Dermatology Objectives – Flashcards
Unlock all answers in this set
Unlock answersquestion
Topical Steroids
answer
Grouped from I-VII Lower the group means stronger the effect Available in ointments, creams, gels, foams, lotions. Ointments seep in better
question
Side effects of Topical Steroids
answer
Skin atrophy Telangiectasia Tachyphylaxis--loss of potency/effectiveness Steroid induced acne HPA axis--hypothalamus pituitary adrenal suppression
question
Impetigo
answer
Contagious infection of the epidermis usually with Staphylococci or streptococci infection. Clinical findings: Lesions consist of macules, vesicles, bullae, pustules, and honey-colored crusts that when removed leave denuded red areas. Assessment: Gram stain is positive. Differential diagnosis: Herpes simplex and contact dermatitis Treatment: soaks and scrubbing. Topicals such as bacitracin, mupirocin, retapamulin are first-line treatment options for infections limited to small areas. In widespread cases, systemic antibiotics-Cephalexin. Doxycycline. Complications: MRSA can cause impetigo. Need to have all family members take a bleach bath
question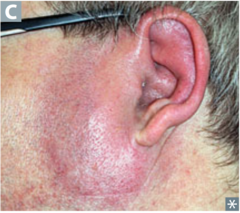
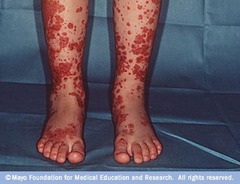
Erysipelas
answer
Superficial form of cellulitis caused by beta-hemolytic streptococci. Clinical findings—Edematous, raised, circumscribed, hot, erythematous area, with or without vesicles or bullae at the border • Central face or lower extremity frequently involved. • Prodrome of Pain, chills, fever, and systemic toxicity may be striking for 4-48 hours • A bright red spot appears and then spreads to form a tense, sharply demarcated, glistening, smooth, hot plaque that may pit if pressed on by a finger. Assessment (including diagnostic studies)—positive blood cultures and leukocytosis Differential diagnosis—Erysipeloid is a benign bacillary infection producing cellulitis of the skin of the fingers or the backs of the hands in fishermen and meat handlers. Prognosis—rapid improvement with treatment. Recurrence of lymphedema. Complications—may complicate any break in the skin and allow a portal of entry for the organism to enter the body •Tinea pedis with fissuring allows the organism into the body •Death from systemic toxicity Treatment—Intravenous antibiotics effective against group A beta-hemolytic streptococci and staphylococci should be considered, but outpatient treatment with oral antibiotics has demonstrated equal efficacy. • Oral regimens include a 7-day course with penicillin VK--first line •dicloxacillin (250 mg) •cephalosporin (250 mg) orally four times a day. •Clindamycin (250 mg twice daily orally for 7-14 days) •Erythromycin
question
Hot Tub Folliculitis (Pseudomonas folliculitis)

answer
Clinical findings—Itching and burning in hairy areas. •50 or more Red, dense Pustules and papules in the hair follicles. •pruritic or burning, tender follicular, pustular lesions that occur within 1-4 days after bathing in a contaminated hot tub, whirlpool, or swimming pool Assessment (including diagnostic studies)—need to do a gram stain and culture to determine if bacterial or non-bacterial. Pseudomonas can survive the heat. Differential diagnosis—malassezia folliculitis, impetigo, eiosinophillic folliculitis requires a biopsy, acne vulgaris Prognosis—stubborn and persistent, requiring prolonged or intermittent courses of antibiotics. Complications—can form abscesses. Prevention—for recurrent infections—mupirocin, rifampin, clindamycin, bleach bathes. Treatment— Topical antibiotics are generally ineffective if bacteria have invaded the hair follicle. • ciprofloxacin for non-neutropenic individuals • antistaphylococcal antibiotics are required if infection has involved the scalp or densely hairy areas, such as the axilla, beard, or groin.
question
Tinea Pedis (athletes foot)

answer
Clinical findings •Most often presents with asymptomatic scaling. •May progress to fissuring or maceration in toe web spaces. •Itching, burning, and stinging of interdigital web; scaling palms and soles; vesicles of soles in inflammatory cases. • Moccasin distribution on the feet • Can get friability of the nail plate Complications •May be a portal of entry for bacteria causing lower extremity cellulitis. Assessment •The fungus is shown in skin scrapings examined microscopically or by culture of scrapings. •The more macerated the feet are the less of a chance that you will get a positive on the KOH because bacteria are taking over Differential diagnosis—contact dermatitis (affects dorsal surfaces and will respond to corticosteroids), psoriasis (negative on fungal cultures), scabies Prevention—hygiene, dry feet, change socks, use antifungal drying powder Treatment—use topical antifungals, spectazole, nizoral, oxistat Oral--itraconazole and terbinafine for systemic Prognosis—chronic affliction, temporarily cleared by therapy only to recur.
question
Tinea Corporis

answer
Pathophysiology-- Infected pet could pass on the infection; pathogen Trichophyton rubrum Clinical findings—Lesions on face and arms. Pruritis. Ring-shaped lesions with an advancing scaly border and central clearing or scaly patches with a distinct border. Assessment (including diagnostic studies)—confirm with KOH or scrapings or culture Differential diagnosis—psoriasis, lupus erythematosus, syphilis, granuloma annulare, and pityriasis rosea. Prognosis—responds promptly to conservative topical therapy or to an oral agent within 4 weeks. Complications—Extension of the disease down the hair follicles (which presents as papules and pustules and is more difficult to cure) and pyoderma. Prevention—treat household pets, keep feet dry, change socks Treatment—most topical antifungals, including econazole, miconazole, clotrimazole, terbinafine, butenafine. Continue treatment 1-2 weeks after clinical clearing. Can use itraconazole and terbinafine for systemic.
question
Tinea Capitis

answer
Fungal infection of the scalp. Alopecia Common in children Assessment KOH + only 29-66%, therefore always culture Can do hair pull test and put in fungal culture Treatment Often use weight based Gris-PEG for 6-8 weeks Only systemic works: griseofulvin, terbinafine, itraconazole
question
Tinea cruris (Jock Itch)

answer
Clinical Findings •Marked itching in intertriginous (rubbing) areas, usually sparing the scrotum. •Peripherally spreading, sharply demarcated, centrally clearing erythematous lesions. •May have associated tinea infection of feet or toenails. Assessment •Laboratory examination with microscope or culture confirms diagnosis. •Do a KOH test Differential diagnosis—candidiasis (bright red and has satellite papules and pustules), seborrheic dermatitis (face, sternum and axilla), intertrigo (red, less scaly and on moist folds of obese people), psoriasis of body folds (can affect the scrotum) Treatment drying powder of miconazole •Topical antifungals •Terbinafine and itraconazole for systemic, griseofulvin for severe cases Prognosis—responds promptly to topical or systemic treatment but often recurs
question
Tinea Barbae

answer
Fungal overgrowth in beard area Pruritic, red, and scaling patches with fragile or broken hairs. Can be exacerbated by frequent shaving Often needs oral therapy--itraconazole and terbinafine for systemic.
question
Tinea Manum

answer
•Itching, burning, and stinging of interdigital web; scaling palms and soles Often presents on just one hand "Two foot one hand" guideline Both feet and one hand--Often on dominant hand Assessment •The fungus is shown in skin scrapings examined microscopically or by culture of scrapings. Differential diagnosis—contact dermatitis (affects dorsal surfaces and will respond to corticosteroids), psoriasis (negative on fungal cultures), scabies Prevention—hygiene, dry feet, change socks, use antifungal drying powder Treatment—use topical antifungals, spectazole, nizoral, oxistat Oral--itraconazole and terbinafine for systemic Prognosis—chronic affliction, temporarily cleared by therapy only to recur.
question
Onychomycosis

answer
Clinical findings—lusterless, brittle, and hypertrophic, and the substance of the nail is friable Distal Subungual--most common Proximal Subungual--may be a sign of HIV Assessment (including diagnostic studies)— •Portions of the nail should be clipped, digested with 10% KOH and examined under the microscope for hyphae. •Fungi may also be cultured from debris collected from underneath the nail plate. •Periodic acid-Schiff stain of a histologic section of the nail plate will also demonstrate the fungus readily. •Each technique is positive in only 50% of cases so several different tests may need to be performed. Differential diagnosis--nail psoriasis--causes hyperkeratosis, Lichen Planus, Eczema, Contact Dermatitis Prognosis—difficult to treat because of the long duration of therapy required and the frequency of recurrences. •Fingernails can virtually always be cured, and toenails are cured 35-50% of the time and are clinically improved about 75% of the time. Complications--friable nail plates Treatment—efinaconazole Jublia 10% has been approved as a topical therapy; preliminary evidence suggests that it performs better than prior topical treatment options. Ciclopirox--another topical • Ketoconazole—dangerous for hepatotoxicity • Griseofulvin Systemic • Terbinafine • Itraconazole • Fluconazole
question
Tinea Versicolor

answer
Clinical findings—asymptomatic lesion, itching, Velvety, tan, or pink macules or white macules that do not tan with sun exposure. Fine scales that are not visible but are seen by scraping the lesion. Central upper trunk the most frequent site but can get them on the neck and groin as well. Common during the summer. Assessment (including diagnostic studies)—Yeast and short hyphae observed on microscopic examination of scales. Large, blunt hyphae and thick-walled budding spores ("spaghetti and meatballs") are seen on KOH. Differential diagnosis—vitiligo (does not scale; total hypopigmentation). Seborrheic dermatitis. Prognosis—Without maintenance therapy, recurrences will occur in over 80% of "cured" cases over the subsequent 2 years. Treatment—Topical treatments selenium sulfide lotion, which may be applied from neck to waist daily and left on for 5-15 minutes for 7 days; this treatment is repeated weekly for a month and then monthly for maintenance. Ketoconazole shampoo, 1% or 2%, lathered on the chest and back and left on for 5 minutes may also be used weekly for treatment and to prevent recurrence. Clinicians must stress that the raised and scaly aspects of the rash are being treated; the alterations in pigmentation may take months to fade or fill in. Ketoconazole—200 mg daily orally for 1 week or 400 mg as a single oral dose, with exercise to the point of sweating after ingestion, results in short-term cure of 90% of cases. Patients should be instructed not to shower for 8-12 hours after take ketoconazole because it is delivered in sweat to the skin. Two doses of oral fluconazole 300 mg, 14 days apart, has similar efficacy. Imidazole creams, solutions, and lotions are quite effective for localized areas but are too expensive for use over large areas such as the chest and back.
question
Herpes Simplex

answer
Etiology—85% of adults have herpes 1 simplex often acquired asymptomatically in childhood. 25% have type 2--causes lesions on genitalia. Up to 70% of such infections appeared to be transmitted during periods of asymptomatic shedding. Genital herpes may also be due to HSV-1. Pathophysiology—may follow minor infections, trauma, stress, or sun exposure; regional lymph nodes may be swollen and tender. Clinical findings—recurrent small grouped vesicles on an erythematous base, especially in the orolabial (vermillion border) and genital areas. •Burning and stinging, neuralgia •Lesions crust and heal in a week Assessment (including diagnostic studies)—Viral cultures and direct fluorescent antibody tests are positive. Can do ELSIA tests. Differential diagnosis—chancroid, syphilis, pyoderma, or trauma Prognosis—Suppressive treatment will reduce outbreaks by 85% and reduces viral shedding by more than 90%. This results in about a 50% reduced risk of transmission. The recommended suppressive doses are taken continuously. Long-term suppression appears very safe, and after 5-7 years a substantial proportion of patients can discontinue treatment. Prevention Use latex and condoms to reduce transmission •Use sunscreen to prevent type 1 treatment must initiated by the patient at the first sign of reoccurrence Complications—Include pyoderma, eczema herpeticum, herpetic whitlow, herpes gladiatorum (epidemic herpes in wrestlers transmitted by contact), proctitis, esophagitis, neonatal infection, keratitis, and encephalitis. Treatment—clinical episodes, the dosage of acyclovir, of valacyclovir, Penciclovir, and famciclovir. The duration of treatment is from 7 to 10 days depending on the severity of the outbreak. Can get vaccination.
question
Herpes Zoster (shingles)

