Derm 12 – Skin Cancer – Flashcards
Unlock all answers in this set
Unlock answersquestion
1. What are the three most common skin cancers? 2. Can you describe the clinical features of these lesions? Would you be able to diagnose one in a relative or patient if you saw it? 3. What is the role of UV radiation in skin cancer formation? 4. Name some oncogenes and tumor suppressors. How are these linked to skin cancer? 5. What does xeroderma pigmentosum teach us about skin cancer biology? 6. What does "basal cell nevus syndrome" teach us about skin cancer formation? 7. Why are organ transplant recipients more susceptible to skin cancer formation?
answer
Questions to ponder before and after the lecture:
question
Most common human malignancy, and incidence and prevalence are on the rise. In 2010, >2million people developed skin cancer. Cancers affecting other organ systems: - Skin: > 2 million - Genitourinary: 480,240 - Digestive (GI, liver, gallbladder, pancreas): 290,200 - Respiratory: 246,210 - Breast: 234,580
answer
Skin Cancer: Epidemiology
question
- Estimated prevalence (2007 SEER data): 13 million caucasians have had at least 1 skin cancer. - 1/5 Americans will develop skin cancer - 90% associated w/ UV radiation - Cost for treatment of non-melanoma skin cancer: > $1 billion Regardless of your future specialty or subspecialty, you will encounter skin cancer in your patients, friends, and family members.
answer
Here are some sobering statistics on skin cancer in the USA:
question
*Basal cell carcinoma (BCC)*: *8*0% (BC=80) *Squamous cell carcinoma (SCC)*: <20% *Malignant melanoma (MM)*: 3.5% (m looks like sideways 3) *Others (ex: sebaceous carcinoma, Merkel cell carcinoma)*: Rare
answer
The most common types of skin cancer are as follows:
question
Most common cancer in USA (>1,000,000 new cases per year); Median age at diagnosis: *68* y/o - 85% are found on *head and neck. (Sun-exposed sites)* *Precursor lesion*: None known *Precursor cell*: *long-term resident progenitor cells of the interfollicular epidermis and the upper infundibulum*

answer
Basal Cell Carcinoma (BCC)
question
*Risk of Metastasis*: Very *low* (Only several hundred reported in literature) - age-adjusted mortality: 0.12/100,000 - *early disease easily treated by surgical excision, curettage, or radiation* - BCCs are *"locally destructive" - neglected disease can lead to significant morbidity and even mortality* *Prognosis*: *Good*, unless lesion is very large or unresectable
answer
Basal Cell Carcinoma (BCC): Mets and Prognosis
question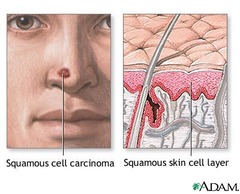
Seen in >250,000 Americans per year - 75% are on *sun-exposed surfaces (head and neck or hands)* *Precursor lesion*: *Actinic keratosis* - clinically appear as *scaly areas* - represent *early dysplasia ("pre-cancer") of epidermis*; a minority of these will progress to SCC - has potential to *progress into full thickness epidermal atypia (SCC in-situ - Bowen's disease) or invasive SCC* *Precursor cell*: *keratinocyte*
answer
Squamous Cell Carcinoma (SCC)
question
0.5-5%; can be higher in certain locations (scalp, lips, ears), and some subgroups (e.g., immunosuppressed patients) - MMPs are a family of 9 or more highly homologous Zn2+ endopeptidase that collectively cleave most of, if not all, the constituents of the ECM. MMP secretion and activation seems to result from a specific interaction between tumor and stromal cells. *Breakdown of tissue architecture mediated by MMPs allows squamous cell carcinoma to expand, invade neighboring blood vessels and spread to distant sites in body.*
answer
Squamous Cell Carcinoma (SCC): Risk of Mets
question
- *early disease easily treated by surgical excision, curettage, or radiation* - once *mets* have occurred, prognosis is *poor*
answer
Squamous Cell Carcinoma (SCC): Prognosis
question
Melanoma occurred in ~68,000 Americans in 2010, and was responsible for ~8700 deaths. - One person an hour dies of melanoma in US *Precursor lesion*: multiple possibilities: - *de novo (no precursor)* - *normal nevi* - *large congenital nevi* - *atypical nevi Precursor cell: melanocyte*

answer
Malignant Melanoma (MM)
question
*Risk of Mets*: depends on multiple factors, including depth of primary lesion, presence of ulceration, mitoses, etc. - *early disease easily tx'ed by surgical excision* *Prognosis*: highly variable" *Melanoma 5-yr relative survival rates (by stage at diagnosis)*: - All stages: 91% - Local disease: 98% - Regional disease: 62% *Distant disease: 15%*
answer
Malignant Melanoma (MM): Mets and Prognosis
question
Cancer can arise from any cell type found in the skin. - Mutations in smooth muscle cells found in arrector pili muscles can lead to leiomyosarcomas - Fibroblast mutations can lead to dermatofibrosarcomas - Endothelial cell mutations can lead to angiosarcoma - Merkel cell mutations can lead to Merkel cell carcinoma All of these are much less common than the "big 3" -- BCC, SCC, and melanoma
answer
Other Cutaneous Malignancies
question
In the 1780's British convicts sent to Australia became an unplanned population study on the role of UV in skin cancer formation. Introduction of a fair-skinned population into a high UV radiation climate highlights the role of sunlight in skin cancer.
