AH1-Chapter 31 Nursing Management of Hematologic Problems – Flashcards
Unlock all answers in this set
Unlock answersquestion
What type of anemia results from red blood cell destruction? Bleeding Hemolytic Hypoproliferative None of the above
answer
Hemolytic Bleeding results from red blood loss. Hemolytic anemia results from red blood cell destruction. Hypoproliferative anemia results from defective red blood cell production.
question
True or False Leukocytosis refers to a decreased level of leukocytes in the circulation.
answer
False Leukocytosis refers to an increased level of leukocytes in the circulation. Leukopenia refers to a decreased level of leukocytes in the circulation.
question
What should any elderly patient be evaluated for whose chief complaint is back pain and has an elevated total protein level? Anemia Leukemia Multiple myeloma Non-Hodgkin's lymphoma
answer
Multiple myeloma Any elderly patient whose chief complaint is back pain and has an elevated total protein level should be evaluated for possible myeloma.
question
Hemolysis means:
answer
(blood rupturing) the rupturing of erythrocytes (red blood cells) and the release of their contents (hemoglobin) into surrounding fluid (e.g., blood plasma).
question
When you think hemolytic, think:
answer
RBC destruction
question
Leukocytosis refers to
answer
an increased level of leukocytes in the circulation.
question
Leukopenia refers to
answer
a decreased level of leukocytes in the circulation.
question
Normal Lab Values: WBC
answer
4500-11,000/mm³
question
Normal Lab Values: Hemoglobin
answer
Male: 13-18 g/dL Female: 12-16 g/dL
question
Normal Lab Values: Hematocrit
answer
Male: 42-52% Female: 35-47%
question
Normal Lab Values: Iron
answer
Male: 75 to 175 g/dL Female: 65 to 165 g/dL
question
Normal Lab Values: Platelet
answer
150,000- 450,000/mm³
question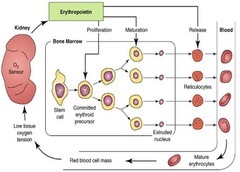
Kidneys and Blood Cell Production
answer
Think about: Renin - Angiotensin - Aldosterone System
question
*Why the Renin-Angiotensin-Aldosterone System begins during heart failure:*
answer
Activation of the renin-angiotensin-aldosterone (RAA) system rapidly kicks in with heart failure. This is due to decreased renal perfusion caused by both a reduction in cardiac output and redistribution of blood away from nonessential organs --> this leads to the kidney starting to retain sodium and water in response to the perception of ineffective blood volume. The perception of decreased blood volume and the increase in sympathetic nervous activity --> stimulates renin release from the juxtaglomerular cells in the kidneys.
question
Erythropoietin (EPO)
answer
is a hormone produced by the kidney that promotes the formation of red blood cells by the bone marrow. medication: Procrit (3 or so times/week)
question
How is erythropoietin made?
answer
The kidney cells that make erythropoietin are specialized so that they are sensitive to low oxygen levels in the blood that travels through the kidney. These cells make and release erythropoietin when the oxygen level is too low. The low oxygen level may indicate anemia, a diminished number of red blood cells, or hemoglobin molecules that carry oxygen through the body.
question
What exactly does erythropoietin (EPO) do?
answer
it stimulates the bone marrow to produce more red blood cells --> this rise in red blood cells increases the oxygen-carrying capacity of the blood.
question
As the prime regulator of red cell production, erythropoietin's major functions are to:
answer
1. Promote the development of red blood cells. 2. Initiate the synthesis of hemoglobin, the molecule within red blood cells that transports oxygen.
question
What medication are dialysis patients often placed on?
answer
Procrit r/t kidney malfunction and lack of erythropoietin production
question
Damage to the kidney can lead to anemia how?
answer
it inhibits the kidney function and possibly inhibits its ability to produce erythropoietin. *medications (filtering of) and radiation can lead to kidney malfunction*
question
Lymphoid cells
answer
T cells and B cells
question
Myloid cells
answer
Erythrocytes Leukocytes Platelets
question
How are RBC's described?
