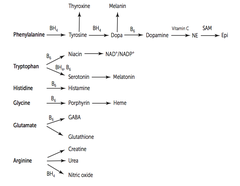
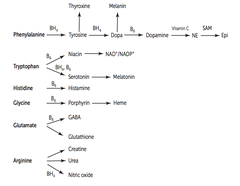
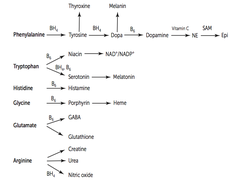
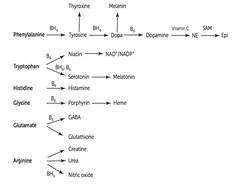
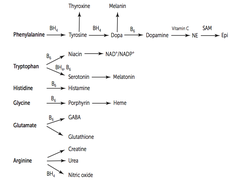
Phenylalanine derivatives
answer
1.) Phenylalanine -->(BH4)Tyrosine --> Thyroxine or Dopa (BH4) Dopa --> Melanin + Dopamine (B6) Dopamine --> (vit C) NE -->(SAM) Epi
question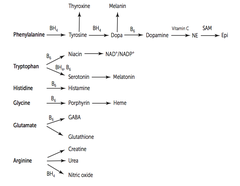
Tryptophan derivatives
answer
Tryptophan --(B6)> Niacin -> NAD/NADP typtophan->(BH4, B6)serotonin-> melatonin
question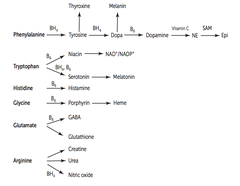
Histadine derivatives
answer
Histadine --(B6)> Histamine
question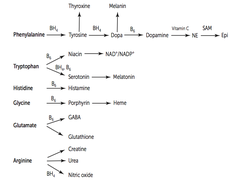
Glycine derivatives
answer
Glycine --(B6)> Porphyrin --> heme
question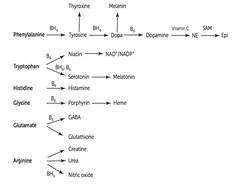
Arginine derivatives
answer
Arginine --> Creatinine, urea, NO (BH4)
question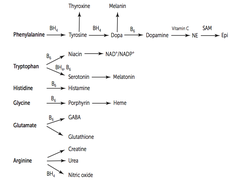
Glutamate derivatives
answer
Glutamate --(B6) GABA Glutamate --> Glutathione
question
catecholamine synthesis

answer
PKU: phenylalanine hydroxylase Alkaptonuria: homogentisate oxidase Albinism: tyrosinase
question
Phenylketonuria

answer
AR ? phenylalanine hydroxylase OR ? tetrahydrobiopterin cofactor (malig PKU) Mental retardation, growth retardation, seizures, fair skin, eczema, musty body odor screened 2-3 days after birth ? phenylalanine and ? tyrosine in diet.
question
Maternal PKU

answer
Lack of proper dietary therapy during pregnancy. Findings in infant: microcephaly, mental retardation, growth retardation, congenital heart defects.
question
Alkaptonuria (ochronosis)
answer
AR, benign deficiency of homogentisic acid oxidase in the degradative pathway of tyrosine to fumarate. Dark connective tissue pigmented sclera urine turns black on standing. May have debilitating arthralgias. (homogentisic acid toxic to cartilage)
question
3 Forms of homocystinuria and their txs

answer
1.) Cystathionine synthase deficiency: ?Met and ? Cysteine and B12 and folate in diet 2.) ? affinity of cystathionine synthase for pyridoxal phosphate: ??? vitB6 and cysteine in diet 3.) Homocysteine methyltransferase deficiency: ? methionine in diet *all AR
question
Homocysteinuria: s/sx

