Feeding and Swallowing Treatment in the Neonate and Infant – Flashcards
Unlock all answers in this set
Unlock answersquestion
Areas of Focus
answer
Pre-feeding Nipple Feeding Scheduling Feeds Spoon Feeding Cup Drinking
question
When is pre-feeding therapy appropriate?
answer
Inadequate NNS Patient is too young oNippling oBaby food Patient isn't ready for oral feeding oLack of motor control in the body oUnstable respiratory status
question
When is pre-feeding therapy appropriate?
answer
If infant isn't oral feeding work on pre-feeding to get them to that point. Have to have NNS before NS. Too young to nipple feed is <32 weeks Ready for Baby food = 4 months Need stable respiratory rate and heart rate at rest to be able to nipple feed
question
Pre-feeding Treatment Activities
answer
Pacifier trials Oral stimulation NNS Pacifier dips Binky trainer Dropper/Syringe •
question
Pacifier trials
answer
• Tube feedings -Offer pacifier during tube feeding to relate feeling of fullness to feeding. Also a way for parent to bond with infant during feeding. • Kangaroo care- common in NICU, place on mom's chest for skin to skin contact, can do in NICU once they are stable. Research shows this stabilizes HR and RR, it increases oxygen levels as well!
question
Oral stimulation
answer
• Orofacial stretches- o Moderate pressure oAddresses OM and OS skill -Orofacial stretches should only be used on term babies, not babies in NICU - good for motor and sensory skills. Similar to passive range of motion exercises (stretching muscles for them) in PT. Normalizing their sensitivity to sensory input and give them positive input around their mouth. Use moderate pressure!! Don't rub, but stretch. • Toweling - Toweling - take towel, rub up arm (outward to inward) towel up arm to check, then work toward face: check, bottom lip, etc. Then move to hands instead of towel. *body first then to mouth* • Touch to the body
question
NNS
answer
• Elicit with gloved finger • Attempt pacifier trials for endurance • Anticipate the gag • Oral and facial stretches -Stimulate ruga of mouth with gloved finger for NNS. Oral and facial stretched to make mouth stronger
question
Pacifier dips
answer
• Need a stable NNS first • Warm up with a dry pacifier • Pacifier dipped in formula • Slowly increase amount • Decrease pause time between dips
question
Binky trainer
answer
• Working toward NS • Mimics bottle feeding • Treatment technique - o Establish NNS o Push tiny taste of formula through pacifier o Slowly increase speed • Bionix Controlled Flow Baby Feeder
question
Dropper/Syringe Treatment technique
answer
Treatment technique: o One drop of formula into oral cavity o Pause for baby to move formula posterior and swallow o Slowly increase speed and volume as tolerated -Medicine cup - place on the edge of their mouth to transition to cup feeding if they won't take bottle
question
When is it appropriate to use a Dropper/Syringe?