answer
by size and by amount of hemoglobin present. Size = "-cytic" Amount of hemoglobin = "-chromic"
question
Reticulocyte Count Normal Range
answer
0.5 - 1.5 *The reticulocyte count is used to help determine if the bone marrow is responding adequately to the body's need for red blood cells (RBCs) and to help determine the cause of and classify different types of anemia.*
question
Why does anemia take a few months to recover
answer
- RBC lifespan is 120 days - can give blood transfusion (very fast recovery) - erythropoietin (EPO) (Procrit)
question
Erythrocyte Dx Tests
answer
Complete Blood Count RBC Hemoglobin (this is a biggie) Hematocrit (this is a biggie) MCV (mean corpuscular volume) MCHC (mean corpuscular hemoglobin concentration)
question
What is Hemoglobin test
answer
- the measure of hemoglobin in the blood - the O2 carrying ability of the blood
question
What is Hematocrit test
answer
the volume percentage (%) of red blood cells in blood.
question
What is MCV (mean corpuscular volume)
answer
a measure of the average red blood cell
question
What is MCHC (mean corpuscular hemoglobin concentration)
answer
a measure of the concentration of hemoglobin in a given volume of packed red blood cells
question
Bone Marrow Aspiration and Biopsy
answer
Informed consent is REQUIRED! Major hazards: Bleeding and Infection
question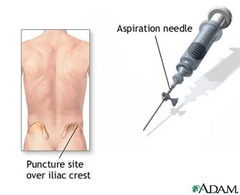
Bone Marrow Aspiration Site
answer
*remember that bone marrow is a liquid and looks like blood*
question
What are the Erythrocyte Disorders that we will cover?
answer
Anemia Polycythemia Vera
question
What is Anemia
answer
- Decrease in quantity of RBCs and/or - an Abnormality in Hgb content - need to identify causative agent
question
Anemia Signs and Symptoms
answer
- fatigue - thirst - cold - pale - mucous membranes pale - cap refill long - cyanosis - tachycardia (heart is trying to compensate for low O2) - dizziness (think safety - slow position change) - nausea - inceased respiratory rates - clubbing with chronic anemia - hair loss in periphery
question
Anemia Tx Focus
answer
- Underlying disorder or causative agent - Symptom relief - transfusion (meds given during: lasix, benadryl, tylenol) - possible fluid volume overload r/t transfusion - transfusion given over long period of time (4 or so hrs/unit) - Procrit
question
How much should the HCT increase with each unit of blood given?
answer
2-3 pts per unit *if there isn't an increase, think about a possible bleed or hemolytic disorder (spleen "eating" RBC's)*
question
Anemia: Nursing Process - Assessment
answer
- Weakness, fatigue, general malaise - Pallor of skin and mucous membranes - Jaundice - Beefy red tongue - Medications (many meds, many side effects) - EtOH (hepatosplenomegaly)(hang banana bag) - Nutrition - Cardiac/GI/Neuro - Unusual cravings (PICA)(ice eating) - Females: Menstrual History (pads per day)
question
Anemia: Nursing Process - Planning and Goals
answer
- Increased tolerance of normal activity - Attainment or maintenance of adequate nutrition - Maintenance of adequate tissue perfusion - Compliance with prescribed therapy - Absence of complications
question
Anemia: Nursing Process - Interventions
answer
- Manage Fatigue - Maintain Adequate Nutrition - Maintain Adequate Perfusion - Comply with Prescribed Therapy - Monitor and Manage Potential Complications
question
Types of Anemia
answer
- Aplastic - Iron Deficiency - Folic Acid Deficiency - Vitamin B12 Deficiency - Sickle Cell
question
The differences in Anemia Treatment is
answer
- Not much difference between the types - biggest difference is the medications used to tx the deficiency
question
Aplastic Anemia
answer
- Caused by decrease in or damage to marrow stem cells - toxic anemia - Neutropenia - wbc below 1500 - Thrombocytopenia - low platelets usu below 100k (can give transfusions - just platelets) - can give plasma to increase blood volume - Anemia = know relationship between HCT and Hgb (Hgb is usu 2-3 times HCT)
question
Iron Deficiency Anemia
answer
- Intake of dietary iron is inadequate for hemoglobin synthesis - think Children and Pregnant women
question
Clinical Management of Iron Deficiency Anemia
answer