answer
Clinical findings—Pain along the course of a nerve followed by grouped vesicular lesions. •Involvement is unilateral; some lesions (fewer than 20) may occur outside the affected dermatome. •Lesions are usually on face or trunk. •Pain usually precedes the eruption by 48 hours and may follow •Regional lymph nodes may be swollen and tender Assessment (including diagnostic studies)—Direct fluorescent antibody positive, especially in vesicular lesions. Differential diagnosis—poison oak and poison ivy dermatitis can occur unilaterally •contact dermatitis is pruritic •herpes simplex, which rarely occurs in a dermatomal distribution •can simulate erysipelas initially on the face •Depending on the dermatome involved, the pain may lead the clinician to diagnose migraine, myocardial infarction, acute abdomen, herniated disk, etc. Prognosis—eruption persists 2-3 weeks and usually does not recur. Motor involvement in 2-3% of patients may lead to temporary palsy. Complications—HIV patients are 20 times more likely to develop before other signs of HIV is present •Persistent neuralgia, anesthesia or scarring of the affected area, facial or other nerve paralysis, and encephalitis may occur. •Postherpetic neuralgia is most common after involvement of the trigeminal region and in patients over the age of 55. Prevention—live vaccine (Zostavax) is available and recommended to prevent both the virus and postherpetic neuralgia. •approved for persons over the age of 50 and recommended in persons aged 60 and older, even in those who have had it previously. Treatment—Early (within 72 hours after onset) and aggressive antiviral treatment reduces the severity and duration of postherpetic neuralgia—immunocompetent individuals •antivirals—oral acyclovir, famciclovir, or valacyclovir—all for 7 days •can give a nerve block for initial pain •if the trigeminal nerve is involved—need to consult and ophthalmologist •can give corticosteroids like prednisone for reduction of pain—would need to taper (these will not reduce the prevalence or duration of postherpetic neuralgia) •corticosteroids should NOT be used in immunosuppressed individuals •can use calamine lotion topically •Can use capsaicin ointment or lidocaine patches •Can use anti-depressants such amitriptyline •Gabapentin and duloxetine for nerve pain relief •Referral to a pain management clinic
question
Pityriasis Rosea

answer
Clinical findings—Itchy, Oval, fawn-colored, scaly eruption following cleavage lines of trunk—2 cm in diameter. Cigarette paper appearance. An initial lesion ("herald patch") that is often larger than the later lesions often precedes the general eruption by 1-2 weeks. Christmas tree pattern. Can get lesion in axilla and groin—inverse. More common in women and during the colder months. Differential diagnosis—syphilis has red, copper, ham colored macules (need to do a serologic test if typical lesion are not present and if there are lesion on the palms, soles, and mucous membranes). Do a KOH to rule out fungal. Tinea corporis—not as many lesions. Tinea versicolor—lacks the rimmed lesions and has hypopigmented lesions. Seborrheic dermatitis can have patches on sternum, axilla and groin. Treatment--indicated only if the patient is symptomatic. UVB treatments or a short course of prednisone for severe or severely symptomatic cases. For mild to moderate cases, topical corticosteroids of medium strength (triamcinolone 0.1%) and oral antihistamines may also be used if pruritus is bothersome. Will go away in 6-8 weeks.
question
Scabies

answer
Risk factors—those in facilities, immunosuppressed individuals Pathophysiology—transmits to those in which are in close physical contact for 15-20 minutes. Or in the infected person's bedding. Clinical findings—Generalized very severe itching. •Brown, linear burrows, vesicles, and pustules, especially on finger webs and in wrist creases and waist lines •Can be on palms and feet, elbows, axilla, umbilicus •Mites, ova, and brown dots of feces (scybala) visible microscopically. •Firm, Red papules or nodules on the scrotum, buttocks, axillary folds, and on the penile glans and shaft are pathognomonic. •Hyperkeratotic type has a flakey crust that contains millions of mites and are highly infectious—can get infected with s. aureus Assessment (including diagnostic studies)—need to scrape the lesions; confirmed by microscopic demonstration of the organism, ova, or feces in a mounted specimen examined with tap water, mineral oil, or KOH. Differential diagnosis—pediculosis, from bedbug and flea bites, and from other causes of pruritus. Complications—can get staph infections which lead to sepsis Treatment—need to clean the bedsheets and clothing and use high heat. •Permethrin cream 5%—neck down for 8-12 hours once a week •Triamcinolone—for continued itching •Oral Ivermectin in immunocompromised patients and for nodular scabies. •Urea can be used to remove the scale Crusted scabies--oral ivermectin and topical permethrin or benzoyl benzoate
question
Seborrheic Dermatitis

answer
Clinical findings—scalp, face, chest, back, umbilicus, eyelid margins, genitalia, and body folds have dry scales (dandruff) or oily yellowish scurf. Pruritis variable. Often coexists with psoriasis. Sebum overproduction with yeast organism Malassezia Differential diagnosis—psoriasis, may simulate intertrigo in flexural areas Prognosis—Lifelong recurrences. Individual outbreaks may last weeks, months, or years. Complications—associated with Parkinsons, HIV, and immunosuppressed individuals Treatment—scalp: shampoos with zinc and ketoconazole. Topical corticosteroids and tar shampoo. Facial—topical corticosteroid, Topical tacrolimus (Protopic) and pimecrolimus (Elidel) are steroid-sparing alternatives. Nizoral cream compounded with 1-2 percent hydrocortisone Non-hairy areas-- Low-potency corticosteroid creams—ie, 1% or 2.5% hydrocortisone, desonide, or alclometasone dipropionate Eyelids—Johnson and Johnson baby shampoo
question
Candidial infections (Thrush)

answer
Fungal infection that occurs on almost any cutaneous or mucosal surface. Risk factors—pregnant women, obesity, diabetics, HIV, elderly with dentures, Th-17 mutations Pathophysiology—Systemic antibiotics, oral corticosteroids, and oral contraceptive agents may be contributory Clinical findings—Severe pruritus of vulva, anus, or body folds. •Superficial denuded, beefy-red areas with or without satellite vesicopustules. •Whitish curd-like concretions on the oral and vaginal mucous membranes. Assessment (including diagnostic studies)—Yeast and pseudohyphae on microscopic examination of scales or curd. Differential diagnosis—intertrigo, seborrheic dermatitis, tinea cruris, "inverse psoriasis," and erythrasma Prognosis—range from the easily cured to the intractable and prolonged. Complications—paronychia, systemic candidiasis in immunosuppressed patients and those taking broad spectrum antibiotics Treatment—clotrimazole solution for nail issues •Skin—clotrimazole cream, hydrocortisone cream, nystatin ointment, fluconazole for widespread disease, gentian violet. •Vulva and anal—Intravaginal clotrimazole, miconazole, nystatin, terconazole, •On breasts—nystatin, clotrimazole cream, gentian violet, and oral fluconazole
question
Dyshidrosis (AKA pomphylx; hand dermatitis, vesiculobullous dermatitis of the palms and soles)

answer
Clinical findings—pruritic "tapioca" vesicles of 1-2 mm on the palms, soles, and sides of fingers. •Vesicles may coalesce to form multiloculated blisters. •Scaling and fissuring may follow drying of the blisters. •Intense itching •Appearance in the third decade, with lifelong recurrences. Differential diagnosis—Unroofing the vesicles and examining the blister roof with a KOH preparation will reveal hyphae in cases of bullous tinea. •Always examine the feet of a patient with a hand eruption because patients with inflammatory tinea pedis may have a vesicular autoeczematization of the palms •Nonsteroidal anti-inflammatory drugs (NSAIDs) may produce an eruption very similar Prognosis—an inconvenience. For some, it can be incapacitating Prevention—one-third to one-half of patients have a relevant contact allergen, especially nickel. Patch testing and avoidance of identified allergens can lead to improvement. Treatment—topical and systemic corticosteroids. Topicals will help with the fissuring and scaling. •PUVA therapy and injection of botulinum toxin into the palms •Use hand creams, use a long stick scrub brush for doing dishes
question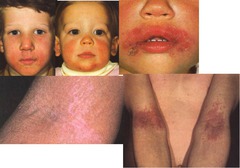
Eczema (Atopic dermatitis)
answer
Clinical findings --triad--asthma, allergies and.... •Itch-scratch cycle Pruritic, xerotic, exudative, or lichenified eruption on face, neck, upper trunk, wrists, and hands and in the antecubital and popliteal folds. •Scaly, red plaques on face, neck and trunk •Papular appearance in African Americans •Personal or family history of allergic manifestations •Tendency to recur. •Onset in childhood in most patients. Onset after age 30 is very uncommon. Risk factors—family history, tendency to recur, skin atrophy Assessment (including diagnostic studies)—will find lichenification on the flexoral regions, hands, nipples •Eosinophilia and increased serum IgE levels may be present. Differential diagnosis—seborrheic dermatitis (not as itchy), psoriasis (thicker scales), secondary, staph or herpetic infections Prognosis—chronic and intermittent course Complications—need to taper corticosteroid treatment so as to not cause acute flare ups Prevention—patient education, occurs in winter often times, soap should be confined to the armpits, groin, feet, scalp (don't use washcloths and brushes), irritation by rough fabrics Management—use an emollient after showering or a corticosteroid (will have to taper later), avoid ointments, heat Topical steroids--triamcinolone •Use oral prednisone for severe and acute •Weeping lesions—use Aveeno, wet dressings, high potency corticosteroids •Scaly—corticosteroids in ointment form; taper and then use emollients Can use IM kenalog •Lichenified lesions—corticosteroid ointments •Use effective moisturizers once symptoms have gone away
question
Contact dermatitis

answer
Clinical findings Results from contact with chemicals or allergens Erythema and edema, with severe pruritus, often followed by vesicles, bullae, weeping or crusting in an area of contact with a suspected agent. •A history of previous reaction to suspected contactant. •Positive patch test •80% of cases are from irritants—soaps, detergents •red and scaly appearance with areas of direct contact; no vesicles •poison ivy or poison oak, topically applied antimicrobials (especially bacitracin and neomycin), anesthetics (benzocaine), hair-care products, preservatives, jewelry (nickel), rubber, essential oils, propolis (from bees), vitamin E and adhesive tape. •Weeping and crusting lesions found outside the areas of direct contact •Bizarre patterns of erythematous macules, papules, and vesicles •hot and swollen, with exudation and crusting, simulating—and at times complicated by—infection. •Location will determine the cause •Assessment •Gram stain to rule out impetigo, should do patch testing to figure out the allergen if the cause is not known •Differential diagnosis •Impetigo or cellulitis, eczema, scabies, pompholyx •Prevention •Figure out the irritant and avoid it, wear gloves and protectants, wash right away with soap and water if poison ivy and oak •Treatment •Topical corticosteroids •Weeping lesions--Gentle compress •Zinc paste with wet dressings •Calamine lotion •Topical corticosteroids with high potency •Systemic therapy--Prednisone 12-21 days and then taper slowly •Prognosis •2-3 weeks for full resolution. Removal of the causative agent is paramount to avoid recurrences
question
Psoriasis
answer
Clinical Findings •Silvery scales on bright red, well-demarcated plaques, usually on the knees, elbows, and scalp. Can have on palms and soles. Pink or red intergluteal folds as well. •Nail findings including pitting (stippling in the nails) and onycholysis (separation of the nail plate from the bed)--10-80% of cases. •Mild itching (usually). •May be associated with arthritis. •Histopathology can be helpful to exclude clinical mimics. Koebner sign (normal skin irritation leads to lesions at the site) Risk factors—Increased risk for cardiovascular events, type 2 diabetes mellitus, metabolic syndrome, and lymphoma. Differential diagnosis—seborrheic dermatitis. Atopic dermatitis is in flexoral areas. Scraping and culture for Candida and examination of scalp and nails will distinguish "inverse psoriasis" from intertrigo and candidiasis. Dystrophic changes in nails may mimic onychomycosis, and a potassium hydroxide (KOH) preparation or fungal culture is valuable in diagnosis Prognosis-- chronic and unpredictable, and the disease may be refractory to treatment. Patients (especially those older than 40 years) should be monitored for metabolic syndrome. Treatment—tiny doses of systemic corticosteroids given to patients may lead to severe rebound flares of their disease when they are tapered. Systemic corticosteroids should never be used to treat. If there is less than 10% of the BSA involved, the easiest regimen is to use a high-potency to ultra-high-potency topical corticosteroid cream or ointment—pulse fashion. Calcipotriene ointment 0.005% or calcitriol ointment 0.003%, both vitamin D analogs, are used twice daily. For the scalp, start with a tar shampoo, used daily if possible. For thick scales, use 6% salicylic acid gel under a shower cap at night. Can use UV phototherapy for limited or moderate disease. Generalized to severe is >30% BSA—use UV light therapy at a center. Methotrexate doses up to 25 mg once weekly for itching—need to do liver checks though. Synthetic retinoid, is most effective for pustular cases. Liver enzymes and serum lipids must be checked periodically—teratogen; no pregnancy. Decreases epidermal proliferation.
question
Lichen Planus
answer
Inflammatory pruritic disease of the skin and mucous membranes characterized by distinct papules and occurring on the flexor surfaces of the trunk Pathophysiology—caused by antihypertensives and diuretics. Sulfonamides, tetracyclines, quinidine, NSAIDs, beta-blockers, and hydrochlorothiazide Clinical findings—Pruritic, violaceous, flat-topped papules with fine white streaks and symmetric distribution. 5 P's—purple, puritic, polygonal, planar, papules Wickham's striae: small network of fine white lines on top of a lesion •Lacy or erosive lesions of the buccal (50% have oral involvement), wrists, vulvar, and vaginal mucosa; nail dystrophy. •Commonly seen along linear scratch marks (Koebner phenomenon—in areas of trauma) on anterior wrists, penis, and legs. •Need to find typical skin lesions, mucosal lesions, and histopathologic features of band-like infiltration of lymphocytes in the upper dermis. Assessment (including diagnostic studies)—Histopathologic examination is diagnostic. •Biopsy of oral lesion and immunofluorescence Differential diagnosis—psoriasis, lichen simplex chronicus, graft-versus-host disease, and syphilis. •Must be differentiated from leukoplakia. Prognosis—benign disease, but it may persist for months or years and may be recurrent. Complications—SCC in those with oral or genital lichen planus Treatment—super potent corticosteroids, cream used nightly under plastic •Systemic corticosteroids—but will relapse after tapering •Oral retinoid and PUVA phototherapy
question
Lichen Simplex Chronicus