answer
??? homocysteine in urine mental retardation osteoporosis tall stature kyphosis lens subluxation (downward and inward) atherosclerosis (stroke and MI) thrombosis
question
Cystinuria: Etiology
answer
AR defect of renal PCT/intestinal AA transporter for COLA: cysteine ornithine lysine arginine hexagonal cystine urine stones *(cysteine=cysteine S=S bond) common (1:7000)
question
Cystinuria: dx, tx
answer
dx: urinary cyanide-nitroprusside test Tx: ? stone solubility acetazolamide and K-citrate to alkalinize urine chelating agents good hydration
question
Maple syrup urine dz: etiology?
answer
Blocked degradation of branched amino acids due to AR ? ?-ketoglutarate dehydrogenase (B1) ? ? ?-ketoacids in blood, esp leucine. I Love Vermont Maple Syrup: Isoleucine, Leucine, Valine severe CNS defects, MR, and death tx: dietary ILV restriction, thiamine supplements
question
Orotic aciduria: etiology? genetics?
answer
Inability to convert orotic acid UMP (de novo pyrimidine synthesis pathway) due to defect in either orotic acid phosphoribosyltransferase or orotidine 5'-phosphate decarboxylase. Autosomal recessive.
question
Orotic aciduria: findings?
answer
Incr orotic acid in urine megaloblastic anemia (does not improve w/ administration of vitamin B12 or folic acid) failure to thrive No hyperammonemia (vs. OTC deficiency -- incr orotic acid w/ hyperammonemia).
question
Orotic aciduria: Tx?
answer
Oral uridine administration.
question
Glycogen regulation by insulin and glucagon/epi