- Stool specimens for occult blood - Colonoscopy or endoscopy (check for bleeding) - Iron supplementation: Dietary and Medication - usually give meds r/t not enough intake in diet
question
Iron Supplements
answer
- causes constipation - usu on supplemental bowel regiment - stool softener, miralax, lots of liquids - causes tarry stool (can through off hemoccult) - drink through a straw (if liquid) - don't drink with milk - Vit C increases absorption - take on empty stomach
question
Folic Acid Deficiency
answer
- Folic acid stored as different compounds called folates - pregnant women - multivitamins have high folic acid level - children = neural tube deficit --> spina bifida
question
Normal Range for Folic Acid
answer
2.5 - 20 ng/mL
question
Vitamin B12 Deficiency Pernicious Anemia
answer
- r/t faulty absorption in GI tract: (crohn's disease, gastrectomy, ileal resection) - dietary deficiency is rare but can develop in strict vegetarians - high cases of this in gastric bypass - probably the most common type of anemia seen - Tx: B-12 is given IM
question
What are normal B-12 Levels
answer
200-900 pg/mL
question
Sickle Cell Anemia
answer
- Hgb molecule is defective - disk shape of cell becomes deformed, rigid and sickle shaped --> can cause damage to vessel walls - pt will c/o pain in certain parts of the body
question
Sickle Cell Anemia Tx
answer
- transfusions - tx symptoms/pain if refuse blood transfusion - possible genetic therapy - protects against malaria - shortened life expectancy
question
Sickle Cell Anemia Signs/Symptoms
answer
- anemia (7-10 hgb) - jaundice - liver trying to get rid of damaged cells and build up in liver decreases fnxn - tachycardia (compensation) - cardiac murmurs - thrombosis - abn cells stick together and clot, cause pain, need blood thinner - infections - WBC might not fnxn corrctly r/t irregular WBC related to malformation - avascular necrosis (often in hip) - stroke - death
question
Sickle Cell Anemia - Sickle Cell Crisis
answer
- Sickle Cell Crisis - Acute Chest Syndrome - get fluids, O2 and pain meds - possibly blood transfusion - think dehydration --> thickens blood --> leads to crisis - affects developmental mile stones in children - Clinical Management: Bone Marrow Transplant, Hydroxyurea, RBC transfusion
question
Sickle Cell Crisis
answer
- intense pain because blood vessels can become blocked or the defective red blood cells can damage organs in the body. - assessment: determine the factor precipitating crisis - manage pain levels - all body systems must be assessed
question
Sickle Cell Crisis Interventions
answer
- manage pain - preventing and managing infection - promote coping skills monitoring for potential complications can affect developmental milestones in children - pts can be at high risk for addiction r/t medications - hydroxyurea helps relieve pain - stem cells from umbilical stem cells can help with autotransfusion
question
Sickle Cell Crisis Nursing Dx
answer
Based on the assessment data, major nursing diagnoses for the patient with sickle cell crisis may include: - Acute pain related to tissue hypoxia due to agglutina- tion of sickled cells within blood vessels - Risk for infection - Risk for powerlessness related to illness-induced helplessness - De?cient knowledge regarding sickle crisis prevention
question
Sickle Cell Crisis Collaborative Problems/Potential Complications
answer
Based on the assessment data, potential complications may include: - Hypoxia, ischemia, infection, and poor wound healing leading to skin breakdown and ulcers - Dehydration - Cerebrovascular accident (CVA, brain attack, stroke) - Anemia - Acute and chronic renal failure - Heart failure, pulmonary hypertension, and acute chest syndrome - Impotence - Poor compliance - Substance abuse related to poorly managed chronic pain
question
Hydroxyurea is
answer
- an antineoplastic drug - used to reduce the number of painful crisis in sickle cell anemia and decreased need for transfusions in adult patients with a history of recurrent moderate to severe crises -
question
Hydroxyurea SE:
answer
nausea, vomiting, diarrhea, constipation, drowsiness
question
Patient, while taking Hydroxyurea, should contact the doctor if what occurs?