answer
o No NNS or inadequate NNS o Averse to pacifier, but not to finger
question
Nipple Feeding: Reminders
answer
Feeding schedule: Stomach needs time to empty between feeds Minimum of 2 hour break between feeds Increasing calories: Change the feeding schedule Increase the caloric density of the formula -Supplement EBM -Superpumping Burping: Newborns GERD Assess need based on behavior
question
Nipple Feeding: Aversion
answer
Causes of aversion: Waiting for signs of stress before removing the nipple Requiring too much Ignoring refusal cues -Pushing the nipple out with the tongue -Tongue bunching -Lack of initiation -Lip pursing Feeding for too long Feeding too often Too much intra-oral stimulation during feeding -Twisting the nipple frequently to initiate a suck -Stripping the tongue to initiate a suck
question
Nipple Feeding: Positioning
answer
Support the infant Swaddling Sidelying Semi-upright Cradle -Support infant - up to 2 months want them to be inflexion , if older, still suppoer lungs body and head in whatever position they're in. Swaddling is important for containment and to keep body organized which helps suck to be more organized. Swaddling offers support for feeding. And is calming (like weighted vest). Best position for feeding is side-lying! (hold on their side with feet facing your belly unless they're too big)
question
Nipple Feeding: OM Deficits
answer
Weak suck: Oral stretches ( can do before or during feeding) -Moderate pressure to palate, gum ridge, cheeks and lips -Provide before the feed and outside of feeding times Therapeutic trials with the pacifier -Resistance - stretch a little bit -Provide before the feed and outside of feeding times Elicit root reflex - only if they're a newborn Provide cheek support -Activates muscles and supports structures -Not pressure, just support -Release periodically Chin support = stabilizing mandible and providing little support (not as much as cheek) -Stabilizes mandible, increasing efficiency of buccal musculature -Not pressure, just support Apply downward pressure on midline of tongue (Weak lingual and buccal musculature Weak Suck Fatigue) -check support - compensatory strategy, also need to be doing something therapeutic to address issue. release periodically and see if they're stronger on their own or still need support. if aspiration issues, try unilateral support
question
OM deficits: Excessive jaw movement
answer
-Align head and neck -Chin support -OM stretches -Pacing throughout the feed if due to fatigue
question
OM Deficits: Poor initiation of sucking
answer
Quiet alert for eating Apply downward pressure on midline of tongue
question
OM deficits: Tongue protrusion
answer
Establish NNS Try another nipple Larger, broader based nipple
question
OM Deficits: Disorganized suck/poorly coordinated SSB Pacing
answer
-Increases endurance throughout the feed -Provides time for the baby to catch her breath -Provides time for the baby to clear residue from the mouth or pharynx Swaddle for stability Slower flow nipple Binky trainer
question
Weak suck
answer
poor suction on nipple
question
Nipple Feeding: OS Impairment:
answer
Signs of a sensory impairment: Inconsistency -Acceptance -Volume -Reaction to the feeding process Sleeping or shutting down during oral feeds
question
Treatment of OS Impairment
answer
Structure- - Have structured feeding time. have to teach them stomach feels full and good, and when they get hungry they need to eat. Need to be hungry so they'll eat more at next feed. Consistency - baby will ne inconsistent so we need to provide them consistency to establish full/empty hunger. Swaddle -Supports body -Organizes mouth Positioning - side-lying is preferable, or to be held tighter and closer to give calming feedback, but settling on one once it works so you'll be consistent. Quiet, low light, low distraction environment - to focus on feeding NEVER force the bottle! Infant massage prior to feeds- can be certified. good for baby's digestion Brushing and joint compressions prior to feeds - Wilbarger Brush (usually used on older) brushing and compression go hand in hand. Brush arm back and forth then right after do joint compression (gives input to joints). proprioceptive input because these kids' proprioceptive systems are usually under-developed
question
Nipple Feeding: Dysphagia
answer
Pacing Nipple change Pacing with nipple change Thickening VitalStim Therapy - need to be certified and understand anatomy and physiology of swallowing and understand the process of swallowing- retraining brain to swallow (cortical reorganization) through nerve that innervate muscle trying to target to strengthen the muscle. Only use vital stim if problem with pharynx (ex: hyolaryngeal excursion): suck-swallow-breath issue, do not use vital stim Electric current contracts muscles to facilitate swallow Increases muscle strength Accelerates cortical reorganization
question
Nipple Feeding: Cleft Lip
answer
Breastfeeding Positioning Cleft next to breast tissue Different positions for right and left Bottle feeding Gently press sides of cleft together
question
Nipple Feeding: Cleft Palate
answer
Decreased negative pressure Position in semi-upright Cheek and chin support Bottles - Haberman Feeder (Only requires positive pressure One way valve Various levels of flow Feeder has control) Mead Johnson Cleft Palate Nurser -Larger nipple with a crosscut -Soft, flexible, plastic bottle Pigeon Bottle -Larger nipple -Soft nipple for easy compression -Small firmer section on top to close off palate Palatal Obturator -Last resort -Plastic plate that covers the cleft
question
Nipple Feeding: Breastfeeding Stages of Milk
answer
Colostrum Transition Milk Mature Milk
question
Colostrum
answer
-Extra protein and antibodies for protection -Laxative effect to assist with passing meconium
question
Transition Milk
answer
-Occurs between ~1-3 weeks postpartum
question
Mature Milk
answer
-Optimal lactose, appropriate casein/whey, sufficient fat - 40% casein (moves slow; curdles in stomach) and 60% weigh (remains liquid and removes quickly)
question
Hindmilk vs Foremilk
answer
Hindmilk is higher in fat and signals fullness Let Down or Milk Ejection Reflex Brain releases oxytocin into blood and breast to help move milk down to the nipple.