answer
Scratch-itch cycle that is difficult to disrupt Clinical findings—Dry, hypertrophic, lichenified plaques appear on the neck, ankles, or perineum patches are rectangular, thickened, and hyperpigmented. The skin lines are exaggerated. •Chronic itching and scratching. •Lichenified lesions with exaggerated skin lines overlying a thickened, well-circumscribed, scaly plaque. •Predilection for nape of neck, wrists, external surfaces of forearms, lower legs, scrotum, and vulva. Differential diagnosis—nummular dermatitis (more acute round, scaly, or moist lesions), dermatitis planus, psoriasis Prognosis—The disease tends to remit during treatment but may recur or develop at another site Complications—can complicate chronic atopic dermatitis or scabetic infestation. Prevention—trim nails, use tape Treatment—superpotent topical corticosteroids are effective, with or without occlusion, when used twice daily for several weeks. •(Cordran) tape may be effective, since it prevents scratching and rubbing of the lesion. •Trim the patient's nails
question
Uriticaria

answer
Etiology—caused by foods, infections, and medications Pathophysiology—can be with IgE (autoantibodies against the receptors) or cascade of complement Clinical findings—Eruptions of evanescent wheals or hives. •Itching is usually intense but may, on rare occasions, be absent. •Special forms have special features (dermatographism, cholinergic, solar, or cold). •Angioedema is involvement of deeper subcutaneous tissue with swelling of the lips, eyelids, palms, soles, and genitalia. They MOVE around. Assessment (including diagnostic studies)—ELISA test, biopsy Differential diagnosis—papular hives from insect bites, acute contact dermatitis Prognosis—Most incidents are acute and self-limited over a period of 1-2 weeks. Chronic type (episodes lasting longer than 6 weeks) may have an autoimmune basis. •Individual lesions only last for about 24 hours •Acute type usually lasts only a few days to weeks. Half of patients whose condition persists for longer than 6 weeks will have it for years. Complications—cholinergic type with hot showers and sweating and cold type with cold weather, wind Management—try to figure out the history to see what is causing it; medications, insect bites, weather, exercise •H1 antihistamines—hydroxyzine, fexofenadine, loratadine, montelukast Steroid sparing--methotrexate. •Can also take H2 antihistamines •UVB phototherapy for chronic
question
Bullous pemphigoid

answer
Autoimmune skin disorder that forms blisters and bullae filled with fluid. Benign pruritic disease characterized by tense blisters in flexural areas Clinical findings—blisters may be preceded by pruritic urticarial or edematous lesions for months. •Oral lesions are present in about one-third of affected persons. Risk factors—men twice as likely to get it. Over the age of 60. Assessment (including diagnostic studies)—biopsy and direct immunofluorescence •Positive ELSIA test Differential diagnosis—pemphigus has acantholysis Prognosis—remits in 5-6 years Treatment—corticosteroids; prednisone, tetracycline, dapsone and methotrexate, rituximab
question
Nikolsky Sign
answer
Dislodgement of intact superficial epidermis by a shearing force, indicating a plane of cleavage in the skin. Bubble with fluid; can press on it and the fluid displaces to the outer edges and can pop. Positive in pemphigus. Negative in Bullous pemphigoid.
question
Acne Vulgaris
answer
Pathophysiology—Chronic disorder of pilosebaceous apparatus--gets obstructed and inflammed Plugging of the infundibulum of the follicles, retention of sebum, overgrowth of the bacteria with resultant release of and irritation by accumulated fatty acids, and foreign-body reaction to extrafollicular sebum Causes breakdown of the sebaceous lipids Producing inflammation Initiates the sequence of lesion development Plugged pores → Papules → pustules → cysts → scars •Can get it from topical corticosteroids and facial creams Clinical findings—The most common of all skin conditions. •Almost universal in puberty, though onset may begin in premenarchal girls and present or persist into the fourth or fifth decade. •Comedones are the hallmark of acne vulgaris. Severity varies from purely comedonal to papular or pustular inflammatory acne to cysts or nodules. Can have white and black heads. Blackheads are open and oxidized. White heads are closed. •Face and upper trunk may be affected, and shoulders •Scarring may be a sequela of the disease or picking by the patient. •Can be painful and itchy Assessment (including diagnostic studies)—should do a bacterial culture to see if staph Differential diagnosis—rosacea, telangiectasia, keratosis pilaris Prognosis—remits frequently, can lead to scarring, can become resistant Complications—women can have hyperandrogenism from polycystic ovary syndrome •Cyst formation, pigmentary changes, scarring, and poor quality of life may result Prevention—patient education, do not pick! Treatment— Want to: Decrease sebaceous activity Decrease P. acnes population Decrease follicular occlusion Decrease follicular inflammation Decrease androgen stimulation of sebaceous glands Comedolytics - Used mainly for comedonal acne Also beneficial in inflammatory acne Examples: topical retinoids Retinoic acid (Retin-A; Avita) Adapalene (Differin) Other: antikeratinizing agent Azaleic acid (Azalex) Antiseptics Useful in inflammatory and comedonal acne Most useful to treat inflammatory acne Effective antibacterial agents; Also comedolytic Often used in combination with comedolytics Examples Benzoyl peroxide (antibacterial, antifungal, anti-yeast) 2.5%, 5%, 10% (mostly OTC) Antibiotics Effective in decreasing P. acnes population Not as effective as oral, but fewer side effects Often used in combination with comedolytics or benzoyl peroxide Erythromycin Clindamycin Oral antibiotics Effective in controlling mild to moderate papular or nodular inflammatory acne-antibacterial but also antiinflammatory Examples Tetracycline, minocycline, doxycycline Erythromycin, amoxicillin, clindamycin Hormonal Therapies Generally only for women Certain oral contraceptives Ovarian androgen suppression Androgen receptor blockers Spironolactone—screening by seeing family med doctor to get long term meds Systemic Retinoids Useful in severe nodulocystic acne and recalcitrant acne Examples---do NOT take during pregnancy Isotretinoin (Accutane)—puts acne into remission; shuts it down Produces remarkable clearing in 95% of patients Provides persistent remission in 85% of patients Because lesions take 4-6 weeks to improve, clinical improvement should be measured by the number of new lesions forming after 6-8 weeks of therapy •Have a diet that is lower in carbs and sugars •Good hygiene; mild soap •Tetracycline, minocycline, and doxycycline are contraindicated in pregnancy. •Can do intralesional injections of triamcinolone •Laser dermabrasion
question
What is the sequence of formation of lesions in acne vulgaris?
answer
Plugged pores → Papules → pustules → cysts → scars Papules--sebum and bacteria mixed. Inflammation is under the surface of the skin and the result is a raised, red, solid blemish Pustules--more inflammation and pus may form causing a red, raised blemish that is often painful to the touch. Pus is a mixture of white blood cells attracted by inflammation, dead skin cells and bacteria.
question
Mild acne
answer
characterized by the presence of few to several comedones, papules and pustules but no nodules Grade 1
question
Moderate acne
answer
Presence of several to many papules and pustules along with nodules/cysts Grade 2-3
question
Severe acne
answer
Presence of numerous or extensive papules and pustules as well as many nodules/cysts, potentially scarring Grade 4
question
Grading scale for acne vulgaris
answer
Grade 1: superficial: noninflammatory, comedones NO papules, pustules, nodules or scars. Grade 2 - superficial: inflammatory papules, pustules NO nodules or scars Palpate skin to determine whether lesion are nodular Seen in T zone and along nose, perinasal, labial areas, and the forehead. Grade 3 - superficial: papules, pustules, comedos, nodules. Also palpable deep inflammatory lesions (nodules and cysts). Patients c/o pain and often pick at lesions. Grade 4 - nodulocystic acne Deep: inflammatory lesions, comedones, papules, pustules multiple nodules and scars.
question
Treatment for grade 1 of acne
answer
Grade 1 - superficial: noninflammatory, comedones First-line therapy Benzoyl peroxide products Topical retinoids Other options Physician-directed extraction α-hydroxy acids Salacylic acid
question
Treatment for grade 2 of acne
answer
Grade 2 mild to moderate- superficial: inflammatory papules, pustules Topical antibiotics Topical retinoids Salicyclic acid or glycolic acid peels Benzoyl peroxide products Shown to decrease resistant strains of P. acnes
question
Treatment for grade 3 of acne
answer
Grade 3 moderate- palpable deep inflammatory lesions (nodules and cysts) First-line treatment Oral antibiotics--clindamycin and benzoyl peroxide Patients with large nodules Often benefit from intralesional corticosteroid injections Hormonal therapy for women--spironolactone In severe cases consider Accutane
question
Treatment for grade 4 of acne
answer
Grade 4 - nodular, cyctic acne Deep: inflammatory, comedos, papules, pustules multiple nodules and scars Accutane Androgen blockers women Intralesional corticosteroids Incision and drainage (likely scarring)
question
Rosacea