answer
- rash, - purple/blue or black discoloration of the skin or nails - loss of feeling in one area of the body - sores on the skin or in the mouth - foul-smelling substance oozing from the skin - swelling of the hands/feet/ankles or lower legs
question
Acute Chest Syndrome is:
answer
a noninfectious vaso-occlusive crisis of the pulmonary vasculature commonly seen in patients with sickle cell anemia. It is characterized by a new infiltrate on a chest x-ray.
question
Acute Chest Syndrome Cause
answer
The crisis is often initiated by a lung infection, and the resulting inflammation and loss of oxygen tension leads to sickling of red cells and further vasoocclusion.
question
Acute Chest Syndrome Symptoms
answer
The crisis is a common complication in sickle-cell patients and can be associated with one or more symptoms including fever, cough, sputum production, dyspnea, or hypoxia.
question
Acute Chest Syndrome Treatment
answer
Broad spectrum antibiotics to cover common infections like strep pneumoniae and mycoplasma, Pain control, and Blood transfusion
question
Polycythemia Vera Etiology:
answer
hyper-cellular bone marrow leading to elevated RBC, WBC, and platelets
question
Polycythemia Vera Symptoms
answer
Symptoms result from increased blood volume and increased blood viscosity - headache - red faced - swollen veins - dizziness r/t too much blood
question
Polycythemia Vera Treatment
answer
relies primarily on phlebotomy to reduce hematocrit - bleed them/ drain them (usually 1 or so a week or monthly)
question
Hemostasis
answer
control of bleeding
question
Platelets
answer
essential in control of bleeding
question
Thrombocytopenia
answer
- a decrease in the number of circulating platelets - no aspirin, no blade razor shaving, no flossing, no contact sports
question
Thrombocytopenia Etiology
answer
- Decreased production in bone marrow - Increased destruction of platelets (d/t antibodies) - Increased consumption (by the spleen)
question
Vitamin K Deficiency leads to
answer
impaired synthesis of coagulation factors - can give Vit K PO or IM - IM to counter Warfarin
question
Thrombocytosis
answer
- Increased number of platelets - Usually due to a stem cell disorder - risk of blood clots - Platelets are immature - Result of contributing diseases: Chronic Inflammatory Disorder, Iron Deficiency, Malignant Disease, Splenectomy - will be on some form of blood thinner
question
White Blood Cell Disorders
answer
White blood cells are formed in the bone marrow and have as a primary function to recognize and fight micro-organisms.
question
Neutropenia is
answer
a decrease in the number of neutrophils resulting in risk of infection - Neupagen - remember precautions: no flowers or fresh fruit or kids, etc
question
Leukemia is
answer
- proliferation of one class of white blood cells - can be acute or chronic - Acute: sudden onset with poorly differentiated cells - Chronic: slow onset with well defined cells
question
Symptoms of Leukemia
answer
- Pallor - Fatigue - Frequent infections - Bleeding, bruising - Bone pain (amped up bone marrow leads to pain) - Weight loss (cancer deprives body of nutrients)
question
Leukemia Tx
answer
- chemotherapy - transfusion of bone marrow, stem cells, platelets - no radiation (can't radiate all of the body and the blood)
question
Chronic Leukemia
answer
- usually seen in older adults (60's) - Cells are fully mature - Early on there are few symptoms - Later there is splenomegaly; hepatomegaly; lymphadenopathy
question
Chronic Lymphocytic Leukemia
answer
- usually seen later in life - presents with anemia and thrombocytopenia - later it will present with fever; night sweats; and weight loss - Primary treatment is chemotherapy
question
Gleevec is
answer
- antineoplastic/enzyme inhibitor - Inhibits kinases which may be produced by malignant cell lines - Inhibits production of malignant cell lines with decreased proliferation of leukemic cells
question
Gleevec SE/AE
answer
- CNS: fatigue, headache, weakness. Resp: cough, dyspnea, epistaxis, nasopharyngitis, pneumonia. - GI: HEPATOTOXICITY, abdominal pain, anorexia, constipation, diarrhea, dyspepsia, nausea, vomiting. - Derm: petechiae, pruritus, skin rash. - F and E: edema (including pleural effusion, pericardial infusion, anasarca, superficial edema and fluid retention), hypokalemia. - Endo: hypothyroidism. - Hemat: BLEEDING, NEUTROPENIA, THROMBOCYTOPENIA. - Metabolic: weight gain. - MS: arthralgia, muscle cramps, musculoskeletal pain, myalgia. - Misc: fever, night sweats.