question
Preterm Colostrum
answer
Medicinal -Greater protection than term colostrum -Anti-inflammatory, anti-infection, and growth properties last for a longer period Assists with growing, maturing, and protecting the intestines -Even small tastes during oral care will help gut peristalsis Aids the baby in transitioning from drinking amniotic fluid to drinking milk In NICU will give colostrum for development
question
Pumping Regimen
answer
Goal is for pumping to occur within 6 hours after birth. Pump a minimum of every 3 hours. -Waiting too long between sessions can result in diluted, lower calorie milk. Dual pump (both breasts) with high quality (ideally hospital grade) breast pump. -Not adequately emptying breasts can lead to issues with volume and make up of breast milk (poor lipid content). (Low lipid content in milk ; More calories derived from lactose than there should be ; feeding intolerance ; Poor weight gain ; Conclusion that baby is not tolerating mom's milk) Pump until the flow slows significantly.
question
Positioning for Breastfeeding
answer
Poor positioning can lead to ineffective feeding for baby and sore nipples for mom. Mom should be comfortable and should support her breast. Baby should be pulled close to mom and up to the level of her breast. Mom should support the baby's whole body (not just the head).
question
Cross-Cradle Hold

answer
Can support neck, head, and body well More common
question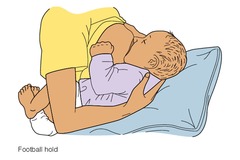
Football Hold
answer
Good for mom's who had C-section Good if any sort of swallow issue as well
question
Side-Lying Hold
answer
If co-sleeping...
question
Australian Hold
answer
*new thing* or "laid back/ biological breast feeding" Not good for preemie without good motor control, but could do with baby who has trouble with flow of milk Should sit in a chair so you can lean back
question
Tips for Breastfeeding with Problem Feeders
answer
Pacifiers in NICU Nipple Shield Bring baby up to level of breast Mom supports breast with hand Educate on volume consumption -Listen for swallows -Look for milk in oral cavity -Wet diapers -Pre and Post weight in newborns (1 gram of weight difference = 1 ml milk transferred) Difficulty with SSB coordination at the breast -Position in football hold -Pump off if strong letdown (Will increase/maintain production if done too long/often) EBM
question
Oral Feeding Schedule
answer
For sensory, OM, and dysphagia Slowly increase amount of feeds Space feeds out -Example: Feeding Schedule: 0600, 0900, 1200, 1500, 1800, 2100, 0000, 0300 Initially PO at 0600 and 1800 Then 0600, 1200, 1800 Then 0600, 1200, 1800, 0000 and so on
question
Spoon Feeding
answer
Spoon Feeding Rice cereal, veggies, fruits, then meats Allergies Treatment technique -Introduce with a pacifier -Small nuk, infadent, Ark probe, Zvibe-Spoon *Rest on lower lip *Textured spoon for low sensory awareness
question
Cup Drinking
answer
Introduce between 6 and 9 months Different sucking pattern than nippling Transitional cup Nuby Straw cup Different sucking pattern than nippling un less you use a glorified bottle If trying to get you on cup drinking - will use straw cup (honey bear)
question
Medicine Cup
answer
For older infant without NNS Treatment technique -Jaw support -Slowly pour liquid into mouth