answer
Role of UV in Skin Cancer: Clinical Observation
question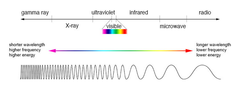
*UVC*: 200-280nm (sometimes listed as 290nm) *UVB*: 280/290 - 315nm (sometimes listed as 320nm) *UVA*: 315/320-400nm *The longer the wavelength, the deeper the penetration into the layers of the skin!*
answer
Electromagnetic spectrum:
question
*UVC*: - very damaging to DNA - fortunately *blocked by ozone* layer (when present) *UVB*: - *wavelength most responsible for sunburn ("solar erythema")* - sunscreens initially developed to try and prevent UVB-induced sunburn - most implicated in experimental models of photocarcinogenesis *UVA*: - less erythemogenic than UVB - predominant wavelength found in *tanning salons* - penetrates window glass - important role in *photoaging (penetrates deeper into the dermis)* - also implicated in *photocarcinogenesis* (make sure your sunscreen blocks UVA in addition to UVB)
answer
UVC, UVA, UVB
question
...
answer
Question: What is the role of sunlight (UV radiation) in skin cancer?
question
The multistage model of carcinogenesis describes three stages that are used to explain the change from a normal to a malignant clone: 1.) *Initiation* 2.) *Promotion* 3.) *Progression* This model is adapted for skin cancer, and known as the *photocarcinogenesis cascade*: *UV exposure --> DNA damage --> Mutations --> Malignant Transformation*
answer
Role of UV in Skin Cancer
question
In this stage, *cell undergoes DNA damage, usually due to a carcinogen* - tissue containing the affected cell is at this stage clinically normal - If mutated DNA is not repaired and/or the mutation does not trigger apoptosis, the cell is primed for further changes along the path to cancer
answer
Role of UV in Skin Cancer: *Initiation*
question
Initiated cell undergoes *further insult that leads to accumulation of further DNA mutations* - accumulated damage, when unchecked, allows *mutated cell to expand and form a clone of mutated cells* - this may eventually lead to *premalignant clinical lesions*
answer
Role of UV in Skin Cancer: *Promotion*
question
- *Further selective genetic damage* allows *mutated clone to progress into a malignant one* - Unchecked, this can *progress into in-situ and invasive cancer*
answer
Role of UV in Skin Cancer: *Progression*
question
...
answer
Question: What are lines of evidence that UV light causes skin cancer?