answer
glucagon and epi (?adrenergic @ liver, mm): ?AC ? ?cAMP ? ?PKA ? phosphorylate/activate glycogen phosphorylase kinase ? glycogenolysis ? ? glucose (PKA also inhibits glycogen synthase) epi @ liver ?-adrenergic also activates glycogen phosphorylase kinase but via ?Ca insulin activates glycogen synthase AND protein phosphatase ? inactivates glycogen phosphorylase ? glycogenesis ? ? glycogen, ? glucose
question
Phosphorylation and Insulin vs. Glucagon
answer
Insulin dephosphorylates (? cAMP --> ? PKA) Glucagon phosphorylates (? cAMP --> ? PKA)
question
Glycogen structure
answer
Branches have alpha(1,6) bonds; Linkages have alpha(1,4) bonds.
question
Glycogen metabolism: mm vs liver
answer
mm: glycogen ? G1P ? G6P ? rapidly metabolized liver: glycogen stored ? glycogenolysis to maintain BGL during fast
question
Glycogen metabolism
answer
1. UDP-glucose pyrophosphorylase 2. glycogen synthase 3. branching enzyme 4. glycogen phosphorylase 5./6. debranching enzyme
question
Glycogen storage diseases
answer
Very Poor Carb Metabolism Von Gierke (type I) Pompe (type II) Cori (type III) McArdle (type IV) *all AR
question
Von Gierke's Disease (type I)
answer
? Glucose-6-phosphatase severe fasting hypoglycemia, ??? glycogen in liver, ? blood lactate, hepatomegaly tx: frequent oral glucose, avoid fructose and galactose
question
Pompe's dz (type II)
answer
? Lysosomal ?-1,4 glucosidase (acid maltase) cardiomegaly and systemic findings leading to early death "Pompe's trashes the Pump (heart, liver, and muscle)."
question
Cori's dz (type III)
answer
? Debranching enzyme (?-1,6-glucosidase) milder form of type I w/ normal blood lactate levels Gluconeogenesis is intact.
question
McArdle's dz (type V)
answer
? Skeletal muscle glycogen phosphorylase (myophosphorylase) ? glycogen in muscle but cannot break it down ? painful muscle cramps, myoglobinuria (red urine) w/ strenuous exercise, arrythmia from electrolyte abnormalities
question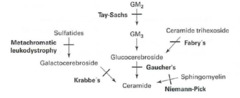
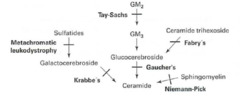
Fabry Disease
answer
XR! lysosomal storage disease (sphingo) ? ?-galactosidase A ? ? Ceramide trihexoside peripheral neuropathy of hands/feet angiokeratomas CV/renal dz
question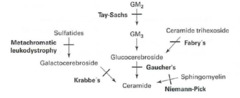
Gaucher Disease
answer
AR lysosomal storage disease (sphingo) ??-glucocerebrosidase ? ?glucocerebroside hepatosplenomegaly pancytopenia aseptic necrosis of femur, bone crises Gaucher's cells (lipid laden macrophages that look like crumpled tissue paper) tx: recombinant glucocerebrosidase most common, Ashkenazi Jews
question
Niemann-Pick dz
answer
AR lysosomal storage disease (sphingo) ? sphingomyelinase ? ?sphingomyelin progressive neurodegeneration hepatosplenomegaly cherry-red spot on macula foam cells (lipid in macro) Ashkenazi Jews "No Man Picks his nose with his sphinger"
question
Tay-Sachs dz
answer
AR lysosomal storage disease (sphingo) ?hexosaminidase A ? ? GM2 ganglioside progressive neurodegeneration, developmental delay lysosome with onion skin cherry red spot on macula no hepatosplenomegaly. Ashkenazi Jews "Tay SaX"
question
Krabbe's dz F
answer
AR lysosomal storage disease (sphingo) ?Galactocerebrosidase ? ? Galactocerebroside, psychosine Peripheral neuropathy developmental delay optic atrophy globoid cells
question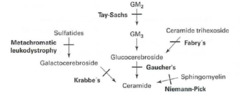
Metachromatic leukodystrophy
answer
AR lysosomal storage disease (sphingo) ?Arylsulfatase A ? ?Cerebroside sulfate central and peripheral demyelination ataxia dementia
question
Hurler's syndrome
answer
AR lysosomal storage disease (muco) ?alpha-L-iduronidase ? ?Heparan sulfate, dermatan sulfate developmental delay gargoylism airway obstruction corneal clouding hepatosplenomegaly
question
Hunter's syndrome
answer
XR lysosomal storage disease: mucopolysaccaridoses ?Iduronate sulfatase ? ?Heparan sulfate, dermatan sulfate Mild Hurler's + aggressive behavior NO corneal clouding "Hunters see clearly and aggressively aim for the X"
question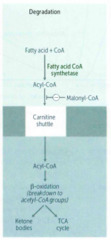
Carnitine deficiency
answer
Inability to transport LCFAs into mitochondrial matrix ? toxic accumulation weakness hypotonia HYPOketotic hypoglycemia
question
Acyl-CoA dehydrogenase deficiency
answer
? Acetyl-CoA ? ?fasting glucose (Acetyl-CoA is a stimulating allosteric regulator of Pyruvate Carboxylase in gluconeogenesis) ?dicarboxylic acids ?glucose and ketones
question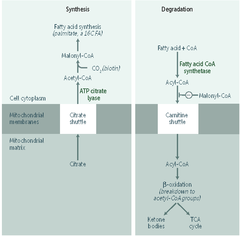
Fatty acids: synthesis v degradation
answer
SYtrate SYnthesis CARnitine CARnage
question
Ketone bodies: in prolonged starvation or diabetic ketoacidosis? ... in alcoholism?
answer
In prolonged starvation or diabetic ketoacidosis, oxaloacetate is depleted for gluconeogenesis In alcoholism, excess NADH shunts oxaloacetate to malate Both processes cause ? acetyl-CoA ? ?TCA cycle ? shunts glucose and FFA to prodxn of ketone bodies.
question
Ketone bodies: made from...? How are they metabolized in brain? How are they excreted?
answer
Made from HMG-CoA. Metabolized in brain to 2 molecules of acetyl-CoA. Excreted in urine.
question
Metabolic fuel use: fasting and starvation -- days 1-3
answer
Blood glucose is maintained by: 1. Hepatic glycogenolysis 2. Adipose release of FFA 3. mm and liver shifting fuel use from glucose to FFA 4. Hepatic gluconeogenesis from peripheral tissue lactate and alanine, and from adipose tissue glycerol and propionyl-CoA from odd-chain FFA metabolism (the only TG components that can contribute to gluconeogenesis)
question
Metabolic fuel use: fasting and starvation -- after day 3
answer
1. ketone bodies from adipose stores 2. after ketone bodies depleted, vital proteins degraded ? organ failure, death *amt of excess stores determines survival time **RBCs lack mitochondria, cannot use ketones
question
Cholesterol synthesis
answer
HMG-CoA ? mevalonate. catalyzed by HMG-CoA reductase (RLS) *HMG-CoA reductase: insulin +, statins - 2/3 of plasma cholesterol is esterified by lecithin-cholesterol acyltransferase (LCAT).
question
Lipid transport enzymes: Pancreatic lipase
answer
Degradation of dietary TG in small intestine
question
Lipid transport enzymes: Lipoprotein lipase (LPL)
answer
@ vasc endothelial surface: degrades TG circulating in chylomicrons and VLDLs
question
Lipid transport enzymes: Hepatic TG lipase (HL)
answer
Degradation of TG remaining in IDL
question
Lipid transport enzymes: Lecithin-cholesterol acyltransferase (LCAT)