question
Lymph System Roles
answer
- Maintain interstitial osmotic pressures - Absorb fat from the small intestine - Fight infection - Filter
question
Lymph System Disorders
answer
- Hodgkin's Disease - Non-Hodgkin's Lymphoma - Multiple Myeloma
question
Hodgkin's Disease
answer
- Cancer of lymphoid tissue - usually lymph nodes and spleen - interferes with the body's ability to fight infection - Diagnosed by presence of Reed Sternberg cells in tissue biopsy - The stage the disease is in dictates the treatment - usually seen in young males - early stages are fairly curable - later stages have worse prognosis - think lymph nodes are everywhere
question
Hodgkin's Disease Tx:
answer
- can use born marrow transfusion - can use chemotherapy - can use radiation
question
Non- Hodgkin's Lymphoma
answer
- Diffuse cancer of the lymphoid organs - Usually involves lymph nodes, liver, spleen, and bone marrow - Classification and ability to tolerate therapy determine treatment - usually in older patients - usually diagnosed at late stage --> more profuse spreading --> poor prognosis - B Symptoms: unintentional weight loss 10% or more, night sweat and fever - can spread to other organ systems r/t lymph system is systemic
question
Non- Hodgkin's Lymphoma is classified by:
answer
the type of lymphocyte that it is affecting - B cell Lymphoma (most common) - T cell Lymphoma - described as indulent or aggressive
question
Non- Hodgkin's Lymphoma symptoms
answer
- swollen lymph nodes - night sweats - fever - chills - fatigue - unexplained weight loss - facial swelling
question
Multiple Myeloma
answer
- Disease of most mature B lymphocyte, plasma cell - Medium survival 3-5 years, no cure - Nonfunctional immunoglobulin Monoclonal or M protein - Back pain with possible lytic lesions - no cure --> mgt of symptoms - check protein levels - usually diagnosed by lytic lesions - Hypercalcemia, anemia, and renal failure
question
What is also refered to as a Myeloma protein?
answer
- immunoglobulin - M Spike - Free light chains (Bence Jones)
question
Multiple Myeloma Etiology
answer
- 3 times as common as leukemia - most common in patients around 60 or 70 - rarely see myeloma cells floating in the blood stream - usually confined to bone marrow - will show anemia r/t myeloma cells overtaking the space where RBC's are made and that leads to lower levels of RBC - causes erosion of the bone --> leads to lytic lesions and hypercalcemia - myeloma proteins fragment --> move to kidneys --> can cause renal insufficiency or failure
question
Myeloma Acronym
answer
C - Calcium problems R - Renal problems A - Anemia B - Bone disorders
question
Multiple Myeloma Tx
answer
- can be considered (for some pts) a chronic disease - treatment can sometimes consist of 6 or so lines of tx - high dose chemotherapy with bone marrow stem cell replacement - proteasome inhibitors (Bortezomib or Carfilzomib) - IMIDs (Thalidomide, Lenolidomide, Pomalidomide) - personalized medications (genomics)
question
proteasome inhibitors (Bortezomib or Carfilzomib)
answer
- IM - as initial therapy or after progression; with melphalan and prednisone) - Inhibits proteasome, a regulator of intracellular protein catabolism, resulting in disruption of various intracellular processes - Leads to the death of rapidly replicating cells, particularly malignant ones
question
IMIDs (Thalidomide, Lenolidomide, Pomalidomide)
answer
- PO - immunosuppressants - used with newly diagnosed multiple myeloma (with dexamethasone) - Inhibits secretion of pro-inflammatory cytokines and increases secretion of anti-inflammatory cytokines - Slows progression of multiple myeloma - may cause neutropenia or thrombocytpenia