answer
Pathophysiology—topical corticosteroids can induce Clinical findings—A chronic disorder affecting the face. •A neurovascular component (erythema and telangiectasis and a tendency to flush easily). •An acneiform component (papules and pustules) may also be present. Pink patches with nodulocystic lesions •A glandular component accompanied by hyperplasia of the soft tissue of the nose--rhinophyma •NO comedones are present •Exacerbation of their case due to heat, hot drinks, spicy food, sunlight, exercise, alcohol, emotions, or menopausal flushing Differential diagnosis— acne vulgaris Carcinoid syndrome Seborrheic dermatitis Perioral dermatitis Lupus erythematosis Prognosis—life-long disease, persistent Complications—associated ophthalmic disease, including blepharitis (watery blood shot eyes) and keratitis, which often requires topical or systemic antibiotic or immunosuppressive therapy Prevention—patient education to avoid the things that exacerbate their case, use sunscreen Treatment— Topical Metronidazole gel, lotion, cream Azelex gel/cream (anti redness) Anti-demodex mite treatments Topical Ivermectin Oral Antibiotics—high or low dosing clindamycin, brimonidine (reduce the redness and flushing) •systemic treatment if topicals don't work—doxycycline, amoxicillin, metronidazole •treat telangiectases with laser therapy
question
Perioral Dermatitis
answer
Clinical findings A papular, erythematous eruption Mostly young women Numerous causes Hormones Topical steroids Contact allergy Irritant including whiteners, cinnamon, tartar control Seen spring and fall Treatment Topical anti bacterials in mild cases Avoidance of contact irritants Oral antibiotics often needed for 6-8 weeks to prevent rebound flare Antibiotics used as an anti inflammatory Can last for months to years if not treated Discontinuation of steroids—may need weaning off due to steroid "addiction" or can have a flare up
question
What do you need to keep in mind when you see acne?
answer
Acne can be one of the presenting signs of systemic disorders. Look at the underlying causes.
question
Epidermal Inclusion Cysts

answer
Benign growths of the upper portion of the hair follicle Dermal tumors containing sebum and keratin debris derived from lining of hair follicle. Clinical findings—Firm dermal papule or nodule. •Overlying black comedone or "punctum" and a cyst sac. •Expressible foul-smelling cheesy material. •Favor the face and trunk •May complicate nodulocystic acne vulgaris •May become red and drain, mimicking an abscess. Assessment (including diagnostic studies)—use dermoscopy Differential diagnosis—lipomas, benign and malignant tumor, melanoma, skin tag Prognosis--if the sac is not removed it will recur Complications—may rupture, creating an acute inflammatory nodule very similar to an abscess Treatment Surgical excision for: Larger cysts (be careful of back midline cysts) Sensitive or cosmetic anatomic sites Those that become recurrently infected Remove with epidermal cyst sac and punctum or recurrence more likely When inflammed/infected may be treated with incision & drainage Pack with iodoform gauze and allow to heal Consider definitive removal after inflammation subsides
question
Recognize the indications, contraindications, risks and benefits for the removal of an epidermal inclusion cysts
answer
Surgical excision for: Larger cysts (be careful of back midline cysts) Sensitive or cosmetic anatomic sites Those that become recurrently infected Remove with epidermal cyst sac and punctum or recurrence more likely When inflammed/infected may be treated with incision & drainage Pack with iodoform gauze and allow to heal Consider definitive removal after inflammation subsides
question
Lipoma

answer
Tumor composed of mature adipose cells Flesh colored, soft, rubbery, sometimes lobulated Family History Treatment Excision only if justified because of sudden enlargement, pain or for cosmetic reasons. Can excise it through a small opening. Usually have more than 1. If there are multiple: Consider syndromes Familial multiple lipomatosis Gardner syndrome Frohlich syndrome Bannaya-Riley Ruvalcaba syndrome Decrum's disease (painful cases)
question
Recognize the indications, contraindications, risks and benefits for the removal of lipomas
answer
Treatment Excision only if justified because of sudden enlargement, pain or for cosmetic reasons. Can excise it through a small opening.
question
Seborrheic Keratosis

answer
Clinical findings Most common benign cutaneous neoplasm Benign papules and plaques, beige to brown or even black, 3-20 mm in diameter, and have irregular borders Sometimes called "barnacles" Inherited familial tendency Rare before age 30. Hormonal influence—perimenopause, pregnant women More likely in face, scalp, trunk, arms and back Lesions have a waxy or warty like appearance and look like they are stuck on. Differential diagnosis: malignant melanoma Treatment: Cryosurgery—frostbite and leaves a white scar Reassurance Curettage Routine skin exams to watch for melanoma Sign of Lesser Trelat—SK that grows can become melanoma
question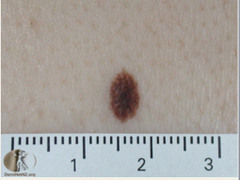
Nevi
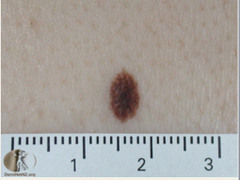
answer
Clinical findings: A benign mole is a small (less than 6 mm) macule or papule with a well-defined border and homogeneous beige or pink to dark brown pigment Appear in childhood--stable age 35 •Junctional—cells are at the junction of the epidermis and dermis Should be well demarcated and symmetrical and uniform in color •Atypical/dysplastic—Irregular border and distribution of color, bigger than 6 mm, evaluated by dermoscopy. o2 First-degree relatives that had melanoma makes it even more important to monitor for atypical nevi. 50% of getting multiple by age 50. •Blue—small and slightly elevated nevi that favor the dorsal aspect of the hands Risk factors: Melanoma is possible for atypical nevi. 2 First degree relatives that had melanoma increases chances. 50% by age 50. Etiology: Exposure to the sun can lead to changes in nevi to become atypical. Genetic. Assessment (including diagnostic studies): look at diameter, color, border and could biopsy. Differential diagnosis: could just be a junctional nevi or blue nevi, melanoma Prognosis: one of the most common skin cancers Complications: could lead to melanoma Prevention: Patients need to be educated to recognized changes in moles and monitor them regularly (6-12 months) Treatment: Frequent visits to the doctor, patient education. Do NOT ruin the architecture of the mole when removing it. Remove the whole mole by shave, punch, ellipse. Removal for cosmetic reasons or because of: Irritation/Inflammation Bleeding/changes Clinically suspicious or evolution Atypical appearance or change in appearance Worrisome features include: Blue/grey/black/pink or unusual pigmentation Asymmetry or Irregular distribution of pigment Irregular borders Larger then 8mm Sudden onset of growth of a stable one ABCDEs--Asymmetry Borders Colors Diameter Evolution Ugly duckling/black sheep one
question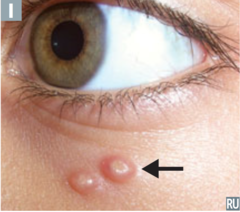
Molluscum Contagiosum
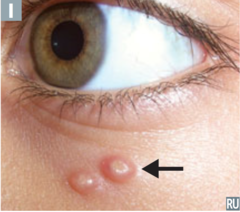
answer
Risk factors—common in those with AIDS and T-Cell lower than 100/mcL Etiology—caused by a poxyvirus Clinical findings—dome shaped, benign, waxy papules that are 2-5 mm in diameter and are umbilicated •Lesions at first are firm, solid, and flesh-colored but upon reaching maturity become soft, whitish, or pearly gray and may suppurate. •On lower abdomen, face and genitals •Spread by wet skin to skin contact •Sexually transmitted Differential diagnosis Treatment—Spontaneous resolution, curettage, cryosurgery, I&D, laser, Aldara or liquid nitrogen, 10% KOH solution applied twice a day. Treat with cantheradin, or monitoring and reassurance. Considered STI if in genital areas Take the ball out—that is the part that is contagious. Not life threatening. 4 can turn into 400. Should treat right away.
question
Questions to ask if there is an allergic reaction
answer
NEW MEDICATIONS •INSECT BITES/STINGS •FOODS •NEW LOTIONS, SOAPS, DETERGENTS, SHAMPOO/CONDITIONER •ENVIRONMENTAL EXPOSURES
question
How does an allergic reaction present?
answer
ERYTHEMA: REDNESS AND LOCAL INFLAMMATION (INCLUDES PAIN & PRURITUS) •URTICARIA (HIVES): RED/WHITE ROUND, RAISED WELTS •ANGIOEDEMA: LOCALIZED SUBCUTANEOUS SWELLING, WHICH RESULTS FROM EXTRAVASATION OF FLUID INTO INTERSTITIAL TISSUES •COMMONLY AFFECTS FACE, LIPS, MOUTH, THROAT, UVULA, PHARYNX, •NAUSEA OR VOMITING •ANAPHYLAXIS: RAPID ONSET LIFE THREATENING REACTION WHICH MAY INVOLVE MUCOSAL SWELLING, DIFFICULTY BREATHING, URTICARIA, NAUSEA/VOMITING, AND HYPOTENSION •CAN OCCUR TO EITHER A NEW OR KNOWN ALLERGEN •TYPICALLY INVOLVES TWO OR MORE BODY SYSTEMS (EX: HIVES AND SHORTNESS OF BREATH--skin and airways)
question
How do you treat ANAPHYLAXIS OR ANGIOEDEMA?
answer
•FLUID RESUSCITATION TO CORRECT HYPOTENSION •EPINEPHRINE 1:1000 CONCENTRATION IM •IV EPINEPHRINE INFUSION SHOULD BE USED IF SIGNS OF SHOCK OR IF UNRESPONSIVE TO IM •ENDOTRACHEAL INTUBATION IF AIRWAY EDEMA OR COMPROMISE •STEROIDS (EXAMPLE: METHYLPREDNISOLONE OR PREDNISONE) •H1 ANTAGONISTS (EXAMPLE: DIPHENHYDRAMINE) •H2 RECEPTOR ANTAGONISTS (EXAMPLE: FAMOTIDINE) •USE A BETA AGONIST IF BRONCHOSPASM (EXAMPLE: ALBUTEROL) •ADMIT TO THE HOSPITAL •REFER TO ALLERGIST
question
How do you treat urticaria?
answer
•STEROIDS •H1 BLOCKER •H2 BLOCKER •OBSERVE FOR 6 HOURS; IF IMPROVING, DISCHARGE HOME WITH RX FOR STEROIDS
question
HYMENOPTERA Stings and Bites Local and systemic reactions
answer
INCLUDES WASPS, BEES, AND STINGING ANTS Local reaction: PAIN, ERYTHEMA, EDEMA, AND PRURITUS AT THE STING SITE Fire ants--LOCAL REACTION CONSISTS OF A STERILE PUSTULE THAT EVOLVES OVER 6 TO 24 HOURS •CAN RESULT IN NECROSIS AND SCARRING •SYSTEMIC REACTIONS INCLUDE: URTICARIA, ANGIOEDEMA, AND ANAPHYLAXIS •MASSIVE ENVENOMATION MAY DEVELOP SEVERE VOMITING, DIARRHEA, RHABDOMYOLYSIS, MYOCARDIAL INJURY, HEPATIC FAILURE, AND RENAL FAILURE
question
Treatment for hymenoptera stings and bites
answer
Treat the anaphylaxis: fluid resuscitation, steroids, epinephrine, H1 and H2 antagonists. DIPHENHYDRAMINE and FAMOTIDIN respectively. Urticaria with steroids and H1 and H2 blockers. If more than 100 stings, admit to the hospital Less than 100, make sure renal functioning is fine. NORMAL CK AND UA TO INDICATE NO RHABDOMYOLYSIS. Remove the stinger. ANY PATIENT WITH A SYSTEMIC REACTION SHOULD BE PRESCRIBED AN EPIPEN AUTOINJECTOR •TEACH HOW TO USE AND WHEN TO USE •PATIENT SHOULD CARRY A MEDICAL ALERT BADGE OR BRACELET •ANY PATIENT WITH A SYSTEMIC REACTION SHOULD BE REFERRED TO ALLERGY & IMMUNOLOGY clinic Can get a delayed reaction 5-14 days later.
question
Bite by a brown recluse spider
answer
VENOM CONTAINS ENZYME SPHINGOMYELINASE, WHICH IS THOUGHT TO CAUSE NECROSIS AND SYSTEMIC SYMPTOMS. Usually on the arm, thorax and inner thighs. Don't feel the bite; but will have 2 small puncture marks with redness RED PLAQUE FORMS WITH POSSIBLE CENTRAL PALLOR; VESICULATION MAY OCCUR •PAIN MAY BE SEVERE FROM 2-8 HOURS POST BITE •TYPICALLY RESOLVES WITHOUT INTERVENTION IN ONE WEEK Can become necrotic--10% of cases ORIGINAL PAPULE OR PLAQUE BECOMES DUSKY RED OR BLUE COLOR IN THE CENTER •DRY DEPRESSED CENTER FORMS AN ESCHAR •ESCHAR BREAKS DOWN TO FORM AN ULCER •TYPICALLY 1-2 CM IN DIAMETER, THOUGH CAN BE UP TO 40 CM •MOST COMMONLY OCCUR OVER FATTY TISSUE ON THE BUTTOCKS OR THIGHS •USUALLY STOP ENLARGING BY 10 DAYS •HEAL WITHIN SEVERAL WEEKS ON THEIR OWN ACCORD; RARELY REQUIRE SURGICAL INTERVENTION Systemic illness is rare and occurs more often in South America where they have a different species MALAISE, NAUSEA/VOMITING, FEVER, MYALGIAS •RARELY CAUSES ANGIOEDEMA, ACUTE HEMOLYTIC ANEMIA, DISSEMINATED INTRAVASCULAR COAGULOPATHY (DIC), RHABDOMYOLYSIS, MYONECROSIS, RENAL FAILURE, COMA, AND DEATH
question
Diagnosis and treatment of brown recluse spider bite
answer
Only definitive if the spider is identified. REQUIRE LABORATORY STUDIES TO EVALUATE FOR HEMOLYSIS, RHABDOMYOLYSIS, AND ACUTE KIDNEY INJURY •CBC WITH DIFFERENTIAL •TYPE/SCREEN & COOMBS TEST ( IF CONCERNED FOR HEMOLYTIC ANEMIA) •CMP •LACTATE DEHYDROGENASE •SERUM URIC ACID (IF CONCERNED FOR RHABDOMYOLYSIS) •UA •PT/INR AND PTT •FIBRINOGEN & D-DIMER (IF INR OR PTT IS ABNORMAL) •EKG (IF FINDINGS CONSISTENT WITH RHABDOMYOLYSIS) Treatment LOCAL SYMPTOMS •CLEAN WITH SOAP AND WATER •ANALGESIA AS NEEDED •TETANUS PROPHYLAXIS IF NOT UP TO DATE •NECROSIS •NO PROVEN THERAPY; SUPPORTIVE CARE ONLY •SURGERY ONLY FOR LESIONS >2 CM IS RESERVED UNTIL 2-3 WEEKS POST BITE •EARLY CURETTAGE AND EXCISION IS NOT RECOMMENDED; LARGE WOUNDS MAY IMPROVE WITH WOUND VAC •ANTIVENOM ONLY INDICATED IN SOUTH AMERICAN BITES WHO PRESENT FORCARE WITHIN 48 HOURS •NOT COMMERCIALLY AVAILABLE IN THE UNITED STATES •SYSTEMIC SYMPTOMS •PATIENTS WITH SYSTEMIC SYMPTOMS OR LABORATORY FINDINGS CONSISTENT WITH RHABDOMYOLYSIS, HEMOLYSIS, OR DIC SHOULD BE HOSPITALIZED
question
Do you give topical steroids to fungal infections?
answer
This will cause an increased reaction. Have to give steroids with an antibiotic
question
Types of Streptococcus
answer
Alpha hemolytic S. pneumoniae Otitis media, sinusitis, pneumonia, meningitis S. viridans Mouth flora Beta hemolytic Group A (S. pyogenes) Pharyngitis, Scarlet fever, rheumatic fever, necrotizing fasciitis "flesh-eating bacteria" Group B (S. agalactiae) Pneumonia, meningitis, cellulitis
question
Types of Stapphylococcus
answer
Coagulase-negative S. epidermidis (lives on our skin) Bacteremia, prosthetic joint infections S. saprophyticus UTIs Coagulase-positive S. aureus Methicillin-sensitive (MSSA) Methicillin-resistant (MRSA) Hospital-associated MRSA Community-associated MRSA
question
What is the cause of MRSA?
answer
Staphylococcus aureus
question
Staph, Strep, and MRSA cutaneous infections
answer
Cellulitis Associated with abscess or furuncles: possibly S. aureus Diffuse: may be Strep Erysipelas Strep, usually S. pyogenes Impetigo S. aureus or S. pyogenes (group A strep) Skin Abscesses S. aureus, especially community-associated MRSA Diabetic Foot ulcers Pyomyositis S. aureus Necrotizing Fasciitis Monomicrobial (Type II) group A streptococcus (GAS, Streptococcus pyogenes) Staphylococcus aureus (MSSA or MRSA)
question
Skin Abscesses