answer
Catalyzes esterification of cholesterol
question
Lipid transport enzymes: Cholesterol ester transfer protein (CETP)

answer
Mediates transfer of chol-esters from HDL to other lipoprotein particles (VLDL, IDL, LDL)
question
Major apolipoproteins: E
answer
E mediates Extra (remnant) uptake chylo, chylo rem, VLDL, IDL, HDL *NOT on LDL
question
Major apolipoproteins: A-I
answer
A-I Activates LCAT (esterification) chylomicron, HDL "beginning and end, from A to Z"
question
Major apolipoproteins: C-II
answer
C-II is a Cofactor for LPL chylomicron, VLDL, HDL
question
Major apolipoproteins: B-48
answer
Mediates chylomicron secretion chylomicron, chylomicron remnant
question
Major apolipoproteins: B-100
answer
B -100 B inds to LDL receptor VLDL, IDL, LDL
question
Lipoprotein composition
answer
varying proportions of cholesterol, TGs, and phospholipids LDL and HDL carry most cholesterol
question
Chylomicron fxn
answer
secreted by intestinal epithelial cells dietary TGs to peripheral tissue cholesterol to liver as chylo remnant after most TGs depleted @ periphery
question
Chylomicron apolipoprotein content
answer
E A1 CII B48
question
VLDL fxn
answer
secreted by liver ? hepatic TGs to peripheral tissue
question
VLDL apolipoprotein content
answer
E CII B100
question
IDL fxn
answer
formed by VLDL degradation delivers TGs and cholesterol to liver
question
IDL apolipoprotein content
answer
E B100
question
LDL fxn
answer
Formed by HL modification of IDL @ periphery Delivers hepatic cholesterol to peripheral tissues Taken up by target cells via receptor-mediated endocytosis
question
LDL apolipoprotein content
answer
only B100!
question
HDL fxn
answer
secreted from liver and intestine EtOH ? synthesis Mediates reverse cholesterol transport from periphery to liver Acts as a repository for apoC and apoE (needed for chylomicron and VLDL metabolism).
question
HDL apolipoprotein content
answer
ApoE ApoA1 ApoCII
question
familial dyslipidemias: Type I - hyperchylomicronemia
answer
AR (the other two are AD!) ? chylomicrons, TG, chol LPL deficiency or altered ApoCII pancreatitis, hepatosplenomegaly, eruptive/pruritic xanthomas *NO ? risk atherosclerosis!
question
familial dyslipidemias: Type IIa - familial hypercholesterolemia
answer
AD ? LDL, Chol absent/? LDL receptors heterozygous (1:500, chol 300) homozygous (rare, chol 700+) ? atherosclerosis ? may have MI before 20 tendon xanthomas corneal arcus
question
familial dyslipidemias: Type IV - hypertriglyceridemia
answer
AD ? VLDL, TG hepatic overproduction of VLDL pancreatitis
question
Abetalipoproteinemia
answer
Hereditary inability to synthesize lipoproteins due to deficiencies in apoB-100 and apoB-48. Autosomal recessive. Sx appear in the first few months of life. Findings: failure to thrive, steatorrhea, acanthocytosis, ataxia, night blindness.