question
UV causes specific damage to DNA that is different from that caused by other carcinogens (e.g. tobacco): 1.) UV damage occurs at *adjacent pyrimidine bases (C or T); adjacent bases become covalently linked as pyrimidine dimers* 2.) During DNA replication, dimers increase *error rate in transcription*, leading to *erroneous substitutions of nucleotides* - Most common errors are: *C to T or CC to TT changes*; known as *"UV signature mutations"* - Identification of these specific changes suggests that UV was the proximate cause 3.) If these mutations occur w/in a *gene related to control of cell growth (oncogene or tumor suppressor gene)*, they can lead to *clonal expansion*
answer
Basic science evidence that UV causes Skin Cancer
question
Immortal, publicly available cancer cell line derived from metastatic melanoma cells - recent catalogue of the different mutations found in COLO-829 showed that most of the mutations were "UV signature mutations"
answer
COLO-829
question
- Genetic risk factors: *fair skin, light eyes, tendency to burn* rather than tan (less natural pigment as protection) - Chronic *sun exposure clearly linked with BCC and SCC* - Skin Cancer formation *Risk drops w/ decrease length* of sun exposure - Amount of ave *annual UV radiation directly correlates with incidence* of skin cancer formation - *Direct relationship* between the incidence of *non-melanoma skin cancer (BCCs and SCCs) and latitude*: the closer to *equator* (more UV exposure), the *higher the risk* - Extended courses of *medical UVA therapy* (in psoriasis and other skin conditions) associated w/ *increased risk for SCC* > BCC - *Intermittent sun* exposure (esp sunburns) linked with *melanoma*
answer
Clinical evidence that UV Light causes Skin Cancer
question
- Indoor tanning: $5 billion estimated revenue; 70% of patrons are women <30yrs of age. - *2.5x* increased risk of *SCC* - *1.5x* increased risk of *BCC* - *Exposure in youth increases melanoma risk by 75%*
answer
Clinical evidence that UV Light causes Skin Cancer - *Tanning*
question
UV exposure leads to DNA damage (UV signature mutations). Genetic defects in DNA repair lead to a dramatically increased skin cancer phenotype
answer
Role of Genetic Defects in Skin Cancer: Clinical Observation
question
...
answer
Question: How do genetic defects lead to skin cancer formation?
question
Once DNA damage has occurred, cell has several options: 1.) *Repair* damaged DNA 2.) Undergo programmed cell death (*apoptosis*) 3.) *Survive* w/ mutations *If cell survives w/out effective DNA repair, they can become precursors of damaged (initiated) clones which may progress to cancer*
answer
Genetic Defects and Skin Cancer
question
*DNA repair occurs by more than one molecular pathway* - *Nucleotide excision repair (damaged DNA is excised and replaced w/ correct base sequence)* is a DNA repair pathway that is well characterized. - Genetic diseases have shed light on the importance of DNA repair.
answer
Role of DNA Repair
question
Group of *autosomal recessive* disorders that involve *defects in DNA nucleotide excision repair enzymes XPA-XPG* - these genes related to several different aspects of DNA repair - *XP-A* caused by reduced recognition of damaged DNA - *XP-B* caused by abnormal helicase (necessary to unwind DNA for repair) Pts w/ XP exposed to UV light, have a *markedly high risk of skin cancer development* (increased at least 1000X). *Strict avoidance of UV is crucial* to decrease skin cancer formation, and to minimize morbidity and mortality of this condition.
answer
Xeroderma pigmentosa (XP)
question
- has been shown that *DNA repair capacity declines with age* - may at least partly explain *increased risk of skin cancer as pt ages* - some pts w/ *skin cancers at a early age* have been shown to have *measurable deficiencies in DNA repair* - evidence that *cells respond to sublethal damage by up-regulating genes involved in DNA repair (SOS response)*. *Lack of this inducible repair capacity may also explain earlier onset of skin cancer in some younger pts*.
answer
Several other clinical examples show role of DNA repair in skin cancer formation:
question
Apoptosis allows removal of mutated cells. *Apoptosis following UV exposure skin is manifested by presence of "sunburn cells" - apoptotic or dying keratinocytes*. - Mouse experiments have shown importance of normal *p53 in facilitating apoptosis*, as well as the role of *Fas and Fas ligand (FasL)* *Keratinocytes express Fas*, and exposure to its ligand (e.g. from T-lymphocytes or other keratinocytes) *induces apoptosis*. In mice *deficient in FasL, sunburn cells are not produced after UV exposure, and mice accumulate far more mutations* in keratinocytes (fewer damaged cells eliminated by apoptosis).