answer
Painful, tender, fluctuant nodules S. aureus, especially community-associated MRSA Other organisms depending on anatomic location Treatment: incision and drainage—just as good as antibiotics Role of antibiotics after I&D is uncertain Would treat high-risk patients, and others depending on severity of infection Must cover MRSA while awaiting cultures Not severe-oral antibiotics--doxycycline Severe-IV antibiotics
question
Diabetic Foot Ulcers

answer
Usually polymicrobial. Require broad-spectrum antibiotic therapy. Treatment Adequate surgical debridement is extremely important--primary treatment (antibiotics can't penetrate dead tissue) PO therapy possible in most cases. Duration depends on several factors--is it a deeper infection? Underlying osteomyelitis? Adequate debridement? All dead tissue cleaned out? S. aureus present?
question
Pyomyositis

answer
Presence of pus within muscle groups S. aureus, occasionally other organisms Geographical distribution, so called 'tropical pyomyositis' (more frequent in temperate climates) Localized pain in a single muscle group, muscle spasm, fever Treatment Surgical incision and drainage necessary--primary Antibiotics depending on culture results--initial antibiotics for staph
question
Necrotizing Fasciitis
answer
Polymicrobial (Type I) mixed infection caused by aerobic and anaerobic bacteria --occurs most commonly after surgical procedures and in patients with diabetes and peripheral vascular disease Monomicrobial (Type II)--one type of bacteria group A streptococcus (GAS, Streptococcus pyogenes) Staphylococcus aureus (MSSA or MRSA) Can occur in any age group and in patients without underlying medical conditions Clinical Findings Unexplained pain, increasing very rapidly over time. Initially overlying skin looks fine. Changes to a red-purple/blue grey within days. Pain out of proportion to exam. subcutaneous gas--crepitis. "Woody" feeling of subcutaueous tissues Blisters/bullae, Fever, Malaise/myalgias Signs of systemic toxicity--hypotension, tachycardia Type 1 Starts in cervical area--dental procedures Male perineum- fournier's gangrene, omphalitis (neonate's umbilical cord--MRSA infected) Assessment with Diagnostic Tests Clinical suspicion Leukocytosis Elevated CK, Creatinine Imaging (CT/MRI) Blood cultures Cultures of bullae (aspirate) are usually NOT useful Prompt surgical exploration with deep tissue cultures--usually diagnosed in the operating room Treatment Surgical debridement of necrotic tissue Aggressive debridement amputation Medical Antimicrobials IV crystalloid fluids and vasopressorsas needed Broad-spectrum empiric IV antibiotic therapy A carbapenem (ex: meropenem) or beta-lactam-beta-lactamase inhibitor (ex: piperacillin-tazobactam) plus •Clindamycin (provides antitoxin effects against toxin-elaborating strains of strep and staph) plus •An agent with activity against MRSA (ex: vancomycin) Penicillin to immunocompromised Adjunct Possibly IVImmunoGlobulin for severe systemic infections (neutralize toxin) Hyperbaric oxygen therapy (HBO)
question
What are the special circumstances of necrotizing fasciitis?
answer
These require different course of antibiotics compared to NF with staph aureus. Saltwater exposure: Vibrio vulnificus Freshwater exposure: Aeromonas hydrophila --lakes, stream, rivers
question
Black Widow Spider Bite

answer
Black with red markings. Venom contains the neurotoxin alpha-latrotoxin •ACETYLCHOLINE, NOREPINEPHRINE, DOPAMINE, GLUTAMATE, AND ENKEPHALIN SYSTEMS ARE ALL SUSCEPTIBLE TO THE TOXIN Signs and Symptoms Mild pinprick bite. 75% are usually on the lower extremities while working outside. Target like lesion and erythema. Systemic symptoms Myalgia--usually abdominal rigidity; back and trunk Radiating pain. Sweating, vomiting, headaches, tachycardia. Diagnosis Made clinically with history--need to catch/see spider COMPLICATIONS Rhabdomyolysis, toxic epidermal necrolysis, ileus, cardiomyopathy Treatment Mild: local skin irritation with muscle pain adjacent to the bite Do a tetanus prophylaxis shot. Oral analgesics as needed for pain: acetaminophen, ibuprofen, hydrocodone, oxycodone Oral benzodiazepines for spasms--valium Moderate: generalized spasmodic muscle pain, involving back, chest, abdomen, sweating Severe: pain and systemic symptoms of HTN, nausea, headache, vomiting Tetantus shot, local wound care, benzodiazepines for spasms. Parenteral opioids for pain. Antiemetic thereapy--ondanestron for nausea/vomiting Use antivenom when mod. to severe treatment doesn't work. Can cause hypersensitivity, anaphylaxis.
question
Bed Bugs

answer
Obligate blood feeding insects that have blood meals of 5-10 minutes. CIMEX LECTULARIUSAND C. HEMIPTERUS--affect humans Common in homes and beds that are frequented by travelers and economically poor homes. Bites usually occur on face, neck, hands, and arms. Asymptomatic pruritic macules 2 to 5 mm erythematous papule or wheal with a central punctum. Can have bullae. Diagnosis: Linear brown streaks of fecal matter on bed sheets. Need to trap the bugs. Treatment Medium potency topical corticosteriod--hydrocortisone 2%. Oral antihistamine--diphenhydramine or hydroxyzine Have to remove the bed bugs
question
Lice (pediculosis capitis)

answer
Adult head bugs are grey-white 2-3 mm in length with eggs called nits. Transmitted through direct contact of the head with the infected individual. Clinical findings Scalp pruritus caused by an allergic reaction to the bug saliva that is injected during feeding. Excoriations on the scalp, neck, and postauricular skin. Diagnosis Wet combing of the hair and visualization of the lice. Use wood's lamp (black light) to see the blue color of the nits. Need to have many in number less than 6.5 mm from the scalp. Treatment Topical pediculicides are 1st line. Permethrin about 2 months Apply shampoo and let it sit for 10 minutes and then wash it out. Use oral ivermectin if failure with the topical agent. Wash and dry bed sheets and clothes of infected with high heat. Or store clothes and linens in plastic bags for 2 weeks and bugs will die.
question
Pressure Ulcers
answer
Localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction. 1-3 million people develop these a year. 60,000 die a year from complications. Cause: prolonged tissue ischemia caused by pressure that exceeds the tissue capillary pressure. Prolonged pressure deprives tissues of oxygen and essential nutrients leading to ischemia and hypoxia which then causes the problem Need 32 mm Hg to close the capillaries. Prevention: Need to reorient the patient's position--2 hours. Provide padding for bony prominences. Identify those at risk: Elderly Chronically ill Cancer, Stroke, Diabetes Immobile Related to fracture, arthritis, pain Weak or debilitated Altered mental status Narcotics, anesthesia, coma Decreased Sensation Paralysis Secondary factors at risk: Illness or debilitation, Fever, Increases metabolic demands, Predisposing ischemia, sweating, Incontinence Skin irritation, contamination, and maceration, Edema, and dry skin. Treatment: find out the underlying systemic cause. Treat nutritional deficits. Multidisciplinary approach--many teams involved. Cleaning—most often skipped Controlling infections Debridement---dead is dead and you're not bringing it back--Need to remove this in order to heal Dressings that promote a moist wound environment > dry Systemic antibiotics if systemic issues. Staging is based on anatomical depth. Once it reaches a certain stage and is on the way to healing, it is always called that stage.
question
Secondary patho-physiologic factors for pressure ulcers
answer
Fever Anemia Infection Ischemia Hypoxemia Malnutrition Spinal cord injury Neurological disease
question
primary patho-physiologic factors for pressure ulcers
answer
Compression Maceration--moisture, tissure damage Immobility--in bed tens to cause issues on the sacrum, heels, malleoli, and trochanteric regions, and ischial tuberosities. Pressure--on bony prominences Friction--dragging force; two surfaces rubbing against each other. Maceration, moisture, tissue damage makes it more susceptible to tissue breakdown. example: sliding across the bed. Shear-- force at a parallel to the area of pressure example: sacral area; downward parallel force while sitting pushing on the skin
question
Staging of pressure ulcers determined by
answer
Based on anatomical depth.
question
Stage 1 of pressure ulcers
answer
STAGE I Intact skin with non-blanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin may not have visible blanching; its color may differ from the surrounding area. Treatment—get them off of that area
question
Stage 2 of pressure ulcers
answer
Stage II: Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough (will not have the yellow or black color—dermis won't present this). May also present as an intact or open/ruptured serum-filled blister. Superficial
question
Stage 3 of pressure ulcers
answer
Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle are not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling. Don't see this phase very often because it goes quickly to stage 4
question
Stage 4 of pressure ulcers
answer
Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often include undermining and tunneling.
question
Unstageable stage of pressure ulcers
answer
Full thickness tissue loss in which the base of the ulcer is covered by slough (yellow, tan, gray, green or brown) and/or eschar (tan, brown or black) in the wound bed. It is at least full thickness
question
Suspected Deep tissue injury
answer
Purple or maroon localized area of discolored intact skin or blood-filled blister due to damage of underlying soft tissue from pressure and/or shear. The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue. If opened up, it would be full thickness ulcer
question
Steven Johnson Syndrome and Toxic Epidermal Necrolysis

answer
1. With less than 10% BSA detachment--mucous membrane affected at 2 or more distinct sites 2. Greater than 30% BSA detachment Overlap for cases with between 10% and 30% BSA detachment. Risk Factors: more likely in an HIV infected person Pathophysiology—Apoptosis of keratinocytes provoked by the activation of a cell-mediated cytotoxic reaction and amplified by cytokines, mainly granulysin •Involved with sulfonamides, NSAIDs, allopurinol, and anticonvulsants—may be systemic or topical Clinical findings—1-3 days of flu like symptoms--fever, malaise Sudden onset of symmetric erythematous skin lesions with history of recurrence. •May be macular, papular, urticarial, bullous, or prupuric. Starts on the neck and thorax and then moves to extremities. •"Target" lesions with clear centers and concentric erythematous rings or "iris" lesions. Well-defined target lesions are rare •two zones of color change and a central blister, or nondescript reddish or purpuric macules favoring the trunk and proximal upper extremities. Oral mucosa involved in 90% of cases at the vermillion border. Ocular mucosa in 80%-conjunctivitis and purulent discharge. Genital erosions. Positive Nikolsky sign--sloughing of epidermis Assessment (including diagnostic studies)—skin biopsy CBC with diff -anemia and lymphopenia CMP -Hypoalbuminemia, electrolyte imbalance, and increased blood urea nitrogen and glucose--kidney functioning Differential diagnosis—autoimmune bullous diseases (eg, pemphigus, pemphigoid, and linear IgA bullous dermatosis), acute systemic lupus erythematosus, vasculitis, and Sweet syndrome. Prognosis—may be serious with a mortality of about 30% in cases with greater than 30% BSA involvement. SCORTEN (a severity of illness scale) predicts mortality--based on 7 points. Complications—dehydration, vision loss, hypovolemic shock, electrolyte imbalance, Multiple organ dysfunction syndrome (MODS), insulin resistance, infection with staph, respiratory failure Prevention—never take the offending medication again Treatment—NEED to have the patient see an ophthalmologist because they could lose their vision •Go to an ICU •Discontinue the medication that caused it and NEVER take it again •Need nutritional and fluid support and treat for infection IV crystalloid fluids like lactated ringers Nonadherent, nanocrystallinegauze materials containing silver or petrolatum-infused gauze Chlorhexidine for topical disinfectant IV narcotics for pain. •Corticosteroids need to be started early—prednisone •Intravenous immunoglobulin •Tumor necrosis factor
question
DRESS (Drug reaction with eosinophilia and systemic symptoms)

answer
drug-induced hypersensitivity reaction •2-8 weeks between drug exposure and disease onset Associated with a reactivation of herpes virus Medications that cause--carbamazepine or phenytoin, lamotrigine Allopurinol, Phenytoin, Sulfasalazine, Vancomycin, Minocycline, Dapsone, Sulfamethoxazole Clinical findings Diagnosis based on-- Skin eruption •Fever •Facial edema •Lymphadenopathy •Exposure to a high-risk medication within 2-6 weeks Initial--Fever, Malaise, Lymphadenopathy, inflammation of mucus membranes Involves the face, upper trunk and extremities Skin eruption ≥50 percent of the BSA and/or includes two or more of: •Facial edema (affects ~50% of patients) •Infiltrated lesions •Scaling •Purpura Red papules and desquamation of palms and soles Internal organ involvement--liver is most common (look for increased liver function tests and bilirubin) Kidney and lungs Assessment CBC with diff & peripheral blood smear (Leukocytosis, high eosinophil count, atypical lymphocytosis) •CMP (increased ALT) •Urinalysis •EKG & Troponin Check for HIV positive Prognosis--can persist for months and occur again, death Treatment Do not take the drug ever again No organ involvement--topical high or super-high potency steroids like betamethasone or clobetasol x 1 week Organs involved: systemic steroids like prednisone 0.5-2mg/kg PO for lung or kidney involvement
question
Neonatal acne

answer
Small pustules on face/ scalp of neonate Presents within 3 months of birth Resolves 1-3 months after appearance No treatment is necessary, will resolve Due to maternal hormones or colonization of Malassezia Some use clotrimazole (Lotrimin- OTC antifungal), but can affect bilirubin levels if used too liberally and is absorbed systemically
question
Infantile Acne

answer
> 6 months old - 3 years old Comedones, papules, pustules, nodules Does have scarring potential May be linked to precocious puberty--may need to be evaluated by an endocrinologis Treatment Topical BZP or erythromycin May need oral antibiotics Cannot use tetracycline family in children because it can stain the enamel of the permanent teeth
question
Verruca

answer
Etiology—caused by the Human Papilloma virus Clinical findings—papules anywhere on the skin or mucous membranes, usually no larger than 1 cm in diameter. •Prolonged incubation period (average 2-18 months). •Spontaneous "cures" are frequent in common type (50% at 2 years). •No symptoms •Pain with pressure—plantar •Itching on anogenital Differential diagnosis—hypertrophic actinic keratosis or squamous cell carcinoma, syphilis, AIDS—wart like lesions from varicella zoster virus, molluscum contagiosum Prognosis—"Recurrences" (new lesions) are frequent. Complications—scarring, hypopigmentation from removal Prevention—vaccine against certain anogenital HPV types (including 6, 11, 16, 18) Treatment—liquid nitrogen or keratolytic agents like salicylic acid •Genital warts—podophyllum resin (don't use if pregnant) and Imiquimod need several treatments (not for plantar warts) •Plantar warts—operative removal, bleomycin (injected) •Laser therapy •Photodynamic therapy LN2/ cryotherapy Duct tape with OTC Electrosurgery/ Excision Imiquimod/ 5-FU Cantharidin (blister beetle juice) CO2 or pulse dye laser
question
Diaper Dermatitis

answer
Caused by Contact sensitivity Irritant Allergic Bacteria Yeast Clinical findings Diapers cause prolonged occlusion and expose the skin to urinary ammonia and fecal enzymes Well demarcated erythema, scaling and maceration Often spares inguinal creases Allergic: often due to rubber components in diapers or dye used in patterned diapers Moisture exposure is prime environment for yeast overgrowth Yeast usually colonizes an irritant dermatitis within 72 hours Typical sign is spread to other intertriginous zones Treatment Need to change diaper frequently Have diaper free time Topical moisture barriers-Petroleum jelly Also important to try different diaper brands or diapers without prints Topical nystatin or clotramizole
question
Birthmarks
answer
Usually benign Treatment options are early excision or monitor over time Some go by 1 cm guideline Lesion will grow as child grows Have to consider risk of melanoma vs. surgery risk
question
Infantile seborrheic dermatitis

answer
"Cradle cap" Salmon colored erythema and greasy scale Self limited Can decrease scale with baby oil and fine toothed comb Low potency topical steroids, tar based shampoos, topical antifungals Often on scalp, but can be present on face, eyebrows etc. Often resolves on its own- within 12 months Treatment Can use low potency topical steroids like desonide, hydrocortisone 2.5% Some use selenium sulfide, ketoconazole or cicloprox
question
Systemic Lupus Erythematosus (SLE)

answer
Autoimmune disease affecting multiple systems (skin, joints, kidneys) Malar rash (butterfly rash) or Discoid rash (circular) Looks like a permanent "wind chap" Often need heavy sun protection and coordination of care with rheumatologist Use SPF 50 or greater. Assessment Blood tests reveal circulating autoantibodies--Antinuclear antibody is positive (not always diagnostic) Take a biospy--lesional and perilesional (gets special stains) Treatment Antimalarials can be helpful--plaquinal (decrease inflammation; need to watch kidney function and get eye exam)
question
Dermatomyosisitis
answer
Rare acquired muscle disease that is accompanied by a skin rash Clinical findings Usually women age 50-70 Heliotrope rash--Upper eyelid bilateral rash Gottran's papules--on hands Treatment Oral corticosteroids Switch to steroid sparing agent later--methotrexate
question
Diabetes Mellitus
answer
High blood sugar levels Complications Foot ulcers Can get shin spots Indented hyperpigmented patches that range in pigment from light brown to purple 30% of patients Due to the conditioin causing changes in small blood vessels of lower extremity Assessment Hemoglobin A1c Blood glucose levels
question
Necrobiosis Lipoidica Diabeticorum (NLD)

answer
Clinical Findings Raised, shiny red/ brown patches that can be yellowish on shin Can develop sores within them that are difficult to heal Looks like a shiny scar with a violet border Assessment Need biopsy to confirm Can be the first sign of DM in some patients Treatment: Support stockings, IL steroids, topical steroids Some thought to using tacrolimis or pulse dye laser
question
Tuberous sclerosis

answer
Clinical findings Genetic disorder Hamartomas on many organs Noncancerous malformations made up of an overgrowth of cells that normally occur in the affected area 3+ "ash leaf" white macules at birth or in infancy can be an indicator Normal organs involved: skin, brain, eye, kidney, heart Complications: high risk for seizures Skin lesions, epileptic seizures and developmental delay common Differential Diagnosis: vitiligo
question
Vasculitis

answer
Clinical findings Inflammation of blood vessels in skin Many are self limiting Often times specific cause is not found Often causes purpuric lesions from blood hemorrhaging into skin Thrombosis can cause tissue necrosis Can affect small, medium and large vessels Biopsy and low dose prednisone
question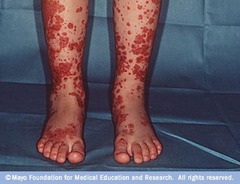
Henoch Schonlein Purpura (HSP)
answer
Children most common Palpable purpura on legs and buttocks Possible systemic involvement Self limited 50% recurrence rate Treatment Could give prednisone but usually weight it out
question
Disseminated Intravascular Coagulation (DIC)

answer
Rapidly evolving widespread purpura Results from severe multisystem disease Caused by uncontrolled activation of clotting factors in blood vessels blood clots throughout the body -body is depleted of platelets -paradoxical increased risk of bleeding Main cause is infection Can also be from acute injuries Heparin is appropriate to treat the thrombosis that occurs with DIC.
question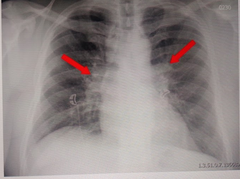
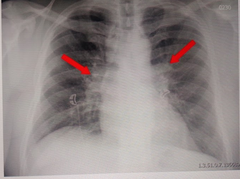
Sarcoidosis
answer
Clinical findings Unknown etiology Differential Diagnosis Shows up as granulomas usually in lungs, but can have several skin findings: Erythema nodosum Lupus pernio Violaceous rash on cheeks Plaques on skin Thickening of scar tissue Assessment Punch biopsy Panel of autoantibodies Treatment IL steroids Potent topical steroids Systemic Steroids Immunosuppressive agents Antimalarials >75% of patients only require symptomatic therapy with NSAIDS. Usually on prenidsone taper over 6 months Antimalarials: have immunomodulating properties
question
Hidradenitis suppurativa (acne inversa)