answer
Role of Apoptosis in Skin Cancer
question
Mutations that *increase potential for unregulated growth are more beneficial to cancer formation*. - Damage to *genes related to cellular proliferation (oncogenes, tumor suppressor genes, and regulators* of these) are of significant consequence in *tumor initiation and progression*
answer
Not all genes are created equal - Oncogenes and Tumor Suppressor Genes
question
Genes involved in *regulation of cellular proliferation and differentiation* - e.g. these genes may code for GF's or their receptors, signal transduction proteins, or nuclear proteins involved in regulation and growth
answer
Proto-Oncogenes
question
Normal proto-oncogenes mutated --> become oncogenes Oncogenes *acquire oncogenic potential w/ DNA mutation* - Examples of oncogenes are *raf, myc, ras* Normal cells need appropriate growth signals to be present to allow for cellular proliferation. An *oncogene allows the cell to be inappropriately "turned on." - ON-go-gene* - If external growth signals are no longer needed, there is a loss of growth regulation - Oncogenes behave in a *dominant fashion: change in 1 of the 2 alleles leads to a gain-of function mutation - only one allele mutation is needed to drive cell growth*
answer
Oncogenes and Skin Cancer
question
Example of proto-oncogene/oncogene Ras family members (ex: H-ras, N-ras, K-ras) is *mutated in a significant number of human cancers* *Proto-oncogene*: involved in signal transduction *Oncogenic transformation*: leads to a chronically active ras, which *increases the signaling cascade, and leads to increased downstream transcription*
answer
Ras Oncogene
question
Oncogenes play role in skin cancer - Mutations in oncogenes are seen in melanoma: *20-30% of melanomas have activating N-Ras mutations, and 55-60% have BRAF mutations* - up to *20-25% of SCCs may have activating mutations in ras oncogene*
answer
Oncogenes in Skin Cancer
question
*Encode proteins whose normal function is to act as a brake on cellular proliferation and differentiation* - Loss of tumor suppressor function can occur by *DNA mutation* or by *inactivation of the protein product* - Tumor suppressors act in *recessive fashion - loss of both alleles is required to remove the brake* - In certain genetic syndromes, an inherited defective allele (heterozygous germline mutation) predisposes the affected pt, because only one mutation (somatic mutation of the remaining normal allele) is required for full loss of function *Two Hit Hypothesis*
answer
Tumor Suppressor Genes
question
In skin, there are *2 key tumor suppressor genes* that play a role in non-melanoma skin cancer development: *Tp53 gene and PTCH (patched) gene* - the *CDKN2A (INK4A) gene locus* is important in some pts w/ *familial melanoma*
answer
Tumor Suppressor Genes and Skin Cancer
question
*Tumor suppressor gene*; controls signaling pathways and helps regulate cell cycle progression, DNA repair, and programmed cell death = protects DNA integrity in response to stressors such as radiation *Mutation in p53* decreases protection and allows for increased mutations; *p53 is an exception to two-hit rule for tumor suppressors* - Normal p53 protein has a tetramer configuration, and incorporation of one mutant allele product into tetramer leads to defective p53 protein (*dominant-negative phenotype*) - Can also be *inactivated when bound by other proteins* (ex: human papillomavirus E6 binding seen in SCCs) - mutations very *common in SCC* - mutations are *UV-induced*, occur *early in progression to SCC*, and are found in *precursor lesions* (actinic keratoses), in-situ disease (SCC in-situ), and invasive SCCs - p53 mutations are also found in *>50% of BCC*
answer
p53
question
*Basal cell nevus syndrome (BCNS)*: autosomal *dominant* disorder w/ a mutation in PTCH ("Patched") - PTCH is a *tumor suppressor* that plays a normal *role in embryonic growth and development* -PTCH mutation leads to a syndrome that includes *multiple BCCs, palmar/plantar pits, skeletal abnormalities, and calcification of the falx cerebri* - *BCC* development in BCNS pts is *still related to sun exposure* (occur more frequently in sun-exposed sites), but pts have *dramatically increased numbers of BCCs* - PTCH mutations also found in *sporadic BCCs in pts who do not have basal cell nevus syndrome*