answer
Self Limited Immunosuppressed obese women Painful, pustules, papules, nodules Severe: sinuses, abscesses, scars Draining In your armpits and groin Smokers Assessment: sterile Treatment Topical steroid Bleach bathes
question
Exanthems

answer
Widespread rash that is usually accompanied by systemic symptoms such as fever, malaise and headache. It is usually caused by an infectious condition such as a virus, and represents either a reaction to a toxin produced by the organism, damage to the skin by the organism, or an immune response. Caused by Chickenpox (varicella) Measles (morbillivirus) Rubella (rubella virus) Roseola (herpes virus 6B) Pityriasis rosea (herpes virus 6 and 7) Erythema multiforme Symptoms Fever Malaise Headache Loss of appetite Abdominal pain Irritability Muscular aches and pains Treatments Paracetamol to reduce fever Moisturizing emollients to reduce itch
question
Condyloma (genital warts)

answer
Treatment Freeze Podophyllum resin (don't use if pregnant) and Imiquimod need several treatments (not for plantar warts)
question
Perioral dermatitis

answer
Pinpoint papules and pustules only No comedones Can progress to periorbital Idiopathic Can be correlated anecdotally to topical steroid use, occlusive cosmetics, or stress Treatment: Oral antibiotic, usually minocycline and topical metronidazole or erythromycin Clears in 6 weeks
question
Varicella Zoster

answer
Herpesvirus-HHV3 Dew drop on a rose petals Itchy Spreads from head to toe Highly contagious: transmission via respiratory, direct contact, and vertical maternal means Assessment Culture Tzanck PCR Serologic testing Complications Secondary infections CNS complications perinatal: occuring within 10 days of birth 1st trimester: Congenital defects include microcephaly, intrauterine growth retardation, asymmetrical arm or leg lengths, ocular abnormalities Treatment Acycolivir
question
Erythema multiforme

answer
Pathophysiology—Herpes simplex is the most common cause of erythema multiforme minor—90% of cases Clinical findings •Sudden onset of symmetric erythematous skin lesions with history of recurrence. •May be macular, papular, urticarial, bullous, or purpuric. •"Target" lesions (with 3 zones of color) with clear centers and concentric erythematous rings or "iris" lesions may be noted in erythema multiforme minor. •Erythema multiforme minor presents on the extensor surfaces, palms, soles, or mucous membranes. Assessment (including diagnostic studies)—skin biopsy, negative immunofluorescent testing Differential diagnosis—urticaria and drug eruptions Prognosis—last 2-6 weeks and may recur Complications—scarring and toxic epidermal necrolysis Prevention—Oral acyclovir prophylaxis of herpes simplex infections may be effective in preventing recurrent herpes-associated erythema multiforme minor Treatment—Oral and topical corticosteroids are useful in the oral variant Prednisone Acyclovir
question
Drug eruptions
answer
Risk factors—Pigmentation may be produced by certain medications, eg, chloroquine, chlorpromazine, minocycline, and amiodarone. •Nonsteroidal anti-inflammatory drugs (NSAIDs) may produce an eruption very similar to that of dyshidrosis on the hands. •Certain genetic polymorphisms of antigen-presenting major histocompatibility (MHC) loci increase the risk for the development of severe drug eruptions, including SJS/TEN and DIHS. Etiology Pathophysiology—Amoxicillin, TMP-SMZ, and ampicillin or penicillin are the most common causes of urticarial and maculopapular reactions. •SJS and TEN are most commonly produced by sulfonamides, anticonvulsants, allopurinol, and NSAIDs. •Phenolphthalein, pyrazolone derivatives, tetracyclines, NSAIDs, TMP-SMZ, and barbiturates are the major causes of fixed drug eruptions Clinical findings—Usually, abrupt onset of widespread, symmetric erythematous eruption. •May mimic any inflammatory skin condition. •Constitutional symptoms (malaise, arthralgia, headache, and fever) may be present •Fixed drug eruptions to phenolphthalein (in laxatives), TMP-SMZ, NSAIDs, and tetracyclines also lead to hyperpigmentation, typically in annular patches. •Drug eruptions are generally classified as "simple" or "complex," referring to the risk of morbidity and mortality associated with the specific eruption. Simple drug eruptions involve an exanthem, usually appear in the second week of medication therapy, and have no associated constitutional or laboratory findings Assessment (including diagnostic studies)—Routinely ordered blood work is of no value in the diagnosis of simple drug eruptions. •In complex drug eruptions, the CBC, liver biochemical tests, and renal function tests should be monitored. •Skin biopsies may be helpful in making the diagnosis. •Serum PCR for HHV-6, Epstein-Barr virus, and cytomegalovirus are routinely performed in some centers. Differential diagnosis—DIHS occurs later than the simple morbilliform drug eruptions with signs and symptoms developing 2-6 weeks after the medication has been started and has associated constitutional and laboratory findings. These may include fevers, chills, hematologic abnormalities (especially eosinophilia), and abnormal liver or kidney function. Prognosis Complications—myocarditis, hypothyroidism Prevention—Pharmacogenetic testing is becoming increasingly utilized to predict who is at risk for and therefore should avoid certain medication exposures Management—Antihistamines may be of value in urticarial and angioneurotic reactions. • Epinephrine 1:1000, 0.5-1 mL intravenously or subcutaneously, should be used as an emergency measure. • In DIHS, systemic corticosteroids is typically used
question
Types of Non-scarring (non-cicatricial) alopecia
answer
Telogen Effluvium Androgenic Alopecia Alopecia Areata Anagen Effluvium Trichotillomania (trichotillosis) Syphilitic Alopecia--moth eaten appearance Endocrinologic Alopecia --Hypothyroidism --Nutrient Deficiency
question
Types of Scarring alopecia
answer
Secondary--from trauma, infection, malignancy Lupus Erythematosus Discoid Lupus Lichen Planopilaris (LPP) Central Centrifugal Cicatrical Alopecia (CCCA) Hot Comb Alopecia Folliculitis Decalvans Pseudofolliculitis barbae Acne keloidalis nuchae Dissecting Cellulitis
question
Alopecia
answer
Risk factors—heart disease and diabetes Clinical findings—Present follicular markings suggest a nonscarring •absent follicular markings suggest a scarring •Telogen—transitory increase in the number of hairs in the telogen (resting) phase of the hair growth cycle. •Pull out the hairs and they will have a white bulb or club end •Hair loss is 150 a day •Typically, there are patches that are perfectly smooth and without scarring. •Tiny hairs 2-3 mm in length, called "exclamation hairs," may be seen. •Telogen hairs are easily dislodged from the periphery of active lesions. The beard, brows, and lashes may be involved. Involvement may extend to all of the scalp hair (totalis) or to all scalp and body hair (universalis). Assessment (including diagnostic studies)—Hair pull test. Serum testosterone, DHEAS, iron, total iron-binding capacity, thyroid function tests, vitamin D level, and a complete blood count will identify most other causes of hair thinning in premenopausal women. Prognosis—some casses are self-limiting, with complete regrowth of hair in 80% of patients with focal disease •Permanent—no regrowth for cicatricial—scarring Complications—Nonscarring alopecia may occur in association with various systemic diseases, such as SLE, secondary syphilis, hyperthyroidism or hypothyroidism, iron deficiency anemia, vitamin D deficiency, and pituitary insufficiency—treat the underlying disease! Treatment—minoxidil 5% is available over the counter and finasteride and can be specifically recommended for persons with recent onset (less than 5 years) and smaller areas of alopecia—androgenic alopecia •serum testosterone, DHEAS, iron, total iron-binding capacity, thyroid function tests, vitamin D level, and a complete blood count will identify most other causes of hair thinning in premenopausal women.
question
Alopecia areata

answer
Nonscarring, noninfectious Body's immune system attacks the anagen hair—lymphocytes Shaft of hair is more broad than at the bottom—exclamation point hair Patchy distribution Nail pitting Sudden onset Assessment: Hair pull test. Pull 4-6 club hairs = abnormal Normal to lose 100 hairs a day. Punch biopsy; more common with scarring Complications Associated with autoimmune disorders, including Hashimoto thyroiditis, pernicious anemia, Addison disease, and vitiligo. Additional comorbidities may include SLE, atopy, and mental health disease. Treatments Intralesional steroids, systemic immunosuppressives, irritants (anthralin) + minoxidil, PUVA Severe forms may be treated by systemic corticosteroid therapy, although recurrences follow discontinuation of therapy •triamcinolone is injected
question
Chronic Telogen Effluvium

answer
Clinical findings Diffuse telogen loss including occipital and temporal area Onset usually abrupt Lasts 6 mo to 7 yrs, may resolve spontaneously Postmenopausal women 67% of cases No significant hormone abnormalities Could be due to medications or serious illness or high stress. Treatment Reassurance Rogaine 5% foam BID Biotin 5,000 mcg daily Ketoconazole 2% Shampoo
question
Androgenic Alopecia

answer
Clinical findings Onset 3-4 decade, 50% M & F Pathogenesis: Progressive miniaturization, not destruction Decrease duration of anagen Increase percent of hairs in telogen Treatment Finasteride (5α-reductase inhibitor) Beware of sexual side effects Minoxidil - 5% foam twice daily Hair grafting Wigs and weaves Women: OCP (dec. androgen production), spironolactone
question
Trichotillomania
answer
Impulse control disorder Area of short, sparse hair, normal scalp Differential Diagnosis: alopecia areata and tinea capitis Assessment Check KOH, consider biopsy Treatment Open discussion with patient Stress management - conscience effort to decrease trauma Consider antidepressant/antianxiety medication
question
Candida onychomycosis
answer
Destruction of the nail and massive nailbed hyperkeratosis Due to C. albicans Seen in patients with chronic mucocutaneous cadidiasis A sign of immunodepression
question
Paronychia

answer
Inflammatory reaction involving folds of nails Acute (bacterial) or Chronic (yeast) Nail dystrophy is common in chronic cases Primary predisposing factor - separation of eponychium from the nail plate Trauma Moisture-induced maceration Common in bartenders, food servers, nurses, physicians, etc Treatment Protection from trauma Concentrated efforts to keep affected fingernails meticulously dry Incision and Drainage Topical antibiotics (Mupirocin or Polysporin) Systemic antibiotics - if severe Start with penicillin or cephalosporin with broad staphylococcal activity MRSA or a mixed anaerobic bacterial infection should be suspected if remains recalcitrant Augmentin useful for mixed anaerobic Chronic Topical or Oral antifungals lead to cure in only 50% of cases Topical steroids to decrease inflammation and allow for tissue repair is more reliable (80%) Miconazole/nystatin combined with topical corticosteroid cream/ointment
question
Onychocryptosis (Ingrown nail)

answer
Nail acts as a foreign body - may cause exuberant granulation tissue Etiology Improper trimming of nail at the lateral edges Improper fitting shoes Treatment Soaking foot in warm soapy water Removal of inciting trigger (improper shoes or nail care) Surgical avulsion Removal of lateral portion of nail plate Removal of overhanging lateral nailfold Medications Isotretinoin lamivudine, and indinavir (HIV medications)
question
Dermatits Herpetiformis
answer
Intensely pruritic Symmetric involvement of extensor surfaces Arranged singly or in clusters Associated with asymptomatic gluten-sensitive enteropathy Target antigen: tissue transglutaminase (tTG) Treatment Dapsone Gluten free diet Decreases risk of GI lymphoma Prognosis: persists indefinitely but good response to therapy
question
Porphyria Cutanea Tarda

answer
Disease of hemoglobin metabolism Many triggers lead to reduced activity in a specific enzyme in the heme metabolic pathway Excess metabolic products build-up in the skin and lead to ultraviolet light sensitivity Blistering in sun exposed areas, notably dorsal forearms, hands, face Diagnosis-elevated urine porphyrins Treatment-Identify underlying trigger, phlebotomy and sun protection
question
Actinic keratosis
answer
Risk factors—smokers, chewing tobacco, herpetic infections Pathophysiology—can lead to squamous cell carcinoma; pre-malignant Clinical findings-- are small (0.2-0.6 cm) macules or papules—flesh-colored, pink, or slightly hyperpigmented—that feel like sandpaper and are tender. Can be hypertrophic. Can grow on the lip. Found mostly in sun-exposed areas. Differential diagnosis—can lead to squamous cell carcinoma Prognosis—crust over after 10-14 days Complications— SCC Treatment—biopsy, liquid nitrogen cryotherapy, topical therapies5-FU (chemotherapies to stop growth), Imiquimod (zyclara) (fake flu), laser therapy, use a topical steroid to make them feel better, Efudex or carac cream. Photodynamic therapy.
question
Cryosurgery
answer
is best for treating thin, well-demarcated lesions and can be used to treat solitary lesions or small numbers of scattered lesions.
question
Basal Cell carcinoma
answer
Most common skin cancer Risk factors • Fair skin • Blue eyes, red hair, sunburns • Family history • Chronic sun exposure • Old age • Arsenic, tar • Organ transplant • Most frequent skin cancer--#1 Clinical findings •Waxy, pearly papule, erythematous patch greater than 6 mm, or nonhealing ulcer in sun-exposed areas (face, trunk, lower legs). •Papule or nodule with a central scab or erosion—stretch the skin to look at •History of bleeding. Nodular has arborizing vessels Pigmented has black discoloration Superficial has scaly red plaque Morpheaform has a scar look •Differential Diagnosis—pigmented BCC looks similar to melanoma •Prognosis—more likely to recur in those that are immunosuppressed •Complications—scarring •Treatment of BCC—electrodessication and curettage •Punch or shave biopsy •Mohs surgery—removal of the tumor followed by immediate frozen section histopathologic examination of margins with subsequent reexcision of tumor-positive areas and final closure of the defect—gives the highest cure rates (98%) and results in least tissue loss. •therapy for tumors of the eyelids, nasolabial folds, canthi, external ear, and temple; for recurrent lesions; or where tissue sparing is needed for cosmesis. •Imiquimod or Efudex •Prevention—monitor patients yearly to detect new lesions, full body check •Nodular Basal Cell •Chronic cell •Easy bleeding •Pearly border •Telangiectasias—arborizing vessels •Head and neck, and trunk and extremities—sun exposure •Look at this with a dermatoscope
question
Squamous cell carcinoma
answer
Risk Factors • Fair skin (burns easily or rarely tans) • Chronic UV exposure • Geography (closer to equator) • History of prior non-melanoma skin CA • Age >50 yrs • Male gender • Chronic scarring/inflammatory conditions • Smoking (lip SCC) • Organ transplant recipients • Chemical carcinogen exposures • Intense PUVA therapy (>300 treatments) • Human Papilloma virus infection - especially HPV 16 • Immunosuppression (intensity & duration) • >10 actinic keratosis Clinical findings—Nonhealing ulcer or warty nodule. •lesions appear as small red, conical, hard nodules that occasionally ulcerate •Prognosis—lesions appear as small red, conical, hard nodules that occasionally ulcerate •Treatment— •Look at whole body skin checks every 3 months and exam lymph nodes Topical Chemotherapy - Imiquimod (Aldara) - 5-fluorouracil (Efudex) Destruction (no margin control) - Cryotherapy or cryotherapy + curettage - Electrodessication with curettage - CO2 laser ablation - Photodynamic therapy - Intralesional interferon - Intralesional bleomycin - Radiation therapy Margin controlled resection - Excision - Mohs micrographic surgery
question
Bowen's disease
answer
•Intraepidermal—leads to invasive •The lesion is usually a small (0.5-3 cm), well-demarcated, slightly raised, pink to red, scaly plaque and may resemble psoriasis or a large actinic keratosis Treatment Efudex or aldara Liquid nitrogen cryotherapy Radiation therapy Curettage electrodessication (ED/C) Surgical excision
question
Erythroplasia of Queyrat
answer
In-situ SCC Uncircumcised men May progress to invasive SCC Treatment Efudex or aldara Liquid nitrogen cryotherapy Radiation therapy Curettage electrodessication (ED/C) Surgical excision
question
Keratoacanthoma
answer
Low grade SCC Rapid growth over weeks Trauma, sun exposure, HPV 11 and 16 May progress to invasive SCC
question
Melanoma
answer
Risk factors—fair colored skin, men over the age of 70 •A patient with a large number of moles is statistically at increased risk and deserves annual total body skin examination by a primary care clinician or dermatologist, particularly if the lesions are atypical. Pathophysiology—sun exposure Clinical findings—types have different mutations (important in treatment) •lentigo maligna (arising on chronically sun-exposed skin of older individuals)--nose and cheecks •superficial spreading malignant (two-thirds of all arising on intermittently sun-exposed skin)—blue-grey veil o 70% of all o high survivability o wouldn't know until the path report •nodular malignant--Trunk, head and neck, ulcerated and bleeding •acral-lentiginous (arising on palms, soles, and nail beds)—difficult to diagnose and is often missed Has Hutchinson's sign—pigment growing in the skin = positive sign •ocular melanoma •malignant types on mucous membranes •Clinical features of pigmented lesions suspicious are: oirregular notched border where the pigment appears to be spreading into the normal surrounding skin oColor variegation is present and is an important indication for referral •May be flat or raised. oA useful mnemonic is the ABCDE rule: "ABCD = Asymmetry, Border irregularity, Color variegation, and Diameter greater than 6 mm." "E" for Evolution can be added. oLook for "ugly duckling sign." -mole different from others Assessment (including diagnostic studies) •Should be suspected in any pigmented skin lesion with recent change in appearance. •Examination with good light may show varying colors, including red, white, black, and blue. •Order Sentinel lymph node biopsy Differential diagnosis—seborrheic keratosis Prognosis—ten-year survival rates—related to (DEPTH) thickness in millimeters—are as follows: less than 1 mm, 95%; 1-2 mm, 80%; 2-4 mm, 55%; and greater than 4 mm, 30%. With lymph node involvement, the 5-year survival rate is 62%; with distant metastases, it is 16%. Complications—bleeding and ulceration Prevention—refer to a specialist, patient education on looking for atypical moles, do a full body skin inspection •Identify the oncogenic mutation—could lead to current immunotherapies available Treatment—the history of a changing mole (evolution) is the single most important historical reason for close evaluation and possible referral. Sentinel Node Biopsy--Indicated for > 1mm thick Total body skin exams LDH level Vitamin D level—take it Ipilimumab (Yervoy) Vemurafenib (Zelboraf)--BRAF inhibitor Pembrolizumab (Keytruda)--help T cell activity
question
Cutaneous T-cell lymphoma
answer
Mycosis Fungoides most common type. Cancer of the T-lymphocytes (white blood cells) affects skin and blood. Occasionally, it also involves lymph nodes and internal organs. Only 10% will progress to a lymph node. No cure. Patients diagnosed early (disease involving less than 10% of the body) will live a NORMAL LIFE EXPECTANCY. Patch, Plaque and Tumor stages. Cause is unknown. Leukemic form is known as "Sezary syndrome." Incidence: 1/100,000. Males>Females. Most cases diagnosed in 5th & 6th decades. More common in African-Americans than Caucasians. Prognosis Related to 'stage' at time of diagnosis. Multiple stages involved: patch stage, plaque stage, tumor stage, and an erythrodermic form.
question
Kaposi Sarcoma
answer
Risk factors—young black men in equatorial Africa • Homosexual Men with HIV and AIDS • High CD4 count and low viral count Etiology—caused by Herpes virus 8 Clinical findings—Pulmonary type can present with shortness of breath, cough, hemoptysis, or chest pain; it may be asymptomatic, appearing only on chest radiograph. • Red or purple plaques or nodules on cutaneous or mucosal surfaces are characteristic • Marked edema may occur with few or no skin lesions. • Occurs often in the GI tract • Can happen in lungs Management—intralesional chemotherapy or radiation • Reduce doses of immunosuppressants • Cryotherapy • Laser surgery
question
Boils (Furuncles and Carbuncles) Staph Aureus and MRSA
answer
I&D of lesions Suspicious lesions/drainage should have a culture and sensitivity performed to help direct course of treatment Antibiotic therapy initiated to control local cellulitis
question
Mycobacterium marinum

answer
Fish handlers Fish tanks Painful—can get into tendons and joints Can lead to tenosynovitis Can treat with Macrolide, tetracyclines, fluroquinolones and sulfonamide antibiotics Have to do a biopsy—saline soaked gauze for a tissue culture.
question
Leprosy
answer
Slowly developing disease that damages the skin and spreads to the nervous system. Painless ulcers and hypopigmented lesions with decreased sensation. Spread by human to human or contact with Nine banded armadillos Mangabey monkeys Chimpanzees Treatment with antibiotics Tetracyclines, Dapsone, Rifampin, Fluroquinolones
question
8 Serotypes of Herpes virus
answer
HHV 1- 'cold sore / fever blister' causes herpetic gingivostomatitis HHV 2- genital herpes and occasionally oral disease HHV 3- 'shingles / chickenpox' or VZV (varicella zoster virus) HHV4 - 'mono / kissing disease' or EBV (Epstein-Barr virus) HHV 5 - CMV (cytomegalovirus) HHV 6 and 7- 6th disease (roseola infantum) HHV 8 - associated with Kaposi sarcoma (cancer in AIDS patients)
question
Treatments and symptoms for the 8 types of herpes: HHV 1- 'cold sore / fever blister' causes herpetic gingivostomatitis HHV 2- genital herpes and occasionally oral disease HHV 3- 'shingles / chickenpox' or VZV (varicella zoster virus) HHV4 - 'mono / kissing disease' or EBV (Epstein-Barr virus) HHV 5 - CMV (cytomegalovirus) HHV 6 and 7- 6th disease (roseola infantum) HHV 8 - associated with Kaposi sarcoma (cancer in AIDS patients)
answer
1--GROUPED VESICLES ON AN ERYTHEMATOUS BASE that evolve to pustules/vesicles and then become eroded to ulcerations with crusts TREATMENT - Oral antivirals started within 72hours 2--below the waist. Treated with antivirals (Famvir, Valtrex, Zovirax) 3--dewdrop on a rose petal' Treat with oral antivirals 4--Severe fatigue, H/A, ST, fever, swollen lymph nodes, jaundice, morbilliform rash (measles like rash), spots inside mouth, enlarged spleen Can get a rash after taking amoxicillin Epstein barr virus Lymph nodes near the ear—mono Lymph nodes near the throat—strep 5--Can cause mucosal ulcerations and severe complications such as hepatiits, leukopenia, pneumonitis and death. Can be a cause of "Blueberry muffin baby" 6 and 7--Produce acute infection in CD4+ T lymphocytes High fever (102.2 - 104) for a few days then subsides and rash appears. Rash starts on trunk and spreads to legs and neck. Lasts for 1-2 days Can develop febrile seizures 8--Associated with Kaposi sarcoma The virus alone is NOT sufficient for the development of the Kaposi's sarcoma Transmitted sexually and contact with saliva
question
Parvovirus B 19
answer
'Fifth disease' = low grade fever, malaise, "slapped cheek" and rash Can cause polyarthropathy syndrome Can temporarily dcrease or halt the body's production of red blood cells, causing anemia. In pregnancy can lead to hydrops fetalis (especially if contracted before 20 weeks gestation) Other condition seen Erythema multiforme, PPGSS (papular-purpuric "gloves and socks" syndrome (purple hands and feet), ITP, Henoch-Schonlein purpura and pseudoappendicitis
question
Measals
answer
Prodromal fever, cough, coryza (head cold, fever, sneezing) and conjunctivitis followed by a red maculopapular rash that turns reddish brown.
question
Hand-foot-mouth disease HFMD

answer
Caused by coxsackievirus a16 and enterovirus 71 Develops ulcers and sores inside and around the mouth and a rash or grey blisters with a red halo on the hands, feet, legs or buttocks. Early sx = ST , fever, and painful blisters Blister is a 'grey blister with a red raw base'
question
HIV/AIDS
answer
Human immunodeficiency virus Leads to acquired immunodeficiency syndrome (AIDS) leads to progressive failure of immune system and allows life threatening opportunistic infections and cancers Occurs by the transfer of blood, semen, vaginal fluid, pre-ejaculate or breast milk. HIV infects CD4+ T cells, macrophages and dendritic cells. Causes a decrease of CD4+ T cells.