answer
PTCH
question
Melanoma genetics are complicated; *DKN2A* = most well described *gene locus associated w/ familial melanoma* - *Germline CDKN2A mutations* seen in up to *25% of familial melanoma* - CDKN2A *encodes for 2 tumor suppressor proteins: p16 and p14ARF* that *regulate cell cycle via retinoblastoma and p53* pathways - *activation of either p16 or p14ARF will lead to cell cycle arrest*

answer
CDKN2A (INK4A)
question
Genetic testing is available for CDKN2A but is not performed routinely; important to note that *familial melanomas account for only ~10% of total melanomas* - in absence of strong evidence of familial disposition to melanoma, *pre-test probability of CDKN2A defect is low in pt w/ single melanoma* *Criteria recommended for those considering testing*: - personal history of 3+ invasive melanomas - and/or Fam Hx of invasive melanoma - AND a Fam Hx of 2+ invasive melanoma or pancreatic cancer (all in same side of the family)
answer
CDKN2A (INK4A): Genetic Testing
question
Complex 1.) CDKN2A, w/ Rb and p53 2.) *Ras/MAPK pathway* also described in melanoma (*BRAF, N-ras - oncogenes*) 3.) *differences in frequency of mutations of melanomas in sun exposed versus non-sun exposed* skin: - Melanomas that occur on skin w/ *intermittent sun exposure* appeared to have *significantly higher rates of BRAF mutation* compared to non-exposed skin (acral and mucosal melanomas) - *c-KIT mutations* appear to occur *more commonly in acral and mucosal melanomas*
answer
Melanoma Genetics (beyond CDKN2A...)
question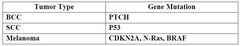
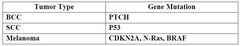
*BCC*: PTCH *SCC*: P53 *Melanoma*: CDKN2A, N-Ras, BRAF
answer
Tumors and Genes Summary
question
Some immunosuppressed patients (ex: organ transplants patients) have a significantly increased incidence of skin cancer.
answer
Multistage Model of Carcinogenesis: Role of Immunosuppression in Skin Cancer: Clinical Obersvation
question
...
answer
Question: Name some reasons why immune suppression can lead to more skin cancers?
question
DNA damage --> DNA repair --> if this does not occur, and cell becomes malignant, *circulating immune cells can remove mutated cells ("immune surveillance")* to prevent them from progressing to cancer 1.) *Organ transplant pts *have increased risk of skin cancer - *SCC*. depending on other risk factors, is *up to 40-250x* that of general pop - *BCC is 5-10x* higher 2.) *Other types of immunosuppression* may also have increased risk - *HIV* --> increased risk for *cutaneous SCC*, and these SCCs can be much *more aggressive*
answer
Multistage Model of Carcinogenesis: Role of Immunosuppression in Skin Cancer *Development*
question
In addition to increased risk of skin cancer formation, *tumors may behave more aggressively* - in a series of cardiac transplant pts in Australia, 27% died of skin cancer (majority were SCCs) - in a series of renal transplant pts in US, 5% died of skin cancer - Even in those pts w/ less aggressive skin cancers, *management of their multiple skin cancers can be difficult*. Skin cancer is a source of *significant morbidity and mortality in transplant pts*.
answer
Multistage Model of Carcinogenesis: Role of Immunosuppression in Skin Cancer *Progression*
question
Multiple reasons why transplant pts have more/more aggressive skin cancers - *Decreased immune surveillance impairs removal of DNA damaged cells* - Decreased surveillance allows for *increased HPV infection* - Transplant associated SCCs have high rates of HPV infection (up to 70-90% tumors have HPV DNA) - HPV thought to act as a *co-carcinogen to UV - HPV protein E6 inactivates tumor suppressor p53, and HPV E7 inactivates tumor suppressor retinoblastoma (Rb)*
answer
Multistage Model of Carcinogenesis: Role of Immunosuppression in Skin Cancer - *Mechanism*
question
- There is an epidemic of skin cancer - 3 most common skin cancers are BCC, SCC, and melanoma - UV radiation is a carcinogen and intimately involved in the development of skin cancer - DNA repair is important in cutaneous malignancies (Xeroderma pigmentosum) - Tumor suppressors play an important role in skin cancers (p53, PTCH, CDKN2A) - Immune surveillance is important in cancer prevention. Organ transplant pts have marked increase in skin cancer risk.
answer
Skin Cancer Summary



